Psychometric Properties of the Arabic Version of the Pictorial Empathy Test for Assessing Affective Empathic Reactions in Patients with Schizophrenia
Abstract
1. Introduction
1.1. Measurement of Affective Empathy in Patients with Schizophrenia
1.2. The Pictorial Empathy Test
1.3. Rationale of This Study
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.2.1. The PET Scale
2.2.2. The Positive and Negative Syndrome (PANSS) Scale
2.2.3. The Global Assessment of Functioning (GAF) Scale
2.2.4. The Toronto Alexithymia Scale (TAS-20)
2.3. Analytic Strategy
3. Results
3.1. Participants
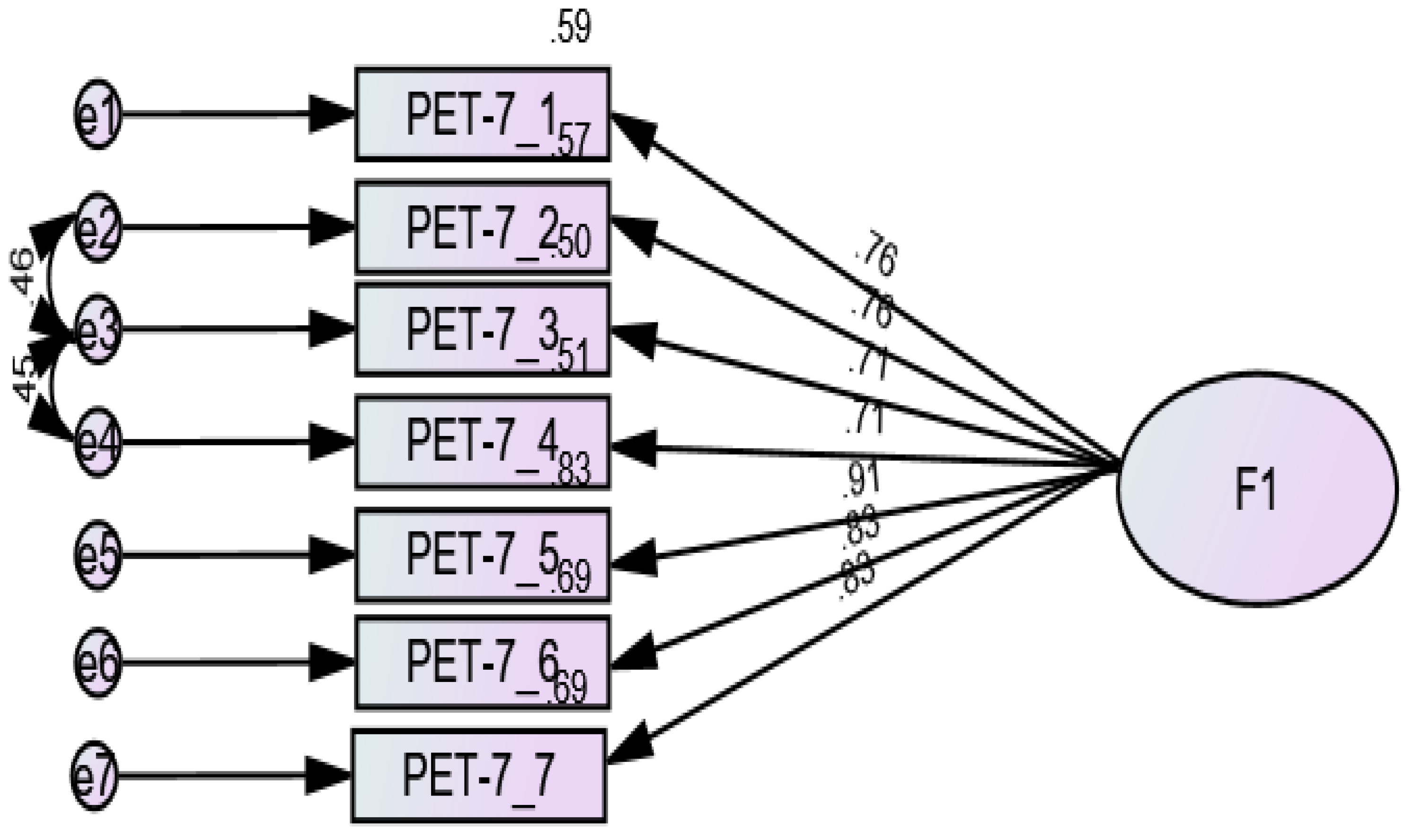
3.2. Confirmatory Factor Analysis
3.3. Sex Invariance
3.4. Bivariate Analysis
3.5. Multivariable Analysis
4. Discussion
4.1. Factor Structure and Internal Consistency of the PET
4.2. Measurement Invariance Across Sex
4.3. Concurrent Validity
4.4. Study Limitations
4.5. Study’s Relevance and Practical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| PET | Pictorial Empathy Test |
| IRI | Interpersonal Reactivity Index |
| QCAE | Questionnaire of Cognitive and Affective Empathy |
| TLI | Tucker-Lewis Index |
| SRMR | Standardized root mean square residual |
| RMSEA | Root mean square error of approximation |
| CFI | comparative fit index |
| PANSS | Positive and Negative Syndrome Scale |
| GAF | Global Assessment of Functioning scale |
| TAS-20 | Toronto Alexithymia Scale |
References
- Eisenberg, N.; Shea, C.L.; Carlo, G.; Knight, G.P. Empathy-related responding and cognition: A “chicken and the egg” dilemma. In Handbook of Moral Behavior and Development; Psychology Press: London, UK, 1991; Available online: https://www.taylorfrancis.com/chapters/edit/10.4324/9781315807287-3/empathy-related-responding-cognition-chicken-egg-dilemma-nancy-eisenberg-cindy-shea-gustavo-carlo-george-knight (accessed on 17 January 2025).
