Thoracic Manual Therapy With or Without Exercise Improves Pain and Disability in Subacromial Pain Syndrome: A Systematic Review of Randomized Trials
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Eligibility Criteria
- -
- Population. Adults with a clinical diagnosis of SPS.
- -
- Interventions. Thoracic-directed care: manual therapy with or without exercise applied to the thoracic spine, delivered either as a stand-alone intervention or as an adjunct to standard non-pharmacological conservative care.
- -
- Comparators. Sham procedures, no treatment/usual care, or the same standard conservative care without the thoracic component.
- -
- Outcomes. Primary: pain and shoulder-related disability. Secondary: shoulder range of motion (ROM), health-related quality of life (QoL), and patient satisfaction (Global Rating of Change, GROC).
- -
- Study design. RCTs.
- -
- Filters. Language and timeframe: English or Spanish; January 2015 to April 2025.
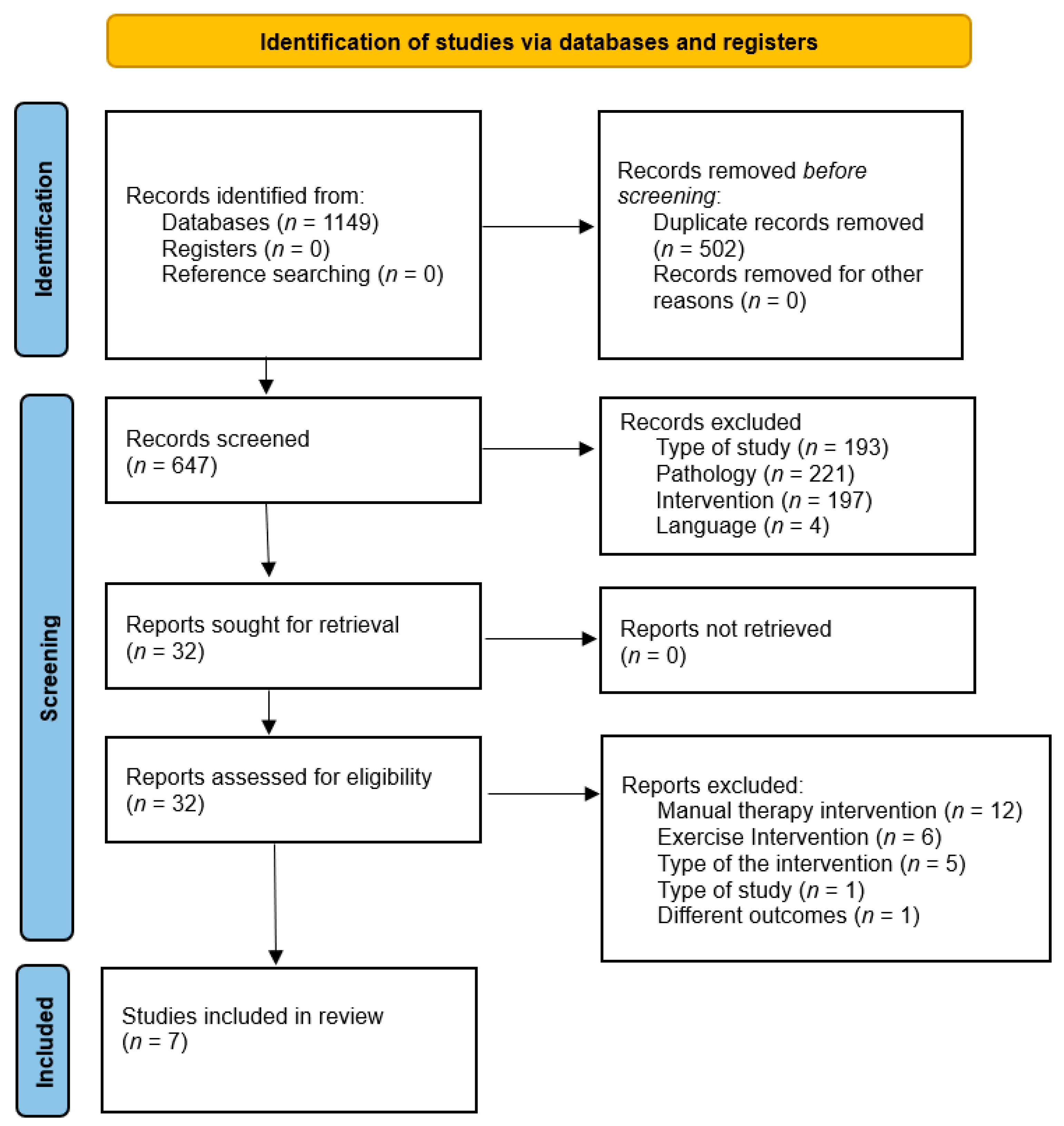
2.4. Study Selection
2.5. Data Extraction
2.6. Methodological Quality Assessment
3. Results
3.1. Characteristics of the Included Studies
3.2. Methodological Quality
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AHD | acromiohumeral distance |
| DASH | Disabilities of the Arm, Shoulder and Hand |
| EMG | electromyography |
| GROC | Global Rating of Change |
| HHD | handheld dynamometry |
| HVLA | high-velocity low-amplitude |
| MCID | minimal clinically important difference |
| MeSH | Medical Subject Headings |
| NPRS | Numeric Pain Rating Scale |
| PEDro | Physiotherapy Evidence Database scale |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
| QoL | quality of life |
| RCT | randomized controlled trial |
| ROM | range of motion |
| SNAGs | sustained natural apophyseal glides |
| SPADI | Shoulder Pain and Disability Index |
| SPS | Subacromial Pain Syndrome |
| TSM | thoracic spine manipulation |
| TSTM | thoracic spine thrust manipulation |
| VAS | Visual Analogue Scale |
| WoS | Web of Science |
| WORC | Western Ontario Rotator Cuff Index |
Appendix A. Detailed Search Strategy According to PRISMA and Model Search Terms
Appendix A.1. Search Terms
| Population | Intervention | Results | Type of Study |
| Shoulder Impingement Syndrome (MeSH) | Exercise Movement Techniques (MeSH) | Pain Measurement (MeSH) | Randomized Controlled Trial (MeSH) |
| Rotator Cuff (MeSH) | Exercise Therapy (MeSH) | Pain (MeSH) | Randomized Clinical Trial |
| Rotator Cuff Tendinopathy | Thoracic Spine Mobilization | Disability Evaluation (MeSH) | |
| Subacromial Shoulder Pain | Exercise Therapy | Pain Intensity | |
| Thoracic Manual Therapy | Symptom | ||
| Therapeutic Exercise | Disability |
Appendix A.2. Search Strategy
Appendix A.2.1. PUBMED
Appendix A.2.2. PEDro
Appendix A.2.3. Cochrane Library
Appendix A.2.4. Web of Science
Appendix B. Detailed Techniques
| Author (Year) | Intervention | Technique Details | Control Group |
| Thoracic manual therapy in isolation | |||
| Haik et al. (2017) [26] | Thoracic manipulation | Middle thoracic spine, patient seated with arms crossed over chest. The therapist was located behind the patient and performed a thrust technique with arms and chest around the thoracic region of the subject. Sham: Same position without performing thrust. The technique was applied twice in a period of 3 to 4 days apart. Sham technique was previously reported as a believable active treatment. | Sham manipulation |
