Effectiveness of Arm Swing Exercise on Comprehensive Health Outcomes: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods and Analysis
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion Criteria
2.4. Outcome Measures
2.5. Articles Selection and Data Extraction
2.5.1. Study Selection Process
2.5.2. Data Extraction
2.6. Quality and Risk of Bias Assessment
2.7. Statistical Analysis
3. Results
3.1. Articles Selection and Characteristics
3.2. Quality and Risk of Bias Assessment
3.3. Data Synthesis of Outcome Measures
3.3.1. Meta-Analysis
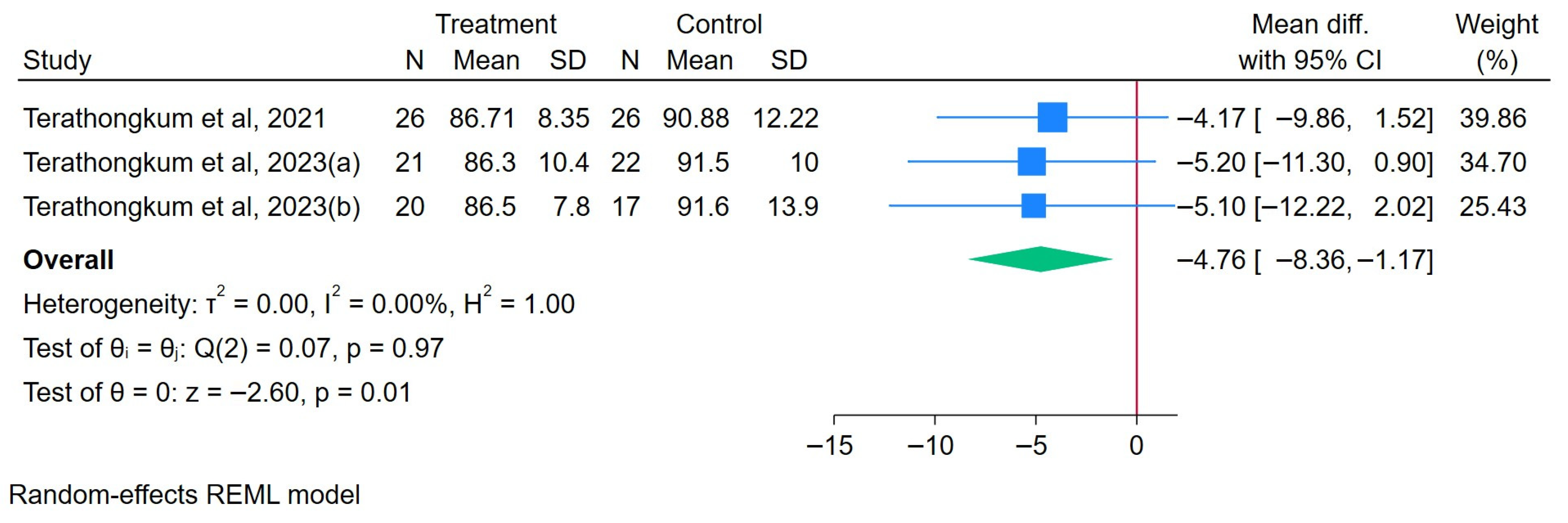
3.3.2. Effects of Arm Swing Exercise on WC
3.3.3. Effects of Arm Swing Exercise on HbA1C
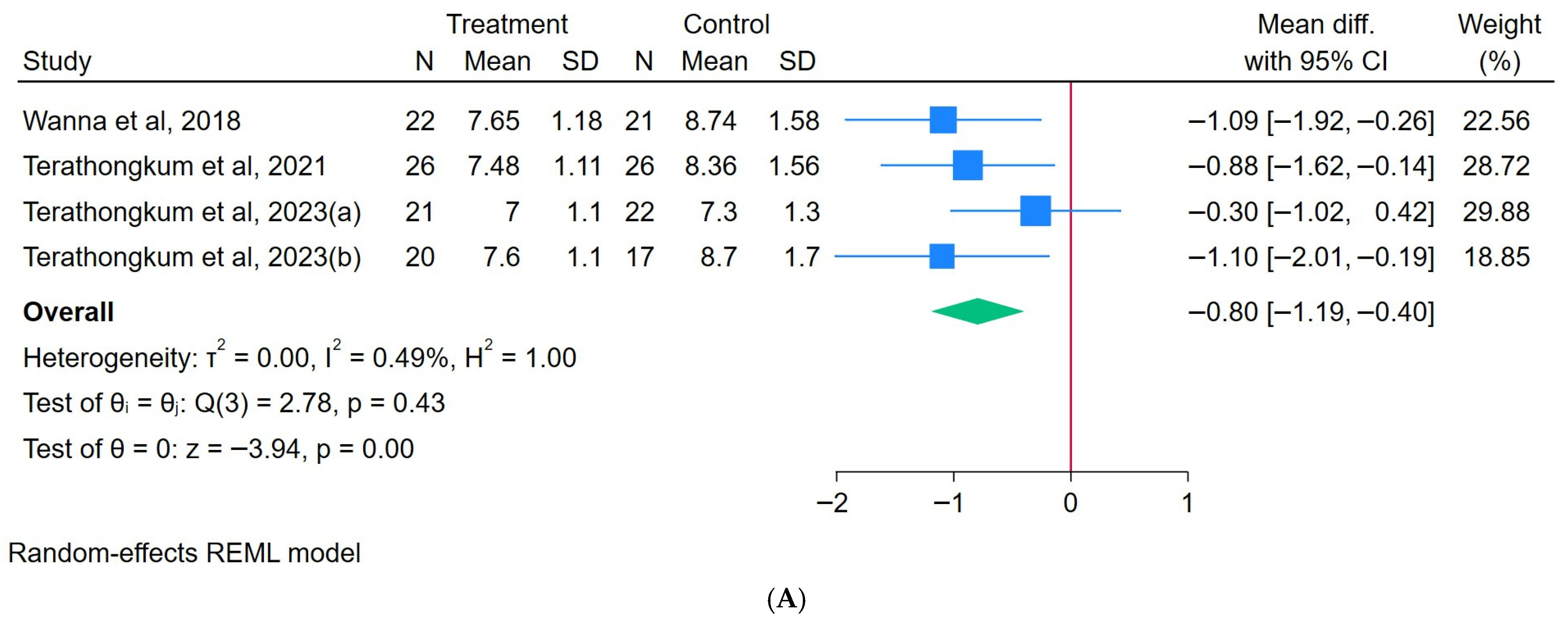
3.3.4. Effects of Arm Swing Exercise on FBG
3.3.5. Effects of Arm Swing Exercise on HDL-C
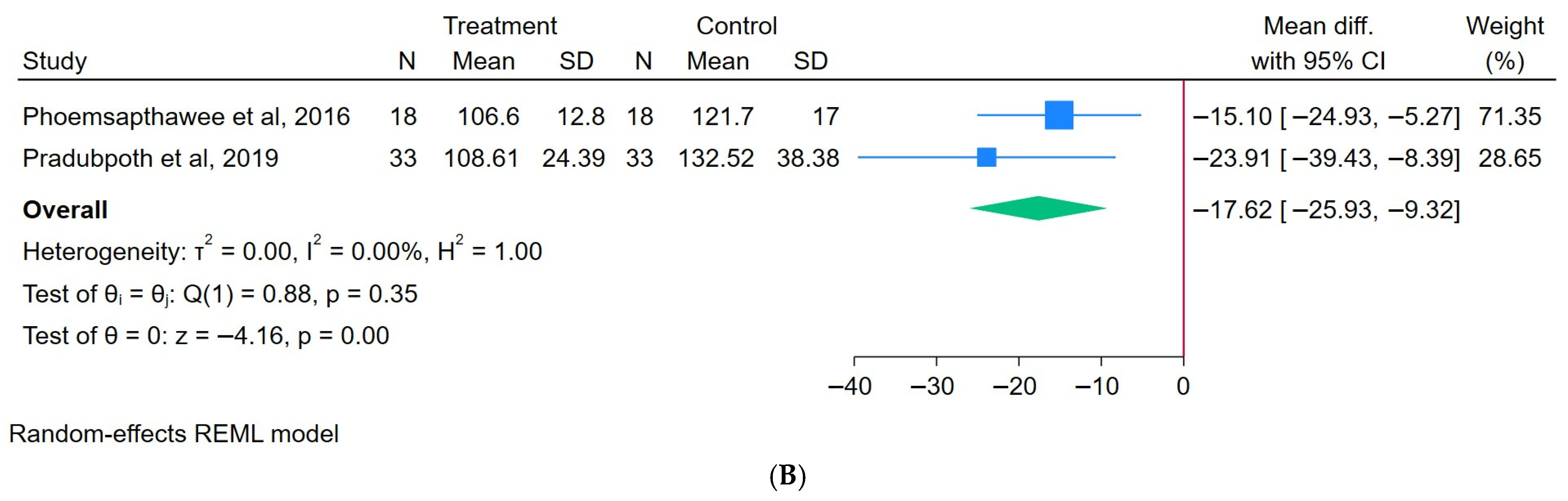
3.3.6. Effects of Arm Swing Exercise on SBP
3.3.7. Effects of Arm Swing Exercise on DBP
4. Discussion
4.1. Effects on Waist Circumference
4.2. Effects on Hemoglobin A1c and Fasting Blood Glucose
4.3. Effects on Cardiovascular Risk Factors
