Upper Cervical Manipulation and Manual Massage Do Not Modulate Sympatho-Vagal Balance or Blood Pressure in Women: A Randomized, Placebo-Controlled Clinical Trial
Abstract
1. Introduction
2. Materials and Methods
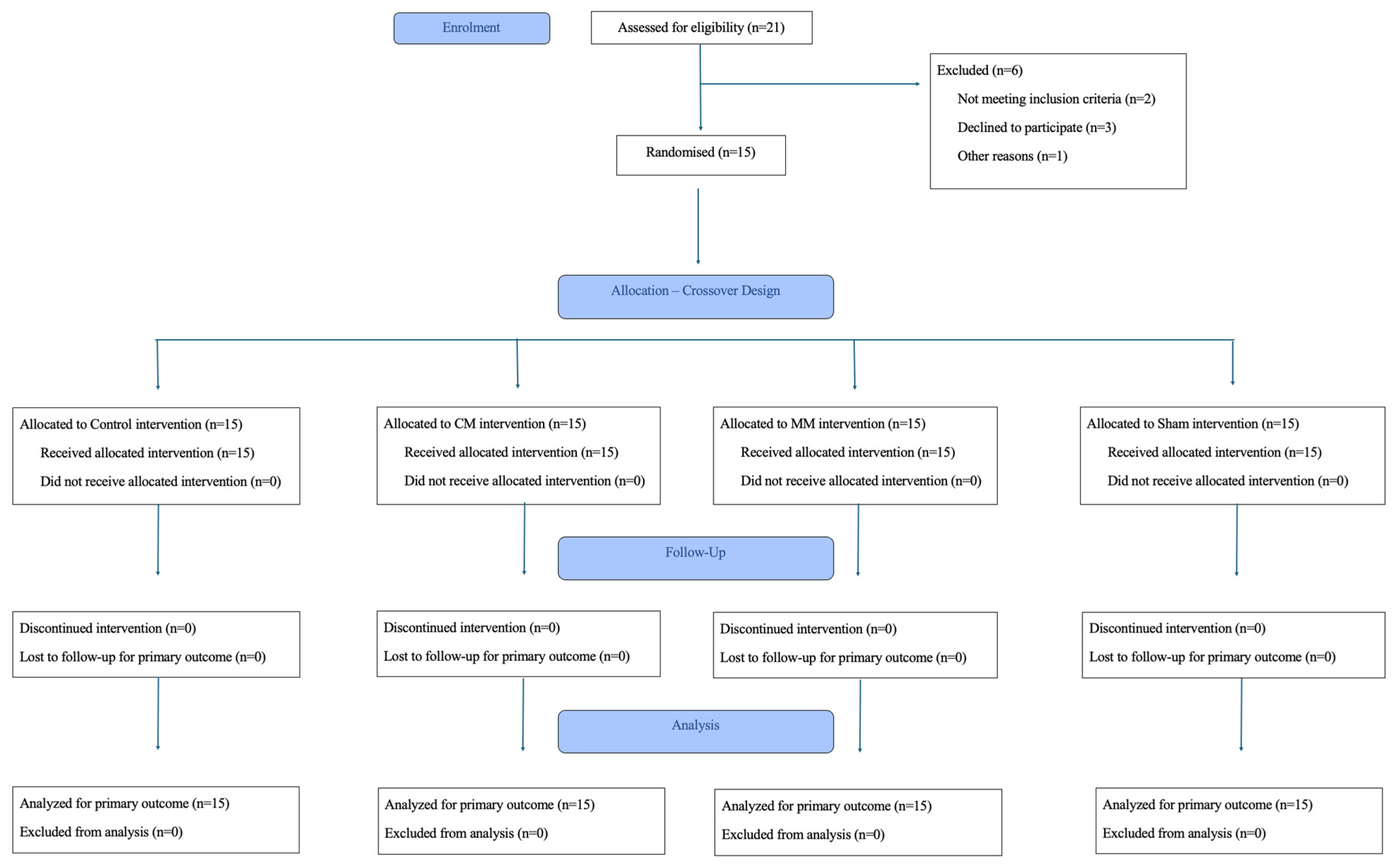
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Randomization
2.5. Interventions
2.6. Outcome Measures
2.7. Data Analysis
3. Results
3.1. Blood Pressure
3.2. Heart Rate Variability—Time-Domain
3.3. Heart Rate Variability—Frequency-Domain
4. Discussion
4.1. Limitation
4.2. Future Research Recommendation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANS | Autonomic Nervous System |
| BP | Blood Pressure |
| CONSORT | Consolidated Standards of Reporting Trials |
| CM | Cervical Spinal Manipulation |
| HRV | Heart Rate Variability |
| MM | Manual Massage |
| NCD | Non-Communicable Diseases |
| SHAM | Simulated Cervical Spinal Manipulation |
| SPIRIT | Standard Protocol Items: Recommendations for Interventional Trials |
References
- Mills, K.T.; Stefanescu, H.J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Schiffrin, E.L. Immune mechanisms in hypertension and vascular injury. Clin. Sci. 2014, 126, 267–274. [Google Scholar] [CrossRef]
- Ringwald-de Meyer, S.; de La Harpe, R.; Vollenweider, P.; Marques-Vidal, P.; Vaucher, J. Factor associated with and risk of cardiovascular disease in people with uncontrolled hypertension. Sci. Rep. 2025, 15, 375. [Google Scholar] [CrossRef]
- Pescatello, L.S.; Buchner, D.M.; Jakicic, J.M.; Powell, K.E.; Kraus, W.E.; Bloodgood, B.; Campbell, A.W.; Dietz, S.; Dipietro, L.; George, S.M.; et al. Physical activity to prevent and treat hypertension: A systematic review. Med. Sci. Sports Exerc. 2019, 51, 1314–1323. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, E.R.; Pescatello, L.S.; Leitão, L.; de Miranda, M.J.C.; Marchetti, P.H.; Novaes, M.R.; da Silva Araújo, G.; Corrêa Neto, V.G.; da Silva Novaes, J. Muscular performance and blood pressure after different pre-strength training strategies in recreationally strength-trained women: Cross-over trial. J. Cardiovasc. Dev. Dis. 2025, 12, 7. [Google Scholar] [CrossRef]
- Jänig, W. The Integrative Action of the Autonomic Nervous System: Neurobiology of Homeostasis; Cambridge University Press: Cambridge, UK; New York, NY, USA, 2006. [Google Scholar]
- Vanderlei, L.C.M.; Pastre, C.M.E.; Hoshi, R.A.; De Carvalho, T.D.; De Godoy, M.F. Basic notions of heart rate variability and its clinical applicability. Rev. Bras. Cir. Cardiovasc. 2009, 24, 205–217. [Google Scholar] [CrossRef]
- Lastova, K.; Nordvall, M.; Walters-Edwards, M.; Allnutt, A.; Wong, A. Cardiac autonomic and blood pressure responses to an acute foam rolling session. J. Strength Cond. Res. 2018, 32, 2825–2830. [Google Scholar] [CrossRef]
- Picchiottino, M.; Honoré, M.; Leboeuf-Yde, C.; Gagey, O.; Cottin, F.; Hallman, D.M. The effect of a single spinal manipulation on cardiovascular autonomic activity and the relationship to pressure pain threshold: A randomized, cross-over, sham-controlled trial. Chiropr. Man. Therap. 2020, 28, 7. [Google Scholar] [CrossRef] [PubMed]
- Jupin, C.; Aibar, V.B.; Sarhan, F.R. Short-Term Effects of Spinal Manual Therapy on the Nervous System in Managing Musculoskeletal Pain: A Systematic Review. J. Clin. Med. 2025, 14, 3830. [Google Scholar] [CrossRef] [PubMed]
