Psychometric Evaluation of the Validity and Reliability of the Italian Version of the London Measure of Unplanned Pregnancy Amongst Postnatal Women
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethics
2.2. Translation Process
2.3. Data Collection Procedure
2.4. Measures
2.4.1. Demographics
2.4.2. The London Measure of Unplanned Pregnancy
2.4.3. The Edinburgh Postnatal Depression Scale
2.4.4. The Generalized Anxiety Disorder-7
2.4.5. Postpartum Specific Anxiety Scale
2.4.6. Postpartum Bonding Questionnaire
2.4.7. Baby Care Questionnaire Version 2
2.5. Data Analysis: Evaluating Psychometric Properties of the LMUP-IT and Hypotheses
2.5.1. Targeting
2.5.2. Reliability
2.5.3. Construct Validity
2.6. Exploratory Analysis of LMUP with Other Measures
3. Results
3.1. Sample Description
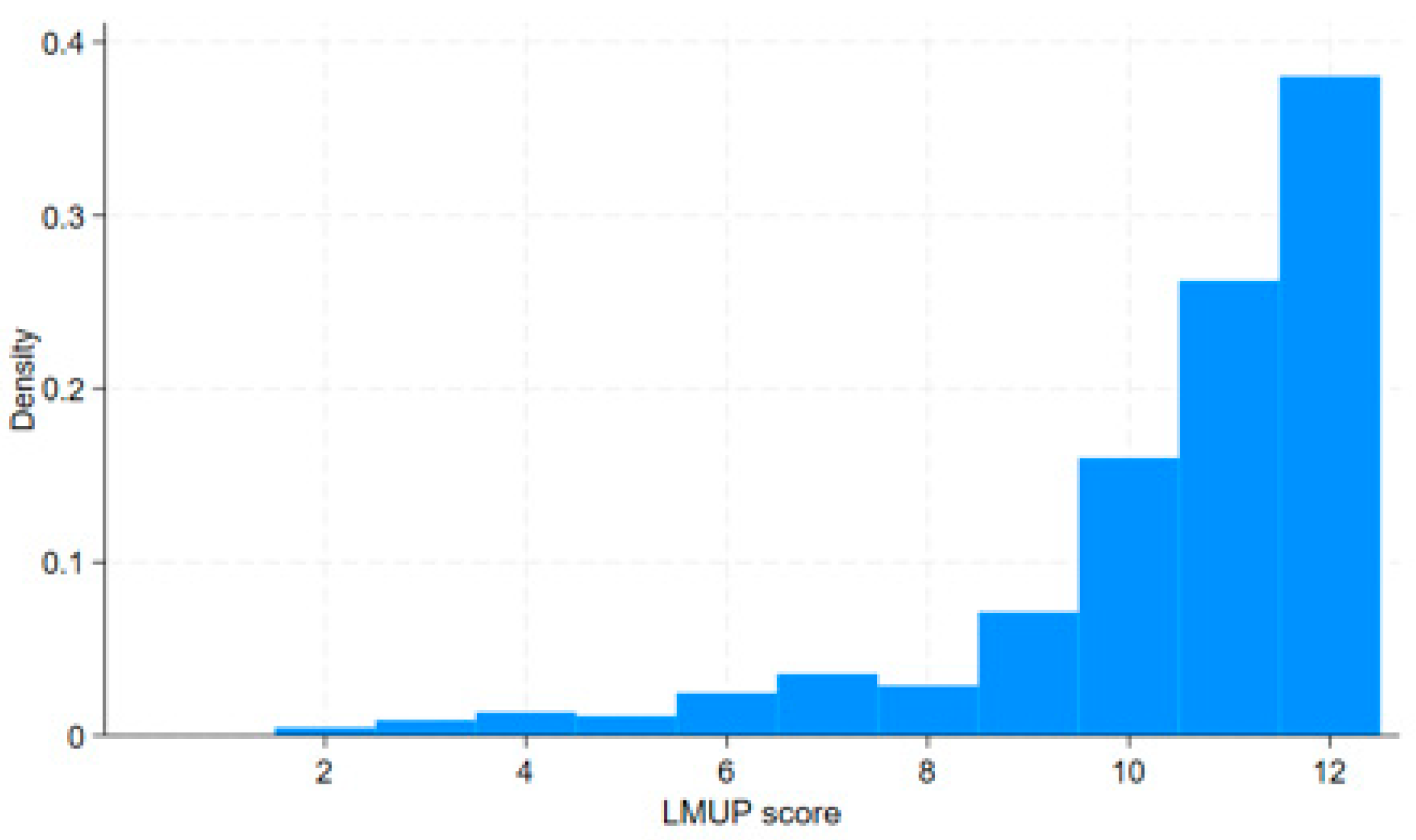
3.2. Targeting
3.3. Reliability
3.4. Construct Validity
