Effect of a Multi-Faceted Training Program on Falls in Senior Pickleball Players
Abstract
1. Introduction
2. Materials and Methods
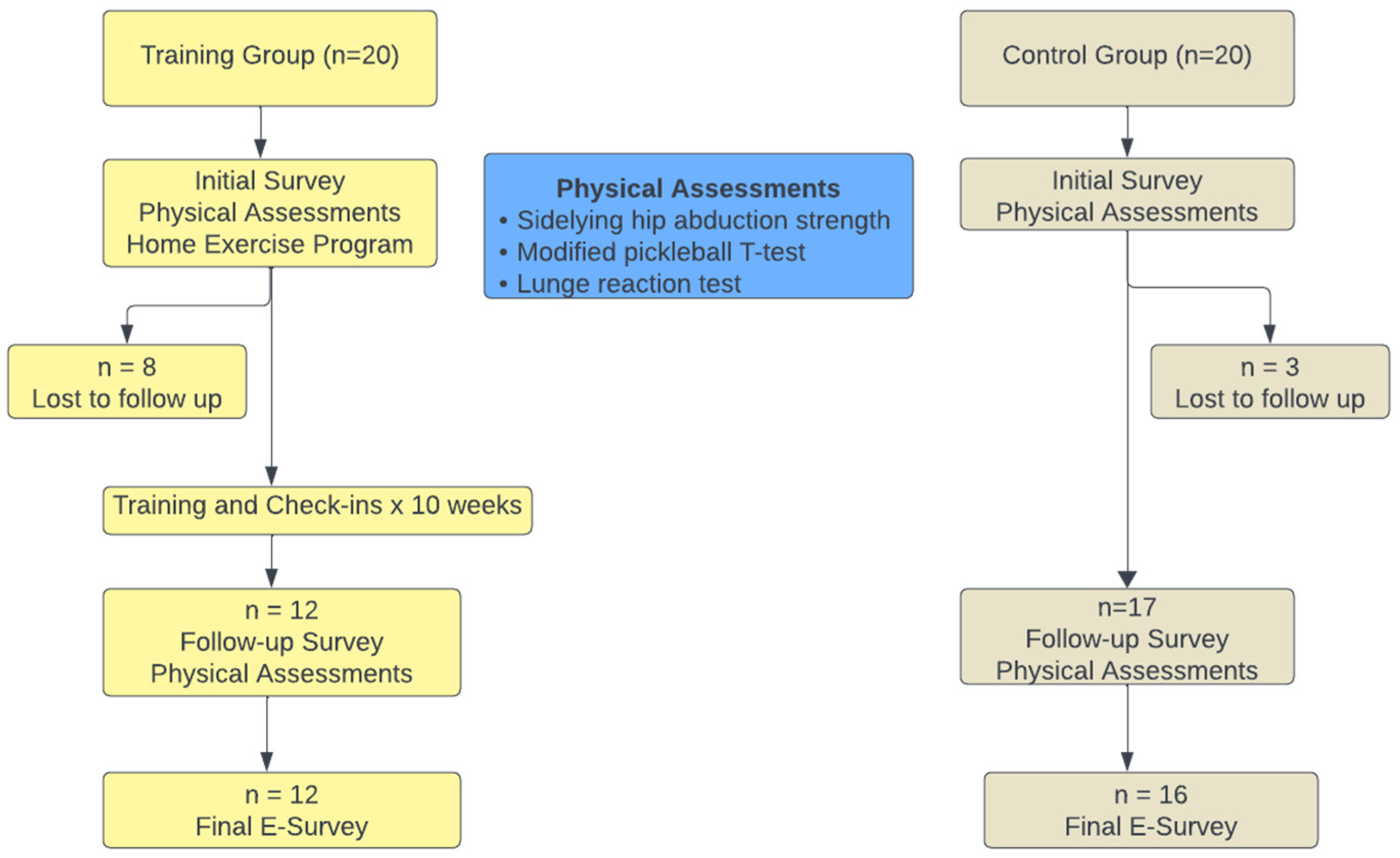
2.1. Study Design
2.2. Participants
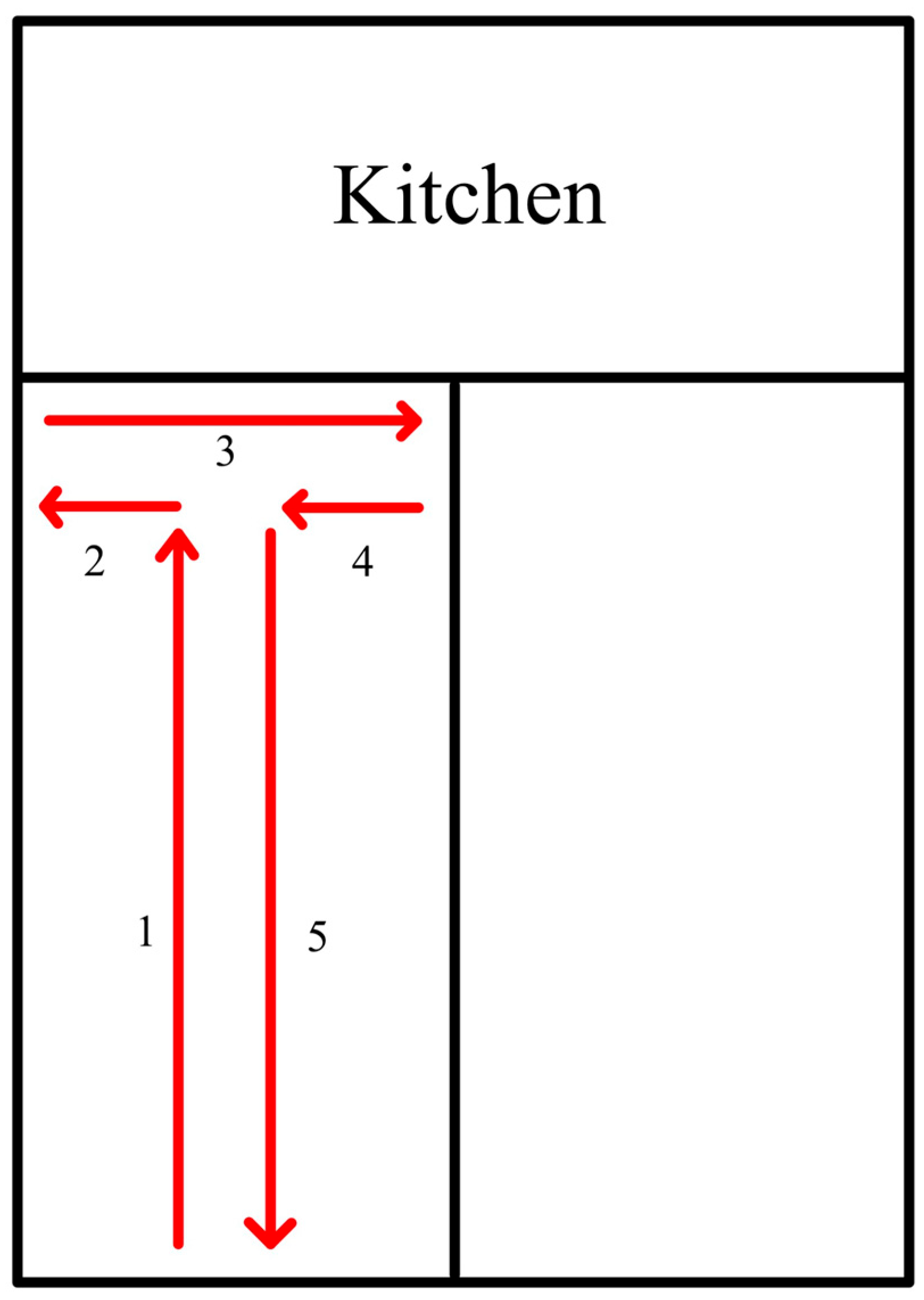
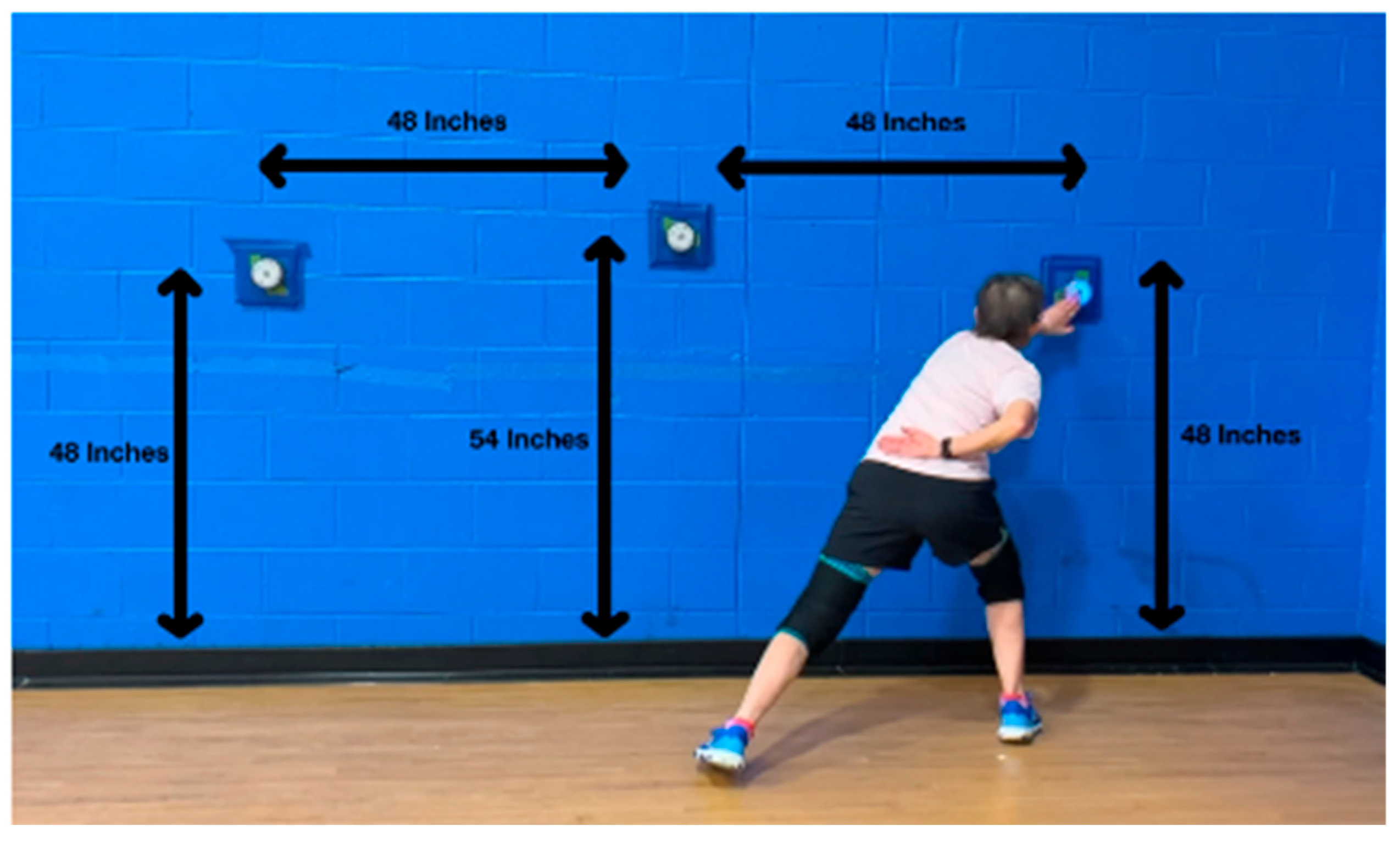
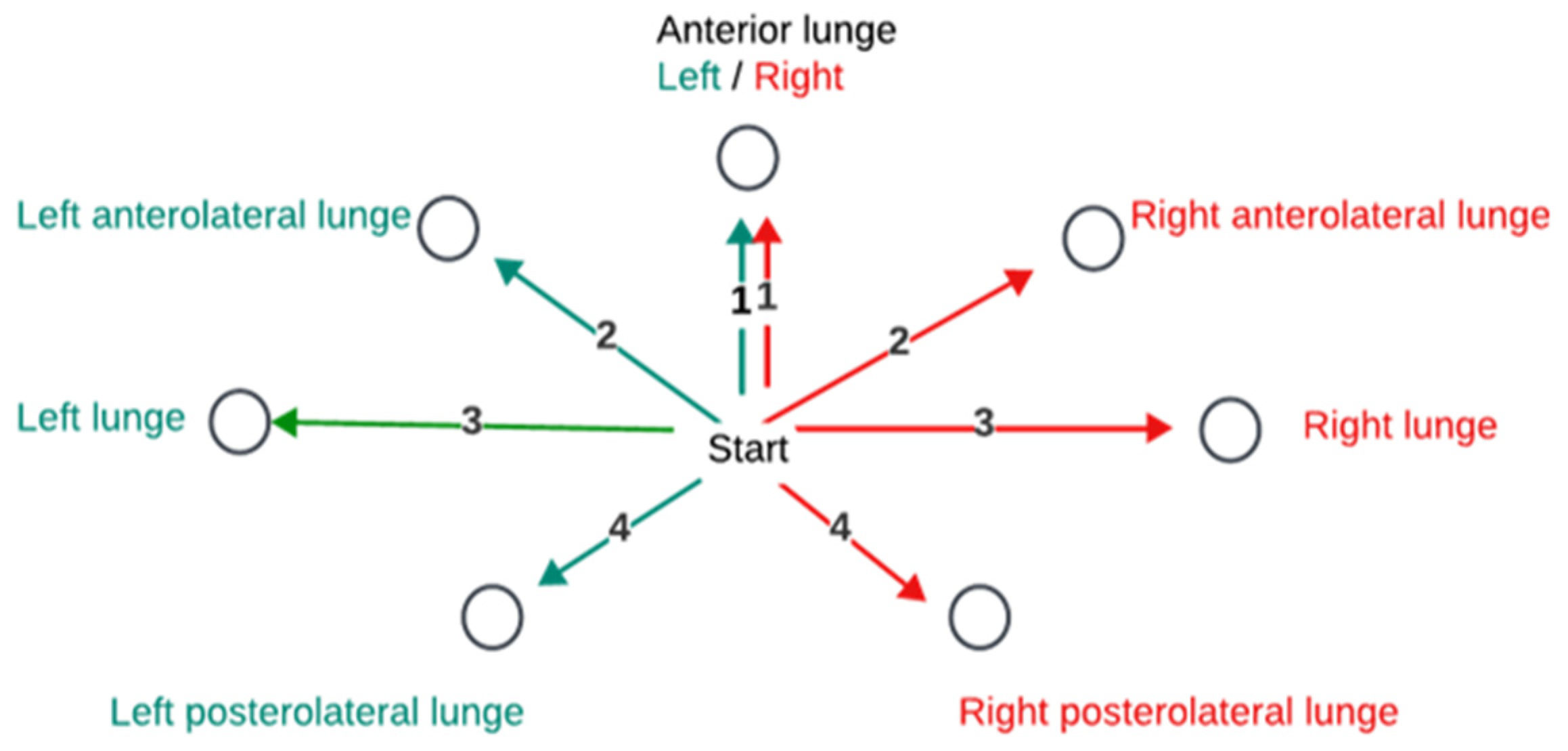
2.3. Procedures
2.4. Statistical Analysis
3. Results
3.1. Baseline
3.2. Changes in Performance Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mackie, B. Pickleball Statistics—The Numbers Behind America’s Fastest-Growing Sport. 