Therapeutic vs. Recreational Use of Cocaine: Avoiding Diagnostic and Judicial Errors Through Interprofessional Collaboration—A Five-Case Report †
Abstract
1. Introduction
2. Analytical Workflow
3. Case Descriptions
3.1. Case I—Pedestrian–Car Accident
3.2. Case 2—Pedestrian–Car Accident
3.3. Case 3—Car–Car Accident
3.4. Case 4—Car Accident
3.5. Case 5—Pedestrian–Car Accident
4. Discussion
- Three cases involved patients between 82 and 84 years old, whereas the mean age of cocaine consumers in Switzerland is around 34 ± 14 years in cases of driving under the influence of drugs (DUID) [8].
- The context of hospitalization, which may be consistent with a potential therapeutic use of cocaine.
- The detection of cocaine and its metabolites in blood, but not in urine (Case 3). This scenario suggests a very recent cocaine administration since the Tmax of cocaine is approximately 0.43 ± 0.34 h and the cocaine metabolites, benzoylecgonine and ecgonine methyl ester, reach maximum urine concentrations within the 4 to 8 h collection period following topical intranasal administration [18,19].
- Inconsistent results within multiple samplings (Case 3).
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Benowitz, N.L. Clinical Pharmacology and Toxicology of Cocaine. Pharmacol. Toxicol. 1993, 72, 3–12. [Google Scholar] [CrossRef]
- Elfers, K.; Menne, L.; Colnaghi, L.; Hoppe, S.; Mazzuoli-Weber, G. Short- and Long-Term Effects of Cocaine on Enteric Neuronal Functions. Cells 2023, 12, 577. [Google Scholar] [CrossRef]
- Fattinger, K.; Benowitz, N.L.; Jones, R.T.; Verotta, D. Nasal Mucosal versus Gastrointestinal Absorption of Nasally Administered Cocaine. Eur. J. Clin. Pharmacol. 2000, 56, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Biebuyck, J.F.; Fleming, J.A.; Byck, R.; Barash, P.G. Pharmacology and Therapeutic Applications of Cocaine. Anesthesiology 1990, 73, 518. [Google Scholar] [CrossRef] [PubMed]
- Coe, M.A.; Jufer Phipps, R.A.; Cone, E.J.; Walsh, S.L. Bioavailability and Pharmacokinetics of Oral Cocaine in Humans. J. Anal. Toxicol. 2018, 42, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Musshoff, F.; Madea, B. Cocaine and Benzoylecgonine Concentrations in Fluorinated Plasma Samples of Drivers under Suspicion of Driving under Influence. Forensic Sci. Int. 2010, 200, 67–72. [Google Scholar] [CrossRef]
- EMCDDA Annual Report: The State of the Drug Problem in Europe. Available online: https://www.euda.europa.eu/publications/annual-report/2010_en (accessed on 9 September 2025).
- Maurer, J.; Vergalito, E.; Prior, A.-F.; Donzé, N.; Thomas, A.; Augsburger, M. Suspicion of Driving under the Influence of Alcohol or Drugs: Cross Sectional Analysis of Drug Prevalence in the Context of the Swiss Legislation. Forensic Sci. Int. 2021, 329, 111081. [Google Scholar] [CrossRef]
- Augsburger, M.; Rivier, L. Drugs and Alcohol among Suspected Impaired Drivers in Canton de Vaud (Switzerland). Forensic Sci. Int. 1997, 85, 95–104. [Google Scholar] [CrossRef]
- Augsburger, M.; Donzé, N.; Ménétrey, A.; Brossard, C.; Sporkert, F.; Giroud, C.; Mangin, P. Concentration of Drugs in Blood of Suspected Impaired Drivers. Forensic Sci. Int. 2005, 153, 11–15. [Google Scholar] [CrossRef]
- Lillsunde, P.; Gunnar, T. Drugs and Driving: The Finnish Perspective. Bull. Narc. 2005, 57, 213–229. [Google Scholar]
- DuPont, R.L.; Voas, R.B.; Walsh, J.M.; Shea, C.; Talpins, S.K.; Neil, M.M. The Need for Drugged Driving per Se Laws: A Commentary. Traffic Inj. Prev. 2012, 13, 31–42. [Google Scholar] [CrossRef]
- Ordinance of the FEDRO on the Control of the Road Traffic. Federal Roads Office. Available online: https://www.Fedlex.Admin.Ch (accessed on 9 September 2025).