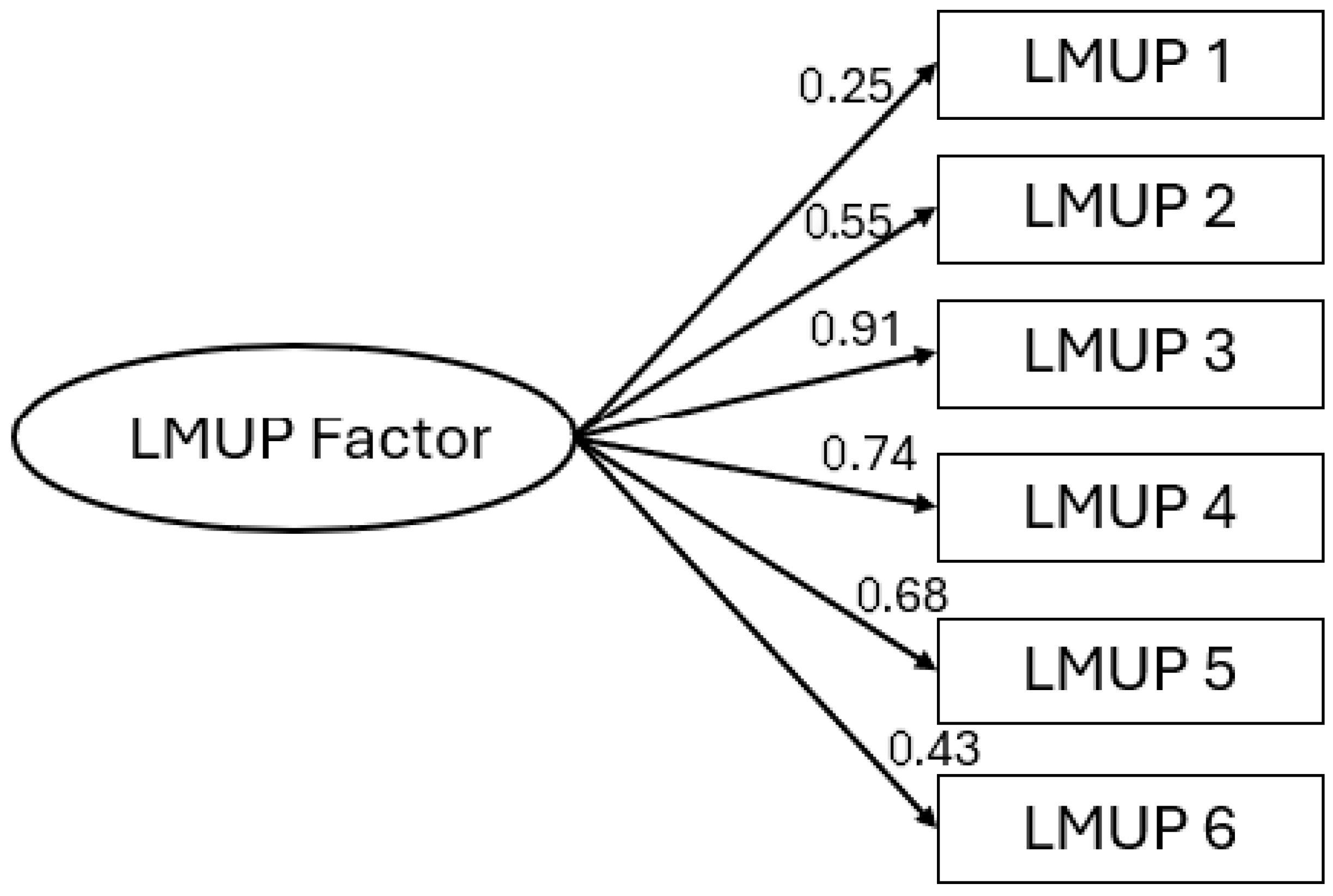
3.4.1. CFA in Italian Sample
3.4.2. Cross-Cultural Validity—Measurement Invariance Testing
3.4.3. Hypothesis Testing with ‘Known Groups’
3.5. Exploratory Analysis of LMUP with Other Measures
4. Discussion
4.1. Summary of Main Findings
4.2. Interpretation in Light of Published Literature
4.3. Strengths, Limitations, and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ranatunga, I.D.J.C.; Jayaratne, K. Proportion of unplanned pregnancies, their determinants and health outcomes of women delivering at a teaching hospital in Sri Lanka. BMC Pregnancy Childbirth 2020, 20, 667. [Google Scholar] [CrossRef] [PubMed]
- European Institute of Women’s Health. Maternal Health in the European Union Report. 2022. Available online: https://eurohealth.ie/wp-content/uploads/2023/12/Maternal-Report-2023.pdf (accessed on 24 June 2025).
