Connect Active Programme (CAP): A Pilot RCT to Enhance Physical Activity and Intergenerational Relationships Through Dyadic Digital Walking Exercises
Abstract
1. Introduction
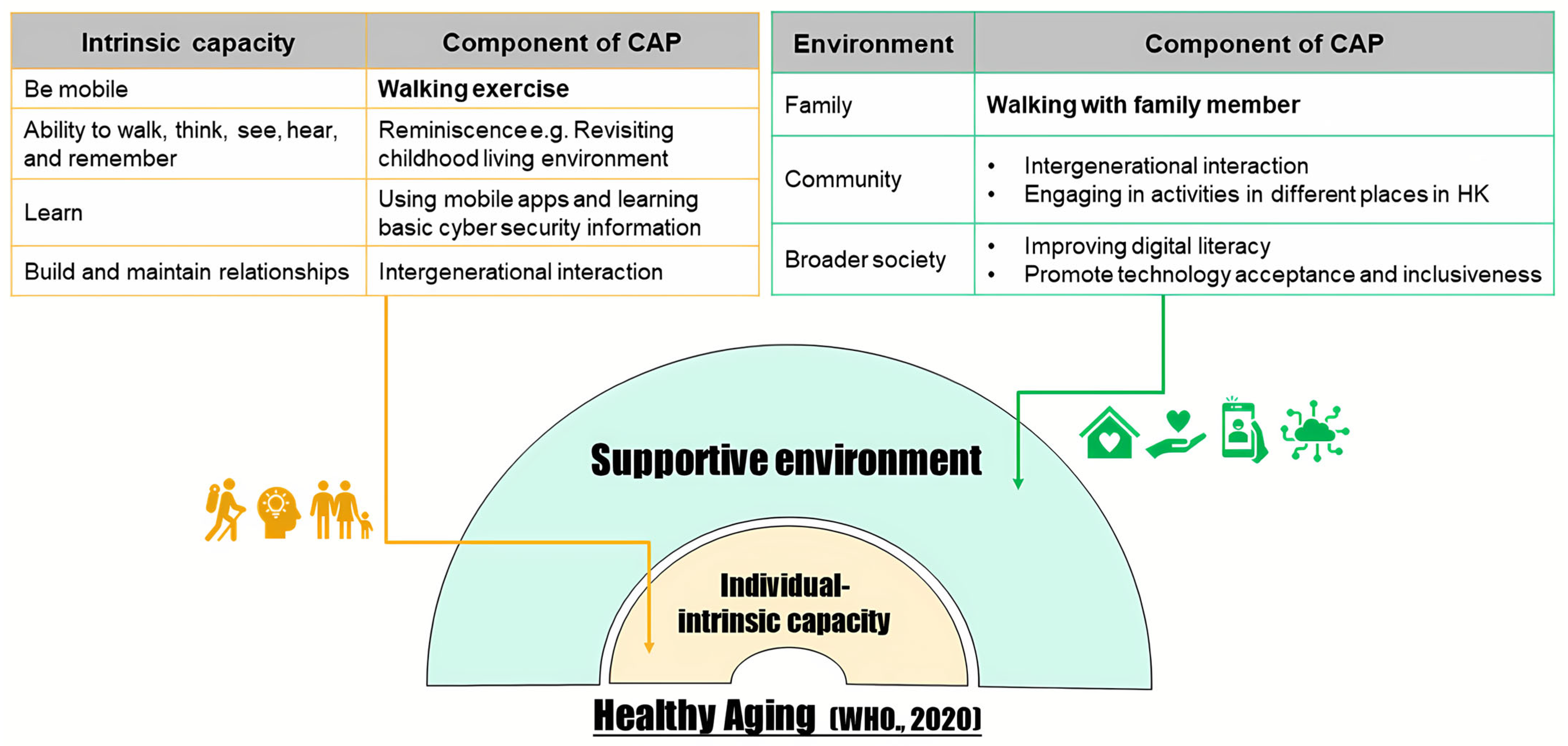
1.1. Conceptual Framework
1.2. Research Aims
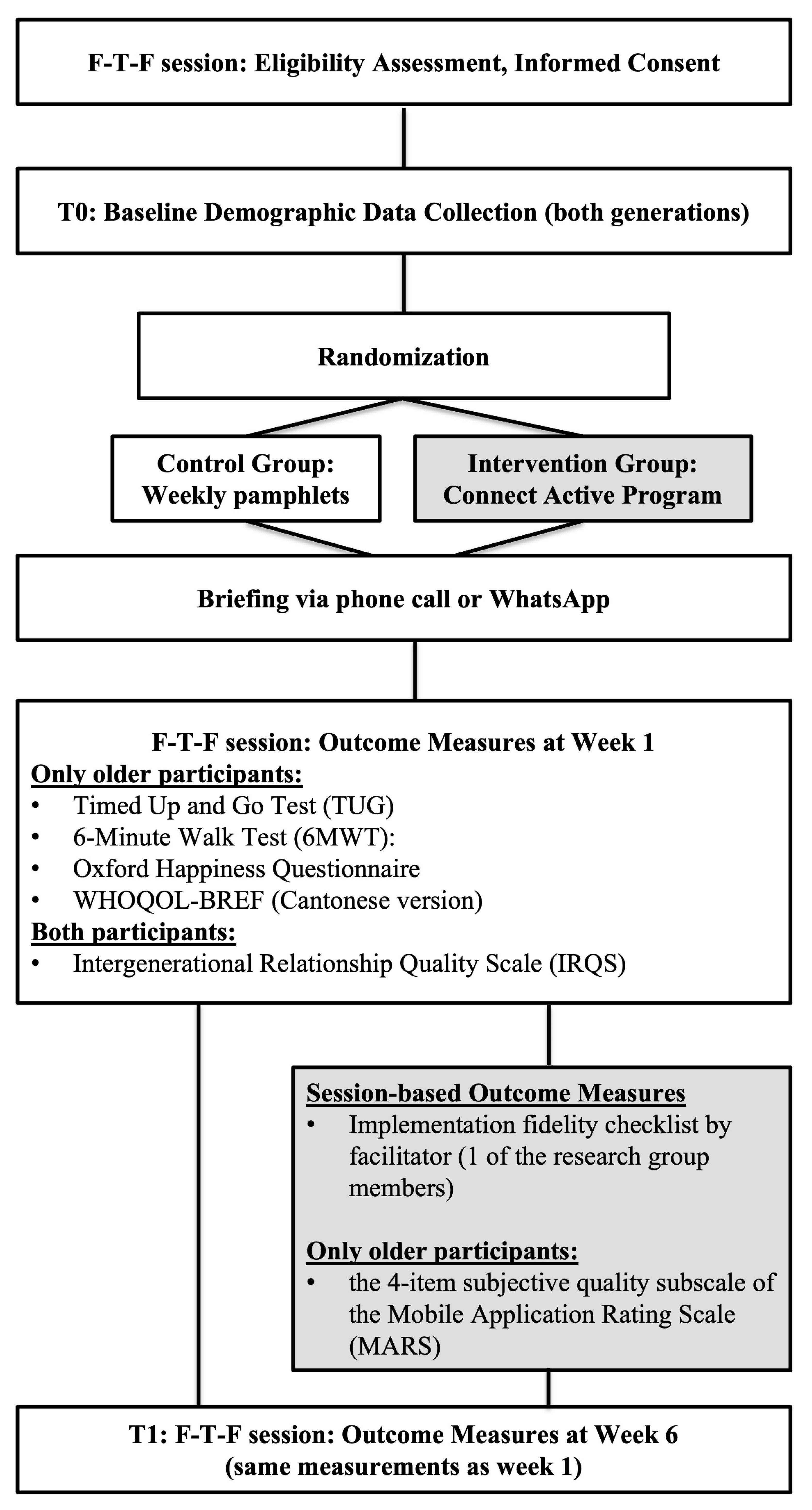
2. Methods
2.1. Study Design & Procedures
2.2. Participants and Sampling
2.3. Randomisation, Allocation Concealment, and Blinding
2.4. Intervention
2.5. Control Group
2.6. Descriptive Measures
2.7. Outcome Measures
2.7.1. Primary Outcome
2.7.2. Secondary Outcomes
- Time Up and Go (TUG) (measured in seconds) was used to assess mobility, movement, static balance, and dynamic balance in people with musculoskeletal impairments and conditions related to ageing, as well as quality of life and pain [32]. The instructions were given as follows: standing up from a chair, walking 3 m, turning, and sitting back down.
- Quality of life was evaluated utilising the World Health Organisation Quality of Life-BREF (WHOQOL-BREF). It contains four realms: physical health, psychological health, social relationships, and environment. A 5-point response scale was used in the scale [33]. WHOQOL-BREF has good validity and reliability [34].
- The Oxford Happiness Questionnaire is a 29-item measure of happiness, from 1, “strongly agree”, to 6, “strongly disagree”. The scale’s reliability was 0.91 [35]. Scores on the Oxford Happiness Questionnaire were not reversed; lower scores indicate higher levels of happiness, as per the original scoring guidelines.
- The intergenerational relationship quality scale (IRQS) was used to appraise the changes in intergenerational relationships. This questionnaire allowed the older participants to self-rate the relationship between the two generations. A five-point response scale was applied in the scale [36]. The Intergenerational Relationship Quality Scale (IRQS) has demonstrated good reliability and validity in prior studies involving older Chinese adults (Cronbach’s alpha = 0.86), making it suitable for our study population.
- The four-item subjective quality subscale of the Mobile Application Rating Scale (MARS) was deployed to assess the overall quality of mobile apps involved in this study [37]. MARS incorporates four objective quality subscales (engagement, functionality, aesthetics, and information quality) and one subjective quality subscale. Since a lengthy questionnaire would be complicated for the older participants to complete, the research team only adopted the subjective quality subscale. All four items were assessed on a five-point scale. The subjective quality subscale showed excellent internal consistency (alpha = 0.93) and inter-rater reliability, with an intraclass correlation coefficient (ICC = 0.83). Higher scores indicate a higher level of subjective quality. The subjective quality subscale of the Mobile Application Rating Scale (MARS) was self-administered by older participants in the intervention group to capture user perspectives on app quality.
