Anesthesiologic Management of Adult and Pediatric Patients with Obstructive Sleep Apnea
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Selection Criteria
3. Pathophysiology and Phenotypes of OSA Related to Anesthesia
4. The Challenge of Preoperative Evaluation
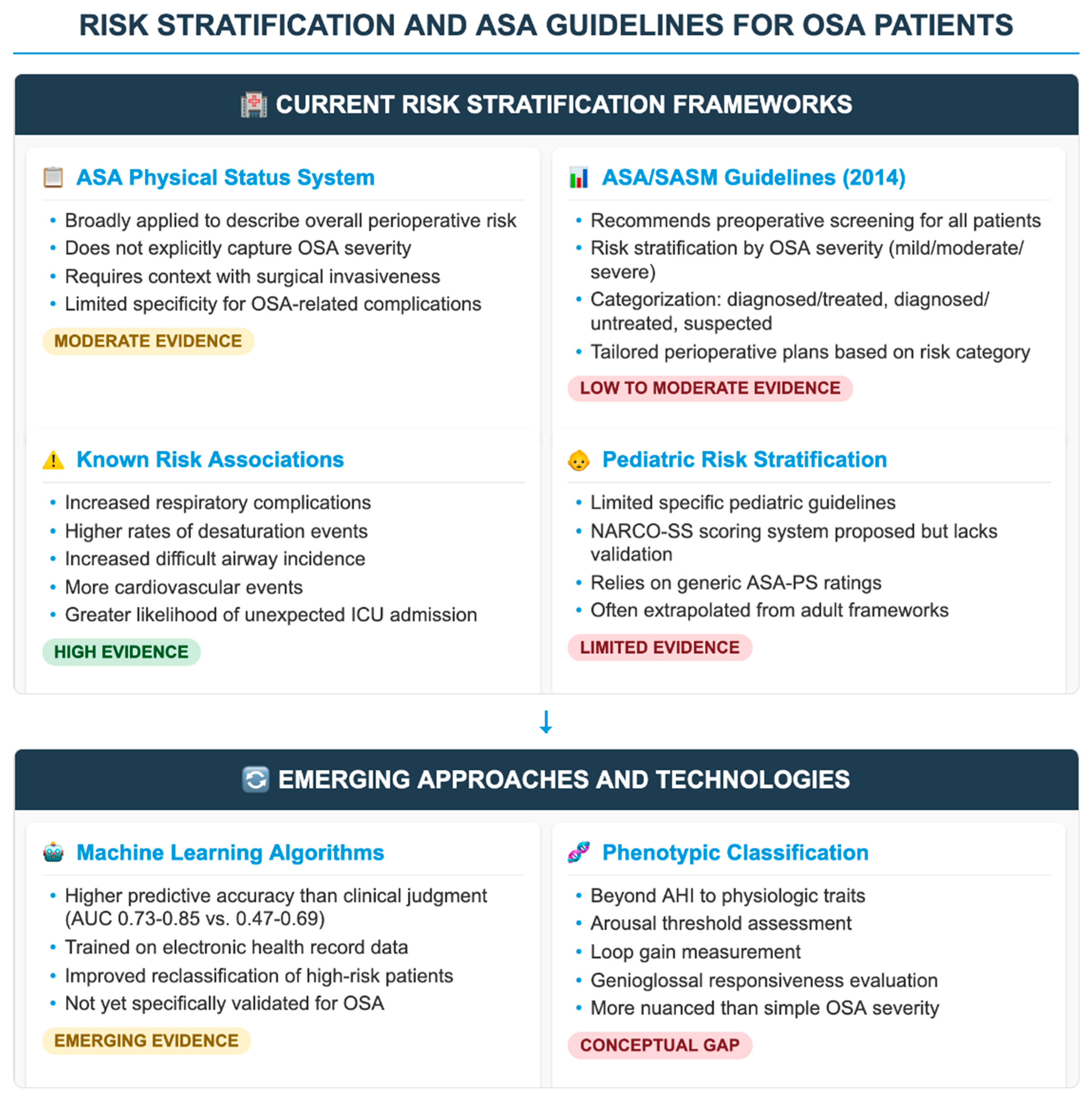
5. Risk Stratification and ASA Guidelines
6. Anesthetic Induction and Airway Management
7. Opioids, Sedation, and Respiratory Depression
7.1. Adult Physiology and Opioid Sensitivity
7.2. Opioid-Sparing Strategies in Adults
7.3. Mechanistic Underpinnings and Phenotype-Specific Risk
8. Intraoperative Ventilation and Monitoring
8.1. Lung-Protective Ventilation (LPV)
8.2. Recruitment Maneuvers (RMs)
8.3. Intraoperative Monitoring
9. Postoperative Complications
10. Role of CPAP and Other Airway Adjuncts in the Perioperative Period
11. Conclusions
11.1. Future Directions
11.2. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFI | Awake Fiberoptic Intubation |
| AHI | Apnea–Hypopnea Index |
| ASA | American Society of Anesthesiologists |
| AUC | Area Under the Curve |
| BiPAP | Bilevel Positive Airway Pressure |
| BMI | Body Mass Index |
| CHASE-OSA | (Pediatric OSA screening model—acronym not explicitly defined) |
| CI | Confidence Interval |
| CPAP | Continuous Positive Airway Pressure |
| DISE | Drug-Induced Sleep Endoscopy |
| EPAP | Expiratory Positive Airway Pressure |
| EtCO2 | End-tidal Carbon Dioxide |
| HCO3− | Bicarbonate |
| HFNC | High-Flow Nasal Cannula |
| HFNO | High-Flow Nasal Oxygen |
| HR | Hazard Ratio |
| HTN | Hypertension |
| ICU | Intensive Care Unit |
| IV | Intravenous |
| LPV | Lung-Protective Ventilation |
| MAD | Mandibular Advancement Device |
| NARCO-SS | Neurological Airway Respiratory Complication–Sleep Score |
| NMB | Neuromuscular Blocker |
| NoSAS | (OSA screening score—acronym not explicitly defined) |
| NSAIDs | Non-Steroidal Anti-Inflammatory Drugs |
| OBA-A | Opioid-Based Anesthesia-Analgesia |
| ODI | Oxygen Desaturation Index |
| OFA | Opioid-Free Anesthesia |
| OHS | Obesity Hypoventilation Syndrome |
| OIRD | Opioid-Induced Respiratory Depression |
| OSA | Obstructive Sleep Apnea |
| OSA-A | Opioid-Sparing Anesthesia–Analgesia |
| PACU | Post-Anesthesia Care Unit |
| PAP | Positive Airway Pressure |
| PEEP | Positive End-Expiratory Pressure |
| PPCs | Postoperative Pulmonary Complications |
| PPG | Photoplethysmography |
| PS | Physical Status |
| PSG | Polysomnography |
| P-SAP | (Pediatric sleep apnea screening score—acronym not explicitly defined) |
| RCT | Randomized Controlled Trial |
| RM | Recruitment Maneuver |
| ROC | Receiver Operating Characteristic |
| SASM | Society of Anesthesia and Sleep Medicine |
| SDB | Sleep-Disordered Breathing |
| SpO2 | Oxygen Saturation |
| STOP-Bang | Snoring, Tiredness, Observed apnea, Pressure (HTN), BMI, Age, Neck circumference, Gender |
| VL | Videolaryngoscopy |
References
- Kaw, R.; Chung, F.; Pasupuleti, V.; Mehta, J.; Gay, P.C.; Hernandez, A.V. Meta-analysis of the association between obstructive sleep apnoea and postoperative outcome. Br. J. Anaesth. 2012, 109, 897–906. [Google Scholar] [CrossRef]