- Loghi, M.; D’Errico, A.; Crialesi, R. L’interruzione Volontaria di Gravidanza in Un’ottica Generazionale. Istituto Nazionale di Statistica. 2024. Available online: https://www.istat.it/wp-content/uploads/2024/08/interruzione-volontaria-gravidanza-Ebook.pdf (accessed on 24 June 2025).
- Nappi, R.E.; Farris, M.; Gallina Toschi, A.; Michieli, R.; Moccia, F.; Orthmann, N.; Arisi, E. Overcoming barriers to oral contraception in Italy an expert opinion to empower women. Gynecol. Endocrinol. 2023, 39. [Google Scholar] [CrossRef] [PubMed]
- Minello, A. Non è un Paese per Madri; Editori Laterza: Bari, Italy, 2022. [Google Scholar]
- Gribaldo, A.; Judd, M.D.; Kertzer, D.I. An imperfect contraceptive society: Fertility and contraception in Italy. Popul. Dev. Rev. 2009, 35, 551–584. [Google Scholar] [CrossRef]
- Michelson, J. What women want when faced with an unplanned pregnancy. Sex. Health 2007, 4, 297. [Google Scholar] [CrossRef]
- Barrett, G.; Smith, S.C.; Wellings, K. Conceptualisation, development, and evaluation of a measure of unplanned pregnancy. J. Epidemiol. Community Health 2004, 58, 426–433. [Google Scholar] [CrossRef]
- Goossens, J.; Verhaeghe, S.; Van Hecke, A.; Barrett, G.; Delbaere, I.; Beeckman, D. Psychometric properties of the Dutch version of the London Measure of Unplanned Pregnancy in women with pregnancies ending in birth. PLoS ONE 2018, 13, e0194033. [Google Scholar] [CrossRef] [PubMed]
- Mallard, S.R.; Houghton, L.A. Socio-demographic characteristics associated with unplanned pregnancy in New Zealand: Implications for access to preconception healthcare. ANZJOG 2013, 53, 498–501. [Google Scholar] [CrossRef]
- Mohllajee, A.P.; Curtis, K.M.; Morrow, B.; Marchbanks, P.A. Pregnancy intention and its relationship to birth and maternal outcomes. Obs. Gynecol. 2007, 109, 678–686. [Google Scholar] [CrossRef]
- Maxson, P.; Miranda, M.L. Pregnancy intention, demographic differences, and psychosocial health. J. Womens Health 2011, 20, 1215–1223. [Google Scholar] [CrossRef]
- Postlethwaite, D.; Armstrong, M.A.; Hung, Y.Y.; Shaber, R. Pregnancy outcomes by pregnancy intention in a managed care setting. Matern. Child. Health J. 2010, 14, 227–234. [Google Scholar] [CrossRef]
- Stephenson, J.; Heslehurst, N.; Hall, J.; Schoenaker, D.A.; Hutchinson, J.; Cade, J.E.; Mishra, G.D. Before the beginning: Nutrition and lifestyle in the preconception period and its importance for future health. Lancet 2018, 391, 1830–1841. [Google Scholar] [CrossRef] [PubMed]
- Yu, P.; Jiang, Y.; Zhou, L.; Li, K.; Xu, Y.; Meng, F.; Zhou, Y. Association between pregnancy intention and smoking or alcohol consumption in the preconception and pregnancy periods: A systematic review and meta-analysis. J. Clin. Nurs. 2022, 31, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Roshanaei, S.; Shaghaghi, A.; Jafarabadi, M.A.; Kousha, A. Measuring unintended pregnancies in postpartum Iranian women: Validation of the London Measure of Unplanned Pregnancy. East. Mediterr. Health J. 2015, 22, 572–578. [Google Scholar] [CrossRef]
