1. Introduction
The post-COVID-19 recovery period offers a critical window for assessing the ongoing psychological impacts of the pandemic on college students, particularly those from culturally marginalized and historically underserved groups. Among these students are Arab/Middle Eastern (AME) individuals, both domestic and international. These groups represent distinct cultural and structural communities shaped by specific sociocultural, institutional, and immigration-related experiences that may have influenced how they were affected by the pandemic’s mental health consequences.
During 2022–2023, more than 38,000 international students from the Middle East and North Africa (MENA) region were enrolled in colleges and universities in the United States (U.S.) [
1]. This group made up nearly 4% of the entire international student population in the U.S. [
2]. In addition, the U.S. is home to roughly 3.7 million Arab Americans, many of whom are of traditional college age, i.e., 18–24 years old. A large number of these students are enrolled in higher education, especially in states such as Michigan, California, New York, and Illinois [
3]. Although their presence in higher education is significant, AME students continue to be underrepresented in mental health research and often encounter barriers to accessing adequate campus support services [
4,
5]. Prior studies have documented that they experience higher rates of anxiety and depression, partly due to racial discrimination, Islamophobia, and systemic marginalization within U.S. educational settings [
6,
7,
8].
While Arab Americans and AME international students may share ethnic roots, their lived experiences within and beyond the U.S. education system can shape their mental health in very different ways. AME international students are at greater risk for depression, anxiety, and loneliness due to the stress of adapting to a new culture, limited access to support networks, and separation from their families and home communities [
9,
10].
Studies conducted during the COVID-19 pandemic highlighted loneliness as a significant concern for young adults. One national study of U.S. young adults during COVID-19 revealed high levels of loneliness, which were strongly linked to mental health struggles such as anxiety and depression and substance use [
11]. While these issues were widespread among college students during the pandemic, the intensity of loneliness and its impact varied across different student groups [
12,
13,
14]. Similar patterns have been reported among international students in other contexts; for example, a systematic review and meta-analysis of Chinese international students during COVID-19 documented elevated depression and anxiety, underscoring the global salience of these concerns [
15]. Moreover, these mental health challenges have also been observed in other countries, including the UK and Australia, where international students report elevated rates of depression, anxiety, and loneliness, often linked to acculturative stress, social isolation, and barriers to accessing culturally appropriate care [
16,
17]. Despite this international evidence, very few studies have explicitly focused on Arab American or AME international students in this context, leaving a major gap in understanding how loneliness manifests in these culturally specific populations. Some researchers have described this situation as part of a broader “social recession,” calling attention to the widespread impact of social isolation on young people’s mental health. This highlights the need for more detailed research on how loneliness affects students from diverse backgrounds [
18,
19,
20].
Although there are well-documented differences in mental health service use among racial and ethnic groups in college settings, there is limited data on how AME students seek out mental health care, especially through digital services. This gap is particularly important because many mental health services shifted to virtual formats during the pandemic. As digital tools become an essential part of campus mental health support, it is critical to understand who is using them and how they are accessed by different groups. Study aims. This study (i) compares the prevalence of depression, anxiety, and loneliness between Arab American and AME international students; (ii) tests bidirectional associations between loneliness and depression/anxiety; and (iii) evaluates whether perceived need mediates the association between symptoms and digital mental health (DMH) service use.
Research Hypotheses
H1. Arab American and AME international students will differ in their prevalence of depression, anxiety, and loneliness.
H2. Loneliness will show a bidirectional association with depression and anxiety.
H3. Perceived need will mediate the relationship between mental health symptoms and DMH service use.
2. Materials and Methods
2.1. Data Source and Sample Selection
This study used secondary data from the 2022–2024 cycle of the Healthy Minds Study (HMS), a national online survey of mental health, health behaviors, and service use among U.S. college and university students [
21]. The HMS employs validated instruments, including the Patient Health Questionnaire-9 (PHQ-9) and the Generalized Anxiety Disorder 7-item scale (GAD-7). Core modules collect data on demographics, mental health conditions, and service utilization, while participating institutions may add optional modules tailored to their needs.
The HMS sample is large and diverse, covering approximately 124 campuses. At each institution, about 4000 students are randomly selected to participate [
22]. With Institutional Review Board (IRB) approval, this study incorporates administrative data supplied by participating institutions. To ensure representativeness, non-response propensity weights were applied using institutional records (e.g., gender, race/ethnicity, academic level, and GPA), consistent with HMS protocols. Due to privacy and ethical considerations, HMS data are restricted but may be accessed upon request and with permission from the Healthy Minds Network [
23]. IRB approval for the use of these secondary data was obtained from the University of Louisville (IRB Number: 25.0308; Approval Date: 5 August 2025).
Figure 1 demonstrates the sample selection process. A total of 181,135 survey responses were collected. Of these, 177,300 non-AME respondents were excluded, retaining a subsample of 3835 AME students. Among these, 535 were removed due to missing data on the key outcome variable, DMH service use. Of the remaining 3300 students, another 51 were removed due to incomplete responses on at least one of the following variables: depression (
n = 16), anxiety (
n = 9), loneliness (
n = 17), and perceived need for mental health care (
n = 9).
The final analytic sample included 3249 AME students with complete data on all study variables. Based on self-reported citizenship and visa status, this sample was further divided into two groups: Arab American (n = 2662) and AME international students (n = 587). Group-level comparisons were conducted only for Hypothesis 1, whereas Hypotheses 2 and 3 were tested across the full Arab/Middle Eastern student sample (combining both groups).