- Maniaci, A.; Lavalle, S.; Parisi, F.M.; Barbanti, M.; Cocuzza, S.; Iannella, G.; Magliulo, G.; Pace, A.; Lentini, M.; Masiello, E.; et al. Impact of obstructive sleep apnea and sympathetic nervous system on cardiac health: A comprehensive review. J. Cardiovasc. Dev. Dis. 2024, 11, 204. [Google Scholar] [CrossRef]
- Chung, F.; Subramanyam, R.; Liao, P.; Sasaki, E.; Shapiro, C.; Sun, Y. High STOP-Bang score indicates a high probability of obstructive sleep apnoea. Br. J. Anaesth. 2012, 108, 768–775. [Google Scholar] [CrossRef]
- Finkel, K.J.; Searleman, A.C.; Tymkew, H.; Tanaka, C.Y.; Saager, L.; Safer-Zadeh, E.; Bottros, M.; Selvidge, J.A.; Jacobsohn, E.; Pulley, D.; et al. Prevalence of undiagnosed obstructive sleep apnea among adult surgical patients in an academic medical center. Sleep Med. 2009, 10, 753–758. [Google Scholar] [CrossRef]
- Mutter, T.C.; Chateau, D.; Moffatt, M.; Ramsey, C.; Roos, L.L.; Kryger, M. A matched cohort study of postoperative outcomes in obstructive sleep apnea: Could preoperative diagnosis and treatment prevent complications? Anesthesiology 2014, 121, 707–718. [Google Scholar] [CrossRef]
- Chung, F.; Memtsoudis, S.G.; Ramachandran, S.K.; Nagappa, M.; Opperer, M.; Cozowicz, C.; Patrawala, S.; Lam, D.; Kumar, A.; Joshi, G.P.; et al. Society of Anesthesia and Sleep Medicine Guidelines on Preoperative Screening and Assessment of Adult Patients with Obstructive Sleep Apnea. Anesth. Analg. 2016, 123, 452–473. [Google Scholar] [CrossRef]
- American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Obstructive Sleep Apnea. Practice guidelines for the perioperative management of patients with obstructive sleep apnea. Anesthesiology 2014, 120, 268–286. [Google Scholar] [CrossRef]
- Roland, P.S.; Rosenfeld, R.M.; Brooks, L.J.; Friedman, N.R.; Jones, J.; Kim, T.W.; Kuhar, S.; Mitchell, R.B.; Seidman, M.D.; Sheldon, S.H.; et al. Clinical practice guideline: Polysomnography for sleep-disordered breathing prior to tonsillectomy in children. Otolaryngol. Head Neck Surg. 2011, 145 (Suppl. 1), S1–S15. [Google Scholar] [CrossRef]
- Adler, A.C.; Chandrakantan, A.; Nathanson, B.H.; von Ungern-Sternberg, B.S. An assessment of opioids on respiratory depression in children with and without obstructive sleep apnea. Paediatr. Anaesth. 2021, 31, 977–984. [Google Scholar] [CrossRef] [PubMed]
- Rosen, D. Anesthetic management of children with sleep-disordered breathing. Paediatr. Anesth. 2011, 21, 787–795. [Google Scholar] [CrossRef]
- Bhattacharjee, R.; Kheirandish-Gozal, L.; Spruyt, K.; Gozal, D. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: A multicenter retrospective study. Am. J. Respir. Crit. Care Med. 2010, 182, 676–683. [Google Scholar] [CrossRef]
- Eckert, D.J. Phenotypic approaches to obstructive sleep apnea–new pathways for targeted therapy. Sleep Med. Rev. 2018, 37, 45–59. [Google Scholar] [CrossRef]
- Jordan, A.S.; White, D.P. Pharyngeal motor control and the pathogenesis of obstructive sleep apnea. Respir. Physiol. Neurobiol. 2008, 160, 1–7. [Google Scholar] [CrossRef]
