Development and Performance of an Artificial Intelligence-Based Deep Learning Model Designed for Evaluating Dental Ergonomics
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
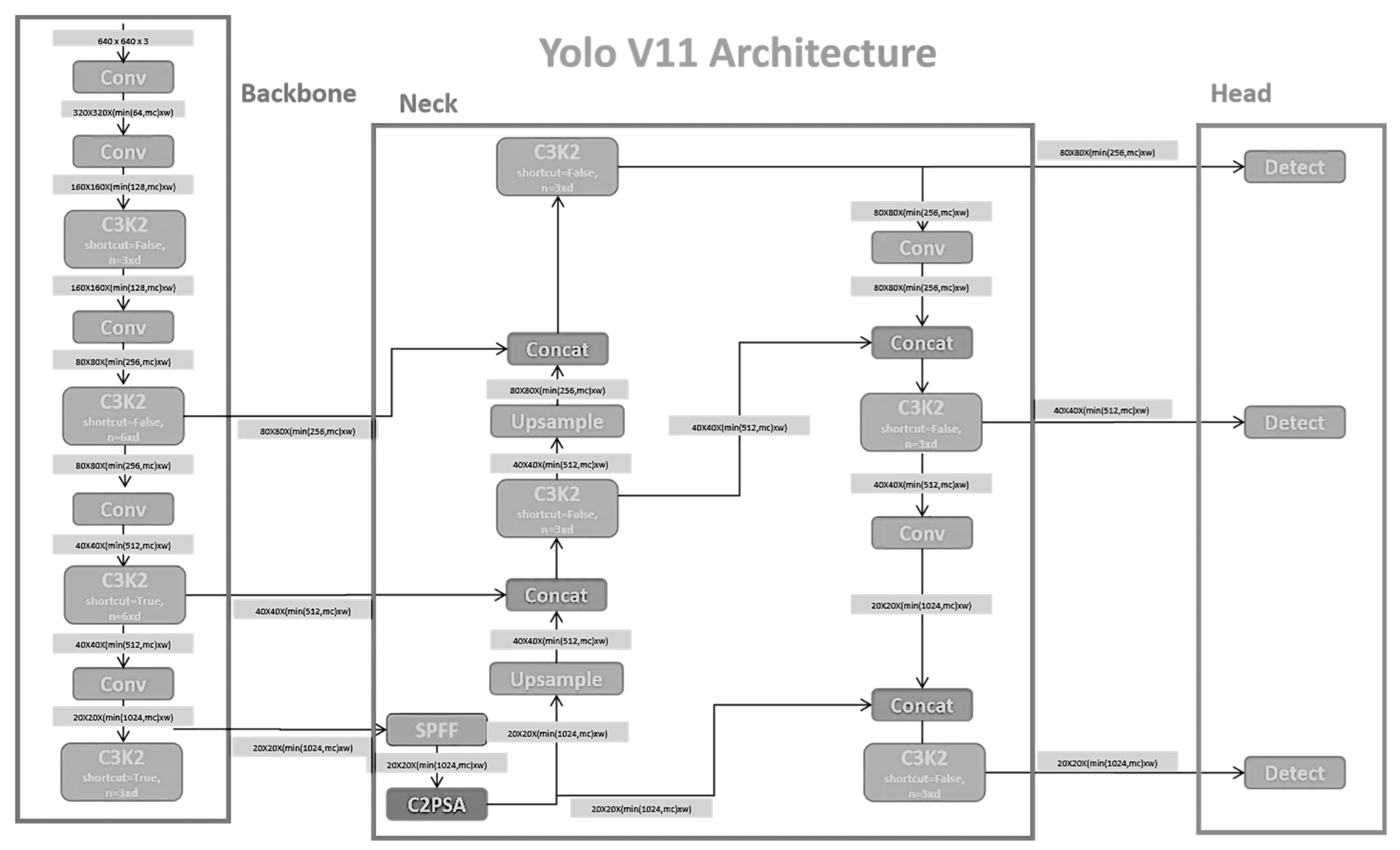
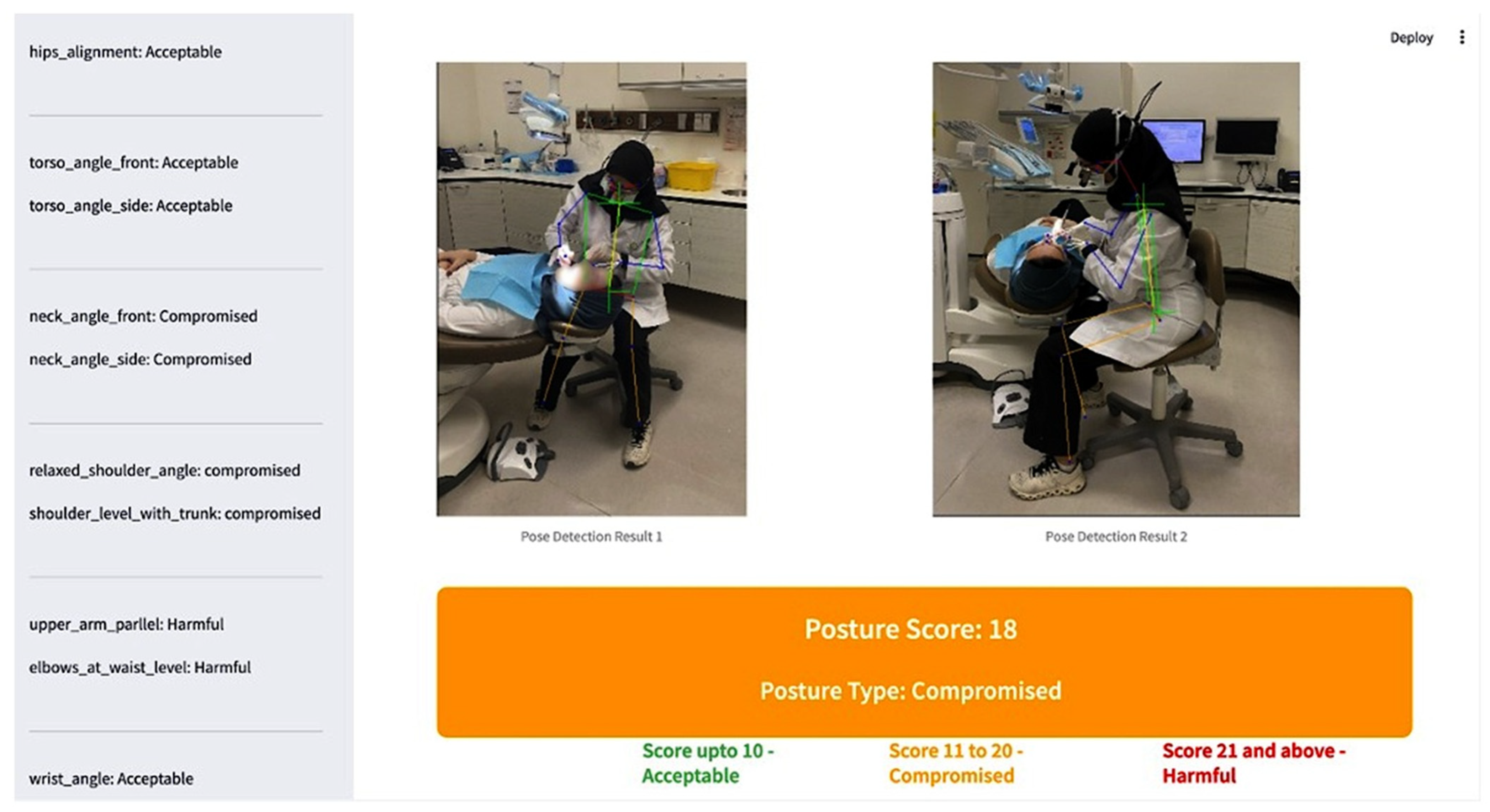
2.3. Model Development
2.4. Labelling of Data
2.5. Data Processing
2.6. Training and Testing
2.7. AI-Based SBK-DentErgo Model Performance Evaluation
2.8. Statistical Analysis and Evaluation Criteria
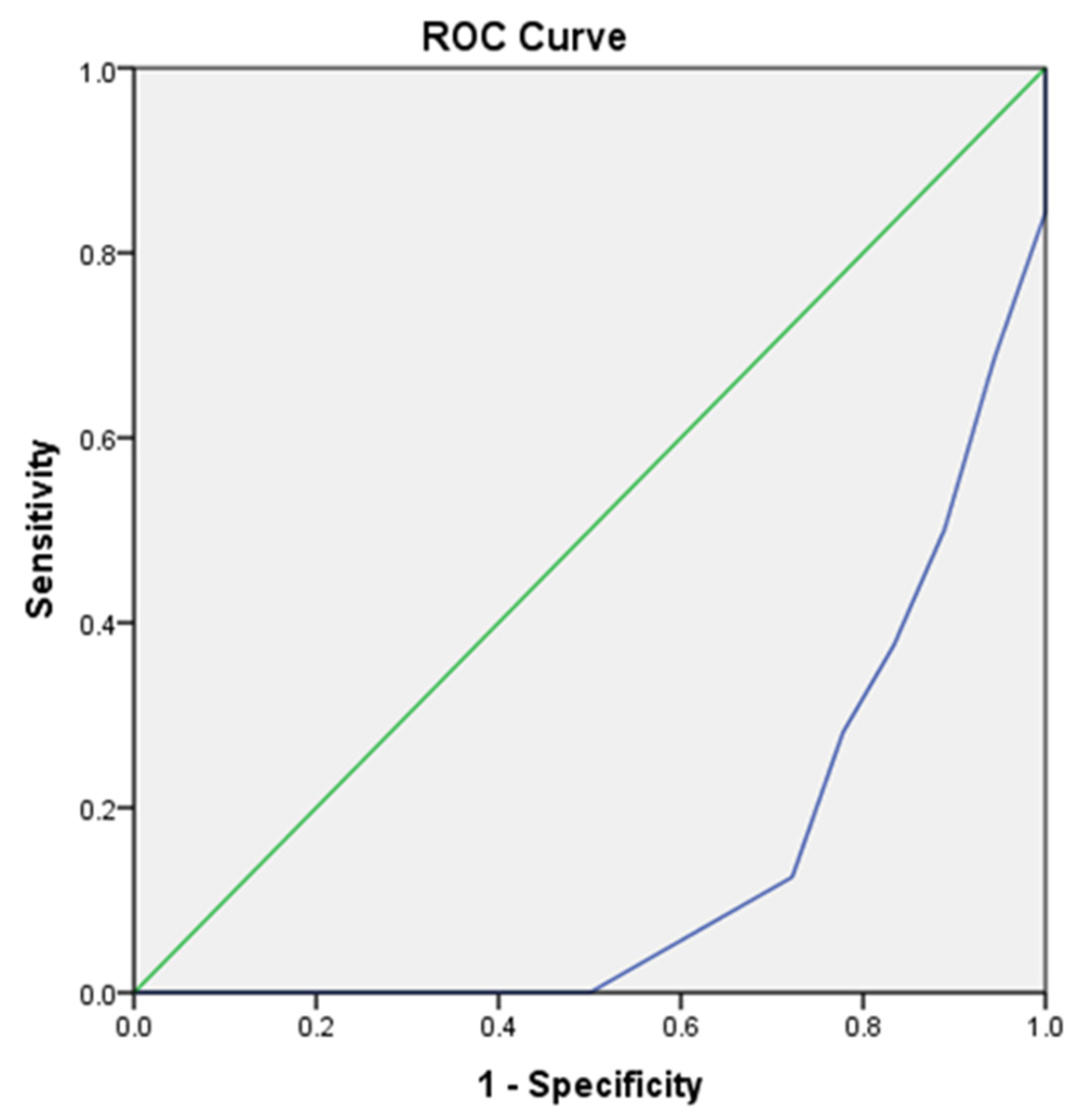
3. Results
4. Discussion
Implications and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| Conv | Convolutional Block |
| C3k2 | Cross-stage partial bottleneck with 3 convolution layers and kernel size 2 |
| Concat | Concatenation of feature maps from different scales. |
| Upsample | Bilinear (sometimes nearest-neighbor) upsampling to double feature map resolution. |
| SPPF/SPFF | Spatial Pyramid Pooling (Fast) captures multi-scale receptive fields by pooling at different kernel sizes. |
| C2PSA | Cross-Stage Partial with Partial Self-Attention (lightweight attention to refine features). |
References
- Fish, D.R.; Morris-Allen, D.M. Musculoskeletal Disorders in Dentists. N. Y. State Dent. J. 1998, 64, 44–48. [Google Scholar] [PubMed]
- Lindfors, P.; Von Thiele, U.; Lundberg, U. Work Characteristics and Upper Extremity Disorders in Female Dental Health Workers. J. Occup. Health 2006, 48, 192–197. [Google Scholar] [CrossRef]
- Nordander, C.; Ohlsson, K.; Åkesson, I.; Arvidsson, I.; Balogh, I.; Hansson, G.-Å.; Strömberg, U.; Rittner, R.; Skerfving, S. Risk of Musculoskeletal Disorders among Females and Males in Repetitive/Constrained Work. Ergonomics 2009, 52, 1226–1239. [Google Scholar] [CrossRef] [PubMed]