4.4. Comparative Effectiveness of ASE Across Health Outcomes in Meta-Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Hung, S.T.; Cheng, Y.C.; Wu, C.C.; Su, C.H. Examining physical wellness as the fundamental element for achieving holistic well-being in older persons: Review of literature and practical application in daily life. J. Multidiscip. Healthc. 2023, 16, 1889–1904. [Google Scholar] [CrossRef]
- Rice, J.; Li, L.C.; Davis, J.C.; Pahor, M.; Madden, K.; Wei, N.; Wong, H.; Skelton, D.A.; McCormick, S.; Falck, R.S.; et al. Supporting physical activity for mobility in older adults with mobility limitations (SuPA Mobility): Study protocol for a randomized controlled trial. Trials 2023, 24, 769. [Google Scholar] [CrossRef]
- Bjelica, B.; Aksović, N.; Bubanj, S.; Zelenović, M.; Stanković, M.; Pajović, L.; Čaprić, I.; Radenković, O.; Kahrović, I.; Murić, B.; et al. Effects of physical activity on patients with diabetes type 2: A systematic review. Balneo PRM Res. J. 2024, 15, 719. [Google Scholar] [CrossRef]
- Amin, M.; Kerr, D.; Atiase, Y.; Aldwikat, R.K.; Driscoll, A. Effect of physical activity on metabolic syndrome markers in adults with type 2 diabetes: A systematic review and meta-analysis. Sports 2023, 11, 101. [Google Scholar] [CrossRef]
- Valenzuela, P.L.; Ruilope, L.M.; Santos-Lozano, A.; Wilhelm, M.; Kränkel, N.; Fiuza-Luces, C.; Lucia, A. Exercise benefits in cardiovascular diseases: From mechanisms to clinical implementation. Eur. Heart J. 2023, 44, 1874–1889. [Google Scholar] [CrossRef]