2025. Available online: https://www.pickleheads.com/blog/pickleball-statistics (accessed on 3 July 2025).
- Webber, S.C.; Anderson, S.; Biccum, L.; Jin, S.; Khawashki, S.; Tittlemier, B.J. Physical activity intensity of singles and doubles pickleball in older adults. J. Aging Phys. Act. 2022, 31, 365–370. [Google Scholar] [CrossRef]
- Stroesser, K.; Mulcaster, A.; Andrews, D.M. Pickleball participation and the health and well-being of adults-A scoping review. J. Phys. Act. Health 2024, 21, 847–860. [Google Scholar] [CrossRef] [PubMed]
- Denning, W.M.; Zagrodnik, J.; Smith, M.; Ruden, T. Physical activity differences between walking and playing pickleball doubles. Sci. Sport 2022, 37, 513.e1–513.e4. [Google Scholar] [CrossRef]
- Heo, J.; Ryu, J.; Yang, H.; Kim, K.M. Serious leisure and depression in older adults: A study of pickleball players. Leis. Stud. 2018, 37, 561–573. [Google Scholar] [CrossRef]
- Azar, F.M.; Lamplot, J.D.; Bernholt, D.L.; Spence, D.D. Pickleball: A standard review of injury prevalence and prevention in a rapidly growing sport. J. Am. Acad. Orthop. Surg. 2024, 32, e1130–e1142. [Google Scholar] [CrossRef] [PubMed]
- Greiner, N. Pickleball: Injury considerations in an increasingly popular sport. Mo. Med. 2019, 116, 488–491. [Google Scholar]
- Kingston, K.; Parker, E.B.; Higgins, A.; Smith, J.T. Emerging patterns of foot and ankle injuries in pickleball players: A short report. Foot Ankle Int. 2024, 45, 1266–1269. [Google Scholar] [CrossRef] [PubMed]
- Meyersohn, N. Pickleball Injuries May Cost Americans Nearly $400 Million This Year. CNN Business, 2023. Available online: https://www.cnn.com/2023/06/27/business/pickleball-injuries-cost-health-care/index.html (accessed on 3 July 2025).