- Valachi, B.; Valachi, K. Mechanisms Leading to Musculoskeletal Disorders in Dentistry. J. Am. Dent. Assoc. 2003, 134, 1344–1350. [Google Scholar] [CrossRef]
- Gupta, A.; Ankola, A.V.; Hebbal, M. Dental Ergonomics to Combat Musculoskeletal Disorders: A Review. Int. J. Occup. Saf. Ergon. 2013, 19, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.G.; Zamparini, F.; Spinelli, A.; Risi, A.; Prati, C. Musculoskeletal Disorders among Italian Dentists and Dental Hygienists. Int. J. Environ. Res. Public Health 2021, 18, 2705. [Google Scholar] [CrossRef]
- AlSahiem, J.; Alghamdi, S.; AlQahtani, R.; Ibraheem Bin-Jardan, L.; Ibrahim Almadani, D.; Ahmed Farooqi, F.; Gaffar, B. Musculoskeletal Disorders among Dental Students: A Survey from Saudi Arabia. BMC Oral Health 2023, 23, 795. [Google Scholar] [CrossRef]
- Gupta, G.; Bhat, M.; Gupta, A.; Mohammed, T.; Bansal, N. Ergonomics in Dentistry. Int. J. Clin. Pediatr. Dent. 2014, 7, 30–34. [Google Scholar] [CrossRef]
- Abichandani, S.; Shaikh, S.; Nadiger, R. Carpal Tunnel Syndrome—An Occupational Hazard Facing Dentistry. Int. Dent. J. 2013, 63, 230–236. [Google Scholar] [CrossRef]
- Hayes, M.; Cockrell, D.; Smith, D. A Systematic Review of Musculoskeletal Disorders among Dental Professionals. Int. J. Dent. Hyg. 2009, 7, 159–165. [Google Scholar] [CrossRef]
- Soo, S.Y.; Ang, W.S.; Chong, C.H.; Tew, I.M.; Yahya, N.A. Occupational Ergonomics and Related Musculoskeletal Disorders among Dentists: A Systematic Review. Work 2022, 74, 469–476. [Google Scholar] [CrossRef]