- Islam, S.M.; Fardousi, A.; Sizear, M.I.; Rabbani, M.G.; Islam, R.; Saif-Ur-Rahman, K.M. Effect of leisure-time physical activity on blood pressure in people with hypertension: A systematic review and meta-analysis. Sci. Rep. 2023, 13, 10639. [Google Scholar] [CrossRef] [PubMed]
- Li, S.; Wang, P.; Cai, Z.; Jiang, W.; Xin, X.; Wang, X.; Zhou, X. Correlates of physical activity levels, muscle strength, working memory, and cognitive function in older adults. Front. Aging Neurosci. 2023, 15, 1283864. [Google Scholar] [CrossRef]
- Xiao, Z.; Cruz, M.; Hojo, E.; Eungpinichpong, W.; Wang, X.; Xiao, L.; Chatchawan, U.; Hu, Y.; Roberts, N.; Ummarino, D. The benefits of Shuai Shou Gong (SSG) demonstrated in a randomized control trial (RCT) study of older adults in two communities in Thailand. PLoS ONE 2023, 18, e0282405. [Google Scholar] [CrossRef] [PubMed]
- Model Learning Center Project for Waist Reduction; Health Promotion Section for Healthy Lifestyles; Thai Health Promotion Foundation (ThaiHealth). Manual for Reducing Waistline and Preventing Diseases. Available online: https://chomcharoen.go.th/index/add_file/G6JN3BzThu103453.pdf (accessed on 25 June 2025).