- Wellman, A.; Malhotra, A.; Jordan, A.S.; Stevenson, K.E.; Gautam, S.; White, D.P. Effect of oxygen in obstructive sleep apnea: Role of loop gain. Respir. Physiol. Neurobiol. 2008, 162, 144–151. [Google Scholar] [CrossRef]
- Malhotra, A.; Huang, Y.; Fogel, R.B.; Pillar, G.; Edwards, J.K.; Kikinis, R.; Loring, S.H.; White, D.P. The male predisposition to pharyngeal collapse: Importance of airway length. Am. J. Respir. Crit. Care Med. 2002, 166, 1388–1395. [Google Scholar] [CrossRef]
- Mezzanotte, W.S.; Tangel, D.J.; White, D.P. Waking genioglossal electromyogram in sleep apnea patients vs. normal controls (a neuromuscular compensatory mechanism). J. Clin. Investig. 1992, 89, 1571–1579. [Google Scholar] [CrossRef] [PubMed]
- Lavalle, S.; Masiello, E.; Iannella, G.; Magliulo, G.; Pace, A.; Lechien, J.R.; Calvo-Henriquez, C.; Cocuzza, S.; Parisi, F.M.; Favier, V.; et al. Unraveling the complexities of oxidative stress and inflammation biomarkers in obstructive sleep apnea syndrome: A comprehensive review. Life 2024, 14, 425. [Google Scholar] [CrossRef]
- Nicastro, V.; Zagaria, A.; Abita, P.; Alberti, G.; Loteta, S.; Azieli, C.; Catalano, N.; Meduri, A.; Romano, G. Association between obstructive sleep apnea and hearing loss: A literary review. Acta Medica Mediterr. 2019, 35, 3363–3368. [Google Scholar] [CrossRef]
- Maniaci, A.; La Via, L.; Lechien, J.R.; Sangiorgio, G.; Iannella, G.; Magliulo, G.; Pace, A.; Mat, Q.; Lavalle, S.; Lentini, M. Hearing Loss and Oxidative Stress: A Comprehensive Review. Antioxidants 2024, 13, 842. [Google Scholar] [CrossRef]
- Edwards, B.A.; Eckert, D.J.; McSharry, D.G.; Sands, S.A.; White, D.P.; Wellman, A. Clinical predictors of the respiratory arousal threshold in patients with obstructive sleep apnea. Am. J. Respir. Crit. Care Med. 2014, 190, 1293–1300. [Google Scholar] [CrossRef]
- Nagappa, M.; Patra, J.; Wong, J.; Subramani, Y.; Singh, M.; Ho, G.; Wong, D.T.; Chung, F. Association of STOP-Bang questionnaire as a screening tool for obstructive sleep apnea and postoperative complications: A systematic review and Bayesian meta-analysis of prospective and retrospective cohort studies. Anesth. Analg. 2017, 125, 1301–1308. [Google Scholar] [CrossRef]
- Kaw, R.; Golish, J.; Ghamande, S.; Burgess, R.; Foldvary, N. Incremental risk of obstructive sleep apnea on cardiac surgical outcomes. J. Cardiovasc. Surg. 2006, 47, 683–689. [Google Scholar] [CrossRef]
- Fritz, B.A.; King, C.R.; Abdelhack, M.; Chen, Y.; Kronzer, A.; Abraham, J.; Tripathi, S.; Ben Abdallah, A.; Kannampallil, T.; Budelier, T.P.; et al. Effect of machine learning models on clinician prediction of postoperative complications: The Perioperative ORACLE randomised clinical trial. Br. J. Anaesth. 2024, 133, 1042–1050. [Google Scholar] [CrossRef]
- Sankar, A.; Johnson, S.R.; Beattie, W.S.; Tait, G.; Wijeysundera, D.N. Reliability of the American Society of Anesthesiologists Physical Status Scale in clinical practice. Br. J. Anaesth. 2014, 113, 424–432. [Google Scholar] [CrossRef]