- Chopra, A.; Devi, S. Musculoskeletal Disorders in Dentistry—A Review. JSM Dent. 2014, 2, 1032. [Google Scholar]
- Kalluri, A.; Puranik, M.P.; Uma, S.R. Musculoskeletal Disorders in Dental Workplace: A Comprehensive Review. Int. J. Appl. Dent. Sci. 2018, 4, 140–145. [Google Scholar]
- Ratushnyi, R.; Stakhanska, O. Ergonomic Interventions and Endodontic Treatment Outcomes: An Analysis of Dentist Working Posture and Error Rates. Saudi Dent. J. 2024, 36, 466–470. [Google Scholar] [CrossRef] [PubMed]
- Lazăr, A.M.; Repanovici, A.; Baritz, M.I.; Scutariu, M.M.; Tătaru, A.I.; Pantea, I. Postural Risks in Dental Practice: An Assessment of Musculoskeletal Health. Sensors 2024, 24, 6240. [Google Scholar] [CrossRef]
- Muthuraj, T.S.; Raja, J.; James, J.R.; Mohan, P.; Subramnian, D.; Varatharajan, A. Standardized Photometric Assessment Method: A Novel Approach for the Analysis of Dental Ergonomic Posture. J. Indian Soc. Periodontol. 2020, 24, 227–232. [Google Scholar] [CrossRef]
- Garbin, A.J.; Garbin, C.A.S.; Diniz, D.G.; Yarid, S.D. Dental Students’ Knowledge of Ergonomic Postural Requirements and Their Application during Clinical Care. Eur. J. Dent. Educ. 2011, 15, 31–35. [Google Scholar] [CrossRef]
- Maillet, J.P.; Millar, A.M.; Burke, J.M.; Maillet, M.A.; Maillet, W.A.; Neish, N.R. Effect of Magnification Loupes on Dental Hygiene Student Posture. J. Dent. Educ. 2008, 72, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Branson, B.G.; Bray, K.K.; Gadbury-Amyot, C.; Holt, L.A.; Keselyak, N.T.; Mitchell, T.V.; Williams, K.B. Effect of Magnification Lenses on Student Operator Posture. J. Dent. Educ. 2004, 68, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Partido, B.B. Longitudinal Effects of Utilising Photography on the Accuracy of Ergonomic Self-Assessments amongst Dental Hygiene Students. Eur. J. Dent. Educ. 2019, 24, 63–70. [Google Scholar] [CrossRef]
- Khanagar, S.B.; Al-Ehaideb, A.; Maganur, P.C.; Vishwanathaiah, S.; Patil, S.; Baeshen, H.A.; Sarode, S.C.; Bhandi, S. Developments, Application, and Performance of Artificial Intelligence in Dentistry—a Systematic Review. J. Dent. Sci. 2021, 16, 508–522. [Google Scholar] [CrossRef]
- Ding, H.; Wu, J.; Zhao, W.; Matinlinna, J.P.; Burrow, M.F.; Tsoi, J.K.H. Artificial Intelligence in Dentistry—A Review. Front. Dent. Med. 2023, 4, 1085251. [Google Scholar] [CrossRef] [PubMed]
- Pîrvu, C.; Pătraşcu, I.; Pîrvu, D.; Ionescu, C. The Dentist’s Operating Posture—Ergonomic Aspects. J. Med. Life 2014, 7, 177–182. [Google Scholar]
- Zúniga, I.A.C.; Malespín, N.L.S.; Vílchez, A.L.V.; Frenky, O.J.D.; Hong, G.; Sáenz, J.R.V. Evaluation of the Ergonomic Sitting Position Adopted by Dental Students While Using Dental Simulators. J. Dent. Sci. 2023, 18, 526–533. [Google Scholar] [CrossRef]
- Khanam, R.; Hussain, M. YOLOV11: An overview of the key architectural enhancements. arXiv 2024, arXiv:2410.17725. Available online: https://arxiv.org/pdf/2410.17725v1 (accessed on 12 March 2025). [CrossRef]
- Rao, S.N. YOLOv11 Architecture Explained: Next-Level Object Detection with Enhanced Speed and Accuracy. Available online: https://medium.com/@nikhil-rao-20/yolov11-explained-next-level-object-detection-with-enhanced-speed-and-accuracy-2dbe2d376f71 (accessed on 15 March 2025).