- Rodríguez-Millán, T.; Sanz-Morère, C.B.; Cherubini, A.; Urrutia, R.; Oliveira Barroso, F.; Pons, J.L.; Tornero, J. Effects of arm swing in lower limb muscle activation and coordination during treadmill walking. Appl. Sci. 2025, 15, 192. [Google Scholar] [CrossRef]
- Kovács, B.; Csala, D.; Sebestyén, Ö.; Matlák, J.; Groszmann, Á.; Tihanyi, J.; Petridis, L. Arm swing during vertical jumps does not increase EMG activity of the lower limb muscles. Phys. Act. Health 2023, 7, 132–142. [Google Scholar] [CrossRef]
- Koo, Y.J.; Ogihara, N.; Koo, S. Active arm swing during running improves rotational stability of the upper body and metabolic energy efficiency. Ann. Biomed. Eng. 2025, 53, 1003–1013. [Google Scholar] [CrossRef]
- Chompoopan, W.; Kuhirunyaratn, P. Effect of arm swing exercises on cardiovascular response and balance of older women. Int. J. GEOMATE 2018, 15, 112–117. [Google Scholar] [CrossRef]
- Kimura, M.; Ruller, S.; Frank, C.; Bell, A.; Jacobson, M.; Pardo, J.P.; Ramsey, T.; Sobala, M.; Fung, C.; Kobewka, D. Incidence, morbidity, and mortality from falls in skilled nursing facilities: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2023, 24, 1690–1699.e6. [Google Scholar] [CrossRef]
- Dent, E.; Dalla Via, J.; Bozanich, T.; Hoogendijk, E.O.; Gebre, A.K.; Smith, C.; Zhu, K.; Prince, R.L.; Lewis, J.R.; Sim, M. Frailty increases the long-term risk for fall and fracture-related hospitalizations and all-cause mortality in community-dwelling older women. J. Bone Miner. Res. 2024, 39, 222–230. [Google Scholar] [CrossRef]
- Ambrogetti, R. The effects of exercise on coronary collateral circulation: A review. Cureus 2022, 14, e32732. [Google Scholar] [CrossRef]
- Prasertsri, P.; Kaewaram, J.; Naravoratham, K.; Trongtosak, P. Influence of arm swing exercise training on blood pressure regulation of cardiac autonomic function and cardiovascular risks in hypertensive elderly subjects. J. Exerc. Physiol. Online 2018, 21, 162–167. [Google Scholar]
- Rao, C.R.; Chandrasekaran, B.; Ravishankar, N.; Rutebemberwa, E.; Okello, D. Physical activity interventions for glycaemic control in African adults: A systematic review and meta-analysis. Diabetes Metab. Syndr. 2022, 16, 102663. [Google Scholar] [CrossRef]
- Chen, J.; Luo, Q.; Su, Y.; Wang, J.; Fang, Z.; Luo, F. Effects of physical activity on the levels of remnant cholesterol: A population-based study. J. Cell Mol. Med. 2023, 28, e18062. [Google Scholar] [CrossRef]
- Barker, T.H.; Stone, J.C.; Sears, K.; Klugar, M.; Tufanaru, C.; Leonardi-Bee, J.; Aromataris, E.; Munn, Z. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid. Synth. 2023, 21, 494–506. [Google Scholar] [CrossRef]
- Barker, T.H.; Habibi, N.; Aromataris, E.; Stone, J.C.; Leonardi-Bee, J.; Sears, K.; Hasanoff, S.; Klugar, M.; Tufanaru, C.; Moola, S.; et al. The revised JBI critical appraisal tool for the assessment of risk of bias quasi-experimental studies. JBI Evid. Synth. 2024, 22, 378–388. [Google Scholar] [CrossRef]
- Prasertsri, P.; Singsanan, S.; Chonanant, C.; Boonla, O.; Trongtosak, P. Effects of arm swing exercise training on cardiac autonomic modulation, cardiovascular risk factors, and electrolytes in persons aged 60–80 years with prehypertension: A randomized controlled trial. J. Exerc. Sci. Fit. 2019, 17, 47–54. [Google Scholar] [CrossRef]
