Optical Coherence Tomography Angiography (OCTA) Characteristics of Acute Retinal Arterial Occlusion: A Systematic Review
Abstract
1. Introduction
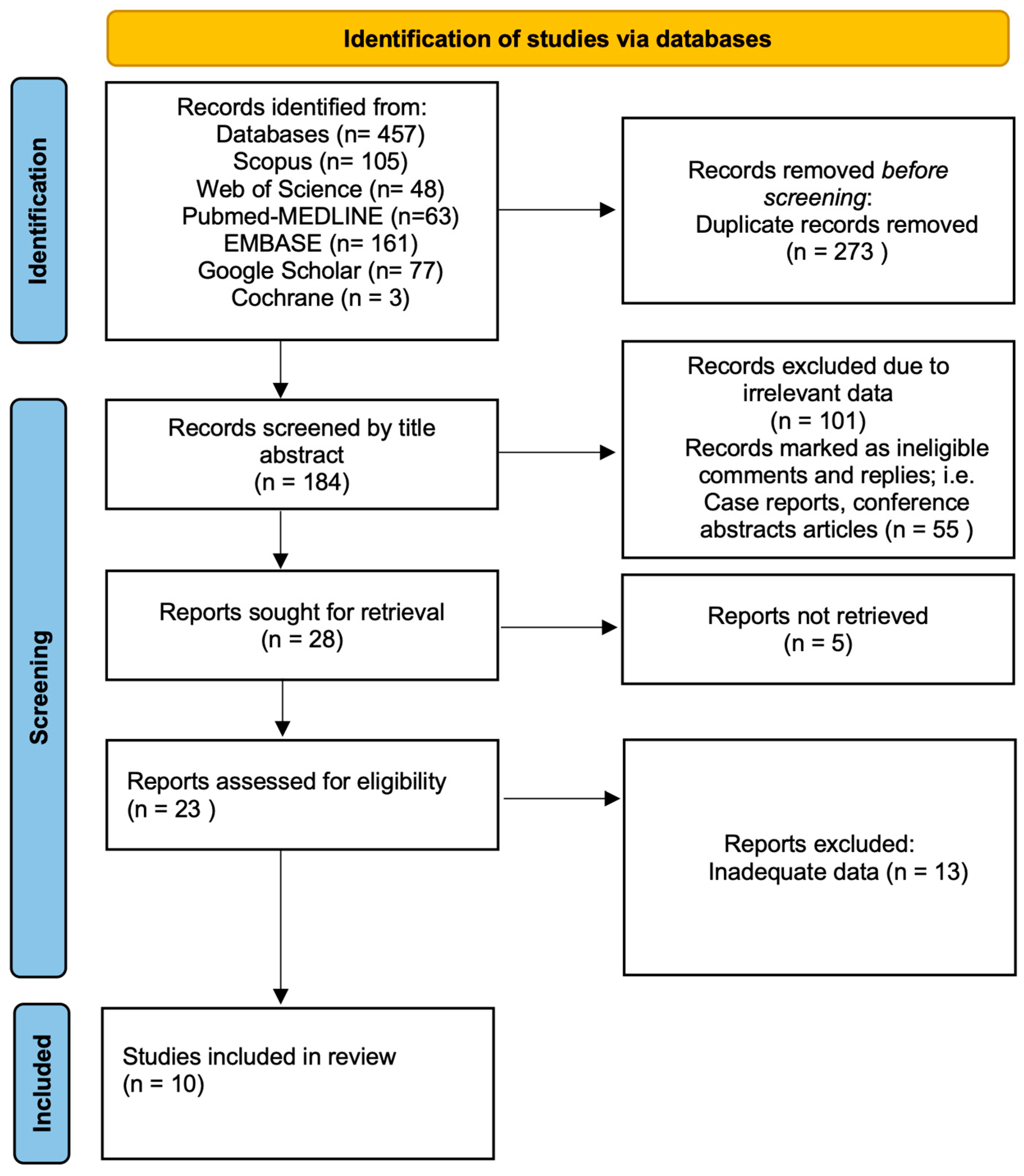
2. Materials and Methods
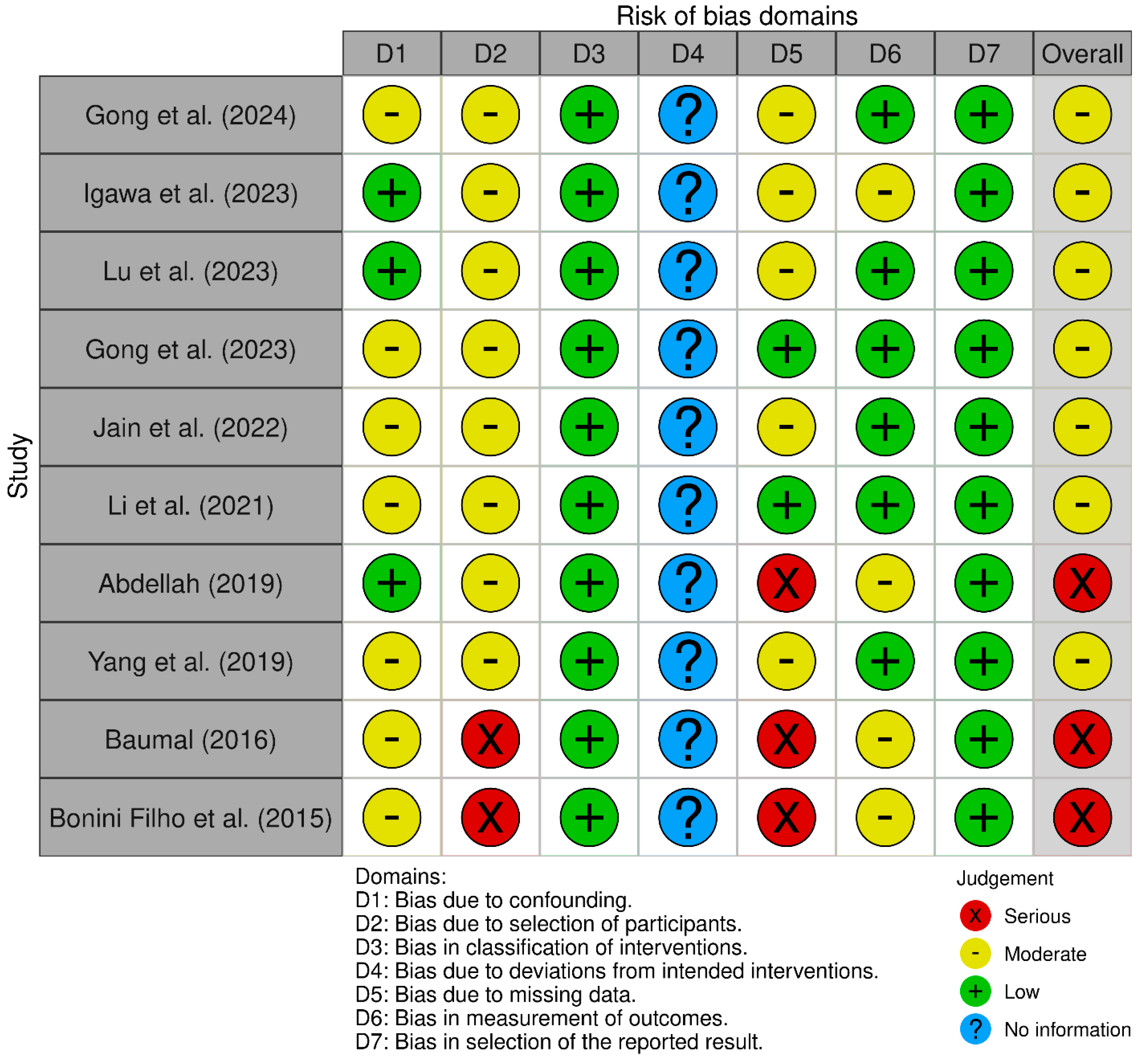
Assessment of the Methodological Quality
3. Results
3.1. Pathophysiology of Acute Retinal Arterial Occlusion
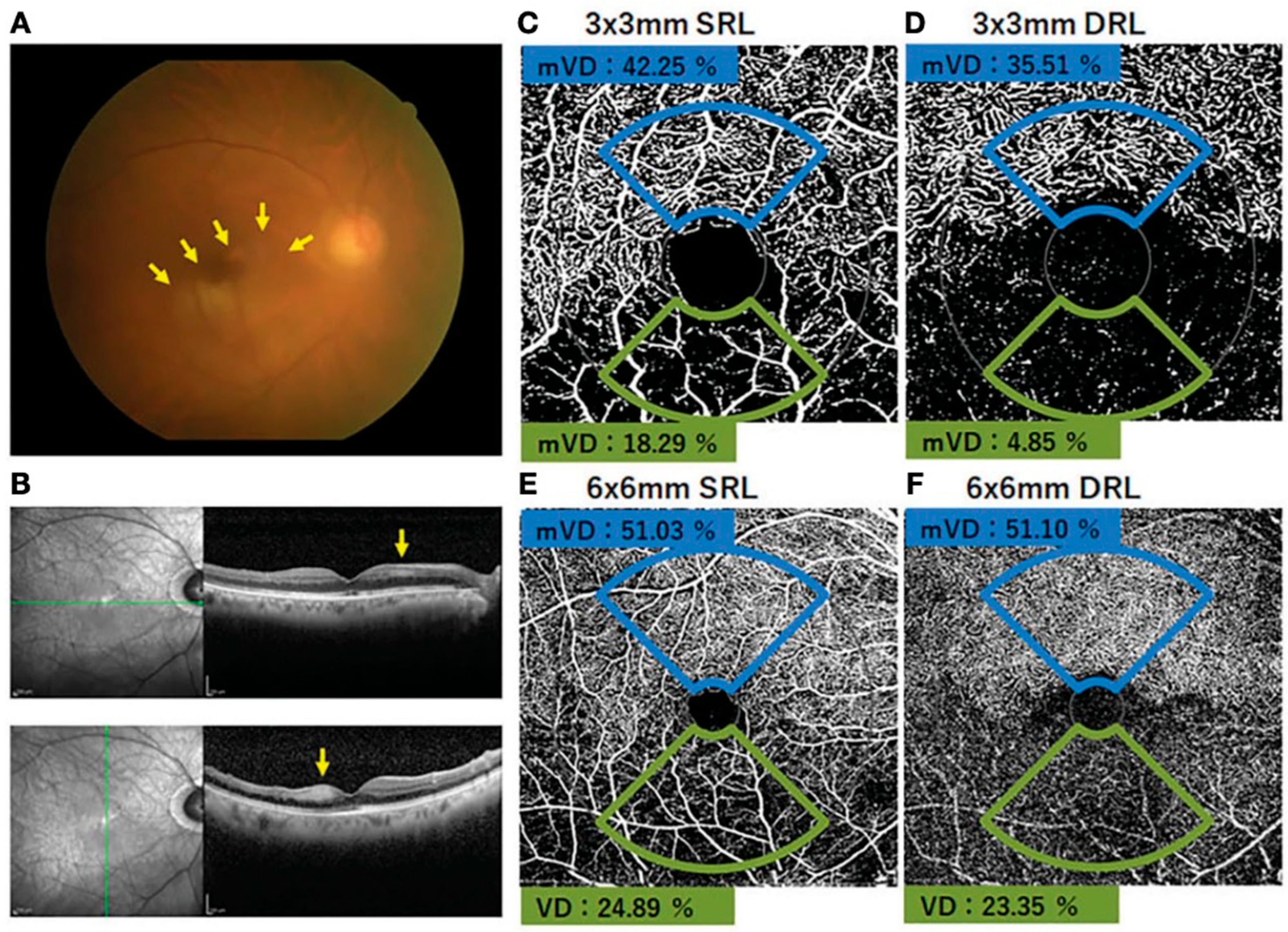
3.2. Imaging Modalities in RAO
3.2.1. Fluorescein Angiography (FA)
3.2.2. Optical Coherence Tomography
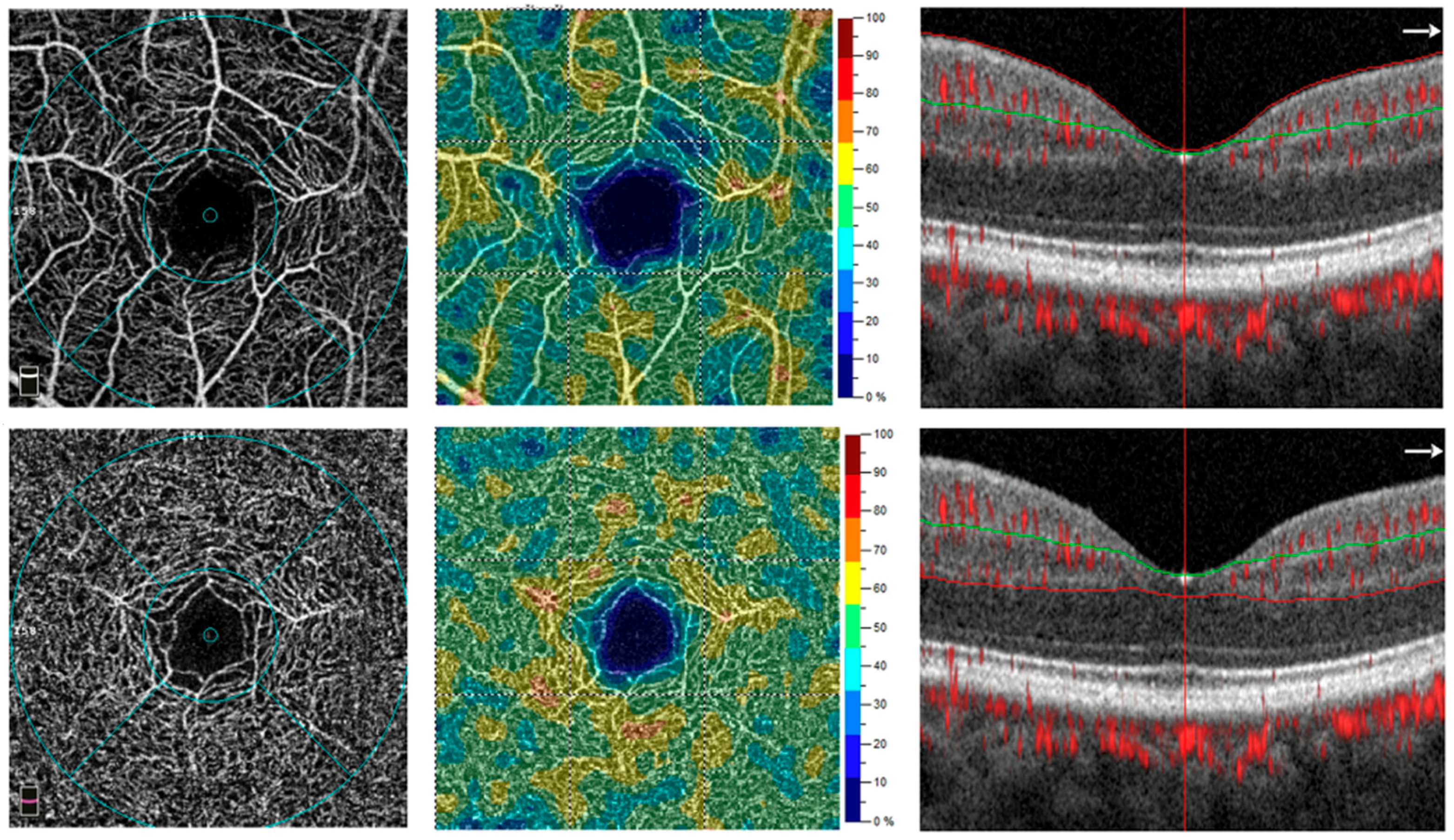
3.2.3. Optical Coherence Tomography Angiography
- SCP and DCP
- FAZ
3.3. Peripapillary Area
3.4. CHOROID
3.5. Limitations of OCTA in RAO
3.6. Clinical Applications of OCTA in Acute RAO
3.7. Monitoring and Follow-Up
3.8. The Applications of Artificial Intelligence
3.9. Future Direction
3.10. Limitations
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| SJ | Saud Aljohani |
| AS | Abdulazizi Alshehri |
References
- Dagra, A.; Lucke-Wold, B.; McGrath, K.; Mehkri, I.; Mehkri, Y.; Davidson, C.G.; Gilberstadt, N.; Douglas, B.W.; Hoh, B. Central retinal artery occlusion: A review of pathophysiological features and management. Stroke Vasc. Interv. Neurol. 2024, 4, e000977. [Google Scholar] [CrossRef]
- Shah, R.; Gilbert, A.; Melles, R.; Patel, A.; Do, T.; Wolek, M.; Vora, R.A. Central retinal artery occlusion: Time to presentation and diagnosis. Ophthalmol. Retin. 2023, 7, 527–531. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Singh, G.; Madike, R.; Cugati, S. Central retinal artery occlusion: A stroke of the eye. Eye 2024, 38, 2319–2326. [Google Scholar] [CrossRef]
- Baumal, C.R. Optical Coherence Tomography Angiography of Retinal Artery Occlusion. Dev. Ophthalmol. 2016, 56, 122–131. [Google Scholar]
- Ørskov, M.; Vorum, H.; Larsen, T.B.; Lip, G.Y.; Bek, T.; Skjøth, F. Clinical risk factors for retinal artery occlusions: A nationwide case–control study. Int. Ophthalmol. 2022, 42, 2483–2491. [Google Scholar] [CrossRef]
- Mac Grory, B.; Schrag, M.; Poli, S.; Boisvert, C.J.; Spitzer, M.S.; Schultheiss, M.; Nedelmann, M.; Yaghi, S.; Guhwe, M.; Moore, E.E.; et al. Structural and Functional Imaging of the Retina in Central Retinal Artery Occlusion—Current Approaches and Future Directions. J. Stroke Cerebrovasc. Dis. 2021, 30, 105828. [Google Scholar] [CrossRef]