2.2. Conceptual Framework
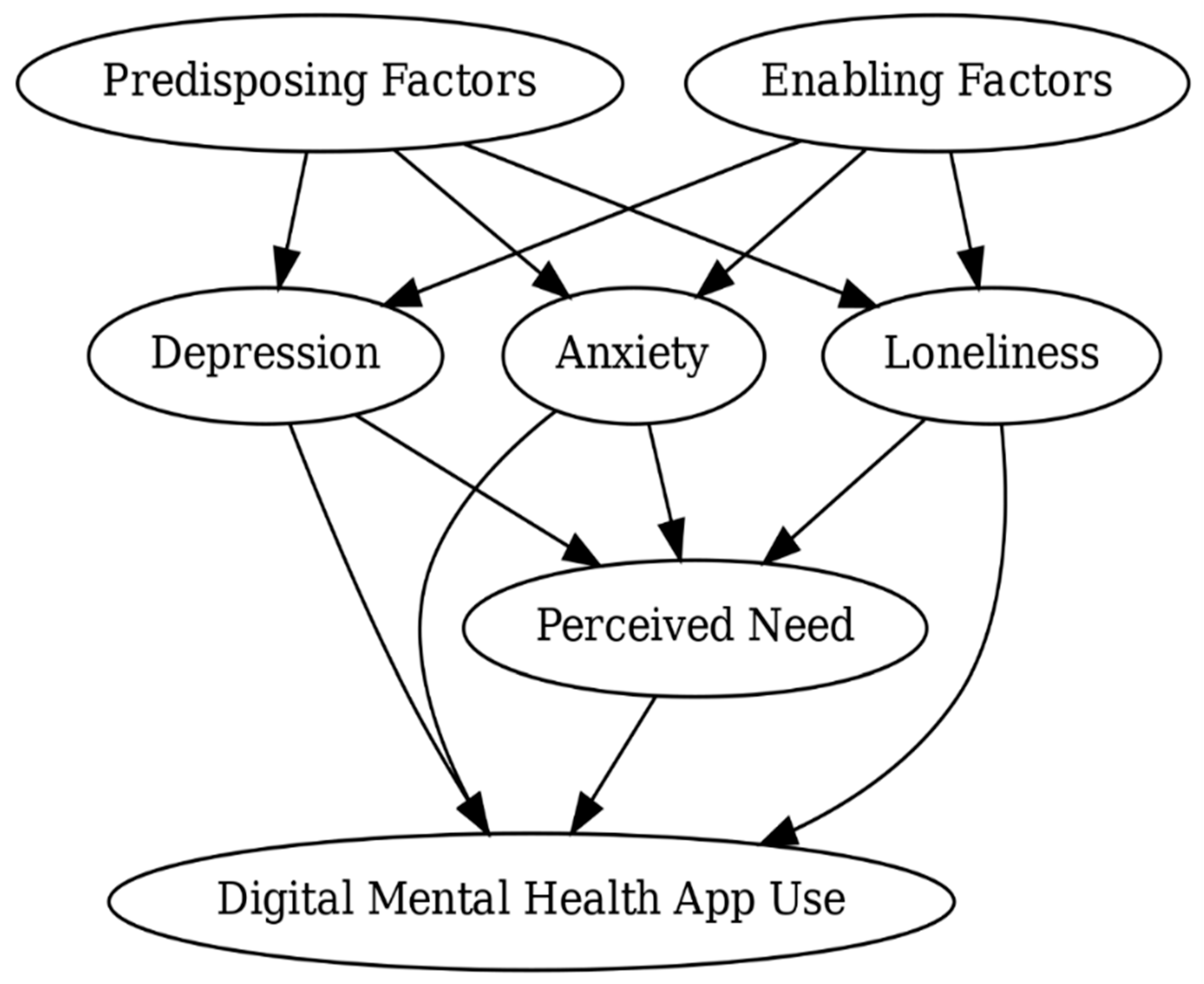
This study’s conceptual framework was guided by Andersen’s Behavioral Model of Health Services Use, which is a widely used theoretical framework for examining the factors influencing health care utilization [
24]. The model identifies three primary domains that shape service use: predisposing factors (e.g., demographic characteristics), enabling factors (e.g., awareness of services or insurance coverage), and need-based factors (e.g., perceived or evaluated illness severity). In this study’s adapted framework, mental health indicators, including depression, anxiety, and loneliness, were conceptualized as need-related factors, which influence students’ perceived need for care and ultimately their utilization of DMH services. Perceived need, defined as a student’s self-acknowledged need for emotional or mental health support, was modeled as a proximal mediator between psychological symptoms and engagement with DMH services [
25]. Enabling factors, including perceived social support, awareness of campus services, and insurance coverage, function as a structural element that can either promote or hinder access to mental health resources [
26,
27]. Predisposing factors, such as age, gender, degree level, race, and international student status, reflect background characteristics that may influence students’ mental health beliefs, prior experiences with care, and cultural perceptions of help-seeking [
26,
27,
28].
Furthermore, loneliness is viewed not just as a symptom of mental health need but also as a factor that can shape how students respond to that need. It may influence whether, and how strongly, perceived need leads to seeking help. This approach is informed by empirical research showing the bidirectional relationship between loneliness and mental health conditions, such as depression and anxiety [
29]. This conceptual approach builds on prior applications of Andersen’s model in studies focused on digital health and college student populations [
24,
25,
26].
Figure 2 illustrates the proposed conceptual relationships among these variables.
2.3. Measures
2.3.1. Digital Mental Health Services Utilization
Digital mental health (DMH) service utilization was assessed using up to three items available across survey datasets: (1) “Have you ever used a smartphone app to manage your wellness or mental/emotional health?” (2) “Do you utilize any self-guided therapy resources through a phone app or website?” and (3) “Have you ever used a mobile app that provides resources or services for mental health support (e.g., BetterHelp, Calm, Headspace, TalkCampus)?” Because not all datasets included all three items, a standardized binary indicator was created to reflect DMH use across all datasets. The coding followed a hierarchical logic: when the first item was available, responses of “Yes” were coded as 1 (indicating use), and “No” as 0. If this item was unavailable or missing, responses to the second item were used, with “Yes” coded as 1 and “No” as 0. If neither of the above items indicated use, the third item was considered, with “Yes” coded as 1 and “No” coded as 0. Responses of “Prefer not to say” were treated as missing. This stepwise process enabled the integration of DMH utilization indicators across multiple survey waves and instruments. Missing values in the constructed variable were retained during initial processing, and cases with missing DMH use were excluded from the final analysis to ensure data completeness for multivariable modeling.
2.3.2. Depression (PHQ-9)
Depression status was assessed using the PHQ-9, a widely validated nine-item questionnaire that asks the following: “Over the last two weeks, how often have you been bothered by any of the following problems?” The items cover symptoms such as lack of interest or pleasure, feeling down or hopeless, sleep issues, fatigue, appetite changes, low self-worth, difficulty concentrating, psychomotor changes, and suicidal thoughts. Each item was answered on a four-point scale: 1 = Not at all, 2 = Several days, 3 = More than half the days, and 4 = Nearly every day. To prepare the data for analysis, responses were recoded from 1–4 into numerical scores ranging from 0–3, aligning with standard PHQ-9 scoring practices. A composite variable, phq9_total, was created by summing the recoded scores across all nine items. A cutoff score of 10 or higher on the PHQ-9 was used to indicate moderate to severe depressive symptoms, consistent with established clinical and research guidelines [
30]. A binary variable, depression_status, was then created: students with a total score of 10 or more were coded as 1, while those scoring below 10 were coded as 0.
2.3.3. Anxiety (GAD-7)
Anxiety status was measured using the GAD-7, a validated seven-item screening tool for generalized anxiety disorder. Participants were asked the following: “Over the last two weeks, how often have you been bothered by the following problems?” The items addressed symptoms such as nervousness, excessive worrying, restlessness, irritability, and fear of impending doom. Response options were as follows: 1 = Not at all, 2 = Several days, 3 = Over half the days, and 4 = Nearly every day. Each item was recoded into a numerical scale from 0 to 3, in line with standard GAD-7 scoring. A total score, gad7_total, was calculated by summing the values across all seven items. A score of 10 or higher indicated moderate to severe anxiety, based on widely accepted research thresholds [
31]. A binary variable, anxiety_status, was then created: respondents scoring 10 or above were coded as 1, while those scoring below 10 were coded as 0. This binary variable allowed for the identification of students at risk for clinically significant anxiety symptoms.
Consistent with established psychometric guidelines and Healthy Minds Study protocols, participants were included in PHQ-9 analyses if they answered at least 7 of the 9 items [
23]. When 1 or 2 items were missing, those missing values were imputed using the mean of the completed items to preserve scoring validity. For the GAD-7, a minimum of 6 completed items was required, with similar mean imputation applied for up to 1 missing item. Respondents who did not meet these minimum criteria were excluded from depression- or anxiety-related analyses to ensure data integrity and adherence to scoring standards [
23,
32].
2.3.4. Loneliness (UCLA 3-Item Scale)
Loneliness was measured using the UCLA 3-item Loneliness Scale, a validated instrument assessing subjective feelings of social isolation and lack of companionship. Participants responded to three questions: how often they feel (1) lacking companionship, (2) left out, and (3) isolated from others, using a 3-point scale (1 = “Hardly ever,” 2 = “Some of the time,” 3 = “Often”). A composite loneliness score (lonesc) was computed by summing the three items (range: 3–9), with higher scores indicating greater loneliness. A binary indicator variable (lonely) was also generated, where values >6 and <9 were coded as lonely (1), and values ≤6 as not lonely (0) [
33]. Respondents missing any of the three items were excluded from the scale.