2.8. Data Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAP | Connect Active Programme |
| PA | Physical Activity |
References
- Zhao, J.; Chau, J.P.C.; Zang, Y.; Lo, S.H.S.; Choi, K.C.; Liang, S. The effects of sitting Tai Chi on physical and psychosocial health outcomes among individuals with impaired physical mobility. Medicine 2020, 99, e21805. [Google Scholar] [CrossRef]
- Cunningham, C.; O’ Sullivan, R.; Caserotti, P.; Tully, M.A. Consequences of physical inactivity in older adults: A systematic review of reviews and meta-analyses. Scand. J. Med. Sci. Sports 2020, 30, 816–827. [Google Scholar] [CrossRef] [PubMed]
- Van Sluijs, E.M.F.; Ekelund, U.; Crochemore-Silva, I.; Guthold, R.; Ha, A.; Lubans, D.; Oyeyemi, A.L.; Ding, D.; Katzmarzyk, P.T. Physical activity behaviours in adolescence: Current evidence and opportunities for intervention. Lancet 2021, 398, 429–442. [Google Scholar] [CrossRef]
- Safi, A.; Cole, M.; Kelly, A.L.; Zariwala, M.G.; Walker, N.C. Workplace Physical Activity Barriers and Facilitators: A Qualitative Study Based on Employees Physical Activity Levels. Int. J. Environ. Res. Public. Health 2022, 19, 9442. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1·6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Department of Health. Fact Sheet on Physical Activity. Available online: https://www.dh.gov.hk/english/useful/useful_dykt/useful_dykt_exercise.html (accessed on 12 August 2024).
- Peters, R.; Ee, N.; Ward, S.A.; Kenning, G.; Radford, K.; Goldwater, M.; Dodge, H.H.; Lewis, E.; Xu, Y.; Kudrna, G.; et al. Intergenerational Programmes bringing together community dwelling non-familial older adults and children: A Systematic Review. Arch. Gerontol. Geriatr. 2021, 94, 104356. [Google Scholar] [CrossRef]
- Seino, S.; Kitamura, A.; Tomine, Y.; Tanaka, I.; Nishi, M.; Taniguchi, Y.; Yokoyama, Y.; Amano, H.; Fujiwara, Y.; Shinkai, S. Exercise Arrangement Is Associated with Physical and Mental Health in Older Adults. Med. Sci. Sports Exerc. 2019, 51, 1146–1153. [Google Scholar] [CrossRef]
- Yamada, P.M.; Teranishi-Hashimoto, C.; Bantum, E.O. Paired exercise has superior effects on psychosocial health compared to individual exercise in female cancer patients. Support. Care Cancer 2021, 29, 6305–6314. [Google Scholar] [CrossRef] [PubMed]
- Napetschnig, A.; Deiters, W. Requirements of Innovative Technologies to Promote Physical Activity Among Senior Citizens: A Systematic Literature Review. Inq. J. Health Care Organ. Provis. Financ. 2025, 62, 469580251349665. [Google Scholar] [CrossRef]
- Lai, D.W.L.; Zhou, J.-J.; Bai, X.; Lam, R.Y.K.; Li, Y.-Z. Intergenerational Engagement and Challenges: Participants’ Perspectives on Intergenerational Activities in Hong Kong. J. Intergener. Relatsh. 2023, 23, 30–49. [Google Scholar] [CrossRef]
- Pillemer, K.; Nolte, J.; Schultz, L.; Yau, H.; Henderson, C.R.; Cope, M.T.; Baschiera, B. The Benefits of Intergenerational Wisdom-Sharing: A Randomized Controlled Study. Int. J. Environ. Res. Public. Health 2022, 19, 4010. [Google Scholar] [CrossRef]
- Tse, M.M.Y.; Ngai, V.H.Y.; Tse, P.P.-S.; Kwok, C.P.S.; Cheung, K.K.M. The habits and preferences of smartphone use in obtaining health-related information among community-dwelling older adults. J. Aging Sci. 2023, 11, 336. Available online: https://www.walshmedicalmedia.com/open-access/the-habits-and-preferences-of-smartphone-use-in-obtaining-healthrelated-information-among-communitydwelling-older-adults.pdf (accessed on 4 May 2025).