- Li, X.; Hao, X.; Luo, J.; Qi, Y.; Luo, J.; Yuan, H.; Xie, L. Optical coherence tomography angiography characteristics and correlated factors with visual acuity in retinal arterial occlusion. Int. Ophthalmol. 2022, 42, 469–477. [Google Scholar] [CrossRef]
- Mac Grory, B.; Schrag, M.; Biousse, V.; Furie, K.L.; Gerhard-Herman, M.; Lavin, P.J.; Sobrin, L.; Tjoumakaris, S.I.; Weyand, C.M.; Yaghi, S.; et al. Management of Central Retinal Artery Occlusion: A Scientific Statement From the American Heart Association. Stroke 2021, 52, e282–e294. [Google Scholar] [CrossRef]
- Madike, R.; Cugati, S.; Chen, C. A review of the management of central retinal artery occlusion. Taiwan J. Ophthalmol. 2022, 12, 273–281. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.C.; Song, S.; Ng, S.M.; Scott, I.U.; Greenberg, P.B. Interventions for acute non-arteritic central retinal artery occlusion. Cochrane Database Syst. Rev. 2023, 2023, CD001989. [Google Scholar] [CrossRef] [PubMed]
- Karabulut, M.; Karalezli, A.; Karabulut, S.; Sül, S. Retinal microvascular differences in type 2 diabetes without clinically apparent retinopathy: An optical coherence tomography angiography study. Med. J. Süleyman Demirel Univ. 2022, 29, 7–13. [Google Scholar] [CrossRef]
- Lu, Y.; Cui, Y.; Zhu, Y.; Lu, E.S.; Zeng, R.; Garg, I.; Katz, R.; Le, R.; Wang, J.C.; Vavvas, D.G.; et al. Quantitative Wide-Field Swept-Source Optical Coherence Tomography Angiography and Visual Outcomes in RAO. Clin. Ophthalmol. 2023, 17, 2505–2513. [Google Scholar] [CrossRef]
- Igawa, Y.; Amaki, H.; Kanno, J.; Tachibana, M.; Konno, S.; Yoshikawa, Y.; Matsumoto, S.; Shoji, T.; Makita, J.; Shinoda, K. Evaluations of microvascular density by optical coherence tomography, angiography, and function by multifocal electroretinography of the macular area in eyes with branch retinal artery occlusion. Front. Ophthalmol. 2023, 8, 3. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.X.; Wu, B.; Xie, S.Y.; Zhang, W.; Chen, S. OCTA characteristics in non-arteritic central retinal artery occlusion and correlation with visual acuity. Int. J. Ophthalmol. 2024, 17, 289–296. [Google Scholar] [CrossRef] [PubMed]