- Bell, S.; D’Angelo, K.; Kawchuk, G.N.; Triano, J.J.; Howarth, S.J. Procedure selection and patient positioning influence spine kinematics during high-velocity, low-amplitude spinal manipulation applied to the low back. J. Manip. Physiol. Ther. 2017, 40, 147–155. [Google Scholar] [CrossRef] [PubMed]
- Hidalgo, B.; Hall, T.; Bossert, J.; Dugeny, A.; Cagnie, B.; Pitance, L. The efficacy of manual therapy and exercise for treating non-specific neck pain: A systematic review. J. Back Musculoskelet. Rehabil. 2017, 30, 1149–1169. [Google Scholar] [CrossRef]
- Gross, A.; Langevin, P.; Burnie, S.J.; Bédard-Brochu, M.-S.; Empey, B.; Dugas, E.; Faber-Dobrescu, M.; Andres, C.; Graham, N.; Goldsmith, C.H.; et al. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database Syst. Rev. 2015, 2015, CD004249. [Google Scholar] [CrossRef]
- Coulter, I.D.; Crawford, C.; Hurwitz, E.L.; Vernon, H.; Khorsan, R.; Booth, M.S.; Herman, P.M. Manipulation and mobilization for treating chronic low back pain: A systematic review and meta-analysis. Spine J. 2018, 18, 866–879. [Google Scholar] [CrossRef]
- Rubinstein, S.M.; de Zoete, A.; Van Middelkoop, M.; Assendelft, W.J.J.; De Boer, M.R.; Van Tulder, M.W. Benefits and harms of spinal manipulative therapy for the treatment of chronic low back pain: Systematic review and meta-analysis of randomised controlled trials. BMJ 2019, 364, l689. [Google Scholar] [CrossRef]
- Beardsley, C.; Škarabot, J. Effects of self-myofascial release: A systematic review. J. Bodyw. Mov. Ther. 2015, 19, 747–758. [Google Scholar] [CrossRef]
- Knutson, G.A. Significant changes in systolic blood pressure post vectored upper cervical adjustment vs resting control groups: A possible effect of the cervico sympathetic and/or pressor reflex. J. Manipulative Physiol. Ther. 2001, 24, 101–109. [Google Scholar] [CrossRef]
- Ward, J.; Tyer, K.; Coats, J.; Williams, G.; Weigand, S.; Cockburn, D. Immediate effects of atlas manipulation on cardiovascular physiology. Clin. Chiropr. 2012, 15, 147–157. [Google Scholar] [CrossRef]
- Yung, E.; Wong, M.; Williams, H.; Mache, K. Blood pressure and heart rate response to posteriorly directed pressure applied to the cervical spine in young, pain-free individuals: A randomized, repeated-measures, double-blind, placebo-controlled study. J. Orthop. Sports Phys. Ther. 2014, 44, 622–626. [Google Scholar] [CrossRef] [PubMed]
- Win, N.N.; Jorgensen, A.M.S.; Chen, Y.S.; Haneline, M.T. Effects of Upper and Lower Cervical Spinal Manipulative Therapy on Blood Pressure and Heart Rate Variability in Volunteers and Patients With Neck Pain: A Randomized Controlled, Cross-Over, Preliminary Study. J. Chiropr. Med. 2015, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Goertz, C.M.; Salsbury, S.A.; Vining, R.D.; Long, C.R.; Pohlman, K.A.; Weeks, W.B.; Lamas, G.A. Effect of Spinal Manipulation of Upper Cervical Vertebrae on Blood Pressure: Results of a Pilot Sham-Controlled Trial. J. Manip. Physiol. Ther. 2016, 39, 369–380. [Google Scholar] [CrossRef] [PubMed]
- Monteiro, E.R.; Pescatello, L.S.; Winchester, J.B.; Neto, V.G.C.; Brown, A.F.; Budde, H.; Marchetti, P.H.; Silva, J.G.; Vianna, J.M.; da Silva Novaes, J. Effects of Manual Therapies and Resistance Exercise on Postexercise Hypotension in Women With Normal Blood Pressure. J. Strength Cond. Res. 2022, 36, 948–954. [Google Scholar] [CrossRef]
