Adherence to the Mediterranean Diet Across the League of Arab States: A Systematic Review
Abstract
1. Introduction
2. Methods
2.1. Literature Search
2.2. Selection Criteria for Studies
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
3. Results
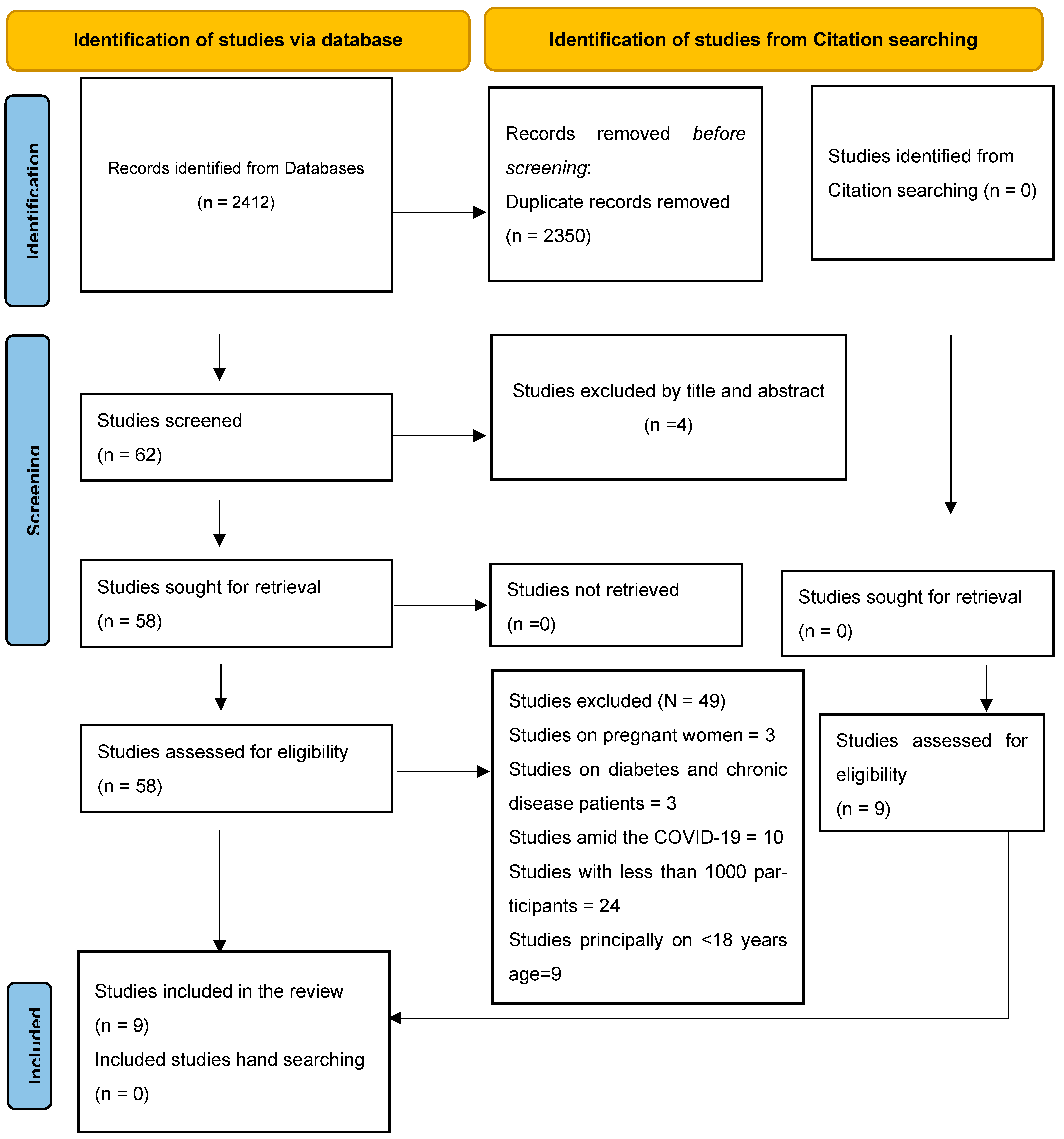
3.1. Study Selection
3.2. Study Characteristics
3.3. MD Adherence Levels
3.4. MD Adherence Subgroups
3.5. Quality Assessment of the Included Studies
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Benhammou, S.; Heras-González, L.; Ibáñez-Peinado, D.; Barceló, C.; Hamdan, M.; Rivas, A.; Mariscal-Arcas, M.; Olea-Serrano, F.; Monteagudo, C. Comparison of Mediterranean diet compliance between European and non-European populations in the Mediterranean basin. Appetite 2016, 107, 521–526. [Google Scholar] [CrossRef]
- Kyriacou, A.; Evans, J.M.; Economides, N.; Kyriacou, A. Adherence to the Mediterranean diet by the Greek and Cypriot population: A systematic review. Eur. J. Public Health 2015, 25, 1012–1018. [Google Scholar] [CrossRef]
- Vilarnau, C.; Stracker, D.M.; Funtikov, A.; da Silva, R.; Estruch, R.; Bach-Faig, A. Worldwide adherence to Mediterranean Diet between 1960 and 2011. Eur. J. Clin. Nutr. 2019, 72, 83–91. [Google Scholar] [CrossRef]
- Romagnolo, D.F.; Selmin, O.I. Mediterranean Diet and Prevention of Chronic Diseases. Nutr. Today 2017, 52, 208–222. [Google Scholar] [CrossRef]
- Dominguez, L.J.; Di Bella, G.; Veronese, N.; Barbagallo, M. Impact of Mediterranean Diet on Chronic Non-Communicable Diseases and Longevity. Nutrients 2021, 13, 2028. [Google Scholar] [CrossRef] [PubMed]
- Obeid, C.A.; Gubbels, J.S.; Jaalouk, D.; Kremers, S.P.J.; Oenema, A. Adherence to the Mediterranean diet among adults in Mediterranean countries: A systematic literature review. Eur. J. Nutr. 2022, 61, 3327–3344. [Google Scholar] [CrossRef] [PubMed]
- Estruch, R.; Ros, E. The role of the Mediterranean diet on weight loss and obesity-related diseases. Rev. Endocr. Metab. Disord. 2020, 21, 315–327. [Google Scholar] [CrossRef] [PubMed]
- Santulli, G.; Pascale, V.; Finelli, R.; Visco, V.; Giannotti, R.; Massari, A.; Morisco, C.; Ciccarelli, M.; Illario, M.; Iaccarino, G.; et al. We are What We Eat: Impact of Food from Short Supply Chain on Metabolic Syndrome. J. Clin. Med. 2019, 8, 2061. [Google Scholar] [CrossRef] [PubMed]
- Salas-Salvadó, J.; Guasch-Ferré, M.; Lee, C.-H.; Estruch, R.; Clish, C.B.; Ros, E. Protective effects of the Mediterranean diet on type 2 diabetes and metabolic syndrome. J. Nutr. 2016, 146, 920S–927S. [Google Scholar] [CrossRef]
- Chen, H.-W.; Liu, K.; Cao, B.-F.; Zhong, Q.; Zhou, R.; Li, L.-H.; Wang, S.-A.; Wei, Y.-F.; Liu, H.-M.; Wu, X.-B. Combined associations of visceral adipose tissue and adherence to a Mediterranean lifestyle with T2D and diabetic microvascular complications among individuals with prediabetes. Cardiovasc. Diabetol. 2024, 23, 201. [Google Scholar] [CrossRef]
- Qu, C.; Zhao, J.; Lai, J.; Wu, X.; Huang, P.; Zhu, T.; Li, Y.; Liu, T.; Yuan, J.; Wang, N.; et al. Adherence to a Mediterranean diet is associated with a lower risk of diabetic kidney disease among individuals with hyperglycemia: A prospective cohort study. BMC Med. 2024, 22, 224. [Google Scholar] [CrossRef] [PubMed]