| Grimes et al. (2019) A [29] | Thoracic manipulation | One of the three interventions was delivered between the levels of C7 and T4, and was performed two times on each participant based on methods used in previous studies. For the supine TSTM, examiner used his body to push down through the participant’s upper arms to provide a high-velocity, low-amplitude thrust in the anterior-to-posterior direction. Sham: Seated manipulation moving the participant through the same motion but delivering no manipulative thrust. This sham technique has been previously validated as a plausible treatment. | Sham manipulation |
| Grimes et al. (2019) B [29] | Thoracic manipulation | One of the three interventions was delivered between the levels of C7 and T4, and was performed two times on each participant based on methods used in previous studies. For the seated TSTM, examiner applied a high-velocity, low-amplitude distraction thrust in a cephalad direction Sham: Same seated sham manipulation | Sham manipulation |
| Hunter et al. (2022) A [27] | Muscle Energy Tecnhique (MET) | MET consisted of the application of lateral force to the spinous process of the thoracic vertebra until initial resistance with the vertebra below was noted. | MET |
| Hunter et al. (2022) B [27] | MET + Soft tissue massage (STM) | Same MET technique. STM was applied to the rotator cuff (subscapularis, infraspinatus, and teres minor) and the triceps muscle of the affected shoulder. The STM techniques included static compression and deep longitudinal stripping to the aforementioned muscles, with active engagement. | Placebo laser |
| Thoracic manual therapy combined with exercise | |||
| Haider et al. (2018) [30] | Non-thrust + 3 thrust manipulations | In thoracic group, thoracic manipulative therapy included one non-thrust mobilization and three different thrust manipulation techniques directed at thoracic spine and exercise therapy including hot or cold pack, mobility exercises (flexion and extension exercises with arms in front of the wall, shoulder flexion 90°, and exercises with shoulder circles) and strengthening exercises (resistance exercise with elbow flexion 90° and an elastic band, shoulder flexion with elbow extension holding bar (1–4 kg), body lift from a seated position with elbows extended, and resistance exercises for external rotation. In group 2, patients received conservative exercise therapy including hot or cold pack, mobility exercises and strengthening exercises. | Shoulder exercises |
| Park et al. (2020) A [28] | Thoracic mobilization | Thoracic spine joint mobilization consisted of oscillatory techniques performed in the prone position, with 30 repetitions per set, four sets in total, and a 1-min rest between sets. Central posterior–anterior mobilization was applied using a grade III large-amplitude rhythmic oscillation, targeting the joint sign segment (the most painful or stiffest level) identified through Maitland’s passive accessory intervertebral motion test. When a joint sign was not present, mobilization was applied at T6–T7. The mobilization session lasted 15 min. The exercise program aimed to enhance thoracic spine extension, trunk extensor strength, and trunk flexor flexibility. It included foam roll stretches as a warm-up, marching on a roller (2 sets of 10 repetitions), thoracic extension against a wall using bodyweight (2 sets of 10 repetitions), and a standing neck/chest stretch as a cool-down. Each exercise session lasted 15 min. | Shoulder exercises |