2.3.5. Perceived Mental Health Need
Perceived mental health need was assessed using a self-reported item that asked participants to indicate their agreement with the statement: “In the past 12 months, I needed help for emotional or mental health problems or challenges such as feeling sad, blue, anxious, or nervous.” Responses were recorded on a six-point Likert scale ranging from 1 (Strongly agree) to 6 (Strongly disagree). To create a binary indicator variable, responses were dichotomized: participants selecting “Strongly agree,” “Agree,” or “Somewhat agree” (values 1–3) were coded as 1, indicating perceived need, while those selecting “Somewhat disagree,” “Disagree,” or “Strongly disagree” (values 4–6) were coded as 0. Missing responses were preserved during processing and subsequently excluded from regression analyses to maintain analytic integrity.
2.3.6. Insurance
Health insurance status was derived from a multi-response item asking participants to indicate the source(s) of their current health insurance coverage. Respondents could select multiple options, including coverage through parents, employers, student plans, government programs, embassies, or self-purchased plans. Two additional response options captured lack of coverage, “I do not have any health insurance coverage,” and uncertainty, “I am uncertain about whether I have health insurance”.
Responses were recoded into a single indicator to create a binary insurance status variable for analysis. Participants were classified as insured (coded as 1) if they selected any coverage source (options 2–8 or 10). Those who indicated no insurance (option 1) or uncertainty about coverage (option 9) were classified as uninsured (coded as 0). The missing cases were retained as a separate category to preserve sample size; however, this group was not included in the substantive interpretation of findings.
2.3.7. Treatment Efficacy (Medication and Therapy)
Beliefs about mental health treatment efficacy were assessed using two items: one regarding medication and one regarding counseling or therapy. Respondents were asked: (1) “How helpful on average do you think medication would be for you if you were having mental or emotional health problems?” and (2) “How helpful on average do you think therapy or counseling would be for you if you were having mental or emotional health problems?” Response options for both items included the following: “Very helpful,” “Helpful,” “Somewhat helpful,” and “Not helpful.” For each, a binary variable was created where responses of “Very helpful,” “Helpful,” or “Somewhat helpful” were coded as 1 (indicating a belief that the treatment would be helpful), and “Not helpful” was coded as 0. The missing cases were retained as a separate category to preserve sample size; however, this group was not included in the substantive interpretation of findings. This approach allowed for the inclusion of treatment belief indicators in multivariable analyses without compromising the integrity of results due to listwise deletion.
2.3.8. Awareness of Campus Mental Health Services
Awareness of available mental health services on campus was assessed using the following item: “If I needed to seek professional help for my mental or emotional health, I would know where to go on my campus.” Responses were collected using a six-point Likert scale, ranging from 1 = Strongly agree to 6 = Strongly disagree. In the 2020–2021 and 2021–2022 survey waves, this item was pre-coded into a binary format. To ensure consistency across years, a harmonized binary variable was used in which students who expressed any level of agreement (Strongly agree, Agree, or Somewhat agree) were coded as 1 “aware”, and those who expressed any level of disagreement “Somewhat disagree, Disagree, or Strongly disagree” were coded as 0 “not aware”.
Missing responses were recoded as a distinct category. These cases were retained for descriptive analysis but omitted from inferential models and interpretation to maintain analytical precision while preserving overall sample size.
2.3.9. Perceived Social Support
Perceived social support was assessed using the item: “My social relationships are supportive and rewarding,” rated on a 7-point Likert scale ranging from 1 (Strongly disagree) to 7 (Strongly agree). To facilitate analysis, responses were recoded into a binary variable. Responses of 5 (Slightly agree), 6 (Agree), or 7 (Strongly agree) were coded as 1, indicating perceived social support. Responses from 1 to 4 (ranging from Strongly disagree to Neutral) were coded as 0, indicating low or uncertain support. Missing responses were retained as a distinct category for descriptive purposes but were excluded from inferential analyses.
2.3.10. Sociodemographic Covariates
Participants self-reported demographic characteristics, including age (categorized as 18–22, 23–25, 26–30, or 31+ years), sex/gender identity (male, female, or other), and degree level (undergraduate, graduate, or non-degree). Race/ethnicity was restricted to students who identified as Arab American or Arab/Middle Eastern. These variables were included as covariates in multivariable models to adjust for demographic variation in mental health outcomes and digital service utilization. Participants responded to the question “Are you an international student?” with binary response options (1 = Yes, 0 = No). This variable was used to distinguish Arab American students from Arab/Middle Eastern international students in all analyses. Missing responses were excluded from the final analytic sample.
2.4. Statistical Analysis
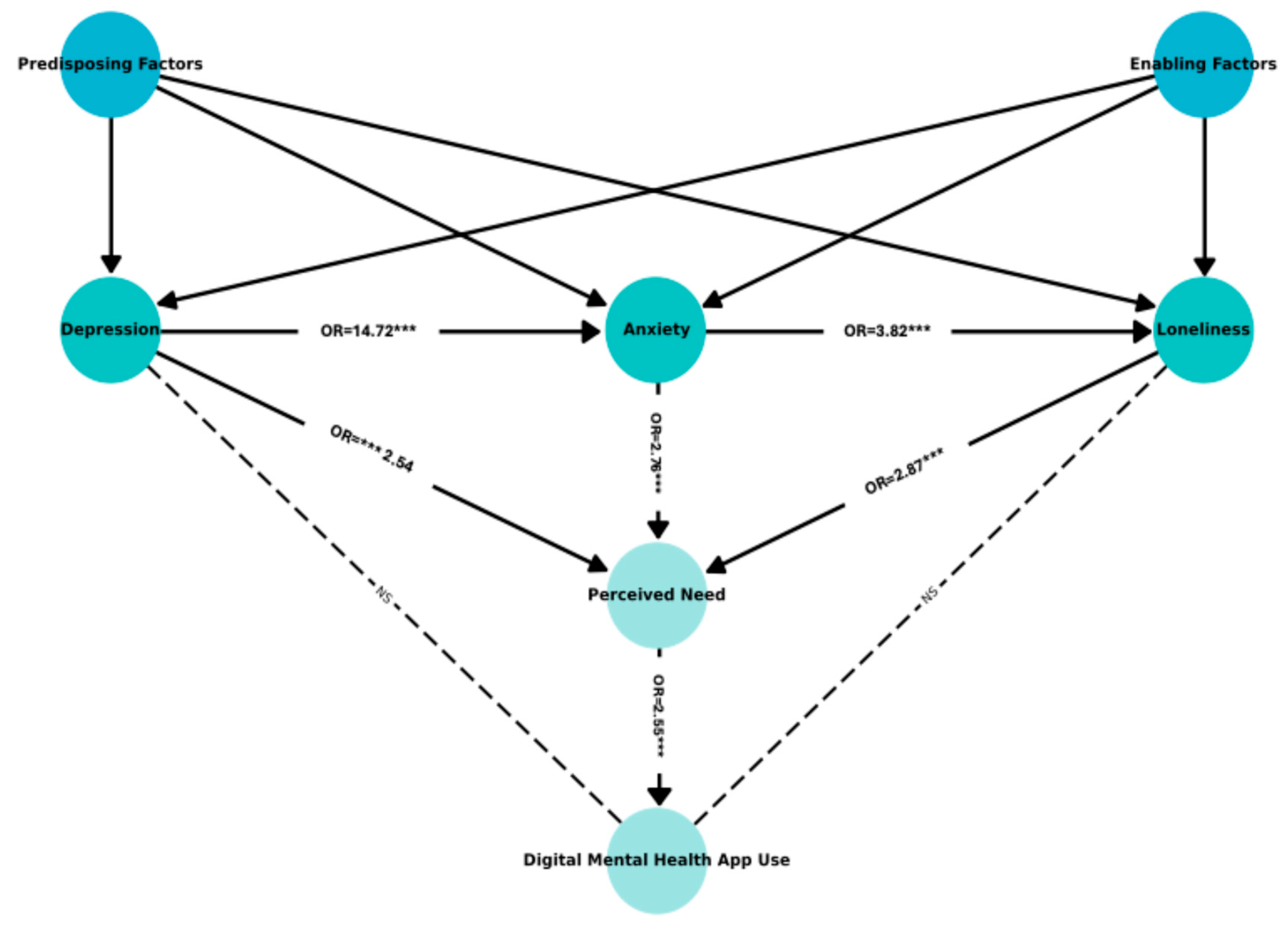
All analyses were conducted using Stata version 18.5. Descriptive analyses were conducted to compare the prevalence of depression, anxiety, and loneliness between Arab American and AME international college students during the post-COVID-19 recovery period (academic years 2022–2023 and 2023–2024). Logistic regression analyses were conducted to examine the bidirectional associations between loneliness and both depression and anxiety, adjusting for a comprehensive set of covariates. The assumptions of the logistic regression analyses (including linearity of the logit, multicollinearity, and influential outliers were tested) and no violations were detected. To examine the relationship between loneliness, perceived need, and the use of DMH services, weighted logistic regression analysis was used. To further contextualize these relationships within a comprehensive framework, we conducted Generalized Structural Equation Modeling (GSEM) to test the full conceptual model (