- Jain, M.; Narayanan, R.; Barik, B.; Sahoo, N.K.; Raval, V.; Reddy, N.G. Internal limiting membrane detachment in acute Central Retinal Artery Occlusion: Clinical features, multimodal imaging, outcomes & prognostic biomarker. Int. J. Retin. Vitr. 2022, 8, 86. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Liu, X.; Li, H.; Xu, J.; Wang, F. Optical coherence tomography angiography characteristics of acute retinal arterial occlusion. BMC Ophthalmol. 2019, 19, 147. [Google Scholar] [CrossRef]
- Filho, M.A.B.; Adhi, M.; de Carlo, T.E.; Ferrara, D.; Baumal, C.R.; Witkin, A.J.; Reichel, E.; Kuehlewein, L.; Sadda, S.R.; Sarraf, D.; et al. Optical Coherence Tomography Angiography in Retinal Artery Occlusion. Retina 2015, 35, 2339–2346. [Google Scholar] [CrossRef]
- Gong, H.; Wu, B.; Xie, S. Visual acuity assessment of central retinal artery occlusion patients with or without paracentral acute middle maculopathy via OCT-A. BMC Ophthalmol. 2023, 23, 412. [Google Scholar] [CrossRef]
- Abdellah, M.M. Multimodal Imaging of Acute Central Retinal Artery Occlusion. Med. Hypothesis Discov. Innov. Ophthalmol. 2019, 8, 283–290. [Google Scholar]
- Sterne, J.A.C.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 12, i4919. [Google Scholar] [CrossRef]
- Kazantzis, D.; Holmes, C.; Wijesingha, N.; Sivaprasad, S. Changes in foveal avascular zone parameters in individuals with prediabetes compared to normoglycemic controls: A systematic review and meta-analysis. Eye 2024, 38, 1855–1860. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Li, X.; Chen, T.; Li, Y.; Wang, C.; Wang, Y.; Wan, Y.; Yang, A.; Xiao, X. Improved visual outcomes of central retinal artery occlusion with local intra-arterial fibrinolysis beyond the conventional time window. J. Thromb. Thrombolysis 2024, 57, 503–511. [Google Scholar] [CrossRef]
- Spaide, R.F.; Fujimoto, J.G.; Waheed, N.K.; Sadda, S.R.; Staurenghi, G. Optical coherence tomography angiography. Prog. Retin. Eye Res. 2018, 64, 1–55. [Google Scholar] [CrossRef]
- Sampson, D.M.; Dubis, A.M.; Chen, F.K.; Zawadzki, R.J.; Sampson, D.D. Towards standardizing retinal optical coherence tomography angiography: A review. Light: Sci. Appl. 2022, 11, 63. [Google Scholar] [CrossRef]
- Chen, X.; Ma, Z.; Wang, C.; Cui, J.; Fan, F.; Gao, X.; Zhu, J. Motion artifact correction for OCT microvascular images based on image feature matching. J. Biophotonics 2024, 17, e202400198. [Google Scholar] [CrossRef] [PubMed]