- Monteiro, E.R.; Budde, H.; Silva, J.G.; Oliveira, A.; Novaes, J.S.; de Jesus, I.R.T. Enhance range-of-motion and hypotensive effect in elderly submitted to three manual therapy techniques: Cross-over study. J. Bodyw. Mov. Ther. 2024, 37, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Kopec, T. Acute Effects of a Single-Session of Full-Body Foam Rolling on Heart Rate Variability. Int. J. Ther. Massage Bodyw. 2022, 15, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Borges, B.L.A.; Bortolazzo, G.L.; Pasin Neto, H. Effects of spinal manipulation and myofascial techniques on heart rate variability: A systematic review. J. Bodyw. Mov. Ther. 2018, 22, 203–208. [Google Scholar] [CrossRef]
- Ketelhut, S.; Oechslin, L.; Zehnder, C.; Kubica, C.; Nigg, C.R. Acute self-myofascial release modulates cardiac autonomic function and hemodynamic parameters at rest and reduces cardiovascular stress reaction. Eur. J. Appl. Physiol. 2024, 124, 1535–1545. [Google Scholar] [CrossRef]
- Courties, A.; Berenbaum, F.; Sellam, J. Vagus nerve stimulation in musculoskeletal diseases. Jt. Bone Spine 2021, 88, 105149. [Google Scholar] [CrossRef]
- Cunningham, C.J.; Martínez, J.L. The Wandering Nerve: Positional Variations of the Cervical Vagus Nerve and Neurosurgical Implications. World Neurosurg. 2021, 156, 105–110. [Google Scholar] [CrossRef]
- Okamoto, T.; Masuhara, M.; Ikuta, K. Acute effects of self-myofascial release using a foam roller on arterial function. J. Strength Cond. Res. 2014, 28, 69–73. [Google Scholar] [CrossRef]
- Hotfiel, T.; Swoboda, B.; Krinner, S.; Grim, C.; Engelhardt, M.; Uder, M.; Heiss, R.U. Acute effects of lateral thigh foam rolling on arterial tissue perfusion determined by spectral doppler and power doppler ultrasound. J. Strength Cond. Res. 2017, 31, 893–900. [Google Scholar] [CrossRef]
- Monteiro, E.R.; Vingren, J.L.; Pescatello, L.S.; Neto, V.G.C.; Brown, A.F.; Kingsley, J.D.; Silva, J.G.; Vianna, J.M.; da Silva Novaes, J. Effects of foam rolling and strength training on post exercise hypotension in normotensive women: A cross-over study. J. Bodyw. Mov. Ther. 2023, 34, 81–86. [Google Scholar] [CrossRef]
- Monteiro, E.R.; Aguilera, L.M.; Ruá-Alonso, M.; Araújo, G.d.S.; Corrêa Neto, V.G.; Bentes, C.M.; Vilaça-Alves, J.; Reis, V.M.; Ferreira, A.d.S.; Marchetti, P.H.; et al. Effect of Manual Massage, Foam Rolling, and Strength Training on Hemodynamic and Autonomic Responses in Adults: A Scoping Review. Healthcare 2025, 13, 1371. [Google Scholar] [CrossRef]
- Hopewell, S.; Chan, A.-W.; Collins, G.S. CONSORT 2025 statement: Updated guideline for reporting randomised trials. BMJ 2025, 389, e081123. [Google Scholar] [CrossRef]
- Chan, A.-W.; Bourton, I.; Hopewell, S.; Moher, D.; Schulz, K.F.; Collins, G.S.; Tunn, R.; Aggarwal, R.; Berkwits, M.; Berlin, J.A.; et al. SPIRIT 2025 statement: Updated guideline for protocols of randomised trials. PLoS Med. 2025, 22, e1004589. [Google Scholar] [CrossRef]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the management of elevated blood pressure and hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef]