Figure 2). Model fit was evaluated using McFadden’s pseudo R
2, derived from the log pseudolikelihood values, consistent with prior applications of GSEM in clinical research [
34].
3. Results
3.1. Sample Characteristics
The study sample included 3249 Arab/Middle Eastern students enrolled at U.S. colleges and universities. Of these, 81.9% identified as Arab American (
n = 2662) and 18.1% as Arab/Middle Eastern international students (
n = 587).
Table 1 presents the demographic and enabling characteristics of these two groups. Gender and academic level distributions differed between groups. Arab American students were predominantly female, younger (67% aged 18–22), and mostly undergrads (74%). In contrast, AME international students were more evenly distributed across age groups, included a higher proportion of males (48%), and were primarily graduate students (59%).
With respect to enabling factors, approximately 71% of Arab Americans and 69% of international students reported having insurance coverage. Awareness of campus services was reported by 59% and 57%, respectively, while perceptions of social support were somewhat higher among Arab Americans (75%) than international students (65%). Beliefs about treatment efficacy were broadly similar across groups, with a considerable proportion of both groups indicating “unknown”.
Comparative analyses of included vs. excluded students were also conducted during revision (
Appendix A Table A1), showing systematic differences in missingness that may affect generalizability.
3.2. Prevalence Comparisons by Group
The analyses in this section address Hypothesis 1, which compared Arab American and AME international students. Hypotheses 2 and 3 were examined using the full Arab/Middle Eastern sample without separating by group.
3.2.1. Depression, Anxiety, and Loneliness
Descriptive analyses were conducted to compare the prevalence of depression, anxiety, and loneliness between Arab American and AME international college students during the post-COVID-19 recovery period (academic years 2022–2023 and 2023–2024). As shown in
Table 1, 44.33% of Arab American students reported symptoms of depression, compared to 40.89% of AME international students, indicating a slightly higher prevalence among Arab Americans. Similarly, anxiety symptoms were more common among Arab American students (40.01%) than AME international students (36.97%). In contrast, feelings of loneliness were nearly identical between the two groups, with 56.20% of Arab American and 56.90% of AME international students reporting loneliness.
3.2.2. Correlates of Depression and Anxiety
As shown in
Table 2, loneliness was significantly associated with increased odds of both depression and anxiety symptoms. In the fully adjusted model, students who reported loneliness had 2.19 times higher odds of depression (OR = 2.19, 95% CI: 1.66–2.88,
p < 0.001) and 1.99 times higher odds of anxiety (OR = 1.99, 95% CI: 1.49–2.65,
p < 0.001) compared to those who did not report loneliness.
Conversely, symptoms of depression were also associated with higher odds of reporting loneliness (OR = 2.16, 95% CI: 1.65–2.84, p < 0.001), as were symptoms of anxiety (OR = 1.97, 95% CI: 1.49–2.60, p < 0.001), supporting the hypothesized bidirectional relationship. In addition, the models demonstrated strong comorbidity between depression and anxiety: students with anxiety had 12.00 times greater odds of reporting depression (OR = 12.00, 95% CI: 9.06–15.91, p < 0.001), while those with depression had 12.07 times greater odds of reporting anxiety (OR = 12.07, 95% CI: 9.12–15.97, p < 0.001).
3.2.3. Loneliness, Perceived Need, and Digital Mental Health Utilization
The path analysis results (
Figure 3 and
Appendix A Table A2) confirmed the conceptual structure in
Figure 2 i.e., depression (β = 0.93, OR = 2.54,
p < 0.001), anxiety (β = 1.02, OR = 2.77,
p < 0.001), and loneliness (β = 1.05, OR = 2.86,
p < 0.001) were all significant predictors of perceived need. Perceived need significantly predicted DMH use (β = 0.94, OR = 2.56,
p < 0.001). However, the direct path from loneliness to DMH use was not statistically significant (β = 0.12, OR = 1.13,
p = 0.685). An interaction term testing the moderating effect of loneliness on the relationship between perceived need and DMH use (loneliness × perceived need) was also non-significant (β = −0.29, OR = 0.75,
p = 0.381), suggesting that loneliness does not significantly moderate this association.
4. Discussion
The hypothesis that AME international students would report higher rates of mental health concerns was not supported. Instead, Arab American students reported slightly higher levels of depression and anxiety, while loneliness was similar between the two groups. These modest differences may reflect the unique sociocultural and structural stressors that Arab American students face, such as racial discrimination, acculturative pressures, and systemic marginalization within U.S. educational settings [
35,
36]. In fact, these results challenge the common assumption that international students are always more vulnerable to psychological distress simply because they are adapting to a new culture and living away from family support.
Several factors may explain these findings. Arab American students often experience ongoing minority stress, including racism, Islamophobia, and cultural marginalization, which can negatively impact mental health [
37,
38]. Unlike international students, who may see their time in the U.S. as temporary, Arab Americans often navigate these systemic challenges as part of their long-term daily lives. Unlike international students, who may see their time in the U.S. as temporary, Arab Americans often navigate these systemic challenges as part of their long-term daily lives. These cultural stressors were not directly measured in this study, but prior research suggests they are likely important contributors to Arab American students’ elevated rates of depression and anxiety. Future research should incorporate direct measures of minority stress and acculturative pressures to better explain these group differences. It’s also possible that AME international students represent a self-selected group with stronger coping skills, higher resilience, and greater motivation qualities that may help them manage emotional distress more effectively. Additionally, they may view their challenges as part of a short-term academic journey, which could reduce the overall emotional burden [
39].