- Lai, H.-J. Investigating older adults’ decisions to use mobile devices for learning, based on the unified theory of acceptance and use of technology. Interact. Learn. Environ. 2020, 28, 890–901. [Google Scholar] [CrossRef]
- Kwan, R.Y.C.; Ng, F.; Lai, M.; Wong, D.; Chan, S. The effects of Digital Buddy programme on older adults’ mental well-being: Study protocol for a multi-centre, cluster randomized controlled trial. Trials 2023, 24, 95. [Google Scholar] [CrossRef]
- Dong, Q.; Liu, T.; Liu, R.; Yang, H.; Liu, C. Effectiveness of Digital Health Literacy Interventions in Older Adults: Single-Arm Meta-Analysis. J. Med. Internet Res. 2023, 25, e48166. [Google Scholar] [CrossRef]
- Knight, T.; Skouteris, H.; Townsend, M.; Hooley, M. The Act of Giving: A Systematic Review of Nonfamilial Intergenerational Interaction. J. Intergener. Relatsh. 2014, 12, 257–278. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, K.; Dabelko-Schoeny, H. A Comprehensive Evaluation of a Lifelong Learning Program: Program 60. Int. J. Aging Hum. Dev. 2016, 84, 88–106. [Google Scholar] [CrossRef] [PubMed]
- Whear, R.; Campbell, F.; Rogers, M.; Sutton, A.; Robinson-Carter, E.; Sharpe, R.; Cohen, S.; Fergy, R.; Garside, R.; Kneale, D.; et al. What is the effect of intergenerational activities on the wellbeing and mental health of older people?: A systematic review. Campbell Syst. Rev. 2023, 19, e1355. [Google Scholar] [CrossRef] [PubMed]
- Au, A.; Ng, E.; Garner, B.; Lai, S.; Chan, K. Proactive Aging and Intergenerational Mentoring Program to Promote the Well-Being of Older Adults: Pilot Studies. Clin. Gerontol. 2015, 38, 203–210. [Google Scholar] [CrossRef]
- Petersen, J. A meta-analytic review of the effects of intergenerational programs for youth and older adults. Educ. Gerontol. 2023, 49, 175–189. [Google Scholar] [CrossRef]
- Giraudeau, C.; Bailly, N. Intergenerational programs: What can school-age children and older people expect from them? A systematic review. Eur. J. Ageing 2019, 16, 363–376. [Google Scholar] [CrossRef] [PubMed]
- Budden, T.; Coall, D.A.; Jackson, B.; Christian, H.; Nathan, A.; Jongenelis, M.I. Barriers and enablers to promoting grandchildren’s physical activity and reducing screen time: A qualitative study with Australian grandparents. BMC Public Health 2024, 24, 1670. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.A.; George, S.M.S.; Leite, R.O.; Esquives, B.N.; Wetstone, R.; Pulgaron, E.R.; Prado, G.; Czaja, S.J. Formative Development of a Technology-Based Physical Activity Intervention for Grandparents and Grandchildren. J. Aging Phys. Act. 2021, 30, 482–494. [Google Scholar] [CrossRef]
- He, A.W.J.; Yuan, R.; Luk, T.T.; Wang, K.M.P.; Chan, S.S.C. Boosting Digital Health Engagement Among Older Adults in Hong Kong: Pilot Pre-Post Study of the Generations Connect Project. JMIR Form. Res. 2025, 9, e69611. [Google Scholar] [CrossRef]
- Innovation and Technology Bureau. Smart City Blueprint 2.0; The Government of the Hong Kong Special Administrative Region: Hong Kong, China, 2020. Available online: https://www.smartcity.gov.hk/modules/custom/custom_global_js_css/assets/files/HKSmartCityBlueprint%28ENG%29v2.pdf (accessed on 28 July 2025).
- WHO. World Health Organization Decade of Healthy Ageing 2021–2030; WHO: Geneva, Switzerland, 2021; Available online: https://www.who.int/initiatives/decade-of-healthy-ageing (accessed on 28 July 2025).
- World Health Organization. Healthy Ageing and Functional Ability. Available online: https://www.who.int/news-room/questions-and-answers/item/healthy-ageing-and-functional-ability (accessed on 4 May 2025).
- Iliano, E.; Beeckman, M.; Latomme, J.; Cardon, G. The GRANDPACT Project: The Development and Evaluation of an Intergenerational Program for Grandchildren and Their Grandparents to Stimulate Physical Activity and Cognitive Function Using Co-Creation. Int. J. Environ. Res. Public. Health 2022, 19, 7150. [Google Scholar] [CrossRef]
- Juris, J.J.; Bouldin, E.D.; Uva, K.; Cardwell, C.D.; Schulhoff, A.; Hiegl, N. Virtual Intergenerational Reverse-Mentoring Program Reduces Loneliness among Older Adults: Results from a Pilot Evaluation. Int. J. Environ. Res. Public. Health 2022, 19, 7121. [Google Scholar] [CrossRef] [PubMed]
- Kammin, E.J. The 6-Minute Walk Test: Indications and Guidelines for Use in Outpatient Practices. J. Nurse Pract. 2022, 18, 608–610. [Google Scholar] [CrossRef]
- Buraschi, R.; Pollet, J.; Villafañe, J.H.; Piovanelli, B.; Negrini, S. Temporal and kinematic analyses of timed up and go test in chronic low back pain patients. Gait Posture 2022, 96, 137–142. [Google Scholar] [CrossRef]
- The Whoqol Group. Development of the World Health Organization WHOQOL-BREF Quality of Life Assessment. Psychol. Med. 1998, 28, 551–558. [Google Scholar] [CrossRef]
- Leung, K.F.; Wong, W.W.; Tay, M.S.M.; Chu, M.M.L.; Ng, S.S.W. Development and validation of the interview version of the Hong Kong Chinese WHOQOL-BREF. Qual. Life Res. 2005, 14, 1413–1419. [Google Scholar] [CrossRef] [PubMed]
- Kamthan, S.; Sharma, S.; Bansal, R.; Pant, B.; Saxena, P.; Chansoria, S.; Shukla, A. Happiness among second year MBBS students and its correlates using Oxford Happiness Questionnaire. J. Oral Biol. Craniofac. Res. 2019, 9, 190–192. [Google Scholar] [CrossRef]
- Bai, X. Development and Validation of a Multidimensional Intergenerational Relationship Quality Scale for Aging Chinese Parents. Gerontologist 2018, 58, e338–e348. [Google Scholar] [CrossRef] [PubMed]
- Stoyanov, S.R.; Hides, L.; Kavanagh, D.J.; Zelenko, O.; Tjondronegoro, D.; Mani, M. Mobile App Rating Scale: A New Tool for Assessing the Quality of Health Mobile Apps. JMIR MHealth UHealth 2015, 3, e27. [Google Scholar] [CrossRef]
- MacFarland, T.W.; Yates, J.M. Introduction to Nonparametric Statistics for the Biological Sciences Using R; Springer International Publishing: Cham, Switzerland, 2016; Available online: http://link.springer.com/10.1007/978-3-319-30634-6 (accessed on 12 August 2024)ISBN 978-3-319-30633-9.