| Park et al. (2020) B [28] | Thoracic Mobilization + Shoulder exercises | The combination group received an intervention consisting of joint mobilization and an exercise program. Joint mobilization involved central posterior–anterior oscillations performed in the prone position for 30 repetitions, with a 1-min rest between 2 sets. The exercise program included foam roll stretches (warm-up), marching on a roller (1 set of 10 repetitions), thoracic extension against a wall using bodyweight (1 set of 10 repetitions), and a standing neck/chest stretch (cool-down). The total duration of the combined therapy was 15 min, equally divided between joint mobilization (7 min 30 s) and exercise (7 min 30 s). | Shoulder exercises |
| Abu El Kassem et al. (2024) [13] | SNAGs + Shoulder Exercises | SNAGs technique on the thoracic spine. The patient sat at the far end of the table, hands behind his neck, protracting the scapulae, and providing the therapist’s hand accessibility to the mid-thoracic spine. The therapist did stand on their most effective side for a centrally administered SNAG. Firstly, a restricted segment of the thoracic spine was detected. The therapist performed passive extension of the thoracic spine and at the same time made palpation of the thoracic spinous process to detect the restricted segment of the thoracic spine. The therapist’s mobilizing hand (ulnar border) was used to apply a cephalad glide in line with the facet joint plane of the involved spinal level, while the other arm held the thoracic wall above the level to be mobilized. The patient was then asked to perform thoracic extension while gliding was applied to the restricted thoracic segment to the end of the range. Traction was administered before glide, which was accomplished via the therapist’s knee extension. The technique was repeated for 6 to 10 times for 3–5 sets with rest in between. Shoulder exercises included pendulum exercises, shoulder range of motion exercises, stretching exercises, strengthening exercises and scapular stabilization exercises. | Shoulder Exercises |
| Michener et al. (2024) [11] | Thoracic + scapular manual therapy + Shoulder exercises | Manual therapy combined both thrust manipulation and non-thrust mobilization. The manual therapy techniques were aimed at three areas. Clinicians were instructed to apply manual techniques for a total duration of 10–15 min, ensuring the use of at least one technique in each of the following regions: thoracic spine, posterior shoulder, and glenohumeral joint. Practitioners could select low-grade techniques for those with moderate to high irritability, whereas high-grade techniques could be used for those with low irritability. Thoracic techniques were thoracic PA glides in prone, thoracic PA glides seated, thoracic thrust in prone (max 2 reps), thoracic thrust in supine (max 2 reps) and distraction thrust (max 2 reps). Shoulder exercises combined progressive resistance exercise with stretching. The program consisted of resistance exercises using body weight or exercise bands to target the shoulder muscles with particular emphasis on the scapular stabilizers and rotator cuff, complemented with flexibility exercises and postural training through chin tucks and scapular retraction. Strengthening exercises were performed using latex-free Thera-Bands, with 2 to 3 sets of 10 repetitions. | Shoulder exercises |
References
- Commissioning Guide: Subacromial Shoulder Pain. London. 2014. Available online: https://bess.ac.uk/wp-content/uploads/2020/06/Subacromial-Shoulder-Commissioning-Guide_final1.pdf (accessed on 17 March 2025).
