Patterns of Perfusion of Free ALT Flaps vs. Propeller Flaps of the Lower Extremity: A Comparative Study with the Use of LDSP †
Abstract
1. Introduction
2. Methods
2.1. Perfusion Monitoring
2.2. Perioperative Protocol
2.3. Statistical Analysis
3. Results
3.1. Patient Demographics
3.2. Perioperative Characteristics and Complications
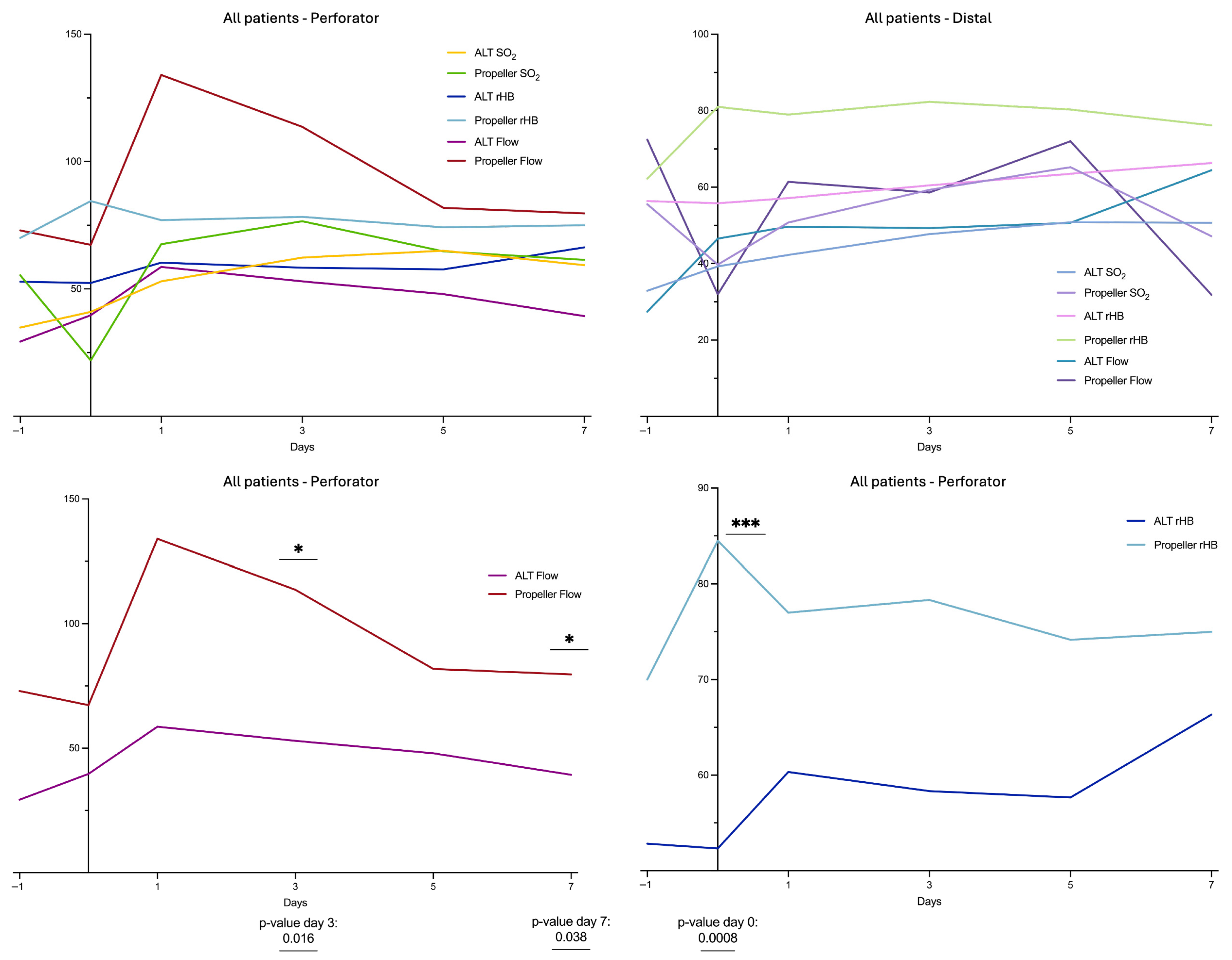
3.3. Perfusion Monitoring
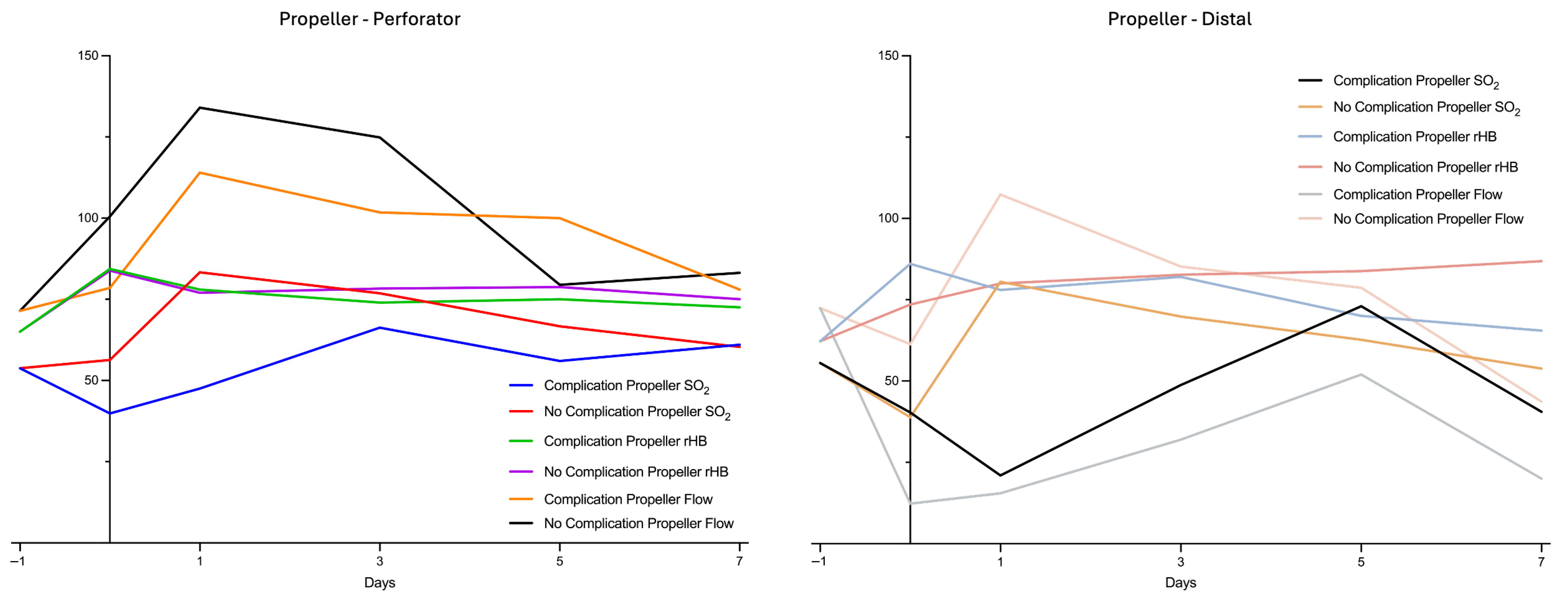
3.4. Comparison of Subgroups in Propeller Flaps
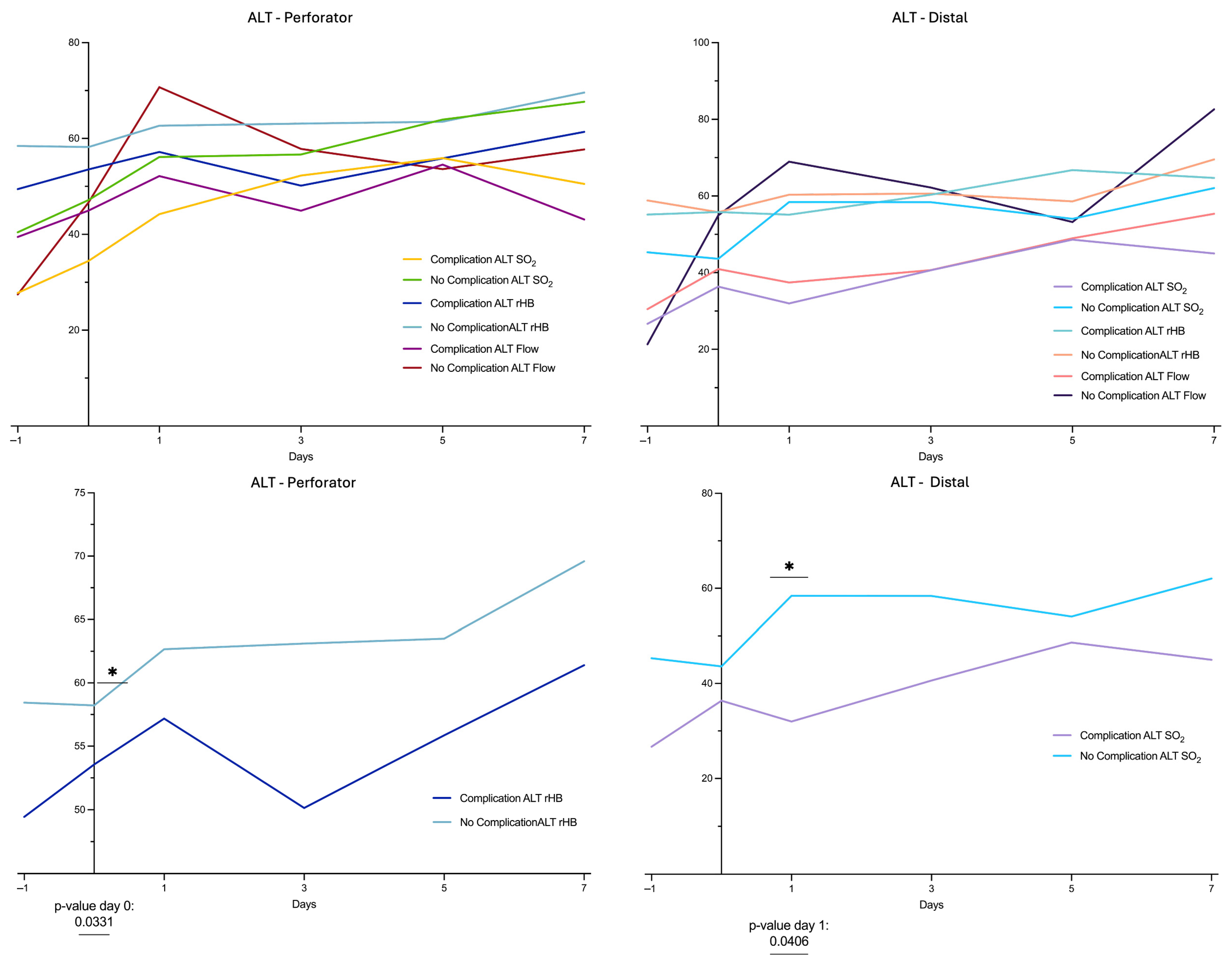
3.5. Comparison of Subgroups in ALT Flaps
3.6. Comparison of Subgroups in Propeller vs. ALT Flaps
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Song, Y.; Chen, G.; Song, Y. The free thigh flap: A new free flap concept based on the septocutaneous artery. Br. J. Plast. Surg. 1984, 37, 149–159. [Google Scholar] [CrossRef]
- Shieh, S.-J.; Chiu, H.-Y.; Yu, J.-C.; Pan, S.-C.; Tsai, S.-T.; Shen, C.-L. Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast. Reconstr. Surg. 2000, 105, 2349–2357. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, S.; Gideroğlu, K.; Aköz, T. Anterolateral thigh flap: Ideal free flap choice for lower extremity soft-tissue reconstruction. J. Reconstr. Microsurg. 2003, 19, 225–234. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.Z.; Mathes, D.W.; Zenn, M.R.; Neligan, P.C. The application of indocyanine green fluorescence angiography in plastic surgery. J. Reconstr. Microsurg. 2011, 27, 355–364. [Google Scholar] [CrossRef]
- Ozkan, O.; Coskunfirat, O.K.; Ozgentas, H.E. The use of free anterolateral thigh flap for reconstructing soft tissue defects of the lower extremities. Ann. Plast. Surg. 2004, 53, 455–461. [Google Scholar] [CrossRef]
- Bergeron, L.; Tang, M.; Morris, S.F. A review of vascular injection techniques for the study of perforator flaps. Plast. Reconstr. Surg. 2006, 117, 2050–2057. [Google Scholar] [CrossRef]
- Yildirim, S.; Avci, G.; Aköz, T. Soft-tissue reconstruction using a free anterolateral thigh flap: Experience with 28 patients. Ann. Plast. Surg. 2003, 51, 37–44. [Google Scholar] [CrossRef]