- Wawer Matos, P.A.; Reimer, R.P.; Rokohl, A.C.; Caldeira, L.; Heindl, L.M.; Große, H.N. Artificial intelligence in ophthalmology—Status quo and future perspectives. Semin. Ophthalmol. 2023, 38, 226–237. [Google Scholar] [CrossRef] [PubMed]
- Du, X.L.; Li, W.B.; Hu, B.J. Application of artificial intelligence in ophthalmology. Int. J. Ophthalmol. 2018, 11, 1555–1561. [Google Scholar] [CrossRef]
- Untracht, G.R.; Durkee, M.S.; Zhao, M.; Kwok-Cheung Lam, A.; Sikorski, B.L.; Sarunic, M.V.; Andersen, P.E.; Sampson, D.D.; Chen, F.K.; Sampson, D.M. Towards standardising retinal OCT angiography image analysis with open-source toolbox OCTAVA. Sci. Rep. 2024, 14, 5979. [Google Scholar] [CrossRef] [PubMed]
| S. No | Databases | Search String | No. of Records |
|---|---|---|---|
| 1 | Web of Science | TS = (“Optical coherence tomography angiography” OR “OCTA”) AND TS = (“Retinal arterial occlusion” OR “Central retinal artery occlusion” OR “Branch retinal artery occlusion” OR “RAO” OR “CRAO” OR “BRAO”) | 48 |
| 2 | Medline | TS = (“Optical coherence tomography angiography” OR “OCTA”) AND TS = (“Retinal arterial occlusion” OR “Central retinal artery occlusion” OR “Branch retinal artery occlusion” OR “RAO” OR “CRAO” OR “BRAO”) | 63 |
| 3 | EMBASE | (“optical coherence tomography angiography”/exp OR “optical coherence tomography angiography”:ti,ab,kw OR “octa”:ti,ab,kw) AND (“retinal artery occlusion”/exp OR “retinal arterial occlusion”:ti,ab,kw OR “central retinal artery occlusion”:ti,ab,kw OR “branch retinal artery occlusion”:ti,ab,kw OR “rao:ti,ab,kw” OR “crao:ti,ab,kw” OR “brao:ti,ab,kw”) | 161 |
| 4 | Scopus | (TITLE-ABS-KEY (“Optical coherence tomography angiography” OR “OCTA”)) AND (TITLE-ABS-KEY (“Retinal arterial occlusion” OR “Central retinal artery occlusion” OR “Branch retinal artery occlusion” OR “RAO” OR “CRAO” OR “BRAO”)) AND (LIMIT-TO (DOCTYPE, “ar”)) AND (LIMIT-TO (LANGUAGE, “English”)) | 105 |
| Study | Overall Risk of Bias | Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions/Exposures | Bias Due to Deviations from Intended Interventions/Exposures | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result |
|---|---|---|---|---|---|---|---|---|