- Branson, B.G.; Williams, K.B.; Bray, K.K.; Mcllnay, S.L.; Dickey, D. Validity and Reliability of a Dental Operator Posture Assessment Instrument (PAI). J. Dent. Hyg. 2002, 76, 255–261. [Google Scholar] [PubMed]
- Nield-Gehrig, J.S.; Gehrig, J.S. Fundamentals of Periodontal Instrumentation, 4th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2000; Volume 1, pp. 15–17. ISBN 9780781728607/0781728606. [Google Scholar]
- Parikh, R.; Mathai, A.; Parikh, S.; Chandra Sekhar, G.; Thomas, R. Understanding and Using Sensitivity, Specificity and Predictive Values. Indian J. Ophthalmol. 2008, 56, 45–50. [Google Scholar] [CrossRef] [PubMed]
- Lietz, J.; Kozak, A.; Nienhaus, A. Prevalence and Occupational Risk Factors of Musculoskeletal Diseases and Pain among Dental Professionals in Western Countries: A Systematic Literature Review and Meta-Analysis. PLoS ONE 2018, 13, e0208628. [Google Scholar] [CrossRef]
- Chenna, D.; Pentapati, K.C.; Kumar, M.; Madi, M.; Siddiq, H. Prevalence of Musculoskeletal Disorders among Dental Healthcare Providers: A Systematic Review and Meta-Analysis. F1000Research 2022, 11, 1062. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Prevalence of Body Area Work-Related Musculoskeletal Disorders among Healthcare Professionals: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 841. [Google Scholar] [CrossRef]
- De Sio, S.; Traversini, V.; Rinaldo, F.; Colasanti, V.; Buomprisco, G.; Perri, R.; Mormone, F.; La Torre, G.; Guerra, F. Ergonomic Risk and Preventive Measures of Musculoskeletal Disorders in the Dentistry Environment: An Umbrella Review. PeerJ 2018, 6, e4154. [Google Scholar] [CrossRef]
- Hussein, A.; Mando, M.; Radisauskas, R. Work-Related Musculoskeletal Disorders among Dentists in the United Arab Emirates: A Cross-Sectional Study. Medicina 2022, 58, 1744. [Google Scholar] [CrossRef] [PubMed]
- Alnaser, M.Z.; Almaqsied, A.M.; Alshatti, S.A. Risk Factors for Work-Related Musculoskeletal Disorders of Dentists in Kuwait and the Impact on Health and Economic Status. Work 2021, 68, 213–221. [Google Scholar] [CrossRef]
- Partido, B. Dental Hygiene Students’ Self-Assessment of Ergonomics Utilizing Photography. J. Dent. Educ. 2017, 81, 1194–1202. [Google Scholar] [CrossRef] [PubMed]
- Partido, B.B.; Wright, B.M. Self-Assessment of Ergonomics amongst Dental Students Utilising Photography: RCT. Eur. J. Dent. Educ. 2018, 22, 223–233. [Google Scholar] [CrossRef]
- Song, L.; Yu, G.; Yuan, J.; Liu, Z. Human Pose Estimation and Its Application to Action Recognition: A Survey. J. Vis. Commun. Image Represent. 2021, 76, 103055. [Google Scholar] [CrossRef]
- Ji, X.; Fang, Q.; Dong, J.; Shuai, Q.; Jiang, W.; Zhou, X. A Survey on Monocular 3D Human Pose Estimation. Virtual Real. Intell. Hardw. 2020, 2, 471–500. [Google Scholar] [CrossRef]
- Chakraborty, B.K.; Sarma, D.; Bhuyan, M.K.; MacDorman, K.F. Review of Constraints on Vision-Based Gesture Recognition for Human–Computer Interaction. IET Comput. Vis. 2018, 12, 3–15. [Google Scholar] [CrossRef]
- Angelini, F.; Fu, Z.; Long, Y.; Shao, L.; Naqvi, S.M. 2D Pose-Based Real-Time Human Action Recognition with Occlusion-Handling. IEEE Trans. Multimed. 2020, 22, 1433–1446. [Google Scholar] [CrossRef]