- Cordova, A.; D’Arpa, S.; Di Lorenzo, S.; Toia, F.; Campisi, G.; Moschella, F. Prophylactic chimera anterolateral thigh/vastus lateralis flap: Preventing complications in high-risk head and neck reconstruction. J. Oral Maxillofac. Surg. 2014, 72, 1013–1022. [Google Scholar] [CrossRef] [PubMed]
- Wink, J.D.; Nelson, J.A.; Cleveland, E.; Grover, R.; Wu, L.C.; Levin, L.S.; Kovach, S.J.; Fischer, J.P. A retrospective review of outcomes and flap selection in free tissue transfers for complex lower extremity reconstruction. J. Reconstr. Microsurg. 2013, 29, 407–416. [Google Scholar] [CrossRef]
- Quaba, O.; Quaba, A. Pedicled Perforator Flaps for the Lower Limb. Semin. Plast. Surg. 2006, 20, 103–111. [Google Scholar] [CrossRef]
- Teo, T.C. The propeller flap concept. Clin. Plast. Surg. 2010, 37, 615–626. [Google Scholar] [CrossRef]
- Jakubietz, R.G.; Jakubietz, M.G.; Gruenert, J.G.; Kloss, D.F. The 180-degree perforator-based propeller flap for soft tissue coverage of the distal, lower extremity: A new method to achieve reliable coverage of the distal lower extremity with a local, fasciocutaneous perforator flap. Ann. Plast. Surg. 2007, 59, 667–671. [Google Scholar] [CrossRef] [PubMed]
- Gir, P.; Cheng, A.; Oni, G.; Mojallal, A.; Saint-Cyr, M. Pedicled-perforator (propeller) flaps in lower extremity defects: A systematic review. J. Reconstr. Microsurg. 2012, 28, 595–602. [Google Scholar] [CrossRef] [PubMed]
- Schaverien, M.; Saint-Cyr, M. Perforators of the Lower Leg: Analysis of Perforator Locations and Clinical Application for Pedicled Perforator Flaps. Plast. Reconstr. Surg. 2008, 122, 161–170. [Google Scholar] [CrossRef]
- Rad, A.N.; Singh, N.K.; Rosson, G.D. Peroneal artery perforator-based propeller flap reconstruction of the lateral distal lower extremity after tumor extirpation: Case report and literature review. Microsurgery 2008, 28, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Pignatti, M.; Ogawa, R.; Hallock, G.G.; Mateev, M.; Georgescu, A.V.; Balakrishnan, G.; Ono, S.; Cubison, T.C.S.; D’arpa, S.; Koshima, I.; et al. The “Tokyo” consensus on propeller flaps. Plast. Reconstr. Surg. 2011, 127, 716–722. [Google Scholar] [CrossRef]