- Pradubpoth, K.; Noonil, N.; Aekwarangkoon, S.; Phonphet, C. Effects of swing arms walking exercise on blood sugar level, blood pressure, and waist circumference in older adults with metabolic syndrome. SCNJ 2019, 6, 154–166. [Google Scholar]
- Tantiprasoplap, S.; Piaseu, N.; Kanungsukkasem, V.; Taneepanichskul, S. A randomized controlled trial comparing the effects of an arm swing exercise and low sodium intake education program with low sodium intake education alone on cardiovascular outcomes in postmenopausal women with prehypertension. J. Med. Assoc. Thai. 2020, 103, 22–31. [Google Scholar]
- Phoemsapthawee, J.; Ammawat, W.; Leelayuwat, N. The benefits of arm swing exercise on cognitive performance in older women with mild cognitive impairment. J. Exerc. Physiol. Online 2016, 19, 123–136. [Google Scholar]
- Prasertsri, P.; Boonla, O.; Phoemsapthawee, J.; Leelayuwat, N. Comparative effects of arm swing and leg cycling exercise on exercise capacity and cardiac autonomic activity of sedentary young adults. J. Exerc. Physiol. Online 2017, 20, 53–65. [Google Scholar]
- Wanna, J.; Terathongkum, S.; Thipsuwannakool, V. Effects of arm swing exercise program on HbA1c and nutritional status in adults with type 2 diabetes in community. BKK Med. J. 2018, 14, 23–28. [Google Scholar] [CrossRef][Green Version]
- Terathongkum, S.; Phonyiam, R.; Koonmee, P. Effects of traditional and modified arm swing exercise programs on blood glucose and nutritional status among people with type 2 diabetes: A secondary data analysis. Pac. Rim Int. J. Nurs. Res. 2021, 25, 452–465. [Google Scholar][Green Version]
- Saelao, K.; Kanungsukkasem, V. Effects of arm swing exercise, walking, and walking exercise combined with arm swing exercise on health-related physical fitness of elderly women. J. Sport Health Sci. 2012, 13, 92–103. [Google Scholar][Green Version]
- Terathongkum, S.; Kittipimpanon, K. Effects of arm swing exercise program on HbA1C and nutritional status in adults and older adults with type 2 diabetes: A quasi-experimental study. Nat. Life Sci. Commun. 2023, 22, e2023048. [Google Scholar] [CrossRef]
- Kiewdee, S.; Inta, N. Effects of arm swing exercise and dietary control program on body mass index and waist circumference among obese persons in Maharaj Nakorn Chiang Mai Hospital. J. Health Sci. Scholarsh. 2023, 10, e2023048. [Google Scholar]
- Ramírez-Manent, J.I.; Jover, A.M.; Martinez, C.S.; Tomás-Gil, P.; Martí-Lliteras, P.; López-González, Á.A. Waist circumference is an essential factor in predicting insulin resistance and early detection of metabolic syndrome in adults. Nutrients 2023, 15, 257. [Google Scholar] [CrossRef]
- Yoo, J.E.; Han, K.; Jung, J.; Hur, Y.; Kim, Y.H.; Kim, E.S.; Son, J.W.; Rhee, E.; Lee, W.; Nam, G.E. Body mass index, waist circumference and cardiovascular diseases in transitional ages (40 and 66 years). J. Cachexia Sarcopenia Muscle 2023, 14, 369–381. [Google Scholar] [CrossRef]