- Chung, F.; Abdullah, H.R.; Liao, P. STOP-Bang questionnaire: A practical approach to screen for obstructive sleep apnea. Chest 2016, 149, 631–638. [Google Scholar] [CrossRef]
- Xue, B.; Li, D.; Lu, C.; King, C.R.; Wildes, T.; Avidan, M.S.; Kannampallil, T.; Abraham, J. Use of machine learning to develop and evaluate models using preoperative and intraoperative data to identify risks of postoperative complications. JAMA Netw. Open 2021, 4, e212240. [Google Scholar] [CrossRef]
- Hu, R.; Liu, J.X.; Jiang, H. Dexmedetomidine versus remifentanil sedation during awake fiberoptic nasotracheal intubation: A double-blinded randomized controlled trial. J. Anesth. 2013, 27, 211–217. [Google Scholar] [CrossRef]
- Maniaci, A.; Lavalle, S.; Gagliano, C.; Lentini, M.; Masiello, E.; Parisi, F.; Iannella, G.; Cilia, N.D.; Salerno, V.; Cusumano, G.; et al. The integration of radiomics and artificial intelligence in modern medicine. Life 2024, 14, 1248. [Google Scholar] [CrossRef]
- Biro, P.; Seifert, B.; Pasch, T. Complaints of sore throat and hoarseness after tracheal intubation: Influence of tracheal tube cuff design. Can. J. Anaesth. 2005, 52, 634–636. [Google Scholar] [CrossRef]
- Myatra, S.N.; Shah, A.; Kundra, P.; Patwa, A.; Ramkumar, V.; Divatia, J.V.; Raveendra, U.S.; Shetty, S.R.; Ahmed, S.M.; Doctor, J.R.; et al. The All India Difficult Airway Association 2016 guidelines for the management of unanticipated difficult tracheal intubation in adults. Indian J. Anaesth. 2016, 60, 885–898. [Google Scholar] [CrossRef]
- Lamperti, M.; Romero, C.S.; Guarracino, F.; Cammarota, G.; Vetrugno, L.; Tufegdzic, B.; Lozsan, F.; Frias, J.J.M.; Duma, A.; Bock, M.; et al. Preoperative assessment of adults undergoing elective noncardiac surgery: Updated guidelines from the European Society of Anaesthesiology and Intensive Care. Eur. J. Anaesthesiol. 2025, 42, 1–35. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, M.; Mason, K.P. Dexmedetomidine: Review, update, and future considerations of paediatric perioperative and periprocedural applications and limitations. Br. J. Anaesth. 2015, 115, 171–182. [Google Scholar] [CrossRef]
- Lyons, C.; Callaghan, M. Uses and mechanisms of apnoeic oxygenation: A narrative review. Anaesthesia 2019, 74, 497–507. [Google Scholar] [CrossRef] [PubMed]
- Al-Husinat, L.; Jouryyeh, B.; Rawashdeh, A.; Alenaizat, A.; Abushehab, M.; Amir, M.W.; Al Modanat, Z.; Battaglini, D.; Cinnella, G. High-flow oxygen therapy in the perioperative setting and procedural sedation: A review of current evidence. J. Clin. Med. 2023, 12, 6685. [Google Scholar] [CrossRef] [PubMed]
- Hemmes, S.N.T.; Serpa Neto, A.; Schultz, M.J. Intraoperative ventilatory strategies to prevent postoperative pulmonary complications: A meta-analysis. Curr. Opin. Anaesthesiol. 2013, 26, 126–133. [Google Scholar] [CrossRef]
- Bluth, T.; Teichmann, R.; Kiss, T.; Bobek, I.; Canet, J.; Cinnella, G.; De Baerdemaeker, L.; Gregoretti, C.; Hedenstierna, G.; Hemmes, S.N.; et al. Protective intraoperative ventilation with higher versus lower levels of positive end-expiratory pressure in obese patients (PROBESE): Study protocol for a randomized controlled trial. Trials 2017, 18, 202. [Google Scholar] [CrossRef]