- Attinger, C.; Cooper, P.; Blume, P. Vascular anatomy of the foot and ankle. Oper. Tech. Plast. Reconstr. Surg. 1997, 4, 183–198. [Google Scholar] [CrossRef]
- Bekara, F.; Herlin, C.; Somda, S.; de Runz, A.; Grolleau, J.L.; Chaput, B. Free versus perforator-pedicled propeller flaps in lower extremity reconstruction: What is the safest coverage? A meta-analysis. Microsurgery 2018, 38, 109–119. [Google Scholar] [CrossRef]
- Masia, J.; Moscatiello, F.; Pons, G.; Fernandez, M.; Lopez, S.; Serret, P. Our experience in lower limb reconstruction with perforator flaps. Ann. Plast. Surg. 2007, 58, 507–512. [Google Scholar] [CrossRef]
- Jakubietz, R.G.; Jakubietz, D.F.; Gruenert, J.G.; Schmidt, K.; Meffert, R.H.; Jakubietz, M.G. Reconstruction of soft tissue defects of the Achilles tendon with rotation flaps, pedicled propeller flaps and free perforator flaps. Microsurgery 2010, 30, 608–613. [Google Scholar] [CrossRef]
- Nelson, J.A.; Fischer, J.P.; Brazio, P.S.; Kovach, S.J.; Rosson, G.D.; Rad, A.N. A review of propeller flaps for distal lower extremity soft tissue reconstruction: Is flap loss too high? Microsurgery 2013, 33, 578–586. [Google Scholar] [CrossRef]
- Kneser, U.; Beier, J.P.; Schmitz, M.; Arkudas, A.; Dragu, A.; Schmidt, V.J.; Kremer, T.; Horch, R.E. Zonal perfusion patterns in pedicled free-style perforator flaps. J. Plast. Reconstr. Aesthetic Surg. 2014, 67, e9–e17. [Google Scholar] [CrossRef]
- Teo, T.C. Propeller Flaps for Reconstruction around the Foot and Ankle. J. Reconstr. Microsurg. 2021, 37, 22–31. [Google Scholar] [CrossRef]
- Yu, P.; Youssef, A. Efficacy of the handheld Doppler in preoperative identification of the cutaneous perforators in the anterolateral thigh flap. Plast. Reconstr. Surg. 2006, 118, 928–933. [Google Scholar] [CrossRef]