- Davis, M. Measuring individual differences in empathy: Evidence for a multidimensional approach. J. Personal. Soc. Psychol. 1983, 44, 113–126. [Google Scholar] [CrossRef]
- Jolliffe, D.; Farrington, D.P. Development and validation of the basic empathy scale. J. Adolesc. 2006, 29, 589–611. [Google Scholar] [CrossRef]
- de Sousa, A.; McDonald, S.; Rushby, J.; Li, S.; Dimoska, A.; James, C. Understanding deficits in empathy after traumatic brain injury: The role of affective responsivity. Cortex A J. Devoted Study Nerv. Syst. Behav. 2011, 47, 526–535. [Google Scholar] [CrossRef]
- Ali, F.; Amorim, I.S.; Chamorro-Premuzic, T. Empathy deficits and trait emotional intelligence in psychopathy and machiavellianism. Personal. Individ. Differ. 2009, 47, 758–762. [Google Scholar] [CrossRef]
- Bonfils, K.A.; Lysaker, P.H.; Minor, K.S.; Salyers, M.P. Affective empathy in schizophrenia: A meta-analysis. Schizophr. Res. 2016, 175, 109–117. [Google Scholar] [CrossRef]
- Meyer, N.; MacCabe, J.H. Schizophrenia. Medicine 2016, 44, 649–653. [Google Scholar] [CrossRef]
- Janoutová, J.; Janácková, P.; Serý, O.; Zeman, T.; Ambroz, P.; Kovalová, M.; Varechová, K.; Hosák, L.; Jirík, V.; Janout, V. Epidemiology and risk factors of schizophrenia. Neuro Endocrinol. Lett. 2016, 37, 1–8. [Google Scholar]
- Kaplan, R.M. Being bleuler: The second century of schizophrenia. Australas Psychiatry 2008, 16, 305–311. [Google Scholar] [CrossRef] [PubMed]
- Patel, K.R.; Cherian, J.; Gohil, K.; Atkinson, D. Schizophrenia: Overview and treatment options. P T. 2014, 39, 638–645. [Google Scholar] [PubMed]
- Rosaria, D.L.; Giulia, V.; Giulia, S.; Paola, F. Emotional intelligence, empathy and alexithymia: A cross-sectional survey on emotional competence in a group of nursing students. Acta Biomed. 2019, 90 (Suppl. 4), 32–43. [Google Scholar] [CrossRef]
- Clark, K.B. Empathy: A neglected topic in psychological research. Am. Psychol. 1980, 35, 187–190. [Google Scholar] [CrossRef]
- Hobeika, E.; Hallit, S.; Sacre, H.; Obeid, S.; Hajj, A.; Salameh, P. Factors associated with empathy among community pharmacists in lebanon. J. Pharm. Policy Pract. 2020, 13, 32. [Google Scholar] [CrossRef] [PubMed]
- Zurek, P.P.; Scheithauer, H. Towards a more precise conceptualization of empathy: An integrative review of literature on definitions, associated functions, and developmental trajectories. Int. J. Dev. Sci. 2017, 11, 57–68. [Google Scholar] [CrossRef]
- Cohen, A.S.; Minor, K.S. Emotional experience in patients with schizophrenia revisited: Meta-analysis of laboratory studies. Schizophr. Bull. 2010, 36, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Achim, A.M.; Ouellet, R.; Roy, M.; Jackson, P.L. Assessment of empathy in first-episode psychosis and meta-analytic comparison with previous studies in schizophrenia. Psychiatry Res. 2011, 190, 3–8. [Google Scholar] [CrossRef]
- Abramowitz, A.C.; Ginger, E.J.; Gollan, J.K.; Smith, M.J. Empathy, depressive symptoms, and social functioning among individuals with schizophrenia. Psychiatry Res. 2014, 216, 325–332. [Google Scholar] [CrossRef]
- Benedetti, F.; Bernasconi, A.; Bosia, M.; Cavallaro, R.; Dallaspezia, S.; Falini, A.; Poletti, S.; Radaelli, D.; Riccaboni, R.; Scotti, G.; et al. Functional and structural brain correlates of theory of mind and empathy deficits in schizophrenia. Schizophr. Res. 2009, 114, 154–160. [Google Scholar] [CrossRef]