- Cheng, R.; Moran, J.; Kim, B.; Yuan, M.S.; O’Leary, C.J.; Wang, C.; Dines, J.S.; Katt, B.M.; Jimenez, A.E. A substantial increase in injuries and hospitalizations associated with playing pickleball from 2020 to 2022. Arthrosc. Sports Med. Rehabil. 2025, 7, 101067. [Google Scholar] [CrossRef]
- Boroumand, S.; Park, N.; Katsnelson, B.; Qian, E.; Norman, M.; Joo, P.; Diatta, F.; Noel, O.; Moran, J.; Jimenez, A. The perils of pickleball: A two decade analysis of upper and lower extremity injuries from America’s fastest growing sport. J. Sports Sci. 2025, 43, 1378–1385. [Google Scholar] [CrossRef]
- Herzberg, S.D.; Bowman, E.N.; Hill, K.L. Evaluation of pickleball-related injuries at a single institution from 2017 to 2022. Orthop. J. Sports Med. 2025, 13, 23259671251316997. [Google Scholar] [CrossRef]
- Weiss, H.; Dougherty, J.; DiMaggio, C. Non-fatal senior pickleball and tennis-related injuries treated in United States emergency departments, 2010–2019. Inj. Epidemiol. 2021, 8, 34. [Google Scholar] [CrossRef]
- Myers, B.; Hanks, J. Hip strength, change of direction, and falls in recreational pickleball players. Int. J. Sports Phys. Ther. 2024, 19, 1116–1125. [Google Scholar] [CrossRef]
- Bahat Öztürk, G.; Kılıç, C.; Bozkurt, M.E.; Karan, M.A. Prevalence and associates of fear of falling among community-dwelling older adults. J. Nutr. Health Aging 2021, 25, 433–439. [Google Scholar] [CrossRef]
- Gazibara, T.; Kurtagic, I.; Kisic-Tepavcevic, D.; Nurkovic, S.; Kovacevic, N.; Gazibara, T.; Pekmezovic, T. Falls, risk factors and fear of falling among persons older than 65 years of age. Psychogeriatrics 2017, 17, 215–223. [Google Scholar] [CrossRef]
- Feng, C.; Adebero, T.; DePaul, V.G.; Vafaei, A.; Norman, K.E.; Auais, M. A systematic review and meta-analysis of exercise interventions and use of exercise principles to reduce fear of falling in community-dwelling older adults. Phys. Ther. 2021, 102, pzab236. [Google Scholar] [CrossRef] [PubMed]
- Sitdhiraksa, N.; Piyamongkol, P.; Chaiyawat, P.; Chantanachai, T.; Ratta-Apha, W.; Sirikunchoat, J.; Pariwatcharakul, P. Prevalence and factors associated with fear of falling in community-dwelling Thai elderly. Gerontology 2021, 67, 276–280. [Google Scholar] [CrossRef]
- Araya, A.-X.; Iriarte, E. Fear of falling among community-dwelling sedentary and active older people. Investig. Educ. Enferm. 2021, 39, 157–166. [Google Scholar] [CrossRef] [PubMed]
- Legters, K. Fear of falling. Phys. Ther. 2002, 82, 264–272. [Google Scholar] [CrossRef]
- Sebastião, E.; Siqueira, V.; Bakare, J.; Bohn, L.; Gallo, L.H. Fear of falling in older adults living in a community-dwelling facility: Prevalence and its impact on activity behavior and physical function. J. Appl. Gerontol. 2024, 43, 1015–1022. [Google Scholar] [CrossRef]
- Lee, E.S.; Kim, B. The impact of fear of falling on health-related quality of life in community-dwelling older adults: Mediating effects of depression and moderated mediation effects of physical activity. BMC Public Health 2024, 24, 2459. [Google Scholar] [CrossRef] [PubMed]
- Shoukat, F.; Ur Rehman, S.S.; Ahmed, A. Effects of physical exercise intervention on improving physical functioning and quality of life among geriatric population: A systematic review of randomized controlled trials. J. Pak. Med. Assoc. 2024, 74, 1481–1487. [Google Scholar] [CrossRef]
- Gafner, S.C.; Bastiaenen, C.H.G.; Ferrari, S.; Gold, G.; Trombetti, A.; Terrier, P.; Hilfiker, R.; Allet, L. The role of hip abductor strength in identifying older persons at risk of falls: A diagnostic accuracy study. Clin. Interv. Aging 2020, 15, 645–654. [Google Scholar] [CrossRef]
- Pirauá, A.L.T.; Cavalcante, B.R.; de Oliveira, V.M.A.; Beltrão, N.B.; de Amorim Batista, G.; Pitangui, A.C.R.; Behm, D.; de Araújo, R.C. Effect of 24-week strength training on unstable surfaces on mobility, balance, and concern about falling in older adults. Scand. J. Med. Sci. Sports 2019, 29, 1805–1812. [Google Scholar] [CrossRef]