Differences in how students disclose their symptoms could also play a role. Arab American students may feel more comfortable acknowledging and reporting psychological distress, while international students might be more likely to downplay or withhold these experiences because of cultural norms or lower mental health literacy. In addition, international students often have access to campus resources and support services specifically designed for them, such as international student advisors and culturally tailored programs. These supports may help reduce some of the psychological challenges they face during their studies. Overall, these findings suggest that simply being an international student or a U.S. citizen does not determine vulnerability to mental health challenges. Instead, factors such as minority stress, discrimination, and access to culturally responsive support services may play a much larger role in shaping mental health outcomes for Arab-identifying students in the U.S.
To further explore group-level differences, we conducted multivariable regression analyses comparing depression and anxiety outcomes among AME international students and Arab American students. After adjusting for sociodemographic characteristics, beliefs about treatment effectiveness, and factors related to access, we found no statistically significant differences between the two groups. This suggests that the initial differences in prevalence might be explained more by underlying structural or individual factors rather than ethnicity or international status alone. Similar within-heritage differences have also been observed in other student populations. Asian American students, for example, have been shown to face greater exposure to model minority stereotypes and more adverse mental health effects compared to their international peers, highlighting how citizenship and sociocultural positioning can influence psychological outcomes even within the same ethnic group [
40].
However, the findings from the present study support Hypothesis 2, indicating a reciprocal relationship between loneliness and mental health conditions like depression and anxiety. Loneliness can both contribute to emotional distress and emerge as a response to it, creating a reinforcing cycle. This bidirectional connection is consistent with earlier research showing that loneliness can act both as a cause and a consequence of psychological distress [
41,
42], and it has also been observed in other student populations; for example, passively sensed data from U.S. college students found that loneliness was strongly associated with subsequent depressive symptoms, while sleep and physical activity served as protective factors [
43]. Although our findings align with this perspective, the cross-sectional design of this study limits causal interpretation. Longitudinal research is needed to clarify the temporal sequence and directionality of these associations. While our models accounted for many sociodemographic and perception-related factors, these results should still be interpreted with caution. Other unmeasured influences, such as financial strain, chronic health problems, or stress related to immigration, may also play an important role in shaping mental health outcomes for this population [
35,
36,
44].
The SEM results showed no significant direct link between symptoms of depression and anxiety and the use of DMH services. Similarly, the direct path from loneliness to DMH use was not significant, suggesting that loneliness influences service utilization only indirectly through perceived need. This suggests that simply having symptoms isn’t enough to motivate students to seek help; what matters more is whether they recognize and acknowledge a need for care. This mediating role of perceived need aligns with previous research highlighting its crucial role in mental health service use [
26,
45,
46]. Evidence from non-U.S. samples reinforces this pattern; for instance, Chinese residents during COVID-19 who reported higher loneliness also reported greater perceived mental health need and higher service use [
47]. Similarly, research on international students in the U.S. during the pandemic found that experiences of discrimination were closely tied to loneliness, anxiety, and depressive symptoms, underscoring the vulnerabilities of culturally marginalized groups [
8].
Importantly, the gap we observed between experiencing symptoms and actually using DMH services points to ongoing access barriers, which may be especially challenging for AME students. Cultural stigma, limited awareness of available services, and skepticism about the usefulness of digital tools have all been identified as common obstacles for these populations [
22,
48]. Our findings also align with prior research showing that engagement with digital mental health (DMH) interventions is shaped by a range of psychosocial and perceptual factors. For example, Borghouts et al. (2021) [
26] identified stigma, low digital literacy, and doubts about usefulness as common barriers to engagement across DMH platforms. These themes were reflected in our data, particularly among AME students who reported limited perceived need and low uptake of DMH services despite experiencing significant psychological distress [
26]. These findings highlight the importance of culturally responsive strategies that not only reduce stigma but also help students see digital mental health services as relevant, trustworthy, and accessible.
5. Limitations
This study has several limitations that should be acknowledged. First, because the study is based on cross-sectional data, we cannot make causal inferences about the relationships between variables. While we observed associations between loneliness, depression, and anxiety, these findings do not establish the temporal direction of effects. Longitudinal studies are needed to confirm the sequence and potential causality of these relationships.
Second, although the Healthy Minds Study provides a large and diverse dataset, this analysis was limited to data from two academic years (2022–2023 and 2023–2024). This is because key measures, including loneliness and DMH service use, were part of optional modules that institutions could choose whether to include. As a result, not all institutions administered these questions, and students at those schools were excluded from the analyses. This may have introduced selection bias, as our final sample may overrepresent students from institutions that opted to collect more detailed mental health data. Additionally, students who were excluded due to missing responses, particularly on treatment belief items, may differ systematically from those who completed the survey, potentially skewing our understanding of help-seeking attitudes in the broader AME student population. Our analysis also did not account for institutional variation in the availability and promotion of digital mental health services, which may affect utilization patterns and further limit the generalizability of these findings. Consequently, our findings might not fully reflect all students across participating institutions. Future research should encourage more consistent use of these modules to improve generalizability.
Although non-response weights were applied, the exclusion of institutions that did not administer optional modules may still bias findings. Comparative analyses of included vs. excluded students (
Appendix A,
Table A1) indicated systematic differences in missingness (e.g., on treatment beliefs and insurance coverage), which may introduce selection bias. This suggests that findings may not fully generalize to all Arab/Middle Eastern students across institutions. Future research should incorporate post-stratification or multiple imputation as formal sensitivity analyses to further test robustness.
Third, while survey weights were used to improve representativeness, the relatively small number of unweighted AME international students might have limited our ability to detect group-level differences.
Fourth, all data were self-reported, which raises the potential for recall errors or social desirability bias. Although the broader dataset includes other relevant factors, such as stigma, financial stress, prior mental health diagnoses, and details about campus-specific support systems, these variables were not included in this analysis. Their exclusion may have limited the range of explanatory variables and introduced residual confounding.
Finally, some constructs were assessed using single-item measures, such as perceived need for care and perceived social support, which may not fully capture the complexity of students’ attitudes, experiences, or motivations related to mental health help-seeking. Future studies should consider using validated multidimensional instruments and incorporating a broader set of psychosocial predictors to more fully capture the factors shaping mental health and help-seeking among AME students.
6. Implications
A central finding from this study is that students’ perceived need for support plays a more crucial role in their use of DMH services than simply experiencing symptoms. This underscores the importance of increasing mental health awareness, reducing stigma, and making campus resources more visible and accessible. Helping students recognize when they need support is a critical first step toward engaging with mental health services.
The findings from this study offer several meaningful insights for mental health service planning and campus policies aimed at supporting AME students in U.S. higher education. Importantly, the results suggest that citizenship status alone does not define vulnerability to mental health challenges. Instead, tailored interventions should address the unique psychosocial stressors experienced by both AME international and Arab American students. The bidirectional relationship between loneliness and internalizing symptoms like depression and anxiety highlights the need for preventive strategies. Fostering more socially connected and inclusive campus environments can help reduce feelings of isolation, ease psychological distress, and ultimately promote better mental health outcomes.