- McKnight, P.E.; Najab, J. Mann-Whitney U Test. In The Corsini Encyclopedia of Psychology, 1st ed.; Weiner, I.B., Craighead, W.E., Eds.; Wiley: Hoboken, NJ, USA, 2010; p. 1. Available online: https://onlinelibrary.wiley.com/doi/10.1002/9780470479216.corpsy0524 (accessed on 12 August 2024)ISBN 978-0-470-17024-3.
- Zhong, S.; Lee, C.; Foster, M.J.; Bian, J. Intergenerational communities: A systematic literature review of intergenerational interactions and older adults’ health-related outcomes. Soc. Sci. Med. 2020, 264, 113374. [Google Scholar] [CrossRef] [PubMed]
- Raffin, J.; de Souto Barreto, P.; Le Traon, A.P.; Vellas, B.; Aubertin-Leheudre, M.; Rolland, Y. Sedentary behavior and the biological hallmarks of aging. Ageing Res. Rev. 2023, 83, 101807. [Google Scholar] [CrossRef]
- Park, J.H.; Moon, J.H.; Kim, H.J.; Kong, M.H.; Oh, Y.H. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J. Fam. Med. 2020, 41, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Ferreira Silva, R.M.; Mendonça, C.R.; Azevedo, V.D.; Raoof Memon, A.; Noll, P.R.E.S.; Noll, M. Barriers to high school and university students’ physical activity: A systematic review. PLoS ONE 2022, 17, e0265913. [Google Scholar] [CrossRef] [PubMed]
- Keadle, S.K.; Conroy, D.E.; Buman, M.P.; Dunstan, D.W.; Matthews, C.E. Targeting Reductions in Sitting Time to Increase Physical Activity and Improve Health. Med. Sci. Sports Exerc. 2017, 49, 1572–1582. [Google Scholar] [CrossRef]
- VanderWeele, T.J.; Trudel-Fitzgerald, C.; Allin, P.; Farrelly, C.; Fletcher, G.; Frederick, D.E.; Hall, J.; Helliwell, J.F.; Kim, E.S.; Lauinger, W.A.; et al. Current recommendations on the selection of measures for well-being. Prev. Med. 2020, 133, 106004. [Google Scholar] [CrossRef]
- World Health Organization. Global Physical Activity Questionnaire (GPAQ); World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/m/item/global-physical-activity-questionnaire (accessed on 4 May 2025).