- Lafayette, T.B.d.G.; Kunst, V.H.d.L.; Melo, P.V.d.S.; Guedes, P.d.O.; Teixeira, J.M.X.N.; Vasconcelos, C.R.d.; Teichrieb, V.; da Gama, A.E.F. Validation of Angle Estimation Based on Body Tracking Data from RGB-D and RGB Cameras for Biomechanical Assessment. Sensors 2022, 23, 3. [Google Scholar] [CrossRef]
- Groos, D.; Ramampiaro, H.; Ihlen, E.A. EfficientPose: Scalable Single-Person Pose Estimation. Appl. Intell. 2020, 51, 2518–2533. [Google Scholar] [CrossRef]
- Samkari, E.; Arif, M.; Alghamdi, M.; Al Ghamdi, M.A. Human Pose Estimation Using Deep Learning: A Systematic Literature Review. Mach. Learn. Knowl. Extr. 2023, 5, 1612–1659. [Google Scholar] [CrossRef]
- Moreira, R.; Fialho, R.; Teles, A.S.; Bordalo, V.; Vasconcelos, S.S.; de Morais Gouveia, G.P.; Bastos, V.H.; Teixeira, S. A Computer Vision-Based Mobile Tool for Assessing Human Posture: A Validation Study. Comput. Methods Programs Biomed. 2022, 214, 106565. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Caballero, A.-J.; Gómez-Palencia, I.-P.; Díaz-Cárdenas, S. Ergonomic Factors That Cause the Presence of Pain Muscle in Students of Dentistry. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e906–e911. [Google Scholar] [CrossRef]
- Dable, R.A.; Wasnik, P.B.; Yeshwante, B.J.; Musani, S.I.; Patil, A.K.; Nagmode, S.N. Postural Assessment of Students Evaluating the Need of Ergonomic Seat and Magnification in Dentistry. J. Indian Prosthodont. Soc. 2014, 14, 51–58. [Google Scholar] [CrossRef]
- Ng, A.; Hayes, M.; Polster, A. Musculoskeletal Disorders and Working Posture among Dental and Oral Health Students. Healthcare 2016, 4, 13. [Google Scholar] [CrossRef]
- Khan, S.A.; Yee Chew, K. Effect of Working Characteristics and Taught Ergonomics on the Prevalence of Musculoskeletal Disorders amongst Dental Students. BMC Musculoskelet. Disord. 2013, 14, 118. [Google Scholar] [CrossRef]

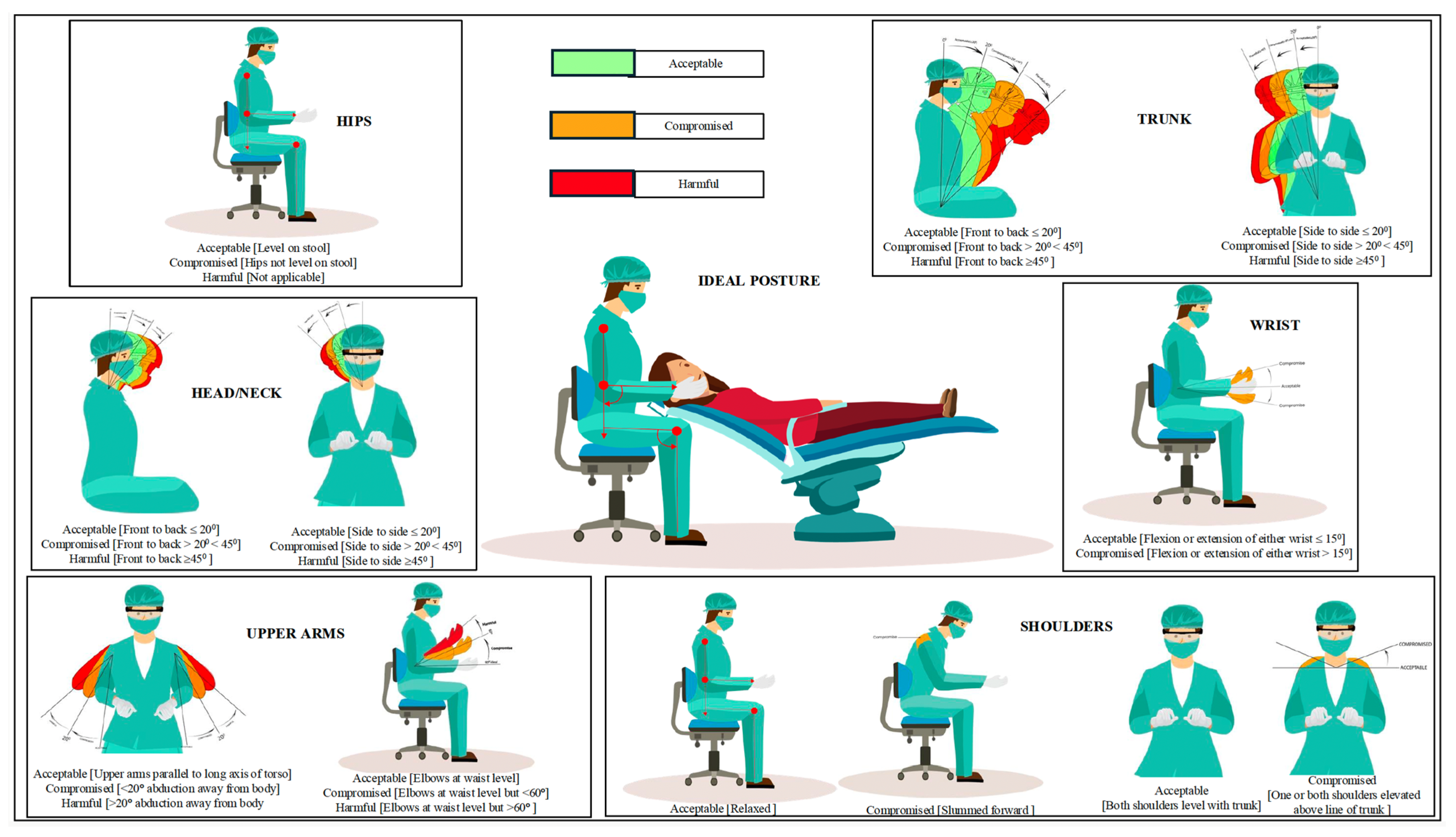

| Posture Aspects | Scoring Criteria | ||
|---|---|---|---|
| Acceptable (1 Point) | Compromised (2 Points) | Harmful (3 Point) | |
| hips | Level on stool | Hips not level on stool | Not applicable |
| trunk | Front to back ≤ 20° | 20° < Front to back < 45° | Front to back ≥ 45° |
| Side to side ≤ 20° | 20° < Side to side < 45° | Side to side ≥ 45° | |
| head/neck | Front to back ≤ 20° | 20° < Front to back < 45° | Front to back ≥ 45° |
| Side to side ≤ 20° | 20° < Side to side < 45° | Side to side ≥ 45° | |
| shoulders | Relaxed | Slummed forward | Not applicable |
| Both shoulders level with trunk | One or both shoulders elevated above line of trunk | Not applicable | |
| upper arms | Upper arms parallel to long axis of torso | <20° abduction away from body | >20° abduction away from body |
| Elbows at waist level | Elbows at waist level but <60° | Elbows at waist level but >60° | |
| wrist | Flexion or extension of either wrist ≤ 15° | Flexion or extension of either wrist > 15° | Not applicable |
| Cohen’s Kappa Statistics for Inter-Rater Reliability of Test Set Evaluated by Calibrated Principal Evaluators | ||||||
|---|---|---|---|---|---|---|
| Evaluator | Total Sets Evaluated | Kappa Value | Sig | |||
| Principal Evaluators | 50 | 0.924 | 0.000 * | |||
| Cohen’s Kappa statistics for inter-rater reliability of 50 sets scored by an AI model against the scores generated by calibrated principal evaluators | ||||||