- Lightdale, J.R.; Goldmann, D.A.; Feldman, H.A.; Newburg, A.R.; DiNardo, J.A.; Fox, V.L. Microstream capnography improves patient monitoring during moderate sedation. Pediatrics 2006, 117, 1515–1523. [Google Scholar] [CrossRef]
- Nagashima, H.; Mikata, R.; Isono, S.; Ogasawara, S.; Sugiyama, H.; Ohno, I.; Yasui, S.; Matsumura, T.; Koroki, K.; Kusakabe, Y.; et al. Phase II study comparing nasal pressure monitoring with capnography during invasive endoscopic procedures: A single-center, single-arm trial. Sci. Rep. 2023, 13, 1265. [Google Scholar] [CrossRef]
- Borczynski, E.; Worobel-Luk, P. Capnography monitoring of patients with obstructive sleep apnea in the post-anesthesia care unit: A best practice implementation project. JBI Database Syst. Rev. Implement Rep. 2019, 17, 1532–1547. [Google Scholar] [CrossRef]
- Ceban, F.; Yan, E.; Pivetta, B.; Saripella, A.; Englesakis, M.; Gan, T.J.; Joshi, G.P.; Chung, F. Perioperative adverse events in adult patients with obstructive sleep apnea undergoing ambulatory surgery: An updated systematic review and meta-analysis. J. Clin. Anesth. 2024, 96, 111464. [Google Scholar] [CrossRef]
- Opperer, M.; Cozowicz, C.; Bugada, D.; Mokhlesi, B.; Kaw, R.; Auckley, D.; Chung, F.; Memtsoudis, S.G. Does obstructive sleep apnea influence perioperative outcome? A qualitative systematic review for the Society of Anesthesia and Sleep Medicine Task Force on preoperative preparation of patients with sleep-disordered breathing. Anesth. Analg. 2016, 122, 1321–1334. [Google Scholar] [CrossRef]
- Cozowicz, C.; Memtsoudis, S.G. Perioperative management of the patient with obstructive sleep apnea: A narrative review. Anesth. Analg. 2021, 132, 1231–1243. [Google Scholar] [CrossRef]
- Ayad, S.; Khanna, A.K.; Iqbal, S.U.; Singla, N. Characterisation and monitoring of postoperative respiratory depression: Current approaches and future considerations. Br. J. Anaesth. 2019, 123, 378–391. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Sessler, D.I.; Dalton, J.E.; Devereaux, P.; Shahinyan, A.; Naylor, A.J.; Hutcherson, M.T.; Finnegan, P.S.; Tandon, V.; Darvish-Kazem, S.; et al. Postoperative hypoxemia is common and persistent: A prospective blinded observational study. Anesth. Analg. 2015, 121, 709–715. [Google Scholar] [CrossRef]
- Gali, B.; Whalen, F.X.; Schroeder, D.R.; Gay, P.C.; Plevak, D.J. Identification of patients at risk for postoperative respiratory complications using a validated screening tool. Anesthesiology 2009, 110, 869–877. [Google Scholar] [CrossRef] [PubMed]
- Lévy, P.; Pépin, J.L.; Wuyam, B.; Veale, D. Respiratory monitoring in sleep apnea syndrome. Sleep 1992, 15 (Suppl. 6), S5–S8. [Google Scholar] [CrossRef] [PubMed]
- Madhusudan, P.; Wong, J.; Prasad, A.; Sadeghian, E.; Chung, F.F. An update on preoperative assessment and preparation of surgical patients with obstructive sleep apnea. Curr. Opin. Anaesthesiol. 2018, 31, 89–95. [Google Scholar] [CrossRef]