- Grussu, P.; Quatraro, R.M.; Nasta, M.T. Profile of mood states and parental attitudes in motherhood: Comparing women with planned and unplanned pregnancies. Birth 2005, 32, 107–114. [Google Scholar] [CrossRef]
- Abbasi, S.; Chuang, C.H.; Dagher, R.; Zhu, J.; Kjerulff, K. Unintended pregnancy and postpartum depression among first-time mothers. J. Womens Health 2013, 22, 412–416. [Google Scholar] [CrossRef]
- Qiu, X.; Zhang, S.; Sun, X.; Li, H.; Wang, D. Unintended pregnancy and postpartum depression: A meta-analysis of cohort and case-control studies. J. Psychosom. Res. 2020, 138, 110259. [Google Scholar] [CrossRef]
- Boden, J.M.; Fergusson, D.M.; Horwood, L.J. Outcomes for children and families following unplanned pregnancy: Findings from a longitudinal birth cohort. Child. Ind. Res. 2015, 8, 389–402. [Google Scholar] [CrossRef]
- Hall, J.A.; Barrett, G.; Copas, A.; Stephenson, J. London Measure of Unplanned Pregnancy: Guidance for its use as an outcome measure. Patient Relat. Outcome Meas. 2017, 8, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Finer, L.B.; Zolna, M.R. Unintended pregnancy in the United States: Incidence and disparities, 2006. Contraception 2011, 84, 478–485. [Google Scholar] [CrossRef]
- The Demographic and Health Surveys (DHS) Program. Available online: https://www.dhsprogram.com/ (accessed on 24 June 2025).
- Barrett, G.; Wellings, K. What is a ‘planned’ pregnancy? Empirical data from a British study. Soc. Sci. Med. 2002, 55, 545–557. [Google Scholar] [CrossRef]
- Luker, K.C. A reminder that human behavior frequently refuses to conform to models created by researchers. Fam. Plann Perspect. 1999, 31, 248–249. [Google Scholar] [CrossRef]
- Petersen, R.; Moos, M.K. Defining and measuring unintended pregnancy: Issues and concerns. Womens Health Issues 1997, 7, 234–240. [Google Scholar] [CrossRef]
- London Measure of Unplanned Pregnancy (LMUP). Available online: https://www.lmup.org.uk/versions.htm (accessed on 17 March 2025).
- Hall, J.A.; Stephenson, J.; Barrett, G. On the stability of reported pregnancy intentions from pregnancy to 1 year postnatally: Impact of choice of measure, timing of assessment, women’s characteristics and outcome of pregnancy. Matern. Child. Health J. 2019, 23, 1177–1186. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; De Vet, H.C. The COSMIN checklist for assessing methodological quality of studies on measurement properties of health status measurement instruments: An international Delphi study. Qual. Life Res. 2010, 19, 539–549. [Google Scholar] [CrossRef] [PubMed]
- Reeve, B.B.; Wyrwich, K.W.; Wu, A.W.; Velikova, G.; Terwee, C.B.; Snyder, C.F.; Schwartz, C.; Revicki, D.A.; Moinpour, C.M.; Butt, Z.; et al. ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual. Life Res. 2013, 22, 1889–1905. [Google Scholar] [CrossRef]
- Barrett, G.; Nolan, E.M.; Gürtin, Z.B.; Stephenson, J.; Hall, J.A. London Measure of Unplanned Pregnancy and newer family forms: An update. J. Epidemiol. Community Health 2020, 74, 765. [Google Scholar] [CrossRef] [PubMed]
- London Measure of Unplanned Pregnancy (LMUP-IT). Available online: https://www.lmup.org.uk/docs/LMUPItalian.pdf (accessed on 24 June 2025). (In Italian).