- Gorrell, L.M.; Sawatsky, A.; Edwards, W.B.; Herzog, W. Vertebral arteries do not experience tensile force during manual cervical spine manipulation applied to human cadavers. J. Man. Manip. Ther. 2022, 31, 261–269. [Google Scholar] [CrossRef]
- Hixson, K.M.; Horris, H.B.; McLeod, T.C.V.; Bacon, C.E.W. The Diagnostic Accuracy of Clinical Diagnostic Tests for Thoracic Outlet Syndrome. J. Sport Rehabil. 2017, 26, 459–465. [Google Scholar] [CrossRef] [PubMed]
- Strazewski, J. The Essentials of Toggle Recoil (HIO); J.W. Strazewski Publisher: Davenport, IA, USA, 2014; p. 120. [Google Scholar]
- 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA. Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Hypertension 2025, 82, e212–e316. [Google Scholar] [CrossRef] [PubMed]
- Chhetri, P.; Shrestha, L.; Mahatra, N.B. Validity of elite-hrv smartphone application for measuring heart rate variability compared to polar v800 heart rate monitor. J. Nepal Health Res. Counc. 2021, 19, 809–813. [Google Scholar] [CrossRef] [PubMed]
- Himariotis, A.T.; Coffey, K.F.; Noel, S.E.; Cornell, D.J. Validity of a smartphone application in calculating measures of heart rate variability. Sensors 2022, 22, 9883. [Google Scholar] [CrossRef]
- 2009 American College of Sports Medicine Position Stand. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med. Sci. Sports Exerc. 2002, 34, 364–380. [Google Scholar] [CrossRef]
- Beck, T.W. The importance of a priori sample size estimation in strength and conditioning research. J. Strength Cond. Res. 2013, 27, 2323–2337. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Bucher, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Pallant, J. SPSS Survival Manual: A Step By Step Guide to Data Analysis Using SPSS Program, 6th ed.; McGraw-Hill Education: London, UK, 2016. [Google Scholar]
- Gould, B.A.; Mann, S.; Davies, A.B.; Altman, D.G.; Raftery, E.B. Does placebo lower blood-pressure? Lancet 1981, 2, 1377–1381. [Google Scholar] [CrossRef] [PubMed]
- Benedetti, F.; Carlino, E.; Pollo, A. How placebos change the patient’s brain. Neuropsychopharmacology 2011, 36, 339–354. [Google Scholar] [CrossRef]
- Wilhelm, M.; Winkler, A.; Rief, V.; Doering, B.K. Effect of placebo groups on blood pressure in hypertension: A meta-analysis of beta-blocker trials. J. Am. Soc. Hypertens 2016, 10, 917–929. [Google Scholar] [CrossRef]
- Liao, I.C.; Chen, S.L.; Wang, M.Y.; Tsai, P.S. Effects of massage on blood pressure in patients with hypertension and prehy-pertension: A meta-analysis of randomized controlled trials. J. Cardiovasc. Nurs. 2016, 31, 73–83. [Google Scholar] [CrossRef] [PubMed]
- Berkley, K.J.; Hubscher, C.H. Are there separate central nervous system pathways for touch and pain? Nat. Med. 1995, 1, 766–773. [Google Scholar] [CrossRef] [PubMed]
- McGlone, F.; Valbo, A.B.; Olausson, H.; Loken, L.; Wessberg, J. Discriminative touch and emotional touch. Can. J. Exp. Psychol. 2007, 61, 173–183. [Google Scholar] [CrossRef]
- Preusser, S.; Thiel, S.D.; Rook, C.; Roggenhofer, E.; Kosatschek, A.; Draganski, B.; Blankenburg, F.; Driver, J.; Villringer, A.; Pleger, B. The perception of touch and the ventral somatosensory pathway. Brain 2015, 138, 540–548. [Google Scholar] [CrossRef]
- Queiroz, A.C.C.; Rezk, C.C.; Teixeira, L.; Tinucci, T.; Mion, D.; Forjaz, C.L.M. Gender influence on post-resistance exercise hypotension and hemodynamics. Int. J. Sports Med. 2013, 34, 939–944. [Google Scholar] [CrossRef] [PubMed]