- Wong, C.-H.M.; Cui, F.; Tan, B.-K.M.; Liu, Z.; Lee, H.-P.; Lu, C.; Foo, C.-L.M.; Song, C.M. Nonlinear finite element simulations to elucidate the determinants of perforator patency in propeller flaps. Ann. Plast. Surg. 2007, 59, 672–678. [Google Scholar] [CrossRef]
- Bernuth, S.; Vater, A.; Fuchs, K.F.; Meffert, R.H.; Jakubietz, R.G. Perfusion changes in perforator-based propeller flaps. J. Reconstr. Microsurg. Open 2023, 8, e45–e50. [Google Scholar] [CrossRef]
- Blough, J.T.; Saint-Cyr, M.H. Propeller flaps in lower extremity reconstruction. Clin. Plast. Surg. 2021, 48, 173–181. [Google Scholar] [CrossRef] [PubMed]
- Shimbo, K.; Kawamoto, H.; Koshima, I. Muscle/musculocutaneous versus fasciocutaneous free flap reconstruction in the lower extremity: A systematic review and meta-analysis. Microsurgery 2022, 42, 835–847. [Google Scholar] [CrossRef]
- Bigdeli, A.K.; Didzun, O.; Thomas, B.; Harrhaus, L.; Gazyakan, E.; Horch, R.E.; Kneser, U. Combined versus Single Perforator Propeller Flaps for Reconstruction of Large Soft Tissue Defects: A Retrospective Clinical Study. J. Pers. Med. 2022, 12, 41. [Google Scholar] [CrossRef] [PubMed]
- Mitsutoshi, O.; Makoto, M.; Naoya, W.; Kohei, S.; Iwasaki, N. Clinical outcomes of perforator-based propeller flaps versus free flaps in soft tissue reconstruction for lower leg and foot trauma: A retrospective single-centre comparative study. MCV Musculoskelet. Disord. 2024, 25, 297. [Google Scholar]
- Innocenti, M.; Menichini, G.; Baldrighi, C.; Delcroix, L.; Vignini, L.; Pierluigi, T. Are There Risk Factors for Complications of Perforator-based Propeller Flaps for Lower-extremity Reconstruction? Clin. Orthop. Relat. Res. 2014, 472, 2276–2286. [Google Scholar] [CrossRef]
- Chaput, B.; Grolleau, J.L.; Garrido, I.; Mojallal, A.; Bertheuil, N.; Carloni, R.; Herlin, C.; Sinna, R. Delayed procedure in propeller perforator flap: Defining the venous perforasome. J. Plast. Reconstr. Aesthetic Surg. 2017, 70, 286–289. [Google Scholar] [CrossRef]