- Cox, J.L.; Holden, J.M.; Sagovsky, R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br. J. Psychiatry 1987, 150, 782–786. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.; Löwe, B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Fallon, V.; Halford, J.C.G.; Bennett, K.M.; Harrold, J.A. The postpartum specific anxiety scale: Development and preliminary validation. Arch. Womens Ment. Health 2016, 19, 1079–1090. [Google Scholar] [CrossRef]
- Winstanley, A.; Gattis, M. The Baby Care Questionnaire: A measure of parenting principles and practices during infancy. Infant. Behav. Dev. 2013, 36, 762–775. [Google Scholar] [CrossRef]
- Brockington, I.F.; Oates, J.; George, S.; Turner, D.; Vostanis, P.; Sullivan, M.; Loh, C.; Murdoch, C. A screening questionnaire for mother-infant bonding disorders. Arch. Women Ment. Health 2001, 3, 133–140. [Google Scholar] [CrossRef]
- Benvenuti, P.; Ferrara, M.; Niccolai, C.; Valoriani, V.; Cox, J.L. The Edinburgh postnatal depression scale: Validation for an Italian sample. J. Affect. Disord. 1999, 53, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Bolgeo, T.; Di Matteo, R.; Simonelli, N.; Dal Molin, A.; Lusignani, M.; Bassola, B.; Vellone, E.; Maconi, A.; Iovino, P. Psychometric properties and measurement invariance of the 7-item General Anxiety Disorder scale (GAD-7) in an Italian coronary heart disease population. J. Affect. Disord. 2023, 334, 213–219. [Google Scholar] [CrossRef]
- Ionio, C.; Ciuffo, G.; Landoni, M.; Smorti, M.; Della Vedova, A.M.; Christiansen, P.; Fallon, V.; Silverio, S.A.; Bramante, A. The Italian language postpartum specific anxiety scale [PSAS-IT]: Translation, psychometric evaluation, and validation. Front. Psychiatry 2023, 14, 1208613. [Google Scholar] [CrossRef]
- Busonera, A.; Cataudella, S.; Lampis Tommasi, M.; Zavattini, G.C. Psychometric properties of the Postpartum Bonding Questionnaire and correlates of mother–infant bonding impairment in Italian new mothers. Midwifery 2017, 55, 15–22. [Google Scholar] [CrossRef] [PubMed]
- Mascheroni, E.; Gattis, M.; Ionio, C. Psychometric properties of the Baby Care Questionnaire in an Italian sample of parents. In Proceedings of the XIV Giornate di Aggiornamento Sull’uso Degli Strumenti in Psicologia Clinica Dello Sviluppo, Bologna, Italy, 17–18 March 2017. [Google Scholar]
- Lang, A.Y.; Hall, J.A.; Boyle, J.A.; Harrison, C.L.; Teede, H.; Moran, L.J.; Barrett, G. Validation of the London Measure of Unplanned Pregnancy among pregnant Australian women. PLoS ONE 2019, 14, e0220774. [Google Scholar] [CrossRef] [PubMed]
- Streiner, D.L.; Norman, G.R. Health Measurement Scales: A Practical Guide to Their Development and Use, 4th ed.; Oxford University Press: New York, NY, USA, 2008. [Google Scholar]
- Cronbach, L.J. Essentials of Psychologic Testing; Harper and Row: New York, NY, USA, 1990. [Google Scholar]
- Malkewitz, C.P.; Schwall, P.; Meesters, C.; Hardt, J. Estimating reliability: A comparison of Cronbach’s α, McDonald’s ωt and the greatest lower bound. Soc. Sci. Humanit. Open 2023, 7, 100368. [Google Scholar] [CrossRef]
- McNeish, D. Thanks coefficient alpha, we’ll take it from here. Psychol. Methods 2018, 23, 412–433. [Google Scholar] [CrossRef] [PubMed]
- Prinsen, C.A.; Vohra, S.; Rose, M.R.; Boers, M.; Tugwell, P.; Clarke, M.; Williamson, P.R.; Terwee, C.B. How to select outcome measurement instruments for outcomes included in a “Core Outcome Set”—A practical guideline. Trials 2016, 17, 1–10. [Google Scholar] [CrossRef]
- Wolf, E.J.; Harrington, K.M.; Clark, S.L.; Miller, M.W. Sample size requirements for structural equation models: An evaluation of power, bias, and solution propriety. Educ. Psych. Meas. 2013, 73, 913–934. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Régnier-Loilier, A.; Vignoli, D. Fertility Intentions and Obstacles to their Realization in France and Italy. Population-E 2011, 66, 361–390. [Google Scholar] [CrossRef]
- Ministero Della Salute Certificato di Assistenza al Parto (CeDAP). Analisi Dell’evento Nascita Anno. 2023. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3524_allegato.pdf (accessed on 20 June 2025).