To be truly effective, mental health services must move beyond a one-size-fits-all approach. Colleges and universities should implement strategies at multiple levels: individual, institutional, and cultural. This might include developing culturally tailored digital tools, incorporating routine mental health screenings into student health services, and training staff to deliver care that is culturally responsive and inclusive. Key factors such as personalization, ease of navigation, and human support have been shown to enhance engagement with digital mental health interventions [
26]. These insights underscore the need for user-centered and culturally responsive design when scaling up DMH services for AME student populations.
Moreover, universities need to address broader structural issues affecting AME students, such as anti-Arab racism, Islamophobia, and systemic marginalization. These factors can harm students’ well-being and create significant barriers to care. Building trust through culturally humble and respectful service delivery is crucial to making mental health support not only accessible but also effective and equitable for AME student populations [
49,
50,
51].
Future research should adopt longitudinal designs to clarify causal and bidirectional relationships between loneliness, mental health symptoms, perceived need, and DMH service use. Incorporating qualitative or mixed-methods approaches could also help uncover cultural attitudes, stigma, and contextual barriers that shape help-seeking behaviors. Studies should further explore campus-level and structural factors, including culturally responsive services and institutional support, and examine less-studied areas like acculturation stress. To improve generalizability and equity, national datasets should ensure adequate representation of AME students and consistently include relevant variables across survey waves.
7. Conclusions
This study provides timely insight into the mental health experiences of Arab American and AME international college students during the post-COVID-19 recovery period. Contrary to common assumptions, Arab American students reported slightly higher levels of depression and anxiety than their international peers, although feelings of loneliness were similar across both groups. Multivariable analyses revealed a strong two-way relationship between loneliness and mental health symptoms, highlighting the critical role of social isolation in shaping mental health outcomes.
One of the most important findings was the role of perceived need, which emerged as a key factor connecting mental health symptoms to DMH service use. This highlights the importance of mental health literacy and students’ ability to recognize their own distress when deciding to seek support. While loneliness itself was not directly linked to DMH service use, its strong connection to depression, anxiety, and perceived need suggests that targeting social connection may indirectly increase engagement with services.
Overall, these findings underscore the importance of developing culturally responsive, campus-based mental health strategies that strengthen social support and enhance access to digital resources. Addressing the unique psychosocial challenges faced by Arab-identifying students, particularly through inclusive policies and tailored programs, may help reduce disparities in mental health care and promote more equitable outcomes across diverse student populations.
Author Contributions
Conceptualization, F.M.A.; methodology, F.M.A.; software, F.M.A. and D.J.R.; validation, F.M.A., C.E.J., D.J.R. and S.M.K.; formal analysis, F.M.A.; investigation, F.M.A.; resources, F.M.A.; data curation, F.M.A.; writing—original draft preparation, F.M.A.; writing—review and editing, F.M.A., C.E.J., D.J.R., S.M.K. and D.A.; visualization, F.M.A.; supervision, C.E.J., D.J.R., S.M.K. and D.A.; project administration, F.M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The Institutional Review Board at University of Louisville approved the study by exempting it with the approval number 25.0308 (approval date 8 May 2025). The study was exempt because it is a secondary, deidentified, publicly available data.
Informed Consent Statement
Patient consent was waived as secondary deidentified data was already publicly available upon request.
Data Availability Statement
Data is available upon reasonable request to authors pending approval from HMS.
Acknowledgments
The authors have reviewed and edited the output and take full responsibility for the content of this publication.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Table A1.
Descriptive Characteristics of Included and Excluded Arab/Middle Eastern (AME) Student Respondents.
Table A1.
Descriptive Characteristics of Included and Excluded Arab/Middle Eastern (AME) Student Respondents.
| | | Included Sample n = 3249 | Excluded Sample n = 586 |
|---|
| Variable | Category | Frequency | Percent (%) | Frequency | Percent (%) |
|---|
| Utilized Digital Mental Health Service | | |
| | Yes | 324 | 9.97 | | |
| | No | 2925 | 90.03 | | |
| Depression Status | | |
| | Yes | 1420 | 43.71 | | |
| | No | 1829 | 56.29 | | |
| Anxiety Status | | |
| | Yes | 1282 | 39.45 | | |
| | No | 1967 | 60.55 | | |
| Loneliness | | |
| | Yes | 1830 | 56.31 | | |
| | No | 1419 | 43.69 | | |
| Perceived Need | | |
| | Yes | 2191 | 67.42 | | |
| | No | 1058 | 32.58 | | |
| Race | | |
| | Arab American | 2662 | 81.93 | 441 | 75.26 |
| | AME International | 587 | 18.07 | 124 | 21.16 |
| | Unknown | 0 | 0.00 | 21 | 3.58 |
| Age Group | | |
| | 18–22 Years | 1973 | 60.73 | 383 | 65.36 |
| | 23–25 Years | 457 | 14.07 | 58 | 9.9 |
| | 26–30 Years | 446 | 13.73 | 69 | 11.77 |
| | 31+ Years | 373 | 11.48 | 76 | 12.97 |
| Gender | | |
| | Male | 979 | 30.14 | 204 | 34.81 |
| | Female | 2082 | 64.08 | 346 | 59.04 |
| | Other | 166 | 5.11 | 26 | 4.44 |
| | Unknown | 22 | 0.68 | 10 | 1.71 |
| Degree Level | | |
| | Undergraduate | 2208 | 67.96 | 322 | 54.95 |
| | Graduate | 905 | 27.85 | 118 | 20.14 |
| | Non-degree | 40 | 1.23 | 16 | 2.73 |
| | Unknown | 96 | 2.95 | 130 | 22.18 |
| Medication Helps | | |
| | Helpful | 1113 | 34.26 | 16 | 2.73 |
| | Not helpful | 425 | 13.08 | 5 | 0.85 |
| | Unknown | 1711 | 52.66 | 565 | 96.42 |
| Therapy Helps | | |
| | Helpful | 1435 | 44.15 | 18 | 3.07 |
| | Not helpful | 107 | 3.29 | 2 | 0.34 |
| | Unknown | 1707 | 52.56 | 566 | 96.59 |
| Insurance Coverage | | |
| | Yes | 2303 | 70.89 | 40 | 6.83 |
| | No | 117 | 3.6 | 2 | 0.34 |
| | Unknown | 829 | 25.52 | 544 | 92.83 |
| Awareness of Services | | |
| | Aware | 694 | 21.36 | 525 | 89.59 |
| | Not Aware | 1901 | 58.52 | 20 | 3.41 |
| | Unknown | 654 | 20.13 | 41 | 7 |
| Perceived Social Support | | |
| | Supportive | 2367 | 72.88 | 294 | 50.17 |
| | Non-supportive | 876 | 26.96 | 100 | 17.06 |
| | Unknown | 6 | 0.18 | 192 | 32.76 |
Table A2.
Summary of Significant Predictors from SEM Analysis.
Table A2.