- Lavalle, S.; Caruso, S.; Foti, R.; Gagliano, C.; Cocuzza, S.; La Via, L.; Parisi, F.M.; Calvo-Henriquez, C.; Maniaci, A. Behçet’s disease, pathogenesis, clinical features, and treatment approaches: A comprehensive review. Medicina 2024, 60, 562. [Google Scholar] [CrossRef]
- van Veldhuisen, S.L.; van Boxel, M.F.; Wiezer, M.J.; van Veen, R.N.; de Castro, S.M.M.; Swank, D.J.; Demirkiran, A.; Boerma, E.G.; Greve, J.W.M.; van Dielen, F.M.H.; et al. Evaluation of CPAP adherence in bariatric patients diagnosed with obstructive sleep apnea: Outcomes of a multicenter cohort study. Sleep Breath 2023, 27, 535–544. [Google Scholar] [CrossRef]
- Chan, M.T.V.; Wang, C.Y.; Seet, E.; Tam, S.; Lai, H.Y.; Chew, E.F.F.; Wu, W.K.K.; Cheng, B.C.P.; Lam, C.K.M.; Short, T.G.; et al. Association of unrecognized obstructive sleep apnea with postoperative cardiovascular events in patients undergoing major noncardiac surgery. JAMA 2019, 321, 1788–1798. [Google Scholar] [CrossRef]
- Singh, P.M.; Borle, A.; Shah, D.; Sinha, A.; Makkar, J.K.; Trikha, A.; Goudra, B.G. Optimizing prophylactic CPAP in patients without obstructive sleep apnoea for high-risk abdominal surgeries: A meta-regression analysis. Lung 2016, 194, 201–217. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, C.; Puig, J.; Serralta, F.; Carrizo, J.; Pozo, N.; Arocas, B.; Gutierrez, A.; Villar, J.; Belda, F.J.; Soro, M. High-flow nasal cannula oxygenation reduces postoperative hypoxemia in morbidly obese patients: A randomized controlled trial. Minerva Anestesiol. 2019, 85, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- Maniaci, A.; La Via, L.; Pecorino, B.; Chiofalo, B.; Scibilia, G.; Lavalle, S.; Scollo, P. Obstructive sleep apnea in pregnancy: A comprehensive review of maternal and fetal implications. Neurol. Int. 2024, 16, 522–532. [Google Scholar] [CrossRef] [PubMed]
| Tool/Score | Parameters Assessed | Sensitivity/Specificity | Clinical Feasibility | Limitations | Validated in Perioperative Context? |
|---|---|---|---|---|---|
| STOP-Bang | Snoring, tiredness, observed apnea, pressure (HTN), BMI, age, neck, and gender | Sensitivity: 84–95% (AHI ≥ 15); Specificity: ~43–56% [20] | High (self-report, quick) | Overestimates risk in obese patients; low specificity at cutoff ≥ 3 | Yes—most widely studied |
| Berlin Questionnaire | Snoring severity, fatigue, HTN, and BMI | Sensitivity: ~68–86%; Specificity: ~39–59% [21] | Moderate (longer form) | Less practical in busy settings; moderate discriminatory power | Limited use in surgical patients |
| NoSAS Score | Neck circumference, BMI, age, sex, and snoring | Sensitivity: ~79%; Specificity: ~69% [22] | Moderate to high | Less validated outside sleep clinics; age-weighted risk may misclassify | Not widely adopted perioperatively |
| P-SAP Score (pediatric) | Snoring, apneas, growth delay, and tonsillar hypertrophy | Variable: sensitivity ~70–80% in small studies | Low (limited awareness) | Pediatric-specific but not standardized; not integrated in surgical workflows | No |
| Polysomnography (PSG) | Gold standard: AHI, desaturation, and arousals | Sensitivity/Specificity: 90–99% (diagnostic) | Low (costly, time-intensive) | Not feasible pre-op for most; delays surgery; poor access in many centers | Yes, but limited by access/time |