| [4] | Serious | Moderate: Small sample, unaddressed heterogeneity | Serious: Non-random enrollment, small sample size | Low: Clear definitions for RAO | Not applicable | Serious: High exclusion rate, inconsistent measurement | Moderate: Manual segmentation, acknowledged artifacts | Low: No explicit selective reporting |
| [13] | Moderate | Low: Within-subject comparison. | Moderate: Convenience sample, very small size | Low: Clear classification of affected/unaffected | Not applicable | Moderate: Exclusions for image quality, unquantified | Moderate: Acknowledged image processing artifacts | Low: No explicit selective reporting |
| [7] | Moderate | Moderate: Lack of adjustment for systemic confounders | Moderate: Retrospective, single-center, convenience | Low: Clear definitions of groups | Not applicable | Low: Based on info, but total exclusions are unknown. | Low: Automated/standardized measurements. | Low: No explicit selective reporting |
| [15] | Moderate | Moderate: Potential unmeasured confounders | Moderate: Retrospective, single-center, reliance on OCT | Low: Robust classification of ILMD | Not applicable | Moderate: Missing data for imaging, unquantified exclusions | Low: Standardized outcomes, dual-reader for quantitative | Low: No explicit selective reporting |
| [12] | Moderate | Low: Within-subject comparison. | Moderate: Convenience sample, image quality exclusions | Low: Clear classification of RAO | Not applicable | Moderate: Significant exclusions for NPA analysis | Low: Automated/dual-reader for measurements. | Low: No explicit selective reporting |
| [18] | Moderate | Moderate: Potential unmeasured confounder | Moderate: Retrospective, single-center, convenience | Low: Clear classification of PAMM | Not applicable | Low: No explicit missing data reported. | Low: Automated/standardized measurements. | Low: No explicit selective reporting |
| [17] | Serious | Moderate: Small sample, unaddressed heterogeneity | Serious: “Offered enrollment,” high exclusion rate | Low: Clear definitions for RAO | Not applicable | Serious: High exclusion/inconsistent measurement | Moderate: Manual segmentation, acknowledged artifacts | Low: No explicit selective reporting |
| [19] | Serious | Low: Within-subject comparison. | Moderate: Convenience sample, small size | Low: Clear CRAO diagnosis | Not applicable | Serious: Significant missing OCTA data | Moderate: Qualitative assessments subjective | Low: No explicit selective reporting |