- Temple, N.J.; Guercio, V.; Tavani, A. The Mediterranean diet and cardiovascular disease: Gaps in the evidence and research challenges. Cardiol. Rev. 2019, 27, 127–130. [Google Scholar] [CrossRef] [PubMed]
- Bonekamp, N.E.; Visseren, F.L.J.; van der Schouw, Y.T.; van der Meer, M.G.; Teraa, M.; Ruigrok, Y.M.; Geleijnse, J.M.; Koopal, C. Cost-effectiveness of Mediterranean diet and physical activity in secondary cardiovascular disease prevention: Results from the UCC-SMART cohort study. Eur. J. Prev. Cardiol. 2024, 31, 1460–1468. [Google Scholar] [CrossRef] [PubMed]
- Mentella, M.C.; Scaldaferri, F.; Ricci, C.; Gasbarrini, A.; Miggiano, G.A.D. Cancer and Mediterranean diet: A review. Nutrients 2019, 11, 2059. [Google Scholar] [CrossRef]
- Franquesa, M.; Pujol-Busquets, G.; García-Fernández, E.; Rico, L.; Shamirian-Pulido, L.; Aguilar-Martínez, A.; Medina, F.X.; Serra-Majem, L.; Bach-Faig, A. Mediterranean diet and cardiodiabesity: A systematic review through evidence-based answers to key clinical questions. Nutrients 2019, 11, 655. [Google Scholar] [CrossRef]
- Shafiei, F.; Salari-Moghaddam, A.; Larijani, B.; Esmaillzadeh, A. Adherence to the Mediterranean diet and risk of depression: A systematic review and updated meta-analysis of observational studies. Nutr. Rev. 2019, 77, 230–239. [Google Scholar] [CrossRef]
- Petersson, S.D.; Philippou, E. Mediterranean Diet, Cognitive Function, and Dementia: A Systematic Review of the Evidence. Adv. Nutr. 2016, 7, 889–904. [Google Scholar] [CrossRef]
- Jennings, A.; Shannon, O.M.; Gillings, R.; Lee, V.; Elsworthy, R.; Bundy, R.; Rao, G.; Hanson, S.; Hardeman, W.; Paddick, S.M.; et al. Effectiveness and feasibility of a theory-informed intervention to improve Mediterranean diet adherence, physical activity and cognition in older adults at risk of dementia: The MedEx-UK randomised controlled trial. BMC Med. 2024, 22, 600. [Google Scholar] [CrossRef]
- Alufer, L.; Tsaban, G.; Rinott, E.; Kaplan, A.; Meir, A.Y.; Zelicha, H.; Ceglarek, U.; Isermann, B.; Blüher, M.; Stumvoll, M.; et al. Long-term green-Mediterranean diet may favor fasting morning cortisol stress hormone; the DIRECT-PLUS clinical trial. Front. Endocrinol. 2023, 14, 1243910. [Google Scholar] [CrossRef]
- Sofi, F.; Cesari, F.; Abbate, R.; Gensini, G.F.; Casini, A. Adherence to Mediterranean diet and health status: Meta-analysis. BMJ 2008, 337, a1344. [Google Scholar] [CrossRef]
- Sofi, F.; Macchi, C.; Abbate, R.; Gensini, G.F.; Casini, A. Mediterranean diet and health. Biofactors 2013, 39, 335–342. [Google Scholar] [CrossRef]
- Soltani, S.; Jayedi, A.; Shab-Bidar, S.; Becerra-Tomás, N.; Salas-Salvadó, J. Adherence to the Mediterranean Diet in Relation to All-Cause Mortality: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Adv. Nutr. 2019, 10, 1029–1039. [Google Scholar] [CrossRef] [PubMed]
- Santonocito, D.; Montenegro, L.; Puglia, C. Mediterranean Food By-products as a Valuable Source of Bioactive Compounds with Health Properties. Curr. Med. Chem. 2024, 32, 4154–4175. [Google Scholar] [CrossRef] [PubMed]