| Overnight oximetry | ODI and desaturation index | Sensitivity: 63–88%; Specificity: 40–70% [23] | Moderate to high (home-based) | Cannot detect hypopneas or arousals; may miss mild/moderate OSA | Growing interest in triage settings |
| Chung 2-step algorithm | STOP-Bang ≥ 3 → HCO3− ≥ 28 or desaturation risk | Higher specificity than STOP-Bang alone [24] | Moderate (requires labs) | Requires labs; less suited to ambulatory or pediatric use | Partial validation |
| OSA Phenotype | Clinical Features | Adult Perioperative Strategies | Pediatric Perioperative Strategies |
|---|---|---|---|
| High loop gain (ventilatory instability) | Hypersensitive ventilatory control and prone to periodic breathing | Avoid excessive supplemental O2 (may worsen instability); titrate opioids carefully; and enhanced capnography and overnight monitoring | Close observation in first 24 h; and avoid rapid discharge after adenotonsillectomy |
| Low arousal threshold | Arouse easily but prone to frequent desaturation under sedatives | Avoid benzodiazepines; consider dexmedetomidine or regional anesthesia; and cautious opioid dosing | Minimize sedative premedication; use short-acting anesthetics; and continuous pulse oximetry post-op |
| Poor muscle responsiveness (pharyngeal dilator dysfunction) | Increased risk of airway collapse and difficult mask ventilation | Prepare advanced airway plan (videolaryngoscopy, awake fiberoptic, HFNO); and avoid deep sedation without airway control | Anticipate difficult intubation in craniofacial anomalies; and consider inhalational induction to maintain spontaneous breathing |
| Anatomical collapsibility (e.g., obesity, tonsillar hypertrophy, retrognathia) | Structural upper airway narrowing | Positioning (ramped, jaw-thrust); PEEP during ventilation; and postoperative CPAP for moderate–severe OSA | Adenotonsillectomy is definitive therapy; perioperative HFNC or CPAP for severe cases; and ICU-level monitoring if desaturation persists |
| Blunted chemoreflex sensitivity | Reduced ventilatory response to hypoxia/hypercapnia and higher opioid sensitivity | Strict opioid-sparing/multimodal analgesia; and capnographic monitoring in PACU/ward | Careful opioid use; multimodal analgesia; and continuous monitoring overnight |
| Technique/Strategy | Clinical Application | Advantages | Limitations/Risks | Evidence Level/Consensus |
|---|---|---|---|---|
| Standard IV induction (propofol-based) | Routine adult induction; moderate OSA | Familiarity; rapid onset | Decreased pharyngeal tone; risk of apnea; worsens airway collapsibility [13] | Widely used; lacks OSA-specific RCTs |
| Inhalational induction (sevoflurane) | Pediatric patients; severe OSA with anticipated airway difficulty | Preserves spontaneous ventilation | Prolonged induction; risk of laryngospasm; limited adult data | Pediatric standard in select cases |