- Kato, S.; Murakami, H.; Demura, S.; Yoshioka, K.; Shinmura, K.; Yokogawa, N.; Igarashi, T.; Yonezawa, N.; Shimizu, T.; Tsuchiya, H. Abdominal trunk muscle weakness and its association with chronic low back pain and risk of falling in older women. BMC Musculoskelet. Disord. 2019, 20, 273–280. [Google Scholar] [CrossRef]
- Simpkins, C.; Yang, F. Muscle power is more important than strength in preventing falls in community-dwelling older adults. J. Biomech. 2022, 134, 111018. [Google Scholar] [CrossRef]
- Sadaqa, M.; Németh, Z.; Makai, A.; Prémusz, V.; Hock, M. Effectiveness of exercise interventions on fall prevention in ambulatory community-dwelling older adults: A systematic review with narrative synthesis. Front. Public Health 2023, 11, 1209319. [Google Scholar] [CrossRef] [PubMed]
- Whipple, M.O.; Hamel, A.V.; Talley, K.M.C. Fear of falling among community-dwelling older adults: A scoping review to identify effective evidence-based interventions. Geriatr. Nurs. 2018, 39, 170–177. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H. Is dual-task training clinically beneficial to improve balance and executive function in community-dwelling older adults with a history of falls? Int. J. Environ. Res. Public Health 2022, 19, 10198. [Google Scholar] [CrossRef]
- Donath, L.; van Dieën, J.; Faude, O. Exercise-based fall prevention in the elderly: What about agility? Sports Med. 2016, 46, 143–149. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, Cd012424. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Kondo, K.; Suzuki, K.; Yamada, M.; Matsumoto, D. Factors associated with falls in community-dwelling older people with focus on participation in sport organizations: The Japan gerontological evaluation study project. BioMed Res. Int. 2014, 2014, 537614. [Google Scholar] [CrossRef]
- Jordre, B.; Schweinle, W.; Oetjen, S.; Dybsetter, N.; Braun, M. Fall history and associated physical performance measures in competitive senior athletes. Top. Geriatr. Rehabil. 2016, 32, 1–16. [Google Scholar] [CrossRef]
- Vitale, K.; Liu, S. Pickleball: Review and clinical recommendations for this fast-growing sport. Curr. Sports Med. Rep. 2020, 19, 406–413. [Google Scholar] [CrossRef] [PubMed]
- Hanks, J.; Myers, B. Risk of upper extremity injury in recreational pickleball players. J. Funct. Morphol. Kinesiol. 2025, 10, 247. [Google Scholar] [CrossRef]
- Terrell, S.L.; Ficquette, P. Exploring training strategies to optimize court performance in older pickleball athletes. Strength. Cond. J. 2023, 45, 1–12. [Google Scholar] [CrossRef]
- Thorborg, K.; Krommes, K.K.; Esteve, E.; Clausen, M.B.; Bartels, E.M.; Rathleff, M.S. Effect of specific exercise-based football injury prevention programmes on the overall injury rate in football: A systematic review and meta-analysis of the FIFA 11 and 11+ programmes. Br. J. Sports Med. 2017, 51, 562–571. [Google Scholar] [CrossRef] [PubMed]
- Ling, D.I.; Cepeda, N.A.; Marom, N.; Jivanelli, B.; Marx, R.G. Injury prevention programmes with plyometric and strengthening exercises improve on-field performance: A systematic review. J. ISAKOS 2020, 5, 48–59. [Google Scholar] [CrossRef]
- Paz, G.A.; Almeida, L.; Ruiz, L.; Casseres, S.; Xavier, G.; Lucas, J.; Santana, H.G.; Miranda, H.; Bonnette, S.; Willardson, J. Myoelectric responses of lower-body muscles performing squat and lunge exercise variations adopting visual feedback with a laser sensor. J. Sport Rehabil. 2020, 29, 1159–1165. [Google Scholar] [CrossRef]
- Boudreau, S.; Dwyer, M.; Mattacola, C.; Latterman, C.; Uhl, T.; McKeon, J. Hip-muscle activation during the lunge, single-leg squat, and step-up-and-over exercises. J. Sport Rehabil. 2009, 18, 91–103. [Google Scholar] [CrossRef]
- Glaviano, N.R.; Saliba, S. Differences in gluteal and quadriceps muscle activation during weight-bearing exercises between female subjects with and without patellofemoral pain. J. Strength. Cond. Res. 2022, 36, 55–62. [Google Scholar] [CrossRef]
- Olsen, A.A.; Li, A.; Johnson, D.D.; Manson, H.C. Pickleball primer: An overview of common injuries, treatment, and optimization strategies in pickleball athlete. J. Am. Acad. Orthop. Surg. 2024, 32, 763–770. [Google Scholar] [CrossRef]