| Evaluator | Total Sets Evaluated | Kappa Value | Sig | |||
| AI-based model | 50 | 0.922 | 0.000 * | |||
| Cohen’s Kappa Statistics for Each of the Ten Sets Scored by Human Evaluators Against the Scores Generated by the AI Model | ||||||
| Evaluator | Total Sets Evaluated | Kappa Value | Sig | |||
| Evaluator 1 | 10 | −0.071 | 0.598 | |||
| Evaluator 2 | 10 | 0.000 | 1.000 | |||
| Evaluator 3 | 10 | −0.053 | 0.725 | |||
| Evaluator 4 | 10 | −0.053 | 0.725 | |||
| Evaluator 5 | 10 | 0.429 | 0.050 | |||
| Intra Class Correlation (ICC)-Intra Rater Reliability Assessment (IRR) | ||||||
| Evaluators (1st vs. 2nd evaluation) | ICC-Single Measures | ICC Averaged Measures | F Test Value | p Value | Average Measures | |
| Lower 95% CI | Upper 95% CI | |||||
| Evaluator 1 | −0.286 | −0.800 | 0.600 | 0.771 | −0.897 | 0.440 |
| Evaluator 2 | 0.053 | 0.100 | 1.111 | 0.439 | −0.563 | 0.634 |
| Evaluator 3 | 0.050 | 0.092 | 1.111 | 0.439 | −2.580 | 0.776 |
| Evaluator 4 | 0.000 | 0.000 | 1.000 | 0.500 | −4.189 | 0.765 |
| Evaluator 5 | 0.426 | 0.597 | 2.379 | 0.106 | −0.740 | 0.902 |
| AI | 1.000 | 1.000 | 25.000 | 0.000 * | - | - |
| Calibrated Evaluators and AI Model Diagnosis of Operator Ergonomics | |||||
|---|---|---|---|---|---|
| AI-Based Diagnosis | Total | ||||
| Positive | Negative | ||||
| Calibrated Evaluators | Positive | Count | 42 | 1 | 43 |
| % within Calibrated Evaluators | 97.7% | 2.3% | 100.0% | ||
| % within AI Scores | 97.7% | 14.3% | 86.0% | ||
| Negative | Count | 1 | 6 | 7 | |
| % within Calibrated Evaluators | 14.3% | 85.7% | 100.0% | ||
| % within AI Scores | 2.3% | 85.7% | 14.0% | ||
| Total | Count | 43 | 7 | 50 | |
| % within Calibrated Evaluators | 86.0% | 14.0% | 100.0% | ||
| % within AI Scores | 100.0% | 100.0% | 100.0% | ||
| Human Evaluation and AI-Based Diagnosis of Operator Ergonomics | |||||
| AI-Based Diagnosis | Total | ||||
| Positive | Negative | ||||
| Human Evaluation | Positive | Count | 8 | 10 | 18 |
| % within Human Evaluation | 44.4% | 55.6% | 100.0% | ||
| % within AI-based diagnosis | 20.5% | 90.9% | 36.0% | ||
| Negative | Count | 31 | 1 | 32 | |
| % within Human Evaluation | 96.9% | 3.1% | 100.0% | ||
| % within AI-based diagnosis | 79.5% | 9.1% | 64.0% | ||
| Total | Count | 39 | 11 | 50 | |
| % within Human Evaluation | 78.0% | 22.0% | 100.0% | ||
| % within AI-based diagnosis | 100.0% | 100.0% | 100.0% | ||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Chi-Square | df | Sig. | ||||||
| (PPV) | 0.977 | 0.023 | 0.902 | 0.999 | 180.60 | 1 | 0.000 * | |||
| (NPV) | 0.857 | 0.132 | 0.506 | 0.991 | 42.000 | 1 | 0.000 * | |||
| Specificity | ||||||||||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | ||||||
| Lower | Upper | Chi-Square | df | Sig. | ||||||
| (Intercept) | 0.857 | 0.132 | 0.506 | 0.991 | 42.000 | 1 | 0.000 * | |||
| Sensitivity | ||||||||||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | ||||||
| Lower | Upper | Chi-Square | df | Sig. | ||||||
| (Intercept) | 0.977 | 0.023 | 0.902 | 0.999 | 180.60 | 1 | 0.000 * | |||
| Risk Estimate | ||||||||||
| Value | 95% Confidence Interval | |||||||||
| Lower | Upper | |||||||||