| Resting Blood Pressure (mmHg) | Upper CM | Manual Massage | SHAM | Control |
|---|---|---|---|---|
| Systolic Blood Pressure | 105 | 110 | 109 | 107 |
| Diastolic Blood Pressure | 70 | 68 | 75 | 70 |
| Dominant Limb | Age (Years) | Body Mass (kg) | Height (m) | BMI (kg/m2) | Physical Activity Level (min) | |
|---|---|---|---|---|---|---|
| n = 15 | R = 13; L = 2 | 21 (9) | 57.30 (11.90) | 1.65 (0.07) | 21.99 (3.34) | 290 (710) |
| Diastolic Blood Pressure mmHg_lf | 0.39 | 0.945 |
| HF POWER ms2_lf | 0.88 | 0.483 |
| LF POWER ms2_lf | 0.48 | 0.869 |
| LF-HF RATIO _lf | 1.20 | 0.335 |
| LN (RMSSD) ms_lf | 0.32 | 0.921 |
| Mean R-R ms_lf | 1.06 | 0.415 |
| PNN50%_lf | 0.47 | 0.856 |
| RMSSD ms_lf | 0.28 | 0.954 |
| SDNN ms_lf | 0.55 | 0.788 |
| Systolic Blood Pressure mmHg_lf | 0.39 | 0.946 |
| TOTAL POWER ms2_lf | 0.79 | 0.573 |
| Systolic Blood Pressure | |||||||
|---|---|---|---|---|---|---|---|
| Protocol | Baseline | Post-0 | Post-15 min | Post-30 min | Post-45 min | Post-60 min | Within Condition |
| Control | 107 (13) | 108 (14) | 106 (10) | 105 (12) | 107 (11) | 109 (11) | 0.539 |
| ES (r) (classification) | 0.08 (no effect) | 0.18 (small) | 0.16 (small) | 0.21 (small) | 0.10 (small) | ||
| Sham | 109 (11) | 109 (9) | 107 (9) | 108 (10) | 107 (13) | 107 (9) | 0.504 |
| ES (r) (classification) | 0.06 (no effect) | 0.25 (small) | 0.13 (small) | 0.14 (small) | 0.19 (small) | ||
| CM | 105 (14) | 106 (11) | 112 (12) | 111 (8) | 108 (12) | 108 (15) | 0.160 |
| ES (r) (classification) | 0.16 (small) | 0.21 (small) | 0.14 (small) | 0.11 (small) | 0.01 (no effect) | ||
| MM | 110 (10) | 108 (9) | 109 (14) | 108 (7) | 108 (8) | 108 (6) | 0.221 |
| ES (r) (classification) | 0.21 (small) | 0.04 (no effect) | 0.22 (small) | 0.15 (small) | 0.22 (small) | ||
| Diastolic Blood Pressure | |||||||
|---|---|---|---|---|---|---|---|
| Protocol | Baseline | Post-0 | Post-15 min | Post-30 min | Post-45 min | Post-60 min | Within Condition |
| Control | 70 (12) | 71 (7) | 70 (8) | 72 (12) | 74 (10) * | 76 (6) | 0.000 * |
| ES (r) (classification) | 0.08 (no effect) | 0.13 (small) | 0.06 (no effect) | 0.66 (large) | 0.49 (medium) | ||
| Sham | 75 (11) | 71 (17) | 73 (9) | 73 (7) | 74 (11) | 76 (9) | 0.068 |
| ES (r) (classification) | 0.28 (small) | 0.19 (small) | 0.02 (no effect) | 0.03 (no effect) | 0.17 (small) | ||
| CM | 70 (7) | 71 (7) | 72 (6) | 71 (8) | 70 (9) | 71 (8) | 0.238 |
| ES (r) (classification) | 0.12 (small) | 0.36 (medium) | 0.24 (small) | 0.14 (small) | 0.25 (small) | ||
| MM | 68 (8) | 71 (7) | 73 (8) | 72 (6) | 71 (5) | 72 (6) | 0.225 |
| ES (r) (classification) | 0.26 (small) | 0.40 (medium) | 0.32 (medium) | 0.20 (small) | 0.26 (small) | ||
| RMSSDms | |||||||
|---|---|---|---|---|---|---|---|
| Baseline | Post-0 min | Post-15 min | Post-30 min | Post-45 min | Post-60 min | Within Condition | |
| Control | 40.05 (43.5) | 63.39 (48.23) | 61.52 (26.37) | 49.30 (24.58) | 63.49 (36.73) | 52.23 (35.94) | 0.008 * |
| ES (r) (classification) | 0.56 (large) * | 0.57 (large) * | 0.16 (small) | 0.39 (medium) | 0.28 (small) | ||
| Sham | 41.88 (42.51) | 79.44 (55.99) | 71.10 (23.02) | 60.53 (39.03) | 75.76 (46.31) | 54.08 (33.68) | 0.007 * |