- Brown, J.S.; Devine, J.C.; Magennis, P.; Sillifant, P.; Rogers, S.N.; Vaughan, E.D. Factors that influence the outcome of salvage in free tissue transfer. Br. J. Oral Maxillofac. Surg. 2003, 41, 16–20. [Google Scholar] [CrossRef]
- Bui, D.T.; Cordeiro, P.G.; Hu, Q.Y.; Disa, J.J.; Pusic, A.; Mehrara, B.J. Free flap reexploration: Indications, treatment, and outcomes in 1193 free flaps. Plast. Reconstr. Surg. 2007, 119, 2092–2100. [Google Scholar] [CrossRef] [PubMed]
- Vijan, S.S.; Tran, V.N. Microvascular breast reconstruction pedicle thrombosis: How long can we wait? Microsurgery 2007, 27, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Chen, K.-T.; Mardini, S.; Chuang, D.C.-C.; Lin, C.-H.; Cheng, M.-H.; Lin, Y.-T.; Huang, W.-C.; Tsao, C.-K.; Wei, F.-C. Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast. Reconstr. Surg. 2007, 120, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Koshima, I.; Nanba, Y.; Tsutsui, T.; Takahashi, Y. New Anterolateral Thigh Perforator Flap with a Short Pedicle for Reconstruction of Defects in the Upper Extremities. Ann. Plast. Surg. 2003, 51, 30–36. [Google Scholar] [CrossRef]

| Characteristics | Propeller (n = 7) | ALT (n = 18) | p-Value |
|---|---|---|---|
| Demographics | |||
| Male sex (n) | 6 (85.7) | 11 (61.1) | 0.36 |
| Female sex (n) | 1 (14.3) | 7 (38.9) | 0.36 |
| Age, median years (IQR) | 62 (25) | 58 (18) | 0.95 |
| Comorbidities | |||
| Hypertension | 3 (42.9) | 7 (38.9) | >0.99 |
| Diabetes | 2 (28.6) | 1 (5.56) | 0.18 |
| Arterial occlusive disease | 1 (14.3) | 5 (27.8) | 0.64 |
| Nicotine | 1 (14.3) | 6 (33.3) | 0.63 |
| Defect Cause | |||
| Trauma | 5 (71.4) | 7 (38.9) | 0.20 |
| Cancer | 1 (14.3) | 1 (5.56) | 0.49 |
| Chronic Wound | 1 (14.3) | 5 (27.8) | 0.64 |
| Infection | 0 (0.00) | 2 (11.1) | >0.99 |
| Wound healing disorder | 0 (0.00) | 2 (11.1) | >0.99 |
| Autoaggression | 0 (0.00) | 1 (5.56) | >0.99 |
| Characteristics | Propeller (n = 7) | ALT (n = 18) | p-Value |
|---|---|---|---|
| Operative time, median minutes (IQR) | 100 (70) | 235 (72.5) | <0.0001 |