- Gjerde, H.; Strand, M.C. Legal Limits for Driving under the Influence of Illicit Drugs: Large Variations between Jurisdictions. Forensic Sci. Int. Rep. 2023, 8, 100336. [Google Scholar] [CrossRef]
- Long, H.; Greller, H.; Mercurio-Zappala, M.; Nelson, L.S.; Hoffman, R.S. Medicinal Use of Cocaine: A Shifting Paradigm Over 25 Years. Laryngoscope 2004, 114, 1625–1629. [Google Scholar] [CrossRef] [PubMed]
- Lutfallah, S.C.; Brown, E.; Spillers, N.J.; Tandon, A.; Kelkar, R.A.; Ahmadzadeh, S.; Viswanath, O.; Varrassi, G.; Shekoohi, S.; Kaye, A.D. Topical Cocaine Hydrochloride Nasal Solution: Anesthetic and Surgical Considerations. Cureus 2023, 15, e42804. [Google Scholar] [CrossRef]
- Maurer, H.H.; Pfleger, K.; Weber, A.A. Mass Spectral and GC Data of Drugs, Poisons, Pesticides, Pollutants and Their Metabolites, 5th ed.; Wiley: Hoboken, NJ, USA, 2016; ISBN 978-3-527-34287-7. [Google Scholar]
- McGrath, J.; McGrath, A.; Burdett, J.; Shokri, T.; Cohn, J.E. Systemic Pharmacokinetics of Topical Intranasal Cocaine in Healthy Subjects. Am. J. Rhinol. Allergy 2020, 34, 336–341. [Google Scholar] [CrossRef]
- Baselt, R.C. Disposition of Toxic Drugs and Chemicals in Man, 11th ed.; Biomedical Publications: Foster City, CA, USA, 2017. [Google Scholar]
- Reichman, O.S.; Otto, R.A. Effect of Intranasal Cocaine on the Urine Drug Screen for Benzoylecgonine. Otolaryngol. Head Neck Surg. 1992, 106, 223–225. [Google Scholar] [CrossRef]
- Larsen, M.H.; Rosenkrantz, O.; Rasmussen, B.S.; Nielsen, M.K.K.; Linnet, K.; Rasmussen, L.S.; Isbye, D. Detection of Cocaine 24 h after Administration before Nasotracheal Intubation. Acta Anaesthesiol. Scand. 2024, 68, 1200–1206. [Google Scholar] [CrossRef]
- Yeo, J.J.Y.; Badrol, S.S.S.; Maan, A.; Chan, J.; Barraclough, J.; Jervis, S. Cocaine Use in Sinonasal Surgery: Patients’ Perspective on Its Use and the Need for Pre-Operative Consent. J. Laryngol. Otol. 2024, 138, 1036–1038. [Google Scholar] [CrossRef]
- Basilicata, P.; Marisei, M.; Guadagni, R.; Sibilio, M.; Niola, M.; Pieri, M. Pediatric Poisoning Management: How Clinical Practice Can Benefit from Forensic Approach. J. Forensic Sci. 2024, 69, 1501–1507. [Google Scholar] [CrossRef] [PubMed]
- Patel, M.; Fraunfelder, F.W. Toxicity of Topical Ophthalmic Anesthetics. Expert Opin. Drug Metab. Toxicol. 2013, 9, 983–988. [Google Scholar] [CrossRef]
- Quiney, R.E. Intranasal Topical Cocaine: Moffett’s Method or Topical Cocaine Paste? J. Laryngol. Otol. 1986, 100, 279–283. [Google Scholar] [CrossRef]