- Rabiee Rad, M.; Ghasempour Dabaghi, G.; Sadri, H.; Darouei, B.; Amani-Beni, R.; Mazaheri-Tehrani, S. Triglyceride glucose-waist circumference as a predictor of mortality and subtypes of cardiovascular disease: A systematic review and meta-analysis. Diabetol. Metab. Syndr. 2025, 17, 59. [Google Scholar] [CrossRef] [PubMed]
- Jayedi, A.; Soltani, S.; Zargar, M.S.; Khan, T.A.; Shab-Bidar, S. Central fatness and risk of all cause mortality: Systematic review and dose-response meta-analysis of 72 prospective cohort studies. BMJ 2020, 370, m3324. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, A.; Jungbluth Rodriguez, K.; Sabag, A.; Mavros, Y.; Parker, H.M.; Keating, S.E.; Johnson, N.A. Effect of aerobic exercise on waist circumference in adults with overweight or obesity: A systematic review and meta-analysis. Obes. Rev. 2022, 23, e13446. [Google Scholar] [CrossRef]
- Ross, R.; Neeland, I.J.; Yamashita, S.; Shai, I.; Seidell, J.; Magni, P.; Santos, R.D.; Arsenault, B.; Cuevas, A.; Hu, F.B.; et al. Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nat. Rev. Endocrinol. 2020, 16, 177–189. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association Professional Practice Committee. 2. Diagnosis and classification of diabetes: Standards of care in diabetes–2024. Diabetes Care 2024, 47 (Suppl. S1), S20–S42. [Google Scholar] [CrossRef]
- Wrench, E.; Rattley, K.; Lambert, J.E.; Killick, R.; Hayes, L.D.; Lauder, R.M.; Gaffney, C.J. There is no dose-response relationship between the amount of exercise and improvement in HbA1c in interventions over 12 weeks in patients with type 2 diabetes: A meta-analysis and meta-regression. Acta Diabetol. 2022, 59, 1399–1415. [Google Scholar] [CrossRef]
- Jayedi, A.; Emadi, A.; Shab-Bidar, S. Dose-dependent effect of supervised aerobic exercise on HbA1c in patients with type 2 diabetes: A meta-analysis of randomized controlled trials. Sports Med. 2022, 52, 1919–1938. [Google Scholar]
- Martinez, M.; Santamarina, J.; Pavesi, A.; Musso, C.; Umpierrez, G.E. Glycemic variability and cardiovascular disease in patients with type 2 diabetes. BMJ Open Diabetes Res. Care 2021, 9, e002032. [Google Scholar] [CrossRef]
- Li, R.; Qu, S.; Zhang, P.; Chattopadhyay, S.; Gregg, E.W.; Albright, A.; Hopkins, D.; Pronk, N.P. Economic evaluation of combined diet and physical activity promotion programs to prevent type 2 diabetes among persons at increased risk: A systematic review for the community preventive services task force. Ann. Intern. Med. 2015, 163, 452–460. [Google Scholar] [CrossRef] [PubMed]
- Aschner, P.M.; Muñoz, O.M.; Girón, D.; García, O.M.; Fernández-Ávila, D.G.; Casas, L.Á.; Bohórquez, L.F.; T, C.M.A.; Carvajal, L.; Ramírez, D.A.; et al. Clinical practice guideline for the prevention, early detection, diagnosis, management and follow up of type 2 diabetes mellitus in adults. Colomb. Med. 2016, 47, 109–131. [Google Scholar] [CrossRef]
- Iaccarino, G.; Franco, D.; Sorriento, D.; Strisciuglio, T.; Barbato, E.; Morisco, C. Modulation of insulin sensitivity by exercise training: Implications for cardiovascular prevention. J. Cardiovasc. Transl. Res. 2021, 14, 256–270. [Google Scholar] [CrossRef]