- Tsofliou, F.; Vlachos, D.; Hughes, C.; Appleton, K.M. Barriers and facilitators associated with the adoption of and adherence to a Mediterranean style diet in adults: A systematic review of published observational and qualitative studies. Nutrients 2022, 14, 4314. [Google Scholar] [CrossRef]
- Sam-Yellowe, T.Y. Nutritional Barriers to the Adherence to the Mediterranean Diet in Non-Mediterranean Populations. Foods 2024, 13, 1750. [Google Scholar] [CrossRef] [PubMed]
- Martínez-González, M.Á.; Hershey, M.S.; Zazpe, I.; Trichopoulou, A. Transferability of the Mediterranean Diet to Non-Mediterranean Countries. What Is and What Is Not the Mediterranean Diet. Nutrients 2017, 9, 1226. [Google Scholar] [CrossRef]
- Middleton, G.; Keegan, R.; Smith, M.F.; Alkhatib, A.; Klonizakis, M. Implementing a Mediterranean diet intervention into a RCT: Lessons learned from a non-Mediterranean based country. J. Nutr. Health Aging 2015, 19, 1019–1022. [Google Scholar] [CrossRef]
- Knight, C.J.; Jackson, O.; Rahman, I.; Burnett, D.O.; Frugé, A.D.; Greene, M.W. The Mediterranean Diet in the Stroke Belt: A Cross-Sectional Study on Adherence and Perceived Knowledge, Barriers, and Benefits. Nutrients 2019, 11, 1847. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Mattei, J. Mediterranean Diet and Cardiometabolic Diseases in Racial/Ethnic Minority Populations in the United States. Nutrients 2018, 10, 352. [Google Scholar] [CrossRef]
- Barakat, H. The Arab World: Society, Culture, and State; University of California Press: Oakland, CA, USA, 1993. [Google Scholar]
- Al-Shamsi, S.; Regmi, D.; Govender, R.D. Incidence of cardiovascular disease and its associated risk factors in at-risk men and women in the United Arab Emirates: A 9-year retrospective cohort study. BMC Cardiovasc. Disord. 2019, 19, 148. [Google Scholar] [CrossRef]
- Al-Muftah, M.; Al-Ejeh, F. Cancer Incidence and Mortality Estimates in Arab Countries in 2018: A GLOBOCAN Data Analysis. Cancer Epidemiol Biomark. Prev. 2023, 32, 1738–1746. [Google Scholar] [CrossRef]
- El-Kebbi, I.M.; Bidikian, N.H.; Hneiny, L.; Nasrallah, M.P. Epidemiology of type 2 diabetes in the Middle East and North Africa: Challenges and call for action. World J. Diabetes 2021, 12, 1401–1425. [Google Scholar] [CrossRef]
- Aidoud, A.; Ziane, E.; Vara, L.; Terrón Sánchez, M.P.; Garrido Álvarez, M.; Rodríguez Moratinos, A.B.; Carrasco Romero, C. Changes in Mediterranean dietary pattern of university students: A comparative study between Spain and Algeria. Nutr. Clin. Y Diet. Hosp. 2019, 39, 26–33. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Blair, I.; Grivna, M.; Sharif, A.A. The “Arab World” is not a useful concept when addressing challenges to public health, public health education, and research in the Middle East. Front. Public Health 2014, 2, 30. [Google Scholar] [CrossRef]
- Cleveland Clinic. Gestational Diabetes. Available online: https://my.clevelandclinic.org/health/diseases/9012-gestational-diabetes (accessed on 13 October 2024).