| [14] | Moderate | Moderate: Potential unadjusted systemic confounders | Moderate: Retrospective, single-center, convenience | Low: Clear NA-CRAO type classification | Not applicable | Moderate: Exclusions for image quality/FFA. | Low: Automated/standardized measurements. | Low: No explicit selective reporting |
| [16] | Moderate | Moderate: Unaddressed systemic confounders | Moderate: Retrospective, single-center, convenience | Low: Clear RAO diagnosis | Not applicable | Moderate: Exclusions for image quality, missing data | Low: Automated/standardized measurements. | Low: No explicit selective reporting |
| Study (First Author, Year) | OCTA Machine Used | Software Used for Analysis | Findings in Superficial Capillary Plexus (SCP) | Findings in Deep Capillary Plexus (DCP) |
|---|---|---|---|---|
| [13] | SS-OCTA (PLEX Elite 9000, Carl Zeiss Meditec, Inc. Jena, Germany). | Built-in segmentation software, Otsu analysis with ImageJ software of the National Institutes of Health (Bethesda, MD, USA). | Significantly lower vessel density in the affected side for a 3 mm concentric circle. No significant difference for a 6 mm concentric circle. | No significant difference in vessel density between affected and unaffected sides for a 3 mm concentric circle. |
| [4] | (RTVue XR Avanti, Optovue Inc., Fremont, CA, USA). | AngioVue SD-OCTA software within the commercially available RTVue XR Avanti device (Optovue Inc., Fremont, CA, USA). | Decreased vascular perfusion. In BRAO, a larger area of decreased vascular perfusion was observed in 75% of eyes compared to DCP. | Decreased vascular perfusion. In acute CRAO, equal areas of decreased vascular perfusion to the SCP. In BRAO, one eye showed a wider area of decreased vascular perfusion, and partial restoration of perfusion in chronic RAO. |
| [7] | RTVue XR (Optovue, Inc., Fremont, CA, USA). | RTVue-XR version 2017.1.0.155. | Significantly reduced vessel density in all areas except the fovea in RAO eyes compared to fellow and normal control eyes. No significant difference between fellow eyes and normal control eyes. | Significantly reduced vessel density in all areas except the fovea in RAO eyes compared to fellow and normal control eyes. Reduced considerably in fellow eyes compared to normal control eyes in all areas except the fovea. |