- Rietz, M.; Lehr, A.; Mino, E.; Lang, A.; Szczerba, E.; Schiemann, T.; Herder, C.; Saatmann, N.; Geidl, W.; Barbaresko, J.; et al. Physical activity and risk of major diabetes-related complications in individuals with diabetes: A systematic review and meta-analysis of observational studies. Diabetes Care 2022, 45, 3101–3111. [Google Scholar] [CrossRef]
- Canoy, D.; Nazarzadeh, M.; Copland, E.; Bidel, Z.; Rao, S.; Li, Y.; Edwards, J.J.; Deenmamode, A.H.P.; Griffiths, M.; Arnold, O.; et al. How much lowering of blood pressure is required to prevent cardiovascular disease in patients with and without previous cardiovascular disease? Curr. Cardiol. Rep. 2022, 24, 851–860. [Google Scholar] [CrossRef] [PubMed]
- Edwards, J.J.; Deenmamode, A.H.P.; Griffiths, M.; Arnold, O.; Cooper, N.J.; Wiles, J.D.; O′DRiscoll, J.M. Exercise training and resting blood pressure: A large-scale pairwise and network meta-analysis of randomised controlled trials. Br. J. Sports Med. 2023, 57, 1317–1326. [Google Scholar] [CrossRef]
- Dassanayake, S.; Sole, G.; Wilkins, G.; Gray, E.; Skinner, M. Effectiveness of Physical Activity and Exercise on Ambulatory Blood Pressure in Adults with Resistant Hypertension: A Systematic Review and Meta-Analysis. High Blood Press. Cardiovasc. Prev. 2022, 29, 275–286. [Google Scholar] [CrossRef]
- Jakus, T.; Jurdana, M.; Žiberna, L.; Pražnikar, Z.J. Acute moderate-intensity exercise increases total antioxidant capacity and anti-inflammatory responses in competitive cyclists: The role of adiponectin. Eur. J. Inflamm. 2021, 19, 1–11. [Google Scholar] [CrossRef]
- Rose, G.L.; Skinner, T.L.; Mielke, G.I.; Schaumberg, M.A. The effect of exercise intensity on chronic inflammation: A systematic review and meta-analysis. J. Sci. Med. Sport 2021, 24, 345–351. [Google Scholar] [CrossRef]
- Gomarasca, M.; Micielska, K.; Faraldi, M.; Flis, M.; Perego, S.; Banfi, G.; Ziemann, E.; Lombardi, G. Impact of 12-week moderate-intensity aerobic training on inflammasome complex activation in elderly women. Front. Physiol. 2022, 13, 792859. [Google Scholar] [CrossRef]
- Liu, Y.; Sun, Z.; Chen, T.; Yang, C. Does exercise training improve the function of vascular smooth muscle? A systematic review and meta-analysis. Res. Sports Med. 2022, 30, 577–592. [Google Scholar] [CrossRef]
- Rosenblat, M.A.; Granata, C.; Thomas, S.G. Effect of interval training on the factors influencing maximal oxygen consumption: A systematic review and meta-analysis. Sports Med. 2022, 52, 1329–1352. [Google Scholar] [CrossRef]
- Hurst, C.; Sayer, A.A. Improving muscle strength and physical function in older people living with sarcopenia and physical frailty: Not all exercise is created equal. J. R. Coll. Physicians Edinb. 2022, 52, 166–171. [Google Scholar] [CrossRef] [PubMed]
- Cannataro, R.; Cione, E.; Bonilla, D.A.; Cerullo, G.; Angelini, F.; D’Antona, G. Strength training in elderly: An useful tool against sarcopenia. Front. Sports Act. Living 2022, 4, 950949. [Google Scholar] [CrossRef] [PubMed]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour; World Health Organization: Geneva, Switzerland, 2020; Available online: https://iris.who.int/bitstream/handle/10665/336656/9789240015128-eng.pdf (accessed on 25 June 2025).