- Stephenson, J.; Patel, D.; Barrett, G.; Howden, B.; Copas, A.; Ojukwu, O.; Pandya, P.; Shawe, J. How Do Women Prepare for Pregnancy? Preconception Experiences of Women Attending Antenatal Services and Views of Health Professionals. PLoS ONE 2014, 9, e103085. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.; Barrett, G.; Mbwana, N.; Copas, A.; Malata, A.; Stephenson, J. Understanding pregnancy planning in a low-income country setting: Validation of the London measure of unplanned pregnancy in Malawi. BMC Pregnancy Childbirth 2013, 13, 200. [Google Scholar] [CrossRef] [PubMed]
- Hall, J.A.; Stephenson, J.; Barrett, G. 2021 Evaluating the Chichewa version of the London Measure of Unplanned Pregnancy in Malawi: A validation update. BMC Res. Notes 2021, 14, 231. [Google Scholar] [CrossRef]
- Leong, L.E.; Cano, A.; Johansen, A.B. Sequential and base rate analysis of emotional validation and invalidation in chronic pain couples: Patient gender matters. J. Pain. 2011, 12, 1140–1148. [Google Scholar] [CrossRef]
- Lebano, A.; Jamieson, L. Childbearing in Italy and Spain: Postponement Narratives. Popul. Dev. Rev. 2020, 46, 121–144. [Google Scholar] [CrossRef]
- Hays, S. The Cultural Contradictions of Motherhood; Yale University Press: New Haven, CT, USA, 1996. [Google Scholar]
- Ennis, L.R. Intensive Mothering: The Cultural Contradictions of Modern Motherhood; Demeter Press: Toronto, ON, Canada, 2014. [Google Scholar]
- Loyal, D.; Sutter, A.L.; Rascle, N. Mothering ideology and work involvement in late pregnancy: A clustering approach. J. Child. Fam. Stud. 2017, 26, 2921–2935. [Google Scholar] [CrossRef]
- McCarthy, O.L.; Palmer, M.J.; Gubijev, A.; Wellings, K.; Mann, S.; Leon, L.; Callaghan, F.; Patterson, S.; French, R.S. Achieving proportional representation in a reproductive health survey through social media: Process and recommendations. BMC Public. Health 2022, 22, 1370. [Google Scholar] [CrossRef]
- Gauthier, A.H. The State and the Family: A Comparative Analysis of Family Policies in Industrialized Countries; Clarendon Press: Oxford, UK, 1996. [Google Scholar]
- Sturm, N.; Koops, J.C.; Rutigliano, R. The influence of partnership status on fertility intentions of childless women and men across European countries. Eur. J. Popul. 2023, 39, 20. [Google Scholar] [CrossRef] [PubMed]
| n (%) | National Data | |
|---|---|---|
| Nationality | ||
| Italian | 437 (97.1%) | 79.9% |
| Others | 13 (2.9%) | 20.1% |
| Educational level | ||
| Secondary school | 20 (4.4%) | 22.0% |
| High school | 158 (35.1%) | 42.4% |
| University degree | 272 (60.4%) | 35.6% |
| Occupational status | ||
| Employed | 405 (90%) | 60.1% |
| Unemployed | 21 (4.7%) | 14.2% |
| Housewife | 24 (5.3%) | 23.7% |
| Marital status | ||
| Married | 248 (55.1%) | 56.4% |
| Maiden | 201 (44.6%) | 41.7% |
| Separated | 1 (0.2%) | 1.9% |
| Couple status | ||
| In couple (married and/or coresident) | 448 (99.5) | - |
| Single | 2 (0.5) | - |
| Baby birth order | ||
| 1° | 312 (69.3%) | - |
| 2° | 112 (24.9%) | - |
| 3° | 20 (4.4%) | - |
| 4° or more | 6 (1.3%) | - |
| Items and Response Categories | n (%) |
|---|---|
| Item 1: Contraception | |
| 0—always using contraception | 8 (1.8) |