| Awake fiberoptic intubation (AFI) | Anticipated difficult airway; severe OSA | Maintains spontaneous breathing; avoids desaturation | Requires patient cooperation; time-consuming; requires expertise [27] | Strong expert consensus; limited trial evidence |
| Videolaryngoscopy (VL) | All OSA severities; standardizing in adult care | Improved glottic visualization; reduced cervical movement | Limited effectiveness in distorted anatomy; device cost; fogging or secretions [25] | High-level observational support; growing use |
| High-flow nasal oxygen (HFNO) | Preoxygenation and apneic oxygenation | Prolongs safe apnea time; improves desaturation threshold | May delay airway intervention; not suitable for full obstruction; variable flow tolerance [22] | Strong physiologic rationale; few RCTs in OSA |
| Use of neuromuscular blockers (NMBs) | Rapid-sequence induction; airway control | Reduces airway resistance; facilitates intubation | If not anticipated properly, can worsen airway obstruction in collapsed airway | Safe with expertise; controversial in OSA [29] |
| Jaw-thrust/positioning maneuvers | All inductions, especially in obese/OSA patients | Improves airway patency; simple and non-invasive | Transient effect; needs manual assistance; not definitive solution | Universal recommendation in OSA [27] |
| Avoidance of premedication (midazolam) | High-risk adult or pediatric patients with severe OSA | Reduces risk of sedation-related apnea | May increase anxiety or uncooperativeness pre-induction | Recommended by ASA/SASM for high-risk OSA [7] |
| Sedation with dexmedetomidine | Sedation during DISE or AFI; awake fiberoptic intubation | Preserves respiratory drive; less desaturation vs. opioids | Bradycardia; hypotension; delayed recovery [29] | Promising alternative; limited comparative studies |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Via, L.; Iannella, G.; Pace, A.; Magliulo, G.; Cuttone, G.; Modica, R.; Lentini, M.; Botto, C.G.; Paternò, D.S.; Sorbello, M.; et al. Anesthesiologic Management of Adult and Pediatric Patients with Obstructive Sleep Apnea. Healthcare 2025, 13, 2183. https://doi.org/10.3390/healthcare13172183
La Via L, Iannella G, Pace A, Magliulo G, Cuttone G, Modica R, Lentini M, Botto CG, Paternò DS, Sorbello M, et al. Anesthesiologic Management of Adult and Pediatric Patients with Obstructive Sleep Apnea. Healthcare. 2025; 13(17):2183. https://doi.org/10.3390/healthcare13172183
Chicago/Turabian StyleLa Via, Luigi, Giannicola Iannella, Annalisa Pace, Giuseppe Magliulo, Giuseppe Cuttone, Rodolfo Modica, Mario Lentini, Carmelo Giancarlo Botto, Daniele Salvatore Paternò, Massimiliano Sorbello, and et al. 2025. "Anesthesiologic Management of Adult and Pediatric Patients with Obstructive Sleep Apnea" Healthcare 13, no. 17: 2183. https://doi.org/10.3390/healthcare13172183
APA StyleLa Via, L., Iannella, G., Pace, A., Magliulo, G., Cuttone, G., Modica, R., Lentini, M., Botto, C. G., Paternò, D. S., Sorbello, M., Lechien, J. R., & Maniaci, A. (2025). Anesthesiologic Management of Adult and Pediatric Patients with Obstructive Sleep Apnea. Healthcare, 13(17), 2183. https://doi.org/10.3390/healthcare13172183