| Study | Country | Design | Participants | Intervention | Duration (WK) | Outcome | |
|---|---|---|---|---|---|---|---|
| Age (Year) | Sample (Intervention/Control) | ||||||
| 1. Saelao et al., 2012 [29] | Thailand | Quasi-experimental | 60–69 yrs | 63 (15/17/15) | ASE 3 days per week and 50 min a day | 8 |
|
| 2. Phoemsapthawee et al., 2016 [25] | Thailand | RCT | 65–87 yrs | 36 (18/18) | ASE 5 days per week; 20 min/day during weeks 1–3, 25 min/day in week 4, and 30 min/day from week 5 onward, with warm-up/cool-down and progression in swing speed | 12 |
|
| 3. Prasertsri et al., 2017 [26] | Thailand | RCT | 21.22 ± 2.84 yrs | 60(20/20/20) | ASE 3 days per week and 30 min a day | 8 |
|
| 4. Wanna et al., 2018 [27] | Thailand | RCT | 20–59 yrs | 43(22/21) | ASE 5 days per week and 30 min a day, with diabetes education and follow-up support | 12 |
|
| 5. Prasertsri et al., 2018 [17] | Thailand | RCT | 71.80 ± 7.16 yrs | 51 (25/26) | ASE 3 days per week and 30 min a day | 12 |
|
| 6. Chompoopan et al., 2018 [13] | Thailand | RCT | >60 yrs | 128 (64/64) | ASE 5 days per week and 30 min a day, with 5 min warm-up and 5 min cool-down | 24 |
|
| 7. Prasertsri et al., 2019 [22] | Thailand | RCT | 60–68 yrs | 50 (25/25) | ASE 3 days per week and 30 min a day; 1-month follow-up assessed for carry-over effects | 12 |
|
| 8. Pradubpoth et al., 2019 [23] | Quasi-experimental research design. | Quasi-experimental | >60 yrs | 66 (33/33) | ASE 5 days per week and 15 min a day | 12 |
|
| 9. Tantiprasoplap et al., 2020 [24] | Thailand | RCT | >60 yrs | 84 (42/42) | ASE 3 days per week and 30–40 min a day, combined with low sodium intake education | 12 |
|
| 10. Terathongkum et al., 2021 [28] | Thailand | Quasi-experimental | >20 yrs | 76 (26/24/26) | ASE 5 days per week and 30 min a day | 12 |
|
| 11. Terathongkum et al., 2023 [30] | Thailand | Quasi-experimental | >18 yrs | 80(41/39) | ASE 5 days per week and 30 min a day | 12 |
|
| 12. Kiewdee et al., 2023 [16] | Thailand | Quasi-experimental | 18–60 yrs | 52 (26/26) | ASE 130 min a day | 16 |
|
| 13. Xiao et al., 2023 [8] | Thailand | RCT | 68.3 + 5.6 yrs | 56 (28/28) | ASE 5 days per week and 40 min a day | 8 |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Whaikid, P.; Piaseu, N. Effectiveness of Arm Swing Exercise on Comprehensive Health Outcomes: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 2357. https://doi.org/10.3390/healthcare13182357
Whaikid P, Piaseu N. Effectiveness of Arm Swing Exercise on Comprehensive Health Outcomes: A Systematic Review and Meta-Analysis. Healthcare. 2025; 13(18):2357. https://doi.org/10.3390/healthcare13182357
Chicago/Turabian StyleWhaikid, Phatcharaphon, and Noppawan Piaseu. 2025. "Effectiveness of Arm Swing Exercise on Comprehensive Health Outcomes: A Systematic Review and Meta-Analysis" Healthcare 13, no. 18: 2357. https://doi.org/10.3390/healthcare13182357
APA StyleWhaikid, P., & Piaseu, N. (2025). Effectiveness of Arm Swing Exercise on Comprehensive Health Outcomes: A Systematic Review and Meta-Analysis. Healthcare, 13(18), 2357. https://doi.org/10.3390/healthcare13182357