- Buonsenso, A.; Fiorilli, G.; Mosca, C.; Centorbi, M.; Notarstefano, C.C.; Di Martino, G.; Calcagno, G.; Intrieri, M.; di Cagno, A. Exploring the Enjoyment of the Intergenerational Physical Activity. J. Funct. Morphol. Kinesiol. 2021, 6, 51. [Google Scholar] [CrossRef]
- Neace, S.M.; Hicks, A.M.; DeCaro, M.S.; Salmon, P.G. Trait mindfulness and intrinsic exercise motivation uniquely contribute to exercise self-efficacy. J. Am. Coll. Health 2022, 70, 13–17. [Google Scholar] [CrossRef] [PubMed]
- Raichlen, D.A.; Aslan, D.H.; Sayre, M.K.; Bharadwaj, P.K.; Ally, M.; Maltagliati, S.; Lai, M.H.C.; Wilcox, R.R.; Klimentidis, Y.C.; Alexander, G.E. Sedentary Behavior and Incident Dementia Among Older Adults. JAMA 2023, 330, 934–940. [Google Scholar] [CrossRef]
- Zou, L.; Herold, F.; Cheval, B.; Wheeler, M.J.; Pindus, D.M.; Erickson, K.I.; Raichlen, D.A.; Alexander, G.E.; Müller, N.G.; Dunstan, D.W.; et al. Sedentary behavior and lifespan brain health. Trends Cogn. Sci. 2024, 28, 369–382. [Google Scholar] [CrossRef] [PubMed]
- Wheeler, M.J.; Dempsey, P.C.; Grace, M.S.; Ellis, K.A.; Gardiner, P.A.; Green, D.J.; Dunstan, D.W. Sedentary behavior as a risk factor for cognitive decline? A focus on the influence of glycemic control in brain health. Alzheimers Dement. Transl. Res. Clin. Interv. 2017, 3, 291–300. [Google Scholar] [CrossRef]
- Cauwenberg, J.V.; Holle, V.V.; Bourdeaudhuij, I.D.; Owen, N.; Deforche, B. Diurnal Patterns and Correlates of Older Adults’ Sedentary Behavior. PLoS ONE 2015, 10, e0133175. [Google Scholar] [CrossRef]
- Ungvari, Z.; Fazekas-Pongor, V.; Csiszar, A.; Kunutsor, S.K. The multifaceted benefits of walking for healthy aging: From Blue Zones to molecular mechanisms. GeroScience 2023, 45, 3211–3239. [Google Scholar] [CrossRef]
- Vaegter, H.B.; Kinnunen, M.; Verbrugghe, J.; Cunningham, C.; Meeus, M.; Armijo-Olivo, S.; Bandholm, T.; Fullen, B.M.; Wittink, H.; Morlion, B.; et al. Physical activity should be the primary intervention for individuals living with chronic pain A position paper from the European Pain Federation (EFIC) ‘On the Move’ Task Force. Eur. J. Pain 2024, 28, 1249–1256. [Google Scholar] [CrossRef]
- Welmer, A.-K.; Rizzuto, D.; Qiu, C.; Caracciolo, B.; Laukka, E.J. Walking Speed, Processing Speed, and Dementia: A Population-Based Longitudinal Study. J. Gerontol. Ser. A 2014, 69, 1503–1510. [Google Scholar] [CrossRef]
- Kim, C.; Kim, B.O.; Lim, K.-B.; Kim, Y.J.; Park, Y.B. The Effect of Power-walking in Phase 2 Cardiac Rehabilitation Program. Ann. Rehabil. Med. 2012, 36, 133–140. [Google Scholar] [CrossRef] [PubMed]
- Murtagh, E.M.; Mair, J.L.; Aguiar, E.; Tudor-Locke, C.; Murphy, M.H. Outdoor Walking Speeds of Apparently Healthy Adults: A Systematic Review and Meta-analysis. Sports Med. 2021, 51, 125–141. [Google Scholar] [CrossRef]
- Kan, S.; Fujita, N.; Shibata, M.; Miki, K.; Yukioka, M.; Senba, E. Three weeks of exercise therapy altered brain functional connectivity in fibromyalgia inpatients. Neurobiol. Pain 2023, 14, 100132. [Google Scholar] [CrossRef] [PubMed]
- Mendez Colmenares, A.; Voss, M.W.; Fanning, J.; Salerno, E.A.; Gothe, N.P.; Thomas, M.L.; McAuley, E.; Kramer, A.F.; Burzynska, A.Z. White matter plasticity in healthy older adults: The effects of aerobic exercise. NeuroImage 2021, 239, 118305. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Chen, C.; Yu, Y.; Zhang, H.; Tan, X.; Zhang, J.; Qi, L.; Lu, Y.; Wang, N. Replacement of leisure-time sedentary behavior with various physical activities and the risk of dementia incidence and mortality: A prospective cohort study. J. Sport. Health Sci. 2023, 12, 287–294. [Google Scholar] [CrossRef]
- Irvine, K.N.; Fisher, D.; Currie, M.; Colley, K.; Warber, S.L. A Nature-Based Intervention for Promoting Physical Activity in Older Adults: A Qualitative Study Using the COM-B Model. Int. J. Environ. Res. Public. Health 2024, 21, 843. [Google Scholar] [CrossRef]
- Krzeczkowska, A.; Spalding, D.M.; McGeown, W.J.; Gow, A.J.; Carlson, M.C.; Nicholls, L.A.B. A systematic review of the impacts of intergenerational engagement on older adults’ cognitive, social, and health outcomes. Ageing Res. Rev. 2021, 71, 101400. [Google Scholar] [CrossRef]
- Schroeder, K.; Ratcliffe, S.J.; Perez, A.; Earley, D.; Bowman, C.; Lipman, T.H. Dance for Health: An Intergenerational Program to Increase Access to Physical Activity. J. Pediatr. Nurs. 2017, 37, 29–34. [Google Scholar] [CrossRef]
- World Health Organization. Digital Health. Available online: https://www.who.int/health-topics/digital-health (accessed on 9 August 2024).