| [15] | Topcon TRITON 3D PLUS Version 10.19 (Topcon, Tokyo, Japan). | Not explicitly stated, likely integrated with the Topcon system. | Showed attenuation of both arteries and veins with significant macular flow void areas. | Showed pruning of both arteries and veins with significant macular flow void areas. |
| [19] | AngioVue XR Avanti system (Optovue Inc., Fremont, CA, USA). | Not explicitly stated, likely integrated with the AngioVue system. | Disruption observed. More compromised than DCP. Marked disruption with decreased vascular perfusion. | Disruption observed. Less compromised than SCP. Marked disruption with decreased vascular perfusion. |
| [12] | Zeiss Plex Elite 9000 WF SS-OCTA (Carl Zeiss Meditec, Inc., Jena, Germany). | Advanced Retina Imaging (ARI) Network (Zeiss Portal v5.4-1206). | Decreased vascular perfusion. Statistically significant inverse correlation between SCP vessel density and vision in all subfields for RAO eyes. No correlation in contralateral eyes. | Less involved than SCP. Inverse correlation between DCP vessel density and vision in all subfields for RAO eyes, but not statistically significant. No correlation in contralateral eyes. |
| [18] | RTVue-XR Avanti (Optovue, Inc., Fremont, CA, USA). | Vue software within the commercially available RTVue XR Avanti device (Optovue Inc., Fremont, CA, USA). | Significantly decreased density in the non-PAMM group with broken, branch-like changes. No significant difference in overall superficial vascular density between PAMM and no-PAMM groups. | Reduced considerably the density in the non-PAMM group with broken branch-like changes. No significant difference in overall deep vascular density between PAMM and no-PAMM groups. |
| [14] | RTVue-XR Avanti. | Not explicitly stated, likely integrated with the RTVue-XR Avanti system. | Vessel density significantly decreased in Type A patients compared to controls. Lowest in Type A at the central fovea and the nasal parafovea compared to B and C types. No significant difference in other regions among types. | Vessel density significantly decreased in all three types of NA-CRAO patients compared to the control group. C type decreased the most (except fovea), but no significant differences were observed among the three types. Common damage targets in all CRAO types. |