Summary of Significant Predictors from SEM Analysis.
| Outcome | Predictor | Direction | Significance | Significance |
|---|
| Depression Status | Female gender (ref: Male) | Positive | p < 0.001 | *** |
| | Other gender identity (ref: Male) | Positive | p < 0.001 | *** |
| | Age 23–25 (ref: 18–22Y) | Positive | p = 0.092 | * |
| | Age 31+ (ref: 18–22Y) | Negative | p = 0.006 | ** |
| | Undergraduate (ref: Graduate) | Positive | p = 0.085 | * |
| | Awareness of services (ref: No) | Negative | p < 0.001 | *** |
| | Perceived social support: Yes (ref: Not Supportive) | Negative | p < 0.001 | *** |
| Anxiety Status | Depression Status | Positive | p < 0.001 | *** |
| | Female gender (ref: Male) | Positive | p < 0.001 | *** |
| | Other gender identity (ref: Male) | Positive | p < 0.001 | *** |
| | Age 31+ (ref: 18–22Y) | Negative | p = 0.018 | ** |
| | Non-degree (ref: Graduate) | Negative | p < 0.001 | *** |
| | Awareness of services (ref: No) | Negative | p < 0.001 | *** |
| | Perceived social support: Yes (ref: Not Supportive) | Negative | p < 0.001 | *** |
| Loneliness | Anxiety Status | Positive | p < 0.001 | *** |
| | Other gender identity (ref: Male) | Positive | p = 0.001 | ** |
| | Age 23–25 (ref: 18–22Y) | Negative | p = 0.084 | * |
| | Age 31+ (ref: 18–22Y) | Negative | p = 0.000 | *** |
| | Perceived social support: Yes (ref: Not Supportive) | Negative | p < 0.001 | *** |
| Perceived Need | Depression Status | Positive | p < 0.001 | *** |
| | Anxiety Status | Positive | p < 0.001 | *** |
| | Loneliness | Positive | p < 0.001 | *** |
| | Female gender (ref: Male) | Positive | p = 0.000 | *** |
| | Other gender identity (ref: Male) | Positive | p = 0.000 | *** |
| | International student status: Yes | Positive | p < 0.001 | *** |
| | Undergraduate (ref: Graduate) | Negative | p = 0.001 | *** |
| | Therapy is helpful (ref: Not helpful | Positive | p = 0.001 | *** |
| | Awareness of services (ref: No) | Positive | p = 0.041 | ** |
| Digital MH Use | Anxiety Status | Positive | p = 0.069 | * |
| | Perceived Need | Positive | p = 0.000 | *** |
| | Female gender (ref: Male) | Positive | p = 0.000 | *** |
| | Other gender identity (ref: Male) | Positive | p = 0.045 | ** |
| | Age 23–25 (ref: 18–22Y) | Positive | p = 0.066 | * |
| | Age 31+ (ref: 18–22Y) | Positive | p = 0.067 | * |
References
- Belgium: Middle East and Refugees Debates with Mogherini, Stoltenberg, MEPs and MPs. Mena Report, 23 February 2016. Available online: https://go.gale.com/ps/i.do?p=AONE&sw=w&issn=22190112&v=2.1&it=r&id=GALE%7CA444097792&sid=googleScholar&linkaccess=fulltext (accessed on 26 June 2025).
- Institute of International Education, Open Doors Report on International Educational Exchange. 2023. Available online: https://opendoorsdata.org (accessed on 23 June 2025).
- Arab American Institute. National Arab American Demographics. 2023. Available online: https://www.aaiusa.org/demographics (accessed on 23 June 2025).
- Al-Krenawi, A.; Graham, J.R. Mental health help-seeking among Arab university students in Israel: Sociocultural and religious influences. Ment. Health Relig. Cult. 2011, 14, 117–127. [Google Scholar] [CrossRef]
- Amer, M.M.; Bagasra, A. Psychological research with muslim americans in the age of islamophobia: Trends, challenges, and recommendations. Am. Psychol. 2013, 68, 134–144. [Google Scholar] [CrossRef]
- El-Sayed, A.M.; Galea, S. The health of Arab-Americans living in the United States: A systematic review of the literature. BMC Public Health 2009, 9, 272. [Google Scholar] [CrossRef] [PubMed]
- Abuelezam, N.N.; El-Sayed, A.M.; Galea, S. The Health of Arab Americans in the United States: An Updated Comprehensive Literature Review. Front. Public Health 2018, 6, 262. [Google Scholar] [CrossRef] [PubMed]
- Maleku, A.; Kim, Y.K.; Kirsch, J.; Um, M.Y.; Haran, H.; Yu, M.; Moon, S.S. The hidden minority: Discrimination and mental health among international students in the US during the COVID-19 pandemic. Health Soc. Care Community 2022, 30, e2419–e2432. [Google Scholar] [CrossRef]
- Hutten, E.; Jongen, E.M.M.; Vos, A.E.C.C.; van den Hout, A.J.H.C.; van Lankveld, J.J.D.M. Loneliness and Mental Health: The Mediating Effect of Perceived Social Support. Int. J. Environ. Res. Public Health 2021, 18, 11963. [Google Scholar] [CrossRef]
- Poyrazli, S.; Lopez, M.D. An exploratory study of perceived discrimination and homesickness: A comparison of international students and American students. J. Psychol. 2007, 141, 263–280. [Google Scholar] [CrossRef]
- Horigian, V.E.; Schmidt, R.D.; Feaster, D.J. Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. J. Psychoact. Drugs 2021, 53, 1–9. [Google Scholar] [CrossRef]
- Cao, W.; Fang, Z.; Hou, G.; Han, M.; Xu, X.; Dong, J.; Zheng, J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020, 287, 112934. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.; Yuan, Y.; Wang, D. Mental health status and its influencing factors among college students during the epidemic of COVID-19. medRxiv 2020, 40, 171–176. [Google Scholar] [CrossRef]
- Huckins, J.F.; Dasilva, A.W.; Wang, W.; Hedlund, E.; Rogers, C.; Nepal, S.K.; Wu, J.; Obuchi, M.; I Murphy, E.; Meyer, M.L.; et al. Mental health and behavior of college students during the early phases of the COVID-19 pandemic: Longitudinal smartphone and ecological momentary assessment study. J. Med. Internet Res. 2020, 22, e20185. [Google Scholar] [CrossRef]
- Ying, Z.; Kondo, A.; Piao, M. Article Mental Health Challenges Among Chinese International Students During COVID-19: A Systematic Review and Meta-Analysis of Depression and Anxiety. J. Int. Stud. 2025, 15, 2166–3750. [Google Scholar] [CrossRef]
- Rosenthal, D.A.; Russell, J.; Thomson, G. The health and wellbeing of international students at an Australian university. High. Educ. 2008, 55, 51–67. [Google Scholar] [CrossRef]
- Wawera, A.S.; McCamley, A. Loneliness among international students in the UK. J. Furth. High. Educ. 2020, 44, 1262–1274. [Google Scholar] [CrossRef]
- Killgore, W.D.S.; Cloonan, S.A.; Taylor, E.C.; Dailey, N.S. Loneliness: A signature mental health concern in the era of COVID-19. Psychiatry Res. 2020, 290, 113117. [Google Scholar] [CrossRef]
- Sutin, A.R.; Luchetti, M.; Terracciano, A. Has loneliness increased during COVID-19? J. Res. Pers. 2020, 89, 104036. [Google Scholar] [CrossRef]
- Murthy, V.H.; Chen, A.T. The Coronavirus Could Cause a Social Recession-The Atlantic. 2020. Available online: https://www.theatlantic.com/ideas/archive/2020/03/america-faces-social-recession/608548/ (accessed on 7 June 2025).
- Healthy Minds Network. Data for Researchers. Available online: https://healthymindsnetwork.org/data-for-researchers/ (accessed on 19 August 2019).
- Abuelezam, N.N.; Lipson, S.K.; Zhou, S.; Abelson, S.; Awad, G.H.; Eisenberg, D.; Galea, S. Mental Health Service Utilization Among Arab and Middle Eastern American College Students. J. Coll. Stud. Ment. Health 2023, 38, 634–647. [Google Scholar] [CrossRef]
- Healthy Minds Network. The Healthy Minds Study (HMS) Protocol 2021–2022. 2021. Available online: https://healthymindsnetwork.org/wp-content/uploads/2021/07/HMS-Protocol-2021-22-3.pdf (accessed on 4 April 2023).