- Van der Windt, D.A.W.M.; Koes, B.W.; de Jong, B.A.; Bouter, L.M. Shoulder disorders in general practice: Incidence, patient characteristics, and management. Ann. Rheum. Dis. 1995, 54, 959–964. [Google Scholar] [CrossRef]
- Struyf, F.; Nijs, J.; Mollekens, S.; Jeurissen, I.; Truijen, S.; Mottram, S.; Meeusen, R. Scapular-focused treatment in patients with shoulder impingement syndrome: A randomized clinical trial. Clin. Rheumatol. 2013, 32, 73–85. [Google Scholar] [CrossRef]
- Stewart, S.G.; Jull, G.A.; Ng, J.K.F.; Willems, J.M. An initial analysis of thoracic spine movement during unilateral arm elevation. J. Man. Manip. Ther. 1995, 3, 15–20. [Google Scholar] [CrossRef]
- Yu, S.; Chen, S.; Yang, Z.; Ma, X.; Huang, J.; Yang, L. The effectiveness of thoracic spine manual therapy in treating subacromial impingement syndrome: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2025; in press. [Google Scholar] [CrossRef]
- Ludewig, P.M.; Reynolds, J.F. The association of scapular kinematics and glenohumeral joint pathologies. J. Orthop. Sports Phys. Ther. 2009, 39, 90–104. [Google Scholar] [CrossRef] [PubMed]
- Phadke, V.; Camargo, P.R.; Ludewig, P.M. Scapular and rotator cuff muscle activity during arm elevation: A review. Braz. J. Phys. Ther. 2009, 13, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Sharma, S.; Sharma, R.K.; Jain, A. Exercise therapy plus manual therapy improves acromiohumeral distance in overhead athletes with shoulder impingement syndrome. Adv. Rehabil. 2022, 36, 1–10. [Google Scholar]
- Sharma, S.; Hussain, M.E.; Sharma, S. Effects of exercise therapy plus manual therapy on muscle activity, latency timing and SPADI in shoulder impingement syndrome. Complement. Ther. Clin. Pract. 2021, 44, 101390. [Google Scholar] [CrossRef]
- Dunning, J.; Butts, R.; Fernández-de-las-Peñas, C.; Walsh, S.; Goult, C.; Gillett, B.; Arias-Buría, J.L.; Garcia, J.; Young, I.A. Spinal manipulation and electrical dry needling in patients with SIS: A multicenter randomized clinical trial. J. Orthop. Sports Phys. Ther. 2021, 51, 72–81. [Google Scholar] [CrossRef]
- Michener, L.A.; McClure, P.W.; Tate, A.R.; Bailey, L.B.; Seitz, A.L.; Straub, R.K.; Thigpen, C.A. Adding manual therapy to an exercise program improves long-term outcomes over exercise alone in subacromial shoulder pain: A randomized clinical trial. JOSPT Open 2024, 2, 29–48. [Google Scholar] [CrossRef]
- Peek, A.L.; Miller, C.; Heneghan, N.R. Thoracic manual therapy in the management of non-specific shoulder pain: A systematic review. J. Man. Manip. Ther. 2015, 23, 176–187. [Google Scholar] [CrossRef]
- Abu El Kasem, S.T.; Alaa, F.A.A.; Abd El-Raoof, N.A.; Abd-Elazeim, A.S. Efficacy of Mulligan thoracic sustained natural apophyseal glides in subacromial pain: A single-blinded randomized controlled trial. J. Man. Manip. Ther. 2024, 32, 584–593. [Google Scholar] [CrossRef]
- Edmondston, S.; Ferguson, A.; Ippersiel, P.; Ronningen, L.; Sodeland, S.; Barclay, L. Clinical and radiological inves-tigation of thoracic spine extension motion during bilateral arm elevation. J. Orthop. Sports Phys. Ther. 2012, 42, 861–869. [Google Scholar] [CrossRef]
- Greendale, G.A.; Nili, N.S.; Huang, M.H.; Seeger, L.; Karlamangla, A.S. Reliability and validity of three non-radiological measures of thoracic kyphosis vs the standing radiological Cobb angle. Osteoporos. Int. 2011, 22, 1897–1905. [Google Scholar] [CrossRef]
- Yamamoto, A.; Takagishi, K.; Kobayashi, T.; Shitara, H.; Ichinose, T.; Takasawa, E.; Shimoyama, D.; Osawa, T. The Impact of faulty posture on rotator cuff tears with and without symptoms. J. Shoulder Elb. Surg. 2015, 24, 446–452. [Google Scholar] [CrossRef]
- Belón-Pérez, P.; Cuesta-Vargas, A.I. Immediate effects of thoracic spine manipulation upon shoulder functionality after sutured rotator cuff repair: A prospective study. J. Manip. Physiol. Ther. 2018, 41, 589–595. [Google Scholar] [CrossRef]