- Harper, S.J.; Jones, N.S. Cocaine: What Role Does It Have in Current ENT Practice? A Review of the Current Literature. J. Laryngol. Otol. 2006, 120, 808–811. [Google Scholar] [CrossRef]
- Page, D.E.; Rimmer, J.; Keane, M.; Manikappa, S.; Butzbach, D.; Giddings, C. Is Atomised Intranasal Cocaine Systemically Absorbed during Endoscopic Sinus Surgery? Rhinology 2019, 57, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Foxton, C.R.; Harper, N.G.P.; Johnstone, A. Moffett’s Solution and the New 2015 UK Drug-Driving Laws: The Case for Consenting Patients for Its Use. Clin. Otolaryngol. 2016, 41, 432. [Google Scholar] [CrossRef]
- Dwyer, C.; Sowerby, L.; Rotenberg, B.W. Is Cocaine a Safe Topical Agent for Use during Endoscopic Sinus Surgery? Laryngoscope 2016, 126, 1721–1723. [Google Scholar] [CrossRef] [PubMed]
- Fu, B.; Sharp, H. Moffett’s Solution—Is It Safe? The UK Experience. Clin. Otolaryngol. 2011, 36, 184–185. [Google Scholar] [CrossRef]
- McGrath, J.; McGrath, A.; Burdett, J.; Shokri, T.; Cohn, J.E. Investigation of Topical Intranasal Cocaine for Sinonasal Procedures: A Randomized, Phase III Clinical Trial. Int. Forum. Allergy Rhinol. 2020, 10, 981–990. [Google Scholar] [CrossRef] [PubMed]
- Francis, A.; Backus, T.C.; Howland, M.A.; Hoffman, R.S. Comment on “Investigation of Topical Intranasal Cocaine for Sinonasal Procedures: A Randomized, Phase III Clinical Trial”. Int. Forum. Allergy Rhinol. 2021, 11, 84. [Google Scholar] [CrossRef]
- Tarver, C.P.; Noorily, A.D.; Sakai, C.S. A Comparison of Cocaine vs. Lidocaine with Oxymetazoline for Use in Nasal Procedures. Otolaryngol. Head Neck Surg. 1993, 109, 653–659. [Google Scholar] [CrossRef]
- Noorily, A.D.; Noorily, S.H.; Otto, R.A. Cocaine, Lidocaine, Tetracaine: Which Is Best for Topical Nasal Anesthesia? Anesth. Analg. 1995, 81, 724–727. [Google Scholar] [CrossRef]
- Husain, S.; Ramos, J.A.; Karaf, J.H.A.; Zahedi, F.D.; Ahmad, N.; Abdullah, B. Efficacy of Topical Tranexamic Acid to Reduce Bleeding in Endoscopic Sinus Surgery for Chronic Rhinosinusitis with Polyposis. Eur. Arch. Otorhinolaryngol. 2022, 280, 737–741. [Google Scholar] [CrossRef] [PubMed]
- Hale, S.J.M.; Kim, R.; Douglas, R.G. Topical Anaesthesia and Decongestion in Rhinology. Rhinology 2024, 62, 143–151. [Google Scholar] [CrossRef]
- Reid, J.W.; Rotenberg, B.W.; Sowerby, L.J. Contemporary Decongestant Practices of Canadian Otolaryngologists for Endoscopic Sinus Surgery. J. Otolaryngol. Head Neck Surg. 2019, 48, 15. [Google Scholar] [CrossRef]
- Irani, D.; Mendelsohn, M. Cocaine Use in Nasal Surgery by ENT Surgeons in Australia. Aust. J. Otolaryngol. 2002, 5, 26–28. [Google Scholar]