- Andersen, R.M. Revisiting the Behavioral Model and Access to Medical Care: Does it Matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Mojtabai, R.; Olfson, M.; Sampson, N.A.; Jin, R.; Druss, B.; Wang, P.S.; Wells, K.B.; Pincus, H.A.; Kessler, R.C. Barriers to mental health treatment: Results from the National Comorbidity Survey Replication. Psychol. Med. 2011, 41, 1751–1761. [Google Scholar] [CrossRef]
- Borghouts, J.; Eikey, E.; Mark, G.; De Leon, C.; Schueller, S.M.; Schneider, M.; Stadnick, N.; Zheng, K.; Mukamel, D.; Sorkin, D.H. Barriers to and Facilitators of User Engagement with Digital Mental Health Interventions: Systematic Review. J. Med. Internet Res. 2021, 23, e24387. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, A.; Griffiths, K.M.; Christensen, H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010, 10, 113. [Google Scholar] [CrossRef]
- Zivin, K.; Eisenberg, D.; Gollust, S.E.; Golberstein, E. Persistence of mental health problems and needs in a college student population. J. Affect. Disord. 2009, 117, 180–185. [Google Scholar] [CrossRef]
- Babitsch, B.; Gohl, D.; von Lengerke, T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: A systematic review of studies from 1998–2011. GMS Psycho-Soc. Med. 2012, 9, Doc11. [Google Scholar]
- Kroenke, K. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Stockton, M.A.; Kraemer, J.; Oga, E.; Kimani, J.; Mbote, D.; Kemunto, C.; Njuguna, S.; Nyblade, L. Validation of a Brief Internalized Sex-work Stigma Scale among Female Sex Workers in Kenya. J. Sex. Res. 2023, 60, 146–152. [Google Scholar] [CrossRef]
- Hughes, M.E.; Waite, L.J.; Hawkley, L.C.; Cacioppo, J.T. A short scale for measuring loneliness in large surveys: Results from two population-based studies. Res. Aging 2004, 26, 655–672. [Google Scholar] [CrossRef] [PubMed]
- Tzang, R.-F.; Chang, Y.-C. Generalized structural equation modeling: Symptom heterogeneity in attention-deficit/hyperactivity disorder leading to poor treatment efficacy. World J. Psychiatry 2022, 12, 787. [Google Scholar] [CrossRef]
- El-Refaay, S.M.; Kenny, C.; Weiss, S. Depression and Anxiety Among Arab Individuals in the United States: A Meta-analysis. J. Immigr. Minor. Health 2024, 27, 329–350. [Google Scholar] [CrossRef] [PubMed]
- Bas-Sarmiento, P.; Saucedo-Moreno, M.J.; Fernández-Gutiérrez, M.; Poza-Méndez, M. Mental Health in Immigrants Versus Native Population: A Systematic Review of the Literature. Arch. Psychiatr. Nurs. 2017, 31, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Awad, G.H. The impact of acculturation and religious identification on perceived discrimination for Arab/Middle Eastern Americans. Cultur. Divers. Ethn. Minor. Psychol. 2010, 16, 59–67. [Google Scholar] [CrossRef]
- Nadal, K.L.; Griffin, K.E.; Wong, Y.; Hamit, S.; Rasmus, M. The Impact of Racial Microaggressions on Mental Health: Counseling Implications for Clients of Color. J. Couns. Dev. 2014, 92, 57–66. [Google Scholar] [CrossRef]
- Lari, S.A.; Zumot, M.S.; Fredericks, S. Navigating mental health challenges in international university students: Adapting to life transitions. Front. Psychiatry 2025, 16, 1574953. [Google Scholar] [CrossRef]
- Li, C.; Hagedorn, L.S.; Cui, H. The model minority myth and Asian students’ mental health: A comparative analysis of Asian American and international students and the moderating role of citizenship status. Cult. Divers. Ethn. Minor. Psychol. 2025. [Google Scholar] [CrossRef]
- Mann, F.; Wang, J.; Pearce, E.; Ma, R.; Schlief, M.; Lloyd-Evans, B.; Ikhtabi, S.; Johnson, S. Loneliness and the onset of new mental health problems in the general population. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 2161–2178. [Google Scholar] [CrossRef] [PubMed]
- Mushtaq, R.; Shoib, S.; Shah, T.; Mushtaq, S.; Loneliness, R.B. Psychiatric Disorders and Physical Health? A Review on the Psychological Aspects of Loneliness. J. Clin. Diagn. Res. 2014, 8, WE01. [Google Scholar] [CrossRef]
- Qirtas, M.M.; Zafeiridi, E.; White, E.B.; Pesch, D. The relationship between loneliness and depression among college students: Mining data derived from passive sensing. Digital Health 2023, 9, 1–15. [Google Scholar] [CrossRef]
- Pampati, S.; Alattar, Z.; Cordoba, E.; Tariq, M.; De Leon, C.M. Mental health outcomes among Arab refugees, immigrants, and U.S. born Arab Americans in Southeast Michigan: A cross-sectional study. BMC Psychiatry 2018, 18, 379. [Google Scholar] [CrossRef]
- Cadigan, J.M.; Lee, C.M.; Larimer, M.E. Young Adult Mental Health: A Prospective Examination of Service Utilization, Perceived Unmet Service Needs, Attitudes, and Barriers to Service Use. Prev. Sci. 2019, 20, 366–376. [Google Scholar] [CrossRef] [PubMed]
- Gbollie, E.F.; Bantjes, J.; Jarvis, L.; Swandevelder, S.; du Plessis, J.; Shadwell, R.; Davids, C.; Gerber, R.; Holland, N.; Hunt, X. Intention to use digital mental health solutions: A cross-sectional survey of university students attitudes and perceptions toward online therapy, mental health apps, and chatbots. Digit. Health 2023, 9, 20552076231216560. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Li, W.-T.; Zhong, B.-L. Feelings of loneliness and mental health needs and services utilization among Chinese residents during the COVID-19 epidemic. Glob. Health 2021, 17, 51. [Google Scholar] [CrossRef] [PubMed]
- Elshamy, F.; Hamadeh, A.; Billings, J.; Alyafei, A. Mental illness and help-seeking behaviours among Middle Eastern cultures: A systematic review and meta-synthesis of qualitative data. PLoS ONE 2023, 18, e0293525. [Google Scholar] [CrossRef] [PubMed]
- Naser, S. Addressing the invisibility of Arab American issues in higher education. Counseling Today, 2021. Available online: https://ctarchive.counseling.org/2021/02/addressing-the-invisibility-of-arab-american-issues-in-higher-education/ (accessed on 26 June 2025).
- Sebti, L.; Baroudi, F. An Exploration of Arab International Students’ Campus Engagement Experiences. J. Comp. Int. High. Educ. 2024, 16, 88–105. [Google Scholar] [CrossRef]
- Naser, S. Counseling Arab-American Students: Are Your Campus Mental Health Professionals Prepared to Support Students from a Variety of Backgrounds? Liberal Education, 2020. Available online: https://www.aacu.org/liberaleducation/articles/counseling-arab-american-students-are-your-campus-mental-health-professionals-prepared-to-support-students-from-a-variety-of-backgrounds (accessed on 26 June 2025).
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).