- Mintken, P.E.; McDevitt, A.W.; Cleland, J.A.; Boyles, R.E.; Beardslee, A.R.; Burns, S.A.; Haberl, M.D.; Hinrichs, L.A.; Michener, L.A. Cervicothoracic manual therapy plus exercise therapy versus exercise therapy alone in shoulder pain: A multicenter randomized controlled trial. J. Orthop. Sports Phys. Ther. 2016, 46, 617–628. [Google Scholar] [CrossRef] [PubMed]
- Lucas, J.; van Doorn, P.; Hegedus, E.; Lewis, J.; van der Windt, D. Global prevalence and incidence of shoulder pain: A systematic review. BMC Musculoskelet. Disord. 2022, 23, 1073. [Google Scholar] [CrossRef] [PubMed]
- Desmeules, F.; Roy, J.S.; Lafrance, S.; Charron, M.; Dubé, M.O.; Dupuis, F.; Beneciuk, J.M.; Grimes, J.; Kim, H.M.; Lamontagne, M.; et al. Rotator cuff tendinopathy diagnosis, nonsurgical medical care, and rehabilitation: A clinical practice guideline. J. Orthop. Sports Phys. Ther. 2025, 55, 235–274. [Google Scholar] [CrossRef]
- Dzakpasu, F.Q.S.; Carver, A.; Brakenridge, C.J.; Cicuttini, F.; Urquhart, D.M.; Owen, N.; Dunstan, D.W. Musculoskeletal pain and sedentary behaviour: A systematic review with meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2021, 18, 159. [Google Scholar] [CrossRef] [PubMed]
- Gebremariam, L.; Hay, E.M.; van der Sande, R.; Rinkel, W.D.; Koes, B.W.; Huisstede, B.M.A. Subacromial impingement syndrome—Effectiveness of physiotherapy and manual therapy. Br. J. Sports Med. 2014, 48, 1202–1208. [Google Scholar] [CrossRef]
- Sheikhzadeh, A.; Wertli, M.M.; Weiner, S.S.; Rasmussen-Barr, E.; Weiser, S. Do psychological factors affect outcomes in musculoskeletal shoulder disorders? A systematic review. BMC Musculoskelet. Disord. 2021, 22, 560. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Cashin, A.G.; McAuley, J.H. Clinimetrics: Physiotherapy Evidence Database (PEDro) scale. J. Physiother. 2020, 66, 59. [Google Scholar] [CrossRef] [PubMed]
- Haik, M.N.; Alburquerque-Sendín, F.; Camargo, P.R. Short-term effects of thoracic spine manipulation on shoulder impingement syndrome: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2017, 98, 1594–1605. [Google Scholar] [CrossRef] [PubMed]
- Hunter, D.J.; Rivett, D.A.; McKiernan, S.; Luton, R.; Snodgrass, S.J. Thoracic manual therapy improves pain and disability vs placebo in SIS: Randomized controlled trial with 1-year follow-up. Arch. Phys. Med. Rehabil. 2022, 103, 1533–1543. [Google Scholar] [CrossRef] [PubMed]
- Park, S.J.; Kim, S.H.; Kim, S.H. Effects of thoracic mobilization and extension exercise on thoracic alignment and shoulder function in SIS: Randomized controlled pilot study. Healthcare 2020, 8, 316. [Google Scholar] [CrossRef] [PubMed]
- Grimes, J.K.; Puentedura, E.J.; Cheng, M.S.; Seitz, A.L. Comparative effects of upper thoracic spine thrust manipulation techniques in SIS: Randomized clinical trial. J. Orthop. Sports Phys. Ther. 2019, 49, 716–724. [Google Scholar] [CrossRef]
- Haider, R.; Bashir, M.S.; Adeel, M.; Ijaz, M.J. Ayub, A. Comparison of conservative exercise therapy with and without Maitland thoracic manipulation in subacromial pain: Clinical trial. J. Pak. Med. Assoc. 2018, 68, 381–387. [Google Scholar]
- Vicente, J.; Wooley, R. Addition of thoracic spine manipulation or mobilization to exercise in adults with SIS: A critically appraised topic. J. Sport Rehabil. 2025, 34, 677–681. [Google Scholar] [CrossRef]
- Mohamed, S.P.; Alatawi, S. Comparison of Kinesio taping and manual therapy with supervised exercise for SIS. Int. J. Physiother. 2019, 6, 177–185. [Google Scholar] [CrossRef]
- Moradi, M.; Shadmehr, A.; Fischer, T.; Moghaddam, B.A.; Ebrahimzade, M.H.; Jalaei, S. Fascial distortion model vs joint mobilization in SIS: Randomized clinical trial. J. Bodyw. Mov. Ther. 2023, 36, 410–416. [Google Scholar] [CrossRef] [PubMed]
- Azin, Z.; Kamali, F.; Salehi Dehno, N.; Abolahrari-Shirazi, S. Manual therapy technique vs therapeutic exercise in SIS: Randomized clinical trial. J. Manip. Physiol. Ther. 2023, 46, 98–108. [Google Scholar] [CrossRef] [PubMed]