- Wilson, N.J.; Cordier, R.; Wilson Whatley, L. Older male mentors’ perceptions of a Men’s Shed intergenerational mentoring program. Aust. Occup. Ther. J. 2013, 60, 416–426. [Google Scholar] [CrossRef]
- Mahoney, N.; Wilson, N.J.; Buchanan, A.; Milbourn, B.; Hoey, C.; Cordier, R. Older male mentors: Outcomes and perspectives of an intergenerational mentoring program for young adult males with intellectual disability. Health Promot. J. Austr. 2020, 31, 16–25. [Google Scholar] [CrossRef]
- Burgess, R.L.; Huston, T.L. Social Exchange in Developing Relationships; Elsevier: Amsterdam, The Netherlands, 2013; 447p, ISBN 978-1-4832-6130-0. [Google Scholar]
- Chippendale, T. Elders’ Life Stories: Impact on the Next Generation of Health Professionals. Curr. Gerontol. Geriatr. Res. 2013, 2013, 493728. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, J.; Lee, J.-M.; Seo, D.-C.; Jung, H.C. Intergenerational Taekwondo Program: A Narrative Review and Practical Intervention Proposal. Int. J. Environ. Res. Public. Health 2022, 19, 5247. [Google Scholar] [CrossRef] [PubMed]
- Murayama, Y.; Ohba, H.; Yasunaga, M.; Nonaka, K.; Takeuchi, R.; Nishi, M.; Sakuma, N.; Uchida, H.; Shinkai, S.; Fujiwara, Y. The effect of intergenerational programs on the mental health of elderly adults. Aging Ment. Health 2015, 19, 306–314. [Google Scholar] [CrossRef]
- Minghetti, A.; Donath, L.; Zahner, L.; Hanssen, H.; Faude, O. Beneficial effects of an intergenerational exercise intervention on health-related physical and psychosocial outcomes in Swiss preschool children and residential seniors: A clinical trial. PeerJ 2021, 9, e11292. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, K.; Joseph, P.; Simmons, L. CONTACT QUALITY AND ATTITUDES TOWARD THE ELDERLY. Educ. Gerontol. 2001, 27, 127–137. [Google Scholar] [CrossRef]
- Bousfield, C.; Hutchison, P. Contact, Anxiety, and Young People’s Attitudes and Behavioral Intentions Towards the Elderly. Educ. Gerontol. 2010, 36, 451–466. [Google Scholar] [CrossRef]
| Demographics | Experimental (n = 10) | Control (n = 10) | |||
|---|---|---|---|---|---|
| Age | M | SD | M | SD | |
| 67.6 | 6.8 | 66.7 | 7.2 | ||
| n | % | n | % | ||
| Gender | Male | 5 | 50 | 5 | 50 |
| Female | 5 | 50 | 5 | 50 | |
| Education level | Below primary | 2 | 20 | 2 | 20 |
| Primary | 2 | 20 | 2 | 20 | |
| Secondary | 4 | 40 | 5 | 50 | |
| Tertiary or above | 2 | 20 | 1 | 10 | |
| Nature of the job | Full-time | 2 | 20 | 2 | 20 |
| Part-time | 0 | 0 | 0 | 0 | |
| Unemployed | 8 | 80 | 8 | 80 | |
| Monthly income (HKD) | ≤10,000 | 6 | 60 | 7 | 70 |
| 10,001–20,000 | 3 | 30 | 3 | 30 | |
| 20,001–30,000 | 1 | 10 | 0 | 0 | |
| >30,000 | 0 | 0 | 0 | 0 | |
| Exercise habit | Yes | 5 | 50 | 4 | 40 |
| No | 5 | 50 | 6 | 60 | |
| Drinking habit | Never | 6 | 60 | 10 | 100 |
| Sometimes | 4 | 40 | 0 | 0 | |
| ≥3 days per week | 0 | 0 | 0 | 0 | |
| Daily | 0 | 0 | 0 | 0 | |
| Smoking habit | Never | 9 | 90 | 10 | 100 |
| Sometimes | 1 | 10 | 0 | 0 | |
| ≥3 days per week | 0 | 0 | 0 | 0 | |
| Daily | 0 | 0 | 0 | 0 | |
| Chronic illness | 0 | 3 | 30 | 3 | 30 |
| 1 | 2 | 20 | 2 | 20 | |
| ≥2 | 5 | 50 | 5 | 50 | |
| Dependency | Independent | 10 | 100 | 10 | 100 |
| Dependent | 0 | 0 | 0 | 0 | |
| Demographics | Experimental (n = 10) | Control (n = 10) | |||
|---|---|---|---|---|---|
| Age | M | SD | M | SD | |
| 28.6 | 7.2 | 30.0 | 6.5 | ||
| n | % | n | % | ||
| Dyadic relationship | Parent–child | 10 | 100 | 10 | 100 |
| Gender | Male | 4 | 40 | 4 | 40 |
| Female | 6 | 60 | 6 | 60 | |
| Education level | Below primary | 0 | 0 | 0 | 0 |
| Primary | 0 | 0 | 0 | 0 | |
| Secondary | 1 | 10 | 1 | 10 | |
| Tertiary or above | 9 | 90 | 9 | 90 | |
| Nature of the job | Full-time | 9 | 90 | 9 | 90 |
| Part-time | 1 | 10 | 1 | 10 | |
| Unemployed | 0 | 0 | 0 | 0 | |
| Monthly income (HKD) | ≤10,000 | 3 | 30 | 3 | 30 |
| 10,001–20,000 | 0 | 0 | 0 | 0 | |
| 20,001–30,000 | 4 | 40 | 2 | 20 | |