- Aoun, C.; Papazian, T.; Helou, K.; El Osta, N.; Khabbaz, L.R. Comparison of five international indices of adherence to the Mediterranean diet among healthy adults: Similarities and differences. Nutr. Res. Pract. 2019, 13, 333–343. [Google Scholar] [CrossRef]
- Altavilla, C.; Caballero-Pérez, P. An update of the KIDMED questionnaire, a Mediterranean Diet Quality Index in children and adolescents. Public Health Nutr. 2019, 22, 2543–2547. [Google Scholar] [CrossRef]
- Chiriacò, M.; Tubili, C.; Bo, S.; Parillo, M.; Vetrani, C.; Mazzotti, A.; Pistis, D.; Marelli, G.; Grandone, I.; Natali, A. Critical evaluation of the questionnaires assessing adherence to the Mediterranean diet that are based on servings. Nutr. Metab. Cardiovasc. Dis. 2023, 33, 724–736. [Google Scholar] [CrossRef]
- Barker, T.H.; Hasanoff, S.; Aromataris, E.; Stone, J.C.; Leonardi-Bee, J.; Sears, K.; Klugar, M.; Tufanaru, C.; Moola, S.; Liu, X.-L.; et al. The revised JBI critical appraisal tool for the assessment of risk of bias for analytical cross-sectional studies. JBI Evid. Synth. 2025, 441–453. [Google Scholar] [CrossRef] [PubMed]
- El Kinany, K.; Deoula, M.M.S.; Hatime, Z.; Boudouaya, H.A.; Atassi, M.; El Asri, A.; Benslimane, A.; Nejjari, C.; Ibrahimi, S.A.; Lagiou, P. Modified Mediterranean diet score adapted to a southern Mediterranean population and its relation to overweight and obesity risk. Public Health Nutr. 2021, 24, 4064–4070. [Google Scholar] [CrossRef] [PubMed]
- Shatwan, I.M.; Alhinai, E.A.; Alawadhi, B.; Surendran, S.; Aljefree, N.M.; Almoraie, N.M. High Adherence to the Mediterranean Diet Is Associated with a Reduced Risk of Obesity among Adults in Gulf Countries. Nutrients 2021, 13, 995. [Google Scholar] [CrossRef]
- Hashim, M.; Radwan, H.; Ismail, L.C.; Faris, M.E.; Mohamad, M.N.; Saleh, S.T.; Sweid, B.; Naser, R.; Hijaz, R.; Altaher, R. Determinants for Mediterranean diet adherence beyond the boundaries: A cross-sectional study from Sharjah, the United Arab Emirates. J. Transl. Med. 2024, 22, 513. [Google Scholar] [CrossRef]
- Biggi, C.; Biasini, B.; Ogrinc, N.; Strojnik, L.; Endrizzi, I.; Menghi, L.; Khémiri, I.; Mankai, A.; Slama, F.B.; Jamoussi, H.; et al. Drivers and Barriers Influencing Adherence to the Mediterranean Diet: A Comparative Study across Five Countries. Nutrients 2024, 16, 2405. [Google Scholar] [CrossRef]
- Zeenny, R.M.; Haddad, C.; Hajj, A.; Zeidan, R.K.; Salameh, P.; Ferrières, J. Adherence to the Mediterranean Diet and Cardiovascular Risk Factors among the Lebanese Population: A Nationwide Cross-Sectional Post Hoc Study. Nutrients 2024, 16, 2426. [Google Scholar] [CrossRef]
- Elmskini, F.Z.; Bouh, A.; Labyad, A.; Elghoulam, N.; Iraqi, H.; Mehdad, S.; Madkour, A.; Moufid, A.; Aabi, M.; Boutayeb, S. Increased nutrition knowledge and adherence to the Mediterranean diet are associated with lower body mass index and better self-rated general health among university students. Human. Nutr. Metab. 2024, 35, 200240. [Google Scholar] [CrossRef]
- Naja, F.; Itani, L.; Hamade, R.; Chamieh, M.C.; Hwalla, N. Mediterranean diet and its environmental footprints amid nutrition transition: The case of Lebanon. Sustainability 2019, 11, 6690. [Google Scholar] [CrossRef]
- Naja, F.; Hwalla, N.; Itani, L.; Baalbaki, S.; Sibai, A.; Nasreddine, L. A novel Mediterranean diet index from Lebanon: Comparison with Europe. Eur. J. Nutr. 2015, 54, 1229–1243. [Google Scholar] [CrossRef] [PubMed]
- El Rhazi, K.; Nejjari, C.; Romaguera, D.; Feart, C.; Obtel, M.; Zidouh, A.; Bekkali, R.; Gateau, P.B. Adherence to a Mediterranean diet in Morocco and its correlates: Cross-sectional analysis of a sample of the adult Moroccan population. BMC Public Health 2012, 12, 345. [Google Scholar] [CrossRef] [PubMed]
- Schröder, H.; Fitó, M.; Estruch, R.; Martínez-González, M.A.; Corella, D.; Salas-Salvadó, J.; Lamuela-Raventos, R.M.; Emilio, R.; Itziar, S.; Miquel, F.; et al. A short screener is valid for assessing Mediterranean diet adherence among older Spanish men and women. J. Nutr. 2021, 141, 1140–1145. [Google Scholar] [CrossRef]