- World Congress on Osteoporosis. Osteoarthritis and Musculoskeletal Diseases (WCO-IOF-ESCEO 2019): Posters Abstracts. Osteoporos Int. 2019, 30 (Suppl. 2), 253–773. [Google Scholar] [CrossRef]
- Ribeiro, D.C.; Jafarian Tangrood, Z.; Wilson, R.; Sole, G.; Abbott, J.H. Tailored exercise and manual therapy vs standardised exercise for subacromial pain: Feasibility randomized controlled trial (Otago MASTER). BMJ Open 2022, 12, e053572. [Google Scholar] [CrossRef]
- Subbiah, K.; Rajappa, S.; Subhashini, A.S.; Ganeshan, S. Functional ability and quality of life status following manual therapy and specific exercise conditioning in subacromial impingement syndrome: A randomised controlled study. J. Clin. Diagn. Res. 2023, 17, YC11–YC16. [Google Scholar] [CrossRef]
- Eliason, A.; Harringe, M.; Engström, B.; Werner, S. Guided exercises with or without joint mobilization or no treatment in patients with SIS: Clinical trial. J. Rehabil. Med. 2021, 53, 2765. [Google Scholar] [CrossRef]
- Land, H.; Gordon, S.; Watt, K. Effect of manual physiotherapy in homogeneous individuals with subacromial shoulder impingement: Randomized controlled trial. Physiother. Res. Int. 2019, 24, e1768. [Google Scholar] [CrossRef]
- Fidelis de Paula Gomes, C.A.; Dibai-Filho, A.V.; Moreira, W.A.; Rivas, S.Q.; Silva Edos, S.; Bogik Garrido, A.C. Effect of adding interferential current to exercise and manual therapy for unilateral SIS: Randomized clinical trial. J. Manip. Physiol. Ther. 2018, 41, 218–226. [Google Scholar] [CrossRef]
- Pekyavas, N.O.; Baltaci, G. Short-term effects of high-intensity laser therapy, manual therapy, and Kinesio taping in SIS. Lasers Med. Sci. 2016, 31, 1133–1141. [Google Scholar] [CrossRef]
- Kim, S.Y.; Dvir, Z.; Oh, J.S. Neurac technique vs manual therapy in acute SIS: Randomized single-blinded controlled trial. J. Back Musculoskelet. Rehabil. 2020, 33, 645–653. [Google Scholar] [CrossRef]
- Elnour, A.A.; Mohammed, M.M.; Fayaz, N.; Waly, A.H.; Al Hamaky, D.M.A. Effect of neuromuscular training on shoulder proprioception and isometric internal rotators muscle strength in patients with shoulder impingement syndrome: A double-blinded randomized controlled trial. J. Popul. Ther. Clin. Pharmacol. 2023, 30, E97–E109. [Google Scholar] [CrossRef]
- Camargo, P.R.; Alburquerque-Sendín, F.; Ávila, M.A.; Haik, M.N.; Vieira, A.; Salvini, T.F. Stretching and strengthening exercises, with and without manual therapy, on scapular kinematics, function, and pain in SIS: Randomized controlled trial. J. Orthop. Sports Phys. Ther. 2015, 45, 984–997. [Google Scholar] [CrossRef]
- Australian New Zealand Clinical Trials Registry ACTRN. Exercise Intervention for Subacromial Impingement Syndrome: Randomized Controlled Trial of Two Rehabilitation Protocols [Internet]. 2015. Available online: https://www.cochranelibrary.com/central/doi/10.1002/central/CN-02433439/full (accessed on 17 March 2025).
- Gutiérrez-Espinoza, H.; Araya-Quintanilla, F.; Zavala-González, J.; Gana-Hervias, G.; Martínez-Vizcaíno, V.; Álvarez-Bueno, C.; Cavero-Redondo, I. Rationale and methods of an RCT comparing specific exercise vs home exercises in SIS. Medicine 2019, 98, e16139. [Google Scholar]
- Basharat, A.; Ramzan, M.; Ali, S.; Qamar, M.M.; Javaid, M.; Ali, M. Exercise therapy mitigate symptoms of subacromial pain syndrome. Rawal. Med. J. 2023, 48, 415–417. [Google Scholar]
- Alfredo, P.P.; Bjordal, J.M.; Steagall Junior, W.; Marques, A.P.; Casarotto, R.A. Efficacy of low-level laser therapy combined with exercise for SIS: Randomized controlled trial. Clin. Rehabil. 2021, 35, 851–860. [Google Scholar] [CrossRef]
- Schenk, R.; Donaldson, M.; Parent-Nichols, J.; Wilhelm, M.; Wright, A.; Cleland, J.A. Effectiveness of cervicothoracic and thoracic manual physical therapy in managing upper quarter disorders: A systematic review. J. Man. Manip. Ther. 2021, 30, 46–55. [Google Scholar] [CrossRef]