| ES (r) (classification) | 0.51 (large) | 0.60 (large) * | 0.39 (medium) | 0.49 (medium) | 0.17 (small) | ||
| CM | 32.86 (18.58) | 59.37 (49.07) | 56.91 (34.55) | 49.91 (45.99) | 48.71 (52.16) | 58.04 (52.27) | 0.008 * |
| ES (r) (classification) | 0.51 (large) | 0.60 (large) * | 0.39 (medium) | 0.49 (medium) | 0.17 (small) * | ||
| MM | 38.05 (33.86) | 57.11 (40.27) | 52.61 (30.84) | 64.02 (33.74) | 52.63 (31.04) | 56.78 (32.42) | 0.159 |
| ES (r) (classification) | 0.47 (medium) | 0.29 (small) | 0.32 (medium) | 0.31 (medium) | 0.31 (medium) | ||
| SDNNms | |||||||
| Control | 52.84 (35.68) | 73.50 (57.76) | 79.16 (29.03) | 78.12 (29.79) | 78.85 (25.45) | 79.01 (23.18) | 0.036 * |
| ES (r) (classification) | 0.23 (small) | 0.42 (medium) | 0.42 (medium) | 0.55 (large) * | 0.44 (medium) | ||
| Sham | 62.08 (40.69) | 74.55 (32.98) | 77.42 (27.26) | 79.53 (2348) | 81.55 (25.88) | 71.88 (36.25) | 0.260 |
| ES (r) (classification) | 0.21 (small) | 0.30 (medium) | 0.37 (medium) | 0.28 (small) | 0.34 (medium) | ||
| CM | 47.19 (27.95) | 62.64 (34.83) | 86.43 (27.46) | 76.26 (31.27) | 93.21 (26.07) | 79.01 (45.66) | 0.008 * |
| ES (r) (classification) | 0.24 (small) | 0.46 (medium) | 0.39 (medium) | 0.60 (large) * | 0.58 (large) * | ||
| MM | 54.03 (30.39) | 67.39 (19.49) | 69.79 (26.40) | 78.49 (29.63) | 71.23 (32.15) | 79.01 (29.03) | 0.027 * |
| ES (r) (classification) | 0.23 (small) | 0.30 (medium) | 0.37 (medium) | 0.48 (medium) | 0.58 (large) | ||
| pNN50% | |||||||
| Control | 14.00 (37) | 46.00 (41) | 33.00 (32) | 30.00 (33) | 37.00 (38) | 28.00 (30) | 0.034 * |
| ES (r) (classification) | 0.52 (large) | 0.42 (medium) | 0.10 (small) | 0.27 (small) | 0.16 (small) | ||
| Sham | 24.00 (38) | 54.00 (47) | 47.00 (25) | 40.00 (24) | 46.00 (27) | 40.00 (38) | 0.019 * |
| ES (r) (classification) | 0.53 (large) | 0.51 (large) | 0.41 (medium) | 0.46 (medium) | 0.20 (small) | ||
| CM | 9.00 (24) | 41.00 (39) | 32.00 (30) | 30.00 (32) | 29.00 (36) | 35.00 (32) | 0.013 * |
| ES (r) (classification) | 0.54 (large) * | 0.54 (large) * | 0.39 (medium) | 0.44 (medium) | 0.58 (large) * | ||
| MM | 17.00 (40) | 34.00 (41) | 32.00 (43) | 31.00 (32) | 34.00 (29) | 32.00 (27) | 0.040 * |
| ES (r) (classification) | 0.32 (medium) | 0.50 (large) | 0.49 (medium) | 0.43 (medium) | 0.43 (medium) | ||
| LN (RMSSD) (ms) | |||||||
| Control | 3.69 (0.93) | 4.25 (0.82) | 4.12 (0.52) | 3.90 (0.47) | 4.15 (0.63) | 3.96 (0.64) | 0.020 * |
| ES (r) (classification) | 0.57 (large) * | 0.49 (medium) | 0.16 (small) | 0.35 (medium) | 0.28 (small) | ||
| Sham | 3.73 (0.91) | 4.37 (0.88) | 4.26 (0.31) | 4.10 (0.58) | 4.33 (0.72) | 3.99 (0.65) | 0.006 * |
| ES (r) (classification) | 0.51 (large) | 0.61 (large) * | 0.40 (medium) | 0.49 (medium) | 0.16 (small) | ||
| CM | 3.49 (0.54) | 4.08 (0.78) | 4.04 (0.52) | 3.91 (0.82) | 3.89 (0.90) | 4.06 (0.85) | 0.008 * |
| ES (r) (classification) | 0.53 (large) | 0.57 (large) * | 0.49 (medium) | 0.49 (medium) | 0.62 (large) * | ||
| MM | 3.64 (0.80) | 4.04 (0.70) | 3.96 (0.57) | 4.16 (0.64) | 3.96 (0.54) | 4.04 (0.57) | 0.139 |
| ES (r) (classification) | 0.48 (medium) | 0.35 (medium) | 0.35 (medium) | 0.34 (medium) | 0.35 (medium) | ||
| MEAN iR-R (ms) | |||||||
| Control | 760.27 (93.89) | 832.38 (141.16) | 864.56 (105.99) | 844.58 (64.55) | 875.01 (113.64) | 833.73 (187.20) | 0.002 * |