- Trichopoulou, A.; Orfanos, P.; Norat, T.; Bueno-de-Mesquita, B.; Ocké, M.C.; Peeters, P.H.; Schouw, Y.T.v.d.; Boeing, H.; Hoffmann, K.; Boffetta, P.; et al. Modified Mediterranean diet and survival: EPIC-elderly prospective cohort study. BMJ 2005, 330, 991. [Google Scholar] [CrossRef] [PubMed]
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean Diet and Survival in a Greek Population. N. Engl. J. Med. 2003, 348, 2599–2608. [Google Scholar] [CrossRef]
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568. [Google Scholar] [CrossRef] [PubMed]
- Fung, T.T.; Rexrode, K.M.; Mantzoros, C.S.; Manson, J.E.; Willett, W.C.; Hu, F.B. Mediterranean Diet and Incidence of and Mortality From Coronary Heart Disease and Stroke in Women. Circulation 2009, 119, 1093–1100. [Google Scholar] [CrossRef] [PubMed]
- Gerber, M. Qualitative methods to evaluate Mediterranean diet in adults|Public Health Nutrition|Cambridge Core. Public Health Nutr. 2006, 9, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Agnoli, C.; Grioni, S.; Sieri, S.; Palli, D.; Masala, G.; Sacerdote, C.; Vineis, P.; Tumino, R.; Giurdanella, M.C.; Pala, V.; et al. Italian Mediterranean Index and risk of colorectal cancer in the Italian section of the EPIC cohort. Int. J. Cancer 2013, 132, 1404–1411. [Google Scholar] [CrossRef] [PubMed]
- Buckland, G.; Agudo, A.; Luján, L.; Jakszyn, P.; Bueno-de-Mesquita, H.B.; Palli, D.; Boeing, H.; Carneiro, F.; Krogh, V.; Sacerdote, C. Adherence to a Mediterranean diet and risk of gastric adenocarcinoma within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort study. Am. J. Clin. Nutr. 2010, 91, 381–390. [Google Scholar] [CrossRef]
- Mendez, M.A.; Popkin, B.M. Globalization, urbanization and nutritional change in the developing world. Ejade Electron. J. Agric. Dev. Econ. 2004, 1, 220–241. [Google Scholar]
- Mattavelli, E.; Olmastroni, E.; Bonofiglio, D.; Catapano, A.L.; Baragetti, A.; Magni, P. Adherence to the Mediterranean Diet: Impact of Geographical Location of the Observations. Nutrients 2022, 14, 2040. [Google Scholar] [CrossRef]
- Trajkovska Petkoska, A.; Ognenoska, V.; Trajkovska-Broach, A. Mediterranean Diet: From Ancient Traditions to Modern Science—A Sustainable Way Towards Better Health, Wellness, Longevity, and Personalized Nutrition. Sustainability 2025, 17, 4187. [Google Scholar] [CrossRef]
- Lăcătușu, C.M.; Grigorescu, E.D.; Floria, M.; Onofriescu, A.; Mihai, B.M. The Mediterranean Diet: From an Environment-Driven Food Culture to an Emerging Medical Prescription. Int. J. Environ. Res Public Health 2019, 16, 942. [Google Scholar] [CrossRef]
- Capurso, A. The Mediterranean diet: A historical perspective. Aging Clin. Exp. Res. 2024, 36, 78. [Google Scholar] [CrossRef]
- Damigou, E.; Faka, A.; Kouvari, M.; Anastasiou, C.; Kosti, R.I.; Chalkias, C.; Panagiotakos, D. Adherence to a Mediterranean type of diet in the world: A geographical analysis based on a systematic review of 57 studies with 1,125,560 participants. Int. J. Food Sci. Nutr. 2023, 74, 799–813. [Google Scholar] [CrossRef]
- Fuller, B.T.; Riehl, S.; Linseele, V.; Marinova, E.; de Cupere, B.; Bretschneider, J.; Richards, M.P.; van Neer, W. Agropastoral and dietary practices of the northern Levant facing Late Holocene climate and environmental change: Isotopic analysis of plants, animals and humans from Bronze to Iron Age Tell Tweini. PLoS ONE 2024, 19, e0301775. [Google Scholar] [CrossRef]
- Uylaşer, V.; Yildiz, G. The historical development and nutritional importance of olive and olive oil constituted an important part of the Mediterranean diet. Crit. Rev. Food Sci.Nutr. 2014, 54, 1092–1101. [Google Scholar] [CrossRef]
- Rashid, K.; Hashimi, M.; Saleem, S. Zaitoon/Olive (Olea Europaea) as Mentioned in The Holy Qur’an and Ahadith and Its Ethno medicinal Importance. Available online: https://www.researchgate.net/publication/369416202_Zaitoon_Olive_as_mentioned_in_Holy_Qur (accessed on 20 August 2025).