| Length of hospital stay, median days (IQR) | 28 (9) | 22 (17) | 0.58 |
| Debridement prior coverage | 3 (42.9) | 2 (11.1) | 0.11 |
| Negative pressure wound therapy | 7 (100) | 17 (94.4) | >0.99 |
| Microbial contamination prior to coverage | 6 (85.7) | 15 (83.3) | >0.99 |
| Complications | |||
| Patients (n) | 4 (57.1) | 12 (66.7) | 0.67 |
| Prolonged wound healing | 3 (42.9) | 8 (44.4) | >0.99 |
| Superficial incisional infection | 0 (0.00) | 2 (11.1) | >0.99 |
| Epidermolysis | 2 (28.6) | 1 (5.56) | 0.18 |
| Partial flap necrosis | 1 (14.3) | 2 (11.1) | >0.99 |
| Complete flap necrosis | 0 (0.00) | 1 (5.5) | >0.99 |
| Flap survival | 7 (100) | 17 (94.4) | >0.99 |
| Reoperation | 2 (28.6) | 6 (33.3) | >0.99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bernuth, S.; Niederegger, T.; Hundeshagen, G.; Fuchs, K.; Meffert, R.H.; Jakubietz, R.G. Patterns of Perfusion of Free ALT Flaps vs. Propeller Flaps of the Lower Extremity: A Comparative Study with the Use of LDSP. Healthcare 2025, 13, 2441. https://doi.org/10.3390/healthcare13192441
Bernuth S, Niederegger T, Hundeshagen G, Fuchs K, Meffert RH, Jakubietz RG. Patterns of Perfusion of Free ALT Flaps vs. Propeller Flaps of the Lower Extremity: A Comparative Study with the Use of LDSP. Healthcare. 2025; 13(19):2441. https://doi.org/10.3390/healthcare13192441
Chicago/Turabian StyleBernuth, Silvia, Tobias Niederegger, Gabriel Hundeshagen, Konrad Fuchs, Rainer H. Meffert, and Rafael G. Jakubietz. 2025. "Patterns of Perfusion of Free ALT Flaps vs. Propeller Flaps of the Lower Extremity: A Comparative Study with the Use of LDSP" Healthcare 13, no. 19: 2441. https://doi.org/10.3390/healthcare13192441
APA StyleBernuth, S., Niederegger, T., Hundeshagen, G., Fuchs, K., Meffert, R. H., & Jakubietz, R. G. (2025). Patterns of Perfusion of Free ALT Flaps vs. Propeller Flaps of the Lower Extremity: A Comparative Study with the Use of LDSP. Healthcare, 13(19), 2441. https://doi.org/10.3390/healthcare13192441