- Lachman, M.E.; Howland, J.; Tennstedt, S.; Jette, A.; Assmann, S.; Peterson, E.W. Fear of falling and activity restriction: The survey of activities and fear of falling in the elderly (SAFE). J. Gerontol. B Psychol. Sci. Soc. Sci. 1998, 53, P43–P50. [Google Scholar] [CrossRef]
- Ellmers, T.J.; Wilson, M.R.; Kal, E.C.; Young, W.R. The perceived control model of falling: Developing a unified framework to understand and assess maladaptive fear of falling. Age Ageing 2023, 52, afad093. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using effect size-or why the p value is not enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
- Maher, J.M.; Markey, J.C.; Ebert-May, D. The other half of the story: Effect size analysis in quantitative research. CBE Life Sci. Educ. 2013, 12, 345–351. [Google Scholar] [CrossRef]
- Morcelli, M.H.; Martineli, R.D.; Harumi, K.A.; Fernandes, C.L.; Zamfolini, H.C.; Ribeiro, M.N.; Mauro, G.; Navega, M.T. Peak torque, reaction time, and rate of torque development of hip abductors and adductors of older women. Physiother. Theory Pract. 2016, 32, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Ceballos-Laita, L.; Carrasco-Uribarren, A.; Cabanillas-Barea, S.; Pérez-Guillén, S.; Medrano-de-la-Fuente, R.; Hernando-Garijo, I.; Jiménez-del-Barrio, S. Relationship between Hip Abductor Muscle Strength and Frontal Plane Kinematics: A Cross-Sectional Study in Elite Handball Athletes. Appl. Sci. 2022, 12, 10044. [Google Scholar] [CrossRef]
- Rodrigues, R.; Gonçalves, V.; Casagrande, R.; Cemin, F.; Nodari, C.; Borges, I.; Fitarelli, L.; Bianchesse, J.; Rocha, E.S.d.; Rabello, R. Are proximal and distal neuromuscular parameters able to predict hip and knee frontal plane kinematics during single-leg landing? Phys. Ther. Sport 2023, 59, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Kozinc, Ž.; Smajla, D.; Šarabon, N. The relationship between lower limb maximal and explosive strength and change of direction ability: Comparison of basketball and tennis players, and long-distance runners. PLoS ONE 2021, 16, e0256347. [Google Scholar] [CrossRef] [PubMed]
- Thomas, C.; Comfort, P.; Jones, P.A.; Dos’Santos, T. A comparison of isometric midthigh-pull strength, vertical jump, sprint speed, and change-of-direction speed in academy netball players. Int. J. Sports Physiol. Perform. 2017, 12, 916–921. [Google Scholar] [CrossRef]
- Dos’Santos, T.; Thomas, C.; Comfort, P.; Jones, P.A. The effect of angle and velocity on change of direction biomechanics: An angle-velocity trade-off. Sports Med. 2018, 48, 2235–2253. [Google Scholar] [CrossRef] [PubMed]
- Young, W. Agility and change of direction speed are independent skills: Implications for agility in invasion sports. Int. J. Sports Sci. Coach. 2015, 10, 159–169. [Google Scholar] [CrossRef]
- Ye, J.; Cheng, R.; Gao, B.; Wang, Y.; Wang, Y. Scientific assessment of agility performance in competitive sports: Evolution, application, reliability, and validity. Strength. Condition J. 2025, 47, 56–75. [Google Scholar] [CrossRef]
- Sekulic, D.; Foretic, N.; Gilic, B.; Esco, M.R.; Hammami, R.; Uljevic, O.; Versic, S.; Spasic, M. Importance of agility performance in professional futsal players; reliability and applicability of newly developed testing protocols. Int. J. Environ. Res. Public Health 2019, 16, 3246. [Google Scholar] [CrossRef]
- Uysal, H.; Korkmaz, S.; Sen, S.; Thapa, R.; Pojskic, H. Effect of speed, agility, and quickness training on linear sprint, jump, and change of direction speed performance in soccer players: A systematic review and three-level meta-analysis. Strength. Cond. J. 2025, 47, 184–204. [Google Scholar] [CrossRef]
- Liu-Ambrose, T.; Khan, K.M.; Eng, J.J.; Janssen, P.A.; Lord, S.R.; McKay, H.A. Resistance and agility training reduce fall risk in women aged 75 to 85 with low bone mass: A 6-month randomized, controlled trial. J. Am. Geriatr. Soc. 2004, 52, 657–665. [Google Scholar] [CrossRef]
- Teng, B.; Gomersall, S.R.; Hatton, A.L.; Khan, A.; Brauer, S.G. Predictors of real-world adherence to prescribed home exercise in older patients with a risk of falling: A prospective observational study. Aging Med. 2023, 6, 361–369. [Google Scholar] [CrossRef] [PubMed]