- Kardouni, J.R.; Pidcoe, P.E.; Shaffer, S.W.; Finucane, S.D.; Cheatham, S.A.; Sousa, C.O.; Michener, L.A. Thoracic spine manipulation in SIS does not immediately alter thoracic or scapular kinematics: Randomized controlled trial. J. Orthop. Sports Phys. Ther. 2015, 45, 527–538. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Ghrouz, A.K.; Hussain, M.E.; Sharma, S.; Aldabbas, M.; Ansari, S. Progressive resistance exercises plus manual therapy improve isometric strength in overhead athletes with SIS: Randomized controlled trial. Biomed. Res. Int. 2021, 2021, 9945775. [Google Scholar] [CrossRef]
- Bialosky, J.E.; Bishop, M.D.; Price, D.D.; Robinson, M.E.; George, S.Z. Mechanisms of manual therapy in musculoskeletal pain: A comprehensive model. Man. Ther. 2009, 14, 531–538. [Google Scholar] [CrossRef] [PubMed]
| Participants | Intervention | |||||||
|---|---|---|---|---|---|---|---|---|
| Author (Year) | Country | Mean Age (SD) | Population | Thoracic Extension Exercises | Control Group | Session Duration | Frequency (Sessions/Week) | Total Number of Sessions |
| Thoracic manual therapy in isolation | ||||||||
| Haik et al. (2017) [26] | Brazil | EG: 32.5 (12.0) CG: 31.3 (11.0) | Adults with SPS n = 61 | Thoracic spine manipulation n = 30 | Sham TSM n = 31 | NR | 2 | 2 |
| Grimes et al. (2019) A [29] | United States | EG: 37.6 (15.3) CG: 36.5 (15.5) | Adults with SPS n = 40 | Supine thrust manipulation n = 20 | Sham manipulation n = 20 | 2 sessions | 1 | 1 |
| Grimes et al. (2019) B [29] | United States | EG: 35.6 (14.7) CG: 36.5 (15.5) | Adults with SPS n = 40 | Seated thrust manipulation n = 20 | Sham manipulation n = 20 | 2 sessions | 1 | 1 |
| Hunter et al. (2022) A [27] | Australia | EG:62.0 (9.6) CG: 61.4 (11.3) | Adults 40+ with SPS n = 50 | MET n = 25 | Placebo laser n = 25 | 15 min | 1 | 4 |
| Hunter et al. (2022) B [27] | Australia | EG: 56.9 (9.2) CG: 61.4 (11.3) | Adults 40+ with SPS n = 50 | MET + Soft Tissue Mobilization n = 25 | Placebo laser n = 25 | 15 min | 1 | 4 |
| Thoracic manual therapy combined with exercise | ||||||||
| Haider et al. (2018) [30] | Pakistan | EG: 49.3 (9.9) CG: 49.8 (9.7) | Adults with SPS n = 40 | Thoracic manipulative therapy + exercise n = 20 | Exercise therapy n = 20 | Not described | 3 | 6 |
| Park et al. (2020) A [28] | Korea | EG: 49.2 (9.48) CG: 50.2 (8.99) | Adults with SPS and thoracic kyphosis n = 20 | Thoracic mobilization + extension exercises n = 10 | Thoracic Mobilization n = 10 | 15 min | 3 | 12 |
| Park et al. (2020) B [28] | Korea | EG: 50.9 (9.10) CG: 50.2 (8.99) | Adults with SPS and thoracic kyphosis n = 20 | Thoracic mobilization + extension exercises n = 10 | Extension exercises n = 10 | 15 min | 3 | 12 |
| Abu El Kassem et al. (2024) [13] | Egypt | EG: 32.15 (4.93) CG: 31.6 (4.59) | Recreational adults with SPS n = 74 | SNAGs + shoulder exercises n = 37 | Traditional shoulder exercises n = 37 | 60 min | 3 | 12 |
| Michener et al. (2024) [11] | United States | EG: 52.3 (13.3) CG: 54.0 (11.1) | Adults with SPS n = 93 | Thoracic & scapular manual therapy + resistance exercise n = 52 | Resistance exercise n = 41 | 45–60 min | 2 | 10 |
| Author (Year) | Intervention | Control Group | Outcome (Tool) | Intragroup Results—MD (SD) | Between Groups MD (95% CI) |
|---|---|---|---|---|---|
| Thoracic manual therapy in isolation | |||||
| Haik et al. (2017) [26] | Thoracic manipulation | Sham manipulation | Pain (VAS) Disability (DASH) Quality of life (WORC) | NR −9.75 (no SD) −13.9% (no SD) | −1.1 (−1.7 to −0.5) * +0.1(−2.5 to 2.8) * −5.0 (−9.7 to −0.3) * |
| Grimes et al. (2019) A [29] | Thoracic supine manipulation | Sham manipulation | Pain and function (PSS) | +15.2 ± 4.8 | +4.0 (−2.0 to 5.8) * |
| Grimes et al. (2019) B [29] | Thoracic seated manipulation | Sham manipulation | Pain and function (PSS) | +13.6 ± 4.4 | +2.0 (−0.5 to 5.3) * |