- Dernini, S.; Berry, E.M. Mediterranean Diet: From a Healthy Diet to a Sustainable Dietary Pattern. Front. Nutr. 2015, 2, 15. [Google Scholar] [CrossRef]
- Kitagawa, T.; Kashiwagi, K.; Isoda, H. Effect of Religious and Cultural Information of Olive Oil on Consumer Behavior: Evidence from Japan. Sustainability 2020, 12, 810. [Google Scholar] [CrossRef]
- Patino-Alonso, M.C.; Recio-Rodríguez, J.I.; Magdalena Belio, J.F.; Colominas-Garrido, R.; Lema-Bartolomé, J.; Arranz, A.G.; Agudo-Conde, C.; Gomez-Marcos, M.A.; García-Ortiz, L.; the EVIDENT Group. Factors Associated with Adherence to the Mediterranean Diet in the Adult Population. J. Acad. Nutr. Diet. 2014, 114, 583–589. [Google Scholar] [CrossRef] [PubMed]
- Vaudin, A.; Wambogo, E.; Moshfegh, A.; Sahyoun, N.R. Awareness and use of nutrition information predict measured and self-rated diet quality of older adults in the USA. Public Health Nutr. 2021, 24, 1687–1697. [Google Scholar] [CrossRef] [PubMed]
- Papadaki, A.; Wood, L.; Sebire, S.J.; Jago, R. Adherence to the Mediterranean diet among employees in South West England: Formative research to inform a web-based, work-place nutrition intervention. Prev. Med. Rep. 2015, 2, 223–228. [Google Scholar] [CrossRef]
- Franks, M.M.; Shields, C.G.; Lim, E.; Sands, L.P.; Mobley, S.; Boushey, C.J. I Will If You Will. Health Educ. Behav. 2012, 39, 324–331. [Google Scholar] [CrossRef]
- Musaiger, A.O.; Hassan, A.S.; Obeid, O. The paradox of nutrition-related diseases in the Arab countries: The need for action. Int. J. Envrion. Res. Public Health 2011, 8, 3637–3671. [Google Scholar] [CrossRef] [PubMed]
- Tariq, M.N.M.; Stojanovska, L.; Dhaheri, A.S.A.; Cheikh Ismail, L.; Apostolopoulos, V.; Ali, H.I. Lifestyle Interventions for Prevention and Management of Diet-Linked Non-Communicable Diseases among Adults in Arab Countries. Healthcare 2023, 11, 45. [Google Scholar] [CrossRef] [PubMed]
- Aboul-Enein, B.H.; Bernstein, J.; Neary, A. Dietary transition and obesity in selected Arabic-speaking countries: A review of the current evidence. East. Mediterr. Health J. 2017, 22, 763–770. [Google Scholar] [CrossRef]
- Muscogiuri, G.; Verde, L.; Sulu, C.; Katsiki, N.; Hassapidou, M.; Frias-Toral, E.; Cucalón, G.; Pazderska, A.; Yumuk, V.D.; Colao, A. Mediterranean diet and obesity-related disorders: What is the evidence? Curr. Obes. Rep. 2022, 11, 287–304. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Date Range | 2010 to November 2024 | N/A |
| Population | At least around 1000 participants in the sample size. Arabic-speaking populations that reside in an Arab League member state. | Much less than 1000 participants as the sample size. Non-Arab or Arabic-speaking populations. Arab diaspora residing outside an Arab League member state. Individuals with chronic illnesses or co-morbidities (e.g., IBD, CVD, diabetes, kidney disease, cancer, HIV), or with impaired food autonomy (e.g., dementia, Alzheimer’s, schizophrenia). Specific subpopulations (e.g., pregnant women, centenarians or elderly people, athletes). Studies conducted amid the COVID-19 pandemic. |
| Measures of interest | Mediterranean diet adherence | N/A |
| Language | English | All other languages. |
| Study type | Peer-reviewed original research articles | Non-peer-reviewed articles. Study protocols. Narratives. Similar article types. Gray literature. Communications. White papers. Conference proceedings. |
| Authors, Year | Target Population (Country) | Study Design | Sample Size * | MD Assessment Tool or Scoring System | Results |
|---|---|---|---|---|---|
| Naja et al., 2019 [48] | Adults over 20 years old (Lebanon) | Cross-sectional | 2610 | LMD, rMED score, Med-DQI, aMed | Low adherence to the MD was observed, with the majority of participants falling between low and moderate adherence, and a minority having high adherence. A higher adherence to the MD was associated with lower water use. All four MD scores were associated with lower greenhouse emissions. |