| [16] | RTVue-XR Avanti (Optovue Inc. Fremont, CA, USA). | AngioVue Analytics, RTVue-XR version 2017.1.0.155 software. | Significant decrease in vessel density in RAO eyes compared with fellow eyes and normal control eyes. Significantly lower in RAO fellow eyes than in normal control eyes. Reduced in the affected hemifield in BRAO. | Significant decrease in vessel density in RAO eyes compared with fellow eyes and normal control eyes. No significant difference between fellow eyes and normal control eyes. Reduced in the affected hemifield in BRAO. |
| [17] | Prototype Angio Vue SD-OCTA software (RTVue XR Avanti; Optovue, Inc.). | AngioVue spectral-domain OCTA software within the commercially available RTVue XR Avanti device (Optovue Inc, Fremont, CA, USA). | Decreased vascular perfusion in all affected eyes. In CRAO with cilioretinal sparing, focal restoration of deep capillary plexus perfusion, while SCP perfusion was abnormal. In BRAO eyes, 75% showed focal restoration of deep capillary plexus perfusion where SCP was abnormal. | Decreased vascular perfusion in all affected eyes. In CRAO, equal areas of decreased vascular perfusion as in SCP. In CRAO with cilioretinal sparing and BRAO eyes (75%), focal restoration of perfusion was observed in regions where SCP was abnormal, and partial restoration of perfusion was observed in chronic RAO. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljohani, S. Optical Coherence Tomography Angiography (OCTA) Characteristics of Acute Retinal Arterial Occlusion: A Systematic Review. Healthcare 2025, 13, 2056. https://doi.org/10.3390/healthcare13162056
Aljohani S. Optical Coherence Tomography Angiography (OCTA) Characteristics of Acute Retinal Arterial Occlusion: A Systematic Review. Healthcare. 2025; 13(16):2056. https://doi.org/10.3390/healthcare13162056
Chicago/Turabian StyleAljohani, Saud. 2025. "Optical Coherence Tomography Angiography (OCTA) Characteristics of Acute Retinal Arterial Occlusion: A Systematic Review" Healthcare 13, no. 16: 2056. https://doi.org/10.3390/healthcare13162056
APA StyleAljohani, S. (2025). Optical Coherence Tomography Angiography (OCTA) Characteristics of Acute Retinal Arterial Occlusion: A Systematic Review. Healthcare, 13(16), 2056. https://doi.org/10.3390/healthcare13162056