- Sople, D.; Wilcox, R.B. Dynamic warm-ups play pivotal role in athletic performance and injury prevention. Arthrosc. Sports Med. Rehabil. 2025, 7, 101023. [Google Scholar] [CrossRef]
| Description | Progressions | |
|---|---|---|
| Fast Feet | Jog in place, then attain a ready position on command Line step overs | None Lateral and front-to-back line step overs progressed via increase in speed |
| Power | Lunge matrix Skater progression | Lunge matrix * Skater progression *
|
| Balance | Partner (or wall) ball toss and catch | Note, if a participant was unable to stand on one leg while performing a secondary task, the drill was performed with a wider base of support, either in tandem stance (slightly easier) or with feet together(significantly easier)
|
| Description | Progressions | |
|---|---|---|
| Change in Direction | Planned change in direction drills performed over half-court-width (~10 feet). |
|
| Agility | Reactive drills where participants responded to a stimulus (BlazePod, researcher, or ball) to change directions |
|
| Strength training exercises |
|
| Training Group | Control Group | |
|---|---|---|
| Age (years) # | 67.1 ± 5.2 (range 57–74) | 65.2 ± 8.9 (range 57–84) |
| Sex | ||
| Female | 8 | 12 |
| Male | 4 | 5 |
| Years playing # | 2.1 ± 1.3 | 3.7 ± 3.9 |
| Times per week playing pickleball # | 3.61 ± 1.67 | 3.83 ± 1.6 |
| Skill level † | ||
| ≤2.0 | 0 | 0 |
| 2.5 | 0 | 1 |
| 3.0 | 7 | 7 |
| 3.5 | 5 | 8 |
| 4.0 | 0 | 1 |
| >4.0 | 0 | 0 |
| Falls (number) | 1.8 ± 1.8 | 1.6 ± 1.5 |
| Walking ‡ | 0 (0–2) | 3 (1.5–6) * |
| Jogging ‡ | 0 (0–0) | 0 (0–0) |
| Cycling ‡ | 0 (0–0) | 0 (0–0) |
| Swimming ‡ | 0 (0–0) | 0 (0–0) |
| Strength training ‡ | 0 (0–3.75) | 1 (0–2.5) |
| Racket sports other than pickleball ‡ | 0 (0–0) | 0 (0–0.5) |
| Balance exercises ‡ | 0 (0–0) | 1 (0–2) * |
| Measure | Group | Intervention Time 1 (mean ± SD) | Intervention Time 2 (mean ± SD) | Change | Effect |
|---|---|---|---|---|---|
| Survey score | Training | 9.2 ± 4.5 | 6.2 ± 3.4 | −3 ‡ | Improved |
| Control | 6.6 ± 3.8 | 7.6 ± 2.7 | +1 ‡ | Declined | |
| Strength (Nm) | Training | 177.9 ± 58.8 | 187.8 ± 57.3 | +9.9 | Improved |
| Control | 178.2 ± 38.9 | 159.8 ± 37.1 | −18.4 * | Declined | |
| Total # | 178.0 ± 47.0 | 171.2 ± 47.5 | |||
| Change in Direction (seconds) | Training | 9.2 ± 1.9 | 8.5 ± 1.9 | −0.7 * | Improved |
| Control | 7.7 ± 1.8 | 8.1 ± 1.7 | +0.4 | Declined | |
| Total # | 8.4 ± 1.9 | 8.3 ± 1.8 | |||
| Agility (Hits) | Training | 15.1 ± 1.6 | 15.5 ± 1.7 | +0.4 | Improved |
| Control | 16.1 ± 1.9 | 15.8 ± 2.1 | −0.3 | Declined | |
| Total # | 15.4 ± 1.7 | 15.6 ± 1.9 |
| Measure | Effect | Statistic | p-Value | Effect Size |
|---|---|---|---|---|
| Survey score | z = −2.427 | p = 0.015 * | r = 0.701 | |
| Strength | Time | F (1, 25) = 2.02 | p = 0.261 | |
| Group | F (1, 25) = 0.59 | p = 0.450 | ||
| Group × Time | F (1, 25) = 14.86 | p < 0.001 * | η2 = 0.240 | |
| Change of Direction | Time | F (1, 26) = 2.02 | p = 0.167 | |
| Group | F (1, 26) = 1.83 | p = 0.188 | ||
| Group × Time | F (1, 26) = 8.21 | p < 0.001 * | η2 = 0.373 | |
| Agility | Time | F (1, 26) = 0.26 | p = 0.615 | |
| Group | F (1, 26) = 0.68 | p = 0.419 | ||
| Group × Time | F (1, 26) = 0.89 | p = 0.354 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Myers, B.; Hanks, J. Effect of a Multi-Faceted Training Program on Falls in Senior Pickleball Players. Healthcare 2025, 13, 2298. https://doi.org/10.3390/healthcare13182298
Myers B, Hanks J. Effect of a Multi-Faceted Training Program on Falls in Senior Pickleball Players. Healthcare. 2025; 13(18):2298. https://doi.org/10.3390/healthcare13182298
Chicago/Turabian StyleMyers, Betsy, and June Hanks. 2025. "Effect of a Multi-Faceted Training Program on Falls in Senior Pickleball Players" Healthcare 13, no. 18: 2298. https://doi.org/10.3390/healthcare13182298
APA StyleMyers, B., & Hanks, J. (2025). Effect of a Multi-Faceted Training Program on Falls in Senior Pickleball Players. Healthcare, 13(18), 2298. https://doi.org/10.3390/healthcare13182298