- Augsburger, M.; Widmer, C.; Deglon, J.; Mangin, P. O36: Driving under the Influence of Cocaine or Therapeutic Administration of Cocaine? Toxicol. Anal. Clin. 2014, 26, S21. [Google Scholar] [CrossRef]
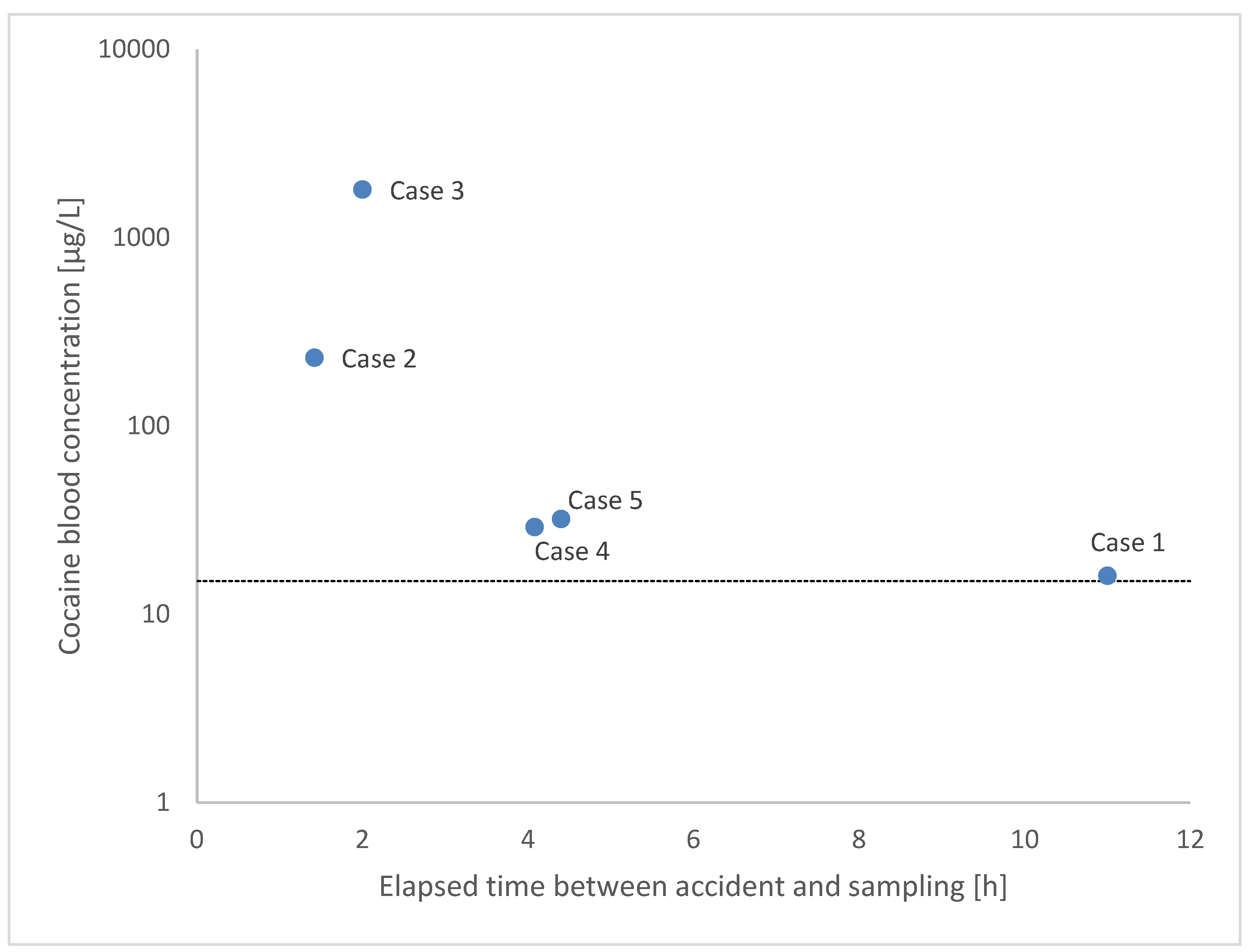
| Case | Sex | Age | Time Elapsed Between Accident and Blood Sampling | Blood (µg/L) | Time Elapsed Between Accident and Urine Sampling | Urine (µg/L) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cocaine | BE | EME | EC | Cocaine | BE | EME | EC | |||||
| #1 Traffic accident, pedestrian | Man | 83 | 11 h 2 min | 16 | 370 | 60 | nd | 11 h 4 min | 1700 | 560 | 1200 | nd |
| #2 Traffic accident, pedestrian | Woman | 84 | 1 h 25 min | 230 | 370 | 42 | nd | (no urine sample) | - | - | - | - |
| #3 Traffic accident, car passenger | Man | 66 | 1 h 30 min | nd | nd | - | nd | 1 h 30 min | nd | nd | - | nd |
| 2 h | 1800 | 460 | - | nd | - | nd | nd | - | nd | |||
| Autopsy | 370 | 200 | - | nd | - | nd | nd | - | nd | |||
| #4 Traffic accident, car driver | Man | 30 | 4 h 5 min | 29 | <20 | nd | nd | 4 h 5 min | nd | nd | nd | nd |
| #5 Traffic accident, pedestrian | Man | 82 | 4 h 24 min | 32 | 45 | <10 | nd | 4 h 29 min | 190 | 120 | nd | nd |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Magliocco, G.; Suppan, L.; Vujic, T.; Palmiere, C.; Thomas, A.; Grabherr, S.; Augsburger, M. Therapeutic vs. Recreational Use of Cocaine: Avoiding Diagnostic and Judicial Errors Through Interprofessional Collaboration—A Five-Case Report. Healthcare 2025, 13, 2318. https://doi.org/10.3390/healthcare13182318
Magliocco G, Suppan L, Vujic T, Palmiere C, Thomas A, Grabherr S, Augsburger M. Therapeutic vs. Recreational Use of Cocaine: Avoiding Diagnostic and Judicial Errors Through Interprofessional Collaboration—A Five-Case Report. Healthcare. 2025; 13(18):2318. https://doi.org/10.3390/healthcare13182318
Chicago/Turabian StyleMagliocco, Gaëlle, Laurent Suppan, Tatjana Vujic, Cristian Palmiere, Aurélien Thomas, Silke Grabherr, and Marc Augsburger. 2025. "Therapeutic vs. Recreational Use of Cocaine: Avoiding Diagnostic and Judicial Errors Through Interprofessional Collaboration—A Five-Case Report" Healthcare 13, no. 18: 2318. https://doi.org/10.3390/healthcare13182318
APA StyleMagliocco, G., Suppan, L., Vujic, T., Palmiere, C., Thomas, A., Grabherr, S., & Augsburger, M. (2025). Therapeutic vs. Recreational Use of Cocaine: Avoiding Diagnostic and Judicial Errors Through Interprofessional Collaboration—A Five-Case Report. Healthcare, 13(18), 2318. https://doi.org/10.3390/healthcare13182318