| El Kinany et al., 2021 [42] | Adults over 18 years old (Morocco) | Cross-sectional | 1492 | MMD | Close adherence to the MD was associated with reduced overweight/obesity risk among Moroccan adults. Those with high adherence to the MD had a 39% reduced risk of excess weight compared with participants in the lowest compliance category. |
| Shatwan et al., 2021 [43] | Adults 20–55 years old (Gulf countries: Saudi Arabia, Oman, Kuwait) | Cross-sectional | 961 | MEDAS | The highest adherence to the MD was associated with a decrease in two obesity indicators, body mass index and hip circumference. Low adherence to the MD was reported among participants from three Gulf countries. |
| Naja et al., 2015 [49] | Adults between 20 and 55 years old (Lebanon) | Cross-sectional | 2048 | MedDietScore, IMI, rMED score, Med-DQI, MDS, Derivation of the LMD | Men, smokers, younger and less physically active participants, and those with lower education levels were less likely to adhere to an MD dietary pattern. |
| El Rhazi et al., 2012 [50] | Adults over 18 years old (Morocco) | Cross-sectional | 2214 | A simplified score of MDS | Adherence to the MD is declining across the Moroccan population, regardless of age or education level. This is especially pronounced in rural communities, among individuals who live alone, and among those residing in affluent households. |
| Elmskini et al., 2024 [47] | Adults over 18 years old (Morocco) | Cross-sectional | 1776 | MedDietScore | Compared to students of medical and paramedical sciences, those in both human and social sciences, natural sciences, and engineering showed higher MD adherence scores. Participants who attended nutrition-related training had higher MD adherence scores than those who did not. Similarly, non-overweight students had significantly higher MD adherence scores compared to their overweight/obese peers. |
| Hashim et al., 2024 [44] | Adults over 25 years old (UAE) | Cross-sectional | 1314 | MEDAS | The study participants had a moderate adherence score. The MD adherence score was associated with physical activity. Nutrition information from dietitians and social media were the two most strongly related predictors for higher adherence. Being a smoker and from a non-Mediterranean country was associated with lower adherence scores. |
| Zeenny et al., 2024 [46] | Adults over 18 years old (Lebanon) | Cross-sectional. | 2048 | LMDS | Higher adherence to the MD was associated with older age, being female, married, participating in regular physical activity, and having cardiovascular disease and diabetes. Adherence was negatively related to current and previous smokers and those with higher distress levels. |
| Biggi et al. 2024 [45] | Adults between the ages of 18–79 (Tunisia and Morocco) | Cross-sectional. | 1617 (Morrocco: 803, Tunisia: 814) | MEDAS | Medium to low adherence was reported among Tunisian and Moroccan participants, with higher adherence observed in Morocco. Positive attitudes toward the healthiness of food were the strongest predictor of adherence, whereas picky eating was a significant negative predictor in both countries. Health motivations positively influenced adherence to the MD among Moroccans. Price and convenience were substantial barriers among Tunisians, whereas a preference for local and seasonal foods promoted adherence among Moroccans. |
| Tool (Theoretical Range) | Used by | Utilized Score Cut-Offs | ||
|---|---|---|---|---|
| Low | Moderate | High | ||
| MEDAS (0–13) | [43,44] | 0–5 | 6–7 | 8–13 |
| [45] | 0–5 | 6–9 | More than 10 | |
| aMed (0–9) | [48] | 0–2.9 | 3–5.9 | 6–9 |
| rMed score (0–18) | [48,49] | 0–6.9 | 7–11.9 | 12–18 |
| Med-DQI (0–14) | [48,49] | 0–4.6 | 4.7–9.3 | 9.4–14 |
| LMD (9–27) | [48,49] | 9–14.9 | 15–20.9 | 21–27 |