| ES (r) (classification) | 0.55 (large) * | 0.66 (large) * | 0.58 (large) * | 0.69 (large) * | 0.55 (large) * | ||
| Sham | 830.15 (198.40) | 919.70 (187.45) | 897.00 (229.02) | 866.99 (214.50) | 918.14 (179.70) | 833.73 (204.33) | 0.008 * |
| ES (r) (classification) | 0.57 (large) * | 0.62 (large) * | 0.44 (medium) | 0.48 (medium) | 0.28 (small) | ||
| CM | 764.71 (159.71) | 857.01 (112.75) | 859.38 (131.51) | 853.64 (76.45) | 846.67 (123.12) | 913.03 (133.61) | 0.003 * |
| ES (r) (classification) | 0.53 (large) | 0.60 (large) * | 0.58 (large) * | 0.55 (large) * | 0.66 (large) * | ||
| MM | 779.00 (87.89) | 838.71 (134.60) | 861.39 (116.44) | 829.93 (167.58) | 860.01 (128.53) | 866.62 (116.20) | 0.001 * |
| ES (r) (classification) | 0.26 (small) | 0.51 (large) | 0.41 (medium) | 0.73 (large) * | 0.58 (large) * | ||
| TOTAL POWER ms2 | |||||||
|---|---|---|---|---|---|---|---|
| Baseline | Post-0 min | Post-15 min | Post-30 min | Post-45 min | Post-60 min | Within Condition | |
| Control | 1346.67 (2004.78) | 2464.36 (4455.47) | 2471.27 (2486.22) | 3302.12 (2981.87) | 3039.01 (2798.19) | 3107.56 (2753.03) | 0.033 * |
| ES (r) (classification) | 0.42 (medium) | 0.35 (medium) | 0.23 (small) | 0.57 (large) * | 0.17 (small) | ||
| Sham | 1968.19 (2919.92) | 2381.00 (3796.07) | 3111.46 (1751.67) | 3021.98 (1302.74) | 3334.23 (5174.11) | 2605.74 (2370.88) | 0.497 |
| ES (r) (classification) | 0.34 (medium) | 0.33 (medium) | 0.31 (medium) | 0.31 (medium) | 0.22 (small) | ||
| CM | 944.18 (704.78) | 2464.36 (3450.03) | 2439.50 (1410.69) | 3021.98 (3887.12) | 2381.87 (4353.62) | 3242.34 (5241.07) | 0.001 * |
| ES (r) (classification) | 0.27 (small) | 0.31 (medium) | 0.55 (large) * | 0.51 (large) | 0.74 (large) * | ||
| MM | 1844.65 (1933.13) | 2160.07 (3516.33) | 2339.49 (2221.31) | 3236.94 (3368.09) | 2320.10 (2588.11) | 3087.02 (1161.28) | 0.049 * |
| ES (r) (classification) | 0.07 (small) | 0.21 (small) | 0.42 (medium) | 0.39 (medium) | 0.44 (medium) | ||
| LF POWER ms2 | |||||||
| Control | 650.67 (1237.53) | 1467.53 (2658.45) | 1540.16 (1464.43) | 1539.34 (1543.21) | 1795.87 (1438.67) | 1900.21 (1514.26) | 0.115 |
| ES (r) (classification) | 0.27 (small) | 0.37 (medium) | 0.31 (medium) | 0.38 (medium) | 0.29 (small) | ||
| Sham | 927.42 (1570.22) | 1081.43 (1200.03) | 1540.16 (653.86) | 1554.75 (1032.19) | 1795.87 (1428.13) | 1282.71 (1741.09) | 0.529 |
| ES (r) (classification) | 0.08 (no effect) | 0.22 (small) | 0.17 (small) | 0.29 (small) | 0.30 (medium) | ||
| CM | 544.98 (281.41) | 1050.85 (2108.26) | 1402.23 (834.30) | 1359.34 (1595.44) | 1896.11 (1917.92) | 2027.90 (3582.68) | 0.001 * |
| ES (r) (classification) | 0.10 (small) | 0.35 (medium) | 0.41 (medium) | 0.49 (medium) | 0.71 (large) * | ||
| MM | 677.05 (1051.34) | 800.48 (648.48) | 1415.73 (1146.53) | 1359.34 (1230.96) | 1479.18 (594.68) | 1632.17 (965.79) | 0.115 |
| ES (r) (classification) | 0.01 (no effect) | 0.14 (small) | 0.14 (small) | 0.20 (small) | 0.25 (small) | ||
| HF POWER ms2 | |||||||
| Control | 693.30 (782.99) | 1907.67 (2228.37) | 1201.11 (2288.40) | 1174.41 (1585.22) | 1734.03 (1695.55) | 784.84 (1655.61) | 0.091 |
| ES (r) (classification) | 0.31 (medium) | 0.21 (small) | 0.14 (small) | 0.21 (small) | 0.05 (no effect) | ||