| Hunter et al. (2022) A [27] | Muscle Energy Tecnhique (MET) + Soft tissue massage (STM) | MET | Pain and Disability (SPADI) Disability (DASH) Pain (VAS) Satisfaction (GROC) | NR NR NR NR | −1.1 (9.8 to 7.5) * −0.26 (6.0 to 5.5) * −7.7 (16.8 to 1.5) * 0.3 (0.4 to 1.0) * |
| Hunter et al. (2022) B [27] | MET + STM | Placebo laser | Pain and Disability (SPADI) Disability (DASH) Pain (VAS) Satisfaction GROC) | NR NR NR NR NR | −13.5 (22.3 to 4.8) * −8.2 (14.0 to 2.3) * −7.8 (17.1 to 1.5) * −2.0 (2.3 to 0,3) * +1.2 (0.5 to 1.9) * |
| Thoracic manual therapy combined with exercise | |||||
| Haider et al. (2018) [30] | Non-thrust + 3 thrust manipulations | Shoulder exercises | Pain (NPRS) Pain and Disability (SPADI) | −0.70 ± 0.92 −12.3 ± 4.7 | −4.65 (−15.2 to −5.8) * + 12.2* |
| Park et al. (2020) A [28] | Thoracic mobilization | Thoracic mobilization + Shoulder exercises | Pain and Disability (SPADI) ROM: (Goniometer): External rotation (ER) Internal rotation (IR) | −8.2 ± 3.1 NR NR | −5.13 * +2.7 * +2.7 (2.09 to 3.24) * |
| Park et al. (2020) B [28] | Shoulder exercises | Thoracic mobilization + Shoulder exercises | Pain and Disability (SPADI) ROM: ER IR | −6.7 ± 2.9 NR NR | −5.77 * 2.0 * 2.3 * |
| Abu El Kassem et al. (2024) [13] | SNAGs + Shoulder exercises | Shoulder exercises | Pain and Disability (SPADI) Pain (VAS) ROM (Goniometer): ER IR | −24.2 ± 8.7 −4.4 ± 1.3 NR NR | 1.61 (9.88 to 16.73) * 1.3 (3.65 to 5.56) * +5.7 (25.88 to 10.51) * +7.1 (26.57 to 7.42) * |
| Michener et al. (2024) [11] | Thoracic + scapular manual therapy + Shoulder exercises | Shoulder exercises | Disability (DASH) Satisfaction (GROC) | −6.7 ± 3.5 +2.3 ± 1.5 | −6.7 (11.4 to 2.1) * NR |
| Author (Year) | Item 1 | Item 2 | Item 3 | Item 4 | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Total PEDro Score (0–10) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hunter et al. (2022) [27] | Y | Y | Y | Y | Y | N | Y | Y | Y | Y | Y | 9 |
| Haik et al. (2017) [26] | Y | Y | N | Y | Y | N | Y | Y | Y | Y | Y | 8 |
| Abu El Kassem et al. (2024) [13] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Michener et al. (2024) [11] | Y | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8 |
| Park et al. (2020) [28] | Y | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7 |
| Grimes et al. (2019) [29] | Y | Y | Y | N | N | N | Y | Y | N | Y | Y | 6 |
| Haider et al. (2023) [30] | N | Y | N | Y | N | N | N | Y | N | Y | Y | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Robles-Pérez, R.; Vallejo-Martínez, R.; Carrasco-Uribarren, A.; Jiménez-del-Barrio, S.; Hernández-Lázaro, H.; Ceballos-Laita, L. Thoracic Manual Therapy With or Without Exercise Improves Pain and Disability in Subacromial Pain Syndrome: A Systematic Review of Randomized Trials. Healthcare 2025, 13, 2479. https://doi.org/10.3390/healthcare13192479
Robles-Pérez R, Vallejo-Martínez R, Carrasco-Uribarren A, Jiménez-del-Barrio S, Hernández-Lázaro H, Ceballos-Laita L. Thoracic Manual Therapy With or Without Exercise Improves Pain and Disability in Subacromial Pain Syndrome: A Systematic Review of Randomized Trials. Healthcare. 2025; 13(19):2479. https://doi.org/10.3390/healthcare13192479
Chicago/Turabian StyleRobles-Pérez, Román, Rodrigo Vallejo-Martínez, Andoni Carrasco-Uribarren, Sandra Jiménez-del-Barrio, Héctor Hernández-Lázaro, and Luis Ceballos-Laita. 2025. "Thoracic Manual Therapy With or Without Exercise Improves Pain and Disability in Subacromial Pain Syndrome: A Systematic Review of Randomized Trials" Healthcare 13, no. 19: 2479. https://doi.org/10.3390/healthcare13192479
APA StyleRobles-Pérez, R., Vallejo-Martínez, R., Carrasco-Uribarren, A., Jiménez-del-Barrio, S., Hernández-Lázaro, H., & Ceballos-Laita, L. (2025). Thoracic Manual Therapy With or Without Exercise Improves Pain and Disability in Subacromial Pain Syndrome: A Systematic Review of Randomized Trials. Healthcare, 13(19), 2479. https://doi.org/10.3390/healthcare13192479