| >30,000 | 3 | 30 | 5 | 50 | |
| Exercise habit | Yes | 7 | 70 | 5 | 50 |
| No | 3 | 30 | 5 | 50 | |
| Drinking habit | Never | 6 | 60 | 8 | 80 |
| Sometimes | 4 | 40 | 2 | 20 | |
| ≥3 days per week | 0 | 0 | 0 | 0 | |
| Daily | 0 | 0 | 0 | 0 | |
| Smoking habit | Never | 10 | 100 | 10 | 100 |
| Sometimes | 0 | 0 | 0 | 0 | |
| ≥3 days per week | 0 | 0 | 0 | 0 | |
| Daily | 0 | 0 | 0 | 0 | |
| Chronic illness | 0 | 10 | 100 | 10 | 100 |
| 1 | 0 | 0 | 0 | 0 | |
| ≥2 | 0 | 0 | 0 | 0 | |
| Dependency | Independent | 10 | 100 | 10 | 100 |
| Dependent | 0 | 0 | 0 | 0 | |
| Objective | Data Measurement | Result |
|---|---|---|
| To examine the effectiveness of the Connect Active Programme (CAP) on improving physical fitness. | 6-Minute Walk Test (6MWT) (measured in minutes) | Statistically significant (p = 0.005 *) |
| To examine the effectiveness of the Connect Active Programme (CAP) on improving physical fitness. | Time Up and Go (TUG) (measured in seconds) | Statistically nonsignificant (p = 0.123) |
| To examine the effectiveness of the Connect Active Programme (CAP) on improving psychological well-being. | WHOQOL-BREF (Cantonese version) | Statistically significant (p = 0.015 *) |
| To examine the effectiveness of the Connect Active Programme (CAP) on improving psychological well-being. | Oxford Happiness Questionnaire | Statistically nonsignificant (p = 0.393) |
| To examine the effectiveness of the Connect Active Programme (CAP) on improving intergenerational relationships. | Intergenerational relationship quality scale (IRQS) of older participants | Statistically nonsignificant (p = 0.315) |
| To examine the effectiveness of the Connect Active Programme (CAP) on improving intergenerational relationships. | Intergenerational relationship quality scale (IRQS) of younger participants | Statistically significant (p < 0.001 *) |
| To examine the experiences and feedback from participants in using the apps and joining the CAP. | Mobile Application Rating Scale (MARS) (session-based only for the experimental group) | Rated below equilibrium |
| Mobile Apps | N | Minimum | Maximum | Mean | Std. Deviation |
|---|---|---|---|---|---|
| Hong Kong Hiking Routes | 10 | 1 | 4 | 2.10 | 0.876 |
| Nike Run Club | 10 | 1 | 4 | 1.80 | 1.033 |
| 10 | 2 | 4 | 3.30 | 0.675 | |
| Google Map | 10 | 1 | 4 | 2.70 | 1.059 |
| Meitu | 10 | 1 | 2 | 1.30 | 0.483 |
| MTR/KMB * | 10 | 1 | 3 | 2.10 | 0.738 |
| Flower Companion | 10 | 1 | 2 | 1.20 | 0.422 |
| Valid N (listwise) | 10 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tse, M.M.Y.; Tse, P.P.-s.; Ip, K.Y.; Lam, H.Y.; Chong, P.S.; Kwok, T.T.O.; Sun, G.Y.; Chu, S.K.W.; To, K.P. Connect Active Programme (CAP): A Pilot RCT to Enhance Physical Activity and Intergenerational Relationships Through Dyadic Digital Walking Exercises. Healthcare 2025, 13, 2043. https://doi.org/10.3390/healthcare13162043
Tse MMY, Tse PP-s, Ip KY, Lam HY, Chong PS, Kwok TTO, Sun GY, Chu SKW, To KP. Connect Active Programme (CAP): A Pilot RCT to Enhance Physical Activity and Intergenerational Relationships Through Dyadic Digital Walking Exercises. Healthcare. 2025; 13(16):2043. https://doi.org/10.3390/healthcare13162043
Chicago/Turabian StyleTse, Mimi Mun Yee, Percy Poo-see Tse, Ka Yan Ip, Ho Yuen Lam, Pak San Chong, Tyrone Tai On Kwok, Grace Yuying Sun, Samuel Kai Wah Chu, and Kin Pong To. 2025. "Connect Active Programme (CAP): A Pilot RCT to Enhance Physical Activity and Intergenerational Relationships Through Dyadic Digital Walking Exercises" Healthcare 13, no. 16: 2043. https://doi.org/10.3390/healthcare13162043
APA StyleTse, M. M. Y., Tse, P. P.-s., Ip, K. Y., Lam, H. Y., Chong, P. S., Kwok, T. T. O., Sun, G. Y., Chu, S. K. W., & To, K. P. (2025). Connect Active Programme (CAP): A Pilot RCT to Enhance Physical Activity and Intergenerational Relationships Through Dyadic Digital Walking Exercises. Healthcare, 13(16), 2043. https://doi.org/10.3390/healthcare13162043