| MMD (0–12) | [42] | 0–6 | - | 7–12 |
| IMI (0–11) | [49] | 0–3.6 | 3.7–7.3 | 7.4–11 |
| MedDietScore (0–55) | [49] | 0–18.3 | 18.4–36.6 | 36.7–55 |
| [47] | Not used | Not used | Not used | |
| MDS (0–9) | [49] | 0–2.9 | 3–5.9 | 6–9 |
| Simplified MDS (0–8) | [50] | 0–4 | - | 5–8 |
| LMDS (0–64) | [46] | Not used | Not used | Not used |
| Authors, Year | Country (Sample Size) | MD Adherence Tool (Tool’s Origin) | Mean Score ± SD | Classification of Mean (Standardized Tertiles) | Classification of Mean (Original Study Cut-Offs) | Distribution of Adherence Categories Reported by the Study * | ||
|---|---|---|---|---|---|---|---|---|
| Low | Moderate | High | ||||||
| Naja et al., 2019 [48] | Lebanon (2610) | LMD (Lebanon) rMED score (Spain) Med-DQI (France) aMed (US) | NR | NA | NA | LMD: 29.8%, rMED: 21.7% Med-DQI: 27.8% aMED: 32% | LMD: 57.5% rMED: 71.5% Med-DQI: 65% aMED: 59.2% | LMD: 12.7% rMED: 6.8% Med-DQI: 7.2% aMED: 8.8% |
| El Kinany et al., 2021 [42] | Morrocco (1492) | MMD (Morrocco) | NR | NA | NA | 21.0% | 56.0% | 23.0% |
| Shatwan et al., 2021 [43] | Gulf countries (961) | MEDAS (Spain) | 5.9 ± 2.03 | Low (0–5) | Low (0–5) | 44.4% | 33.1% | 22.4% |
| Naja et al., 2015 [49] | Lebanon (2048) | MedDietScore (Greece) IMI (Italy) rMED score (Spain) Med-DQI (France) MDS (Europe) LMD (Lebanon) | MedDietScore: 27.23 ± 4.65 IMI: 3.56 ± 1.76 rMED: 8.27 ± 2.49 Med-DQI: 6.20 ± 1.81 MDS: 4.18 ± 1.49 LMD: 17.38 ± 3.40 | MedDietScore: Moderate (18.4–36.6) IMI: Low (0–3.6) rMED: Moderate (6.1–12) Med-DQI: Moderate (4.7–9.3) MDS: Moderate (3–5.9) LMD: Moderate (15–20.9) | MedDietScore: Moderate (18.4–36.6) IMI: Low (0–3.6) rMED: Moderate (6.1–12) Med-DQI: Moderate (4.7–9.3) MDS: Moderate (3–5.9) LMD: Moderate (15–20.9) | NR | NR | NR |
| El Rhazi et al., 2012 [50] | Morocco (2214) | A simplified score of MDS (Greece) | 5.1 ± 1.2 | Moderate (2.68–5.33) | High (5–8) | 29.9% | NA | 70.1% |
| Elmskini et al., 2024 [47] | Morocco (1776) | MedDietScore (Greece) | 23.27 ± 5.47 | Moderate (18.4–36.6) | No categorization implemented | NR | NR | NR |
| Hashim et al., 2024 [44] | UAE (1314) | MEDAS (Spain) | 5.96 ± 1.92 | Moderate (4.34–8.66) | Low (0–5) | 36.0% | 41.0% | 23.0% |
| Zeenny et al., 2024 [46] | Lebanon (2048 [Females: 1054; Males: 994]) | LMDS (Lebanon) | Females: 30.90 ± 4.59 Males: 30.17 ± 4.84 | Moderate for both (42.7–64) | No categorization implemented | NR | NR | NR |
| Biggi et al., 2024 [45] | Morocco (803) Tunisia (814) | MEDAS (Spain) | Morrocco: 7.62 ± 1.84; Tunisia: 7.21 ± 1.91 | Moderate for both (4.34–8.66) | Moderate for both (6–9) | Morocco: 11.8%, Tunisia: 19.4% | Morocco: 73.6%, Tunisia: 69.3% | Morocco: 14.6%, Tunisia: 11.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Faris, M.E.; Benajiba, N.; Aboul-Enein, B.H.; Abu Shihab, K.; Alshaalan, R.; Aldahash, R.; Almoayad, F. Adherence to the Mediterranean Diet Across the League of Arab States: A Systematic Review. Healthcare 2025, 13, 2217. https://doi.org/10.3390/healthcare13172217
Faris ME, Benajiba N, Aboul-Enein BH, Abu Shihab K, Alshaalan R, Aldahash R, Almoayad F. Adherence to the Mediterranean Diet Across the League of Arab States: A Systematic Review. Healthcare. 2025; 13(17):2217. https://doi.org/10.3390/healthcare13172217
Chicago/Turabian StyleFaris, MoezAlIslam E., Nada Benajiba, Basil H. Aboul-Enein, Katia Abu Shihab, Rasha Alshaalan, Rehab Aldahash, and Fatmah Almoayad. 2025. "Adherence to the Mediterranean Diet Across the League of Arab States: A Systematic Review" Healthcare 13, no. 17: 2217. https://doi.org/10.3390/healthcare13172217
APA StyleFaris, M. E., Benajiba, N., Aboul-Enein, B. H., Abu Shihab, K., Alshaalan, R., Aldahash, R., & Almoayad, F. (2025). Adherence to the Mediterranean Diet Across the League of Arab States: A Systematic Review. Healthcare, 13(17), 2217. https://doi.org/10.3390/healthcare13172217