| Sham | 971.18 (1469.83) | 1152.90 (2539.24) | 1792.10 (1614.62) | 1734.03 (885.14) | 1734.03 (2310.83) | 1026.63 (1422.45) | 0.15 |
| ES (r) (classification) | 0.37 (medium) | 0.53 (large) | 0.40 (medium) | 0.47 (medium) | 0.08 (no effect) | ||
| CM | 381.95 (530.48) | 1311.49 (1728.06) | 1247.38 (977.78) | 843.58 (1808.54) | 679.32 (2591.78) | 1271.04 (2771.01) | 0.073 |
| ES (r) (classification) | 0.48 (medium) | 0.36 (medium) | 0.38 (medium) | 0.29 (small) | 0.41 (medium) | ||
| MM | 778.91 (1426.57) | 1331.16 (2020.04) | 1345.73 (675.12) | 1726.65 (1992.47) | 1109.43 (2271.16) | 1271.04 (1486.11) | 0.130 |
| ES (r) (classification) | 0.41 (medium) | 0.24 (small) | 0.32 (medium) | 0.22 (small) | 0.23 (small) | ||
| LF/HF RATIO | |||||||
| Control | 0.98 (0.83) | 1.00 (0.37) | 1.28 (1.29) | 1.14 (1.93) | 1.10 (2.22) | 1.87 (2.74) | 0.111 |
| ES (r) (classification) | 0.04 (no effect) | 0.12 (small) | 0.28 (small) | 0.18 (small) | 0.42 (medium) | ||
| Sham | 1.19 (1.09) | 0.82 (0.76) | 0.89 (0.76) | 0.93 (0.53) | 0.86 (0.81) | 1.87 (2.01) | 0.149 |
| ES (r) (classification) | 0.23 (small) | 0.35 (medium) | 0.36 (medium) | 0.13 (small) | 0.17 (small) | ||
| CM | 1.34 (0.91) | 0.94 (1.18) | 1.05 (1.17) | 1.17 (1.08) | 1.23 (1.51) | 1.12 (1.87) | 0.98 |
| ES (r) (classification) | 0.27 (small) | 0.02 (no effect) | 0.05 (no effect) | 0.14 (small) | 0.17 (small) | ||
| MM | 1.38 (1.18) | 0.69 (0.67) | 0.78 (1.09) | 0.80 (0.55) | 0.94 (0.97) | 1.49 (2.14) | 0.022 * |
| ES (r) (classification) | 0.30 (medium) | 0.10 (small) | 0.01 (no effect) | 0.24 (small) | 0.55 (large) * | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monteiro, E.R.; Pescatello, L.S.; Garcia, G.H.; de Meirelles, A.G.; de Oliveira, F.; de Souza, R.C.; Nogueira, L.A.C.; Lopes, A.J.; Moreira-Gonçalves, D. Upper Cervical Manipulation and Manual Massage Do Not Modulate Sympatho-Vagal Balance or Blood Pressure in Women: A Randomized, Placebo-Controlled Clinical Trial. Healthcare 2025, 13, 2554. https://doi.org/10.3390/healthcare13202554
Monteiro ER, Pescatello LS, Garcia GH, de Meirelles AG, de Oliveira F, de Souza RC, Nogueira LAC, Lopes AJ, Moreira-Gonçalves D. Upper Cervical Manipulation and Manual Massage Do Not Modulate Sympatho-Vagal Balance or Blood Pressure in Women: A Randomized, Placebo-Controlled Clinical Trial. Healthcare. 2025; 13(20):2554. https://doi.org/10.3390/healthcare13202554
Chicago/Turabian StyleMonteiro, Estêvão Rios, Linda S. Pescatello, Gustavo Henrique Garcia, Alexandre Gonçalves de Meirelles, Francine de Oliveira, Rafael Cotta de Souza, Leandro Alberto Calazans Nogueira, Agnaldo José Lopes, and Daniel Moreira-Gonçalves. 2025. "Upper Cervical Manipulation and Manual Massage Do Not Modulate Sympatho-Vagal Balance or Blood Pressure in Women: A Randomized, Placebo-Controlled Clinical Trial" Healthcare 13, no. 20: 2554. https://doi.org/10.3390/healthcare13202554
APA StyleMonteiro, E. R., Pescatello, L. S., Garcia, G. H., de Meirelles, A. G., de Oliveira, F., de Souza, R. C., Nogueira, L. A. C., Lopes, A. J., & Moreira-Gonçalves, D. (2025). Upper Cervical Manipulation and Manual Massage Do Not Modulate Sympatho-Vagal Balance or Blood Pressure in Women: A Randomized, Placebo-Controlled Clinical Trial. Healthcare, 13(20), 2554. https://doi.org/10.3390/healthcare13202554