| Odds Ratio for Predicted (1/2) | 252.000 | 13.855 | 458.353 | |||||||
| For Cohort Actual = 1 | 6.837 | 1.113 | 41.995 | |||||||
| For Cohort Actual = 2 | 0.027 | 0.004 | 0.193 | |||||||
| N of Valid Cases | 50 | |||||||||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Chi-Square | df | Sig. | |||||||
| (PPV) | 0.444 | 0.117 | 0.234 | 0.670 | 14.400 | 1 | 0.000 * | ||||
| (NPV) | 0.031 | 0.308 | 0.002 | 0.130 | 1.032 | 1 | 0.310 | ||||
| Specificity | |||||||||||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | |||||||
| Lower | Upper | Chi-Square | df | Sig. | |||||||
| (Intercept) | 0.091 | 0.086 | 0.005 | 0.343 | 1.100 | 1 | 0.294 | ||||
| Sensitivity | |||||||||||
| Parameter | B | Std. Error | 95% Profile Likelihood Confidence Interval | Hypothesis Test | |||||||
| Lower | Upper | Chi-Square | df | Sig. | |||||||
| (Intercept) | 0.205 | 0.064 | 0.099 | 0.348 | 10.065 | 1 | 0.002 * | ||||
| Risk Estimate | |||||||||||
| Value | 95% Confidence Interval | ||||||||||
| Lower | Upper | ||||||||||
| Odds Ratio for Predicted (1/2) | 0.026 | 0.003 | 0.232 | ||||||||
| For cohort Actual = 1 | 0.226 | 0.118 | 0.430 | ||||||||
| For cohort Actual = 2 | 8.744 | 1.340 | 57.046 | ||||||||
| N of Valid Cases | 50 | ||||||||||
| Summary of Outcomes in AI-Based Evaluation | ||||
|---|---|---|---|---|
| Outcome | N | |||
| Positive | 43 | |||
| Negative | 07 | |||
| Summary of Outcomes in Human Evaluation | ||||
| Outcome | N | |||
| Positive | 32 | |||
| Negative | 18 | |||
| Area Under the Curve | ||||
| Test Result Variable(s): AI | ||||
| AI-based Diagnosis Area Under the Curve | Std. Error a | Asymptotic Sig. b | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||
| 0.917 | 0.079 | 0.000 | 0.762 | 1.000 |
| Test Result Variable(s): Human Evaluation Score | ||||
| Human Evaluation Area Under the Curve | Std. Error a | Asymptotic Sig. b | Asymptotic 95% Confidence Interval | |
| Lower Bound | Upper Bound | |||
| 0.143 | 0.059 | 0.000 | 0.027 | 0.259 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khanagar, S.B.; Alshehri, A.; Albalawi, F.; Kalagi, S.; Alghilan, M.A.; Awawdeh, M.; Iyer, K. Development and Performance of an Artificial Intelligence-Based Deep Learning Model Designed for Evaluating Dental Ergonomics. Healthcare 2025, 13, 2277. https://doi.org/10.3390/healthcare13182277
Khanagar SB, Alshehri A, Albalawi F, Kalagi S, Alghilan MA, Awawdeh M, Iyer K. Development and Performance of an Artificial Intelligence-Based Deep Learning Model Designed for Evaluating Dental Ergonomics. Healthcare. 2025; 13(18):2277. https://doi.org/10.3390/healthcare13182277
Chicago/Turabian StyleKhanagar, Sanjeev B., Aram Alshehri, Farraj Albalawi, Sara Kalagi, Maryam A. Alghilan, Mohammed Awawdeh, and Kiran Iyer. 2025. "Development and Performance of an Artificial Intelligence-Based Deep Learning Model Designed for Evaluating Dental Ergonomics" Healthcare 13, no. 18: 2277. https://doi.org/10.3390/healthcare13182277
APA StyleKhanagar, S. B., Alshehri, A., Albalawi, F., Kalagi, S., Alghilan, M. A., Awawdeh, M., & Iyer, K. (2025). Development and Performance of an Artificial Intelligence-Based Deep Learning Model Designed for Evaluating Dental Ergonomics. Healthcare, 13(18), 2277. https://doi.org/10.3390/healthcare13182277