| 1—using sometimes or failed at least once | 15 (3.3) |
| 2—not using contraception | 427 (94.9) |
| Item 2: Timing | |
| 0—wrong time | 5 (1.1) |
| 1—ok, but not quite right time | 39 (8.7) |
| 2—right time | 406 (90.2) |
| Item 3: Intention | |
| 0—did not intend to get pregnant | 25 (2.6) |
| 1—intentions kept changing | 48 (10.7) |
| 2—intended to get pregnant | 377 (83.8) |
| Item 4: Desire for a baby | |
| 0—did not want to have a baby | 10 (2.2) |
| 1—mixed feelings about having a baby | 85 (18.9) |
| 2—wanted to have a baby | 355 (78.9) |
| Item 5: Partner discussion | |
| 0—Never discussed having children or solo pregnancy | 3 (0.7) |
| 1—discussed but not agreed to get pregnant | 78 (17.3) |
| 2—Agreed to get pregnant | 355 (82.0) |
| Item 6: Preconceptual preparations | |
| 0—no actions | 102 (22.7) |
| 1—1 action | 124 (27.6) |
| 2—2 or more actions | 224 (49.8) |
| Invariance | ∆CFI | ∆RMSEA | ∆SRMR |
|---|---|---|---|
| Metric | <0.001 | <0.001 | <0.038 * |
| Scalar | <0.001 | <0.001 | <0.004 |
| Strict | <0.001 | <0.001 | <0.012 |
| Measure | r, (df), p |
|---|---|
| PSAS Total | 0.10, (447), p = 0.034 |
| EPDS Total | −0.12, (439), p = 0.011 |
| GAD Total | −0.14, (430), p = 0.003 |
| PBQ Impaired Bonding | −0.22, (427), p < 0.001 |
| PBQ Rejection Pathological anger | −0.19, (427), p < 0.001 |
| PBQ Infant-focused Anxiety | −0.22, (427), p < 0.001 |
| PBQ Incipient Abuse | −0.08, (427), p = 0.090 |
| BCQ Attunement | 0.03, (322), p = 0.562 |
| BCQ Structure | 0.13, (322), p = 0.017 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Smorti, M.; Christiansen, P.; Barrett, G.; Hall, J.A.; Ionio, C.; Ciuffo, G.; Landoni, M.; Della Vedova, A.M.; Payne, E.; Richell, M.; et al. Psychometric Evaluation of the Validity and Reliability of the Italian Version of the London Measure of Unplanned Pregnancy Amongst Postnatal Women. Healthcare 2025, 13, 2052. https://doi.org/10.3390/healthcare13162052
Smorti M, Christiansen P, Barrett G, Hall JA, Ionio C, Ciuffo G, Landoni M, Della Vedova AM, Payne E, Richell M, et al. Psychometric Evaluation of the Validity and Reliability of the Italian Version of the London Measure of Unplanned Pregnancy Amongst Postnatal Women. Healthcare. 2025; 13(16):2052. https://doi.org/10.3390/healthcare13162052
Chicago/Turabian StyleSmorti, Martina, Paul Christiansen, Geraldine Barrett, Jennifer A. Hall, Chiara Ionio, Giulia Ciuffo, Marta Landoni, Anna Maria Della Vedova, Elana Payne, Mia Richell, and et al. 2025. "Psychometric Evaluation of the Validity and Reliability of the Italian Version of the London Measure of Unplanned Pregnancy Amongst Postnatal Women" Healthcare 13, no. 16: 2052. https://doi.org/10.3390/healthcare13162052
APA StyleSmorti, M., Christiansen, P., Barrett, G., Hall, J. A., Ionio, C., Ciuffo, G., Landoni, M., Della Vedova, A. M., Payne, E., Richell, M., Worrall, S., Mauri, G., Fallon, V., Bramante, A., & Silverio, S. A. (2025). Psychometric Evaluation of the Validity and Reliability of the Italian Version of the London Measure of Unplanned Pregnancy Amongst Postnatal Women. Healthcare, 13(16), 2052. https://doi.org/10.3390/healthcare13162052