- Lehmann, A.; Bahçesular, K.; Brockmann, E.; Biederbick, S.-E.; Dziobek, I.; Gallinat, J.; Montag, C. Subjective experience of emotions and emotional empathy in paranoid schizophrenia. Psychiatry Res. 2014, 220, 825–833. [Google Scholar] [CrossRef]
- Huo, L.; Qu, D.; Pei, C.; Wu, W.; Ning, Y.; Zhou, Y.; Zhang, X.Y. Alexithymia in chronic schizophrenia and its mediating effect between cognitive deficits and negative symptoms. Schizophr. Res. 2023, 261, 275–280. [Google Scholar] [CrossRef]
- van ‘t Wout, M.; Aleman, A.; Bermond, B.; Kahn, R.S. No words for feelings: Alexithymia in schizophrenia patients and first-degree relatives. Compr. Psychiatry. 2007, 48, 27–33. [Google Scholar] [CrossRef]
- Sifneos, P.E. The prevalence of ‘alexithymic’ characteristics in psychosomatic patients. Psychother. Psychosom. 1973, 22, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Gawęda, Ł.; Krężołek, M. Cognitive mechanisms of alexithymia in schizophrenia: Investigating the role of basic neurocognitive functioning and cognitive biases. Psychiatry Res. 2019, 271, 573–580. [Google Scholar] [CrossRef] [PubMed]
- Salovey, P.; Mayer, J.D. Emotional intelligence. Imagin. Cogn. Personal. 1989, 9, 185–211. [Google Scholar] [CrossRef]
- Green, M.F. What are the functional consequences of neurocognitive deficits in schizophrenia? Am. J. Psychiatry 1996, 153, 321–330. [Google Scholar] [CrossRef]
- Smith, M.J.; Horan, W.P.; Cobia, D.J.; Karpouzian, T.M.; Fox, J.M.; Reilly, J.L.; Breiter, H.C. Performance-based empathy mediates the influence of working memory on social competence in schizophrenia. Schizophr. Bull. 2014, 40, 824–834. [Google Scholar] [CrossRef]
- Fulford, D.; Holt, D.J. Social withdrawal, loneliness, and health in schizophrenia: Psychological and neural mechanisms. Schizophr. Bull. 2023, 49, 1138–1149. [Google Scholar] [CrossRef]
- Sze, J.A.; Gyurak, A.; Goodkind, M.S.; Levenson, R.W. Greater emotional empathy and prosocial behavior in late life. Emotion 2012, 12, 1129–1140. [Google Scholar] [CrossRef]
- Guadagni, V.; Burles, F.; Valera, S.; Hardwicke-Brown, E.; Ferrara, M.; Campbell, T.; Iaria, G. The relationship between quality of sleep and emotional empathy. J. Psychophysiol. 2017, 31, 158–166. [Google Scholar] [CrossRef]
- Utomo, K.D.M. Investigations of cyber bullying and traditional bullying in adolescents on the roles of cognitive empathy, affective empathy, and age. Int. J. Instr. 2022, 15, 937–950. [Google Scholar] [CrossRef]
- Winters, D.E.; Wu, W.; Fukui, S. Longitudinal effects of cognitive and affective empathy on adolescent substance use. Subst Use Misuse 2020, 55, 983–989. [Google Scholar] [CrossRef]
- Tasios, K.; Douzenis, A.; Gournellis, R.; Michopoulos, I. Empathy and violence in schizophrenia and antisocial personality disorder. Healthcare 2024, 12, 89. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.S.; Mateen, M.A.; Brozovich, F.A.; Zaki, J.; Goldin, P.R.; Heimberg, R.G.; Gross, J.J. Empathy for positive and negative emotions in social anxiety disorder. Behav. Res. Ther. 2016, 87, 232–242. [Google Scholar] [CrossRef] [PubMed]
- Latkin, C.A.; Edwards, C.; Davey-Rothwell, M.A.; Tobin, K.E. The relationship between social desirability bias and self-reports of health, substance use, and social network factors among urban substance users in baltimore, maryland. Addict. Behav. 2017, 73, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Baron-Cohen, S.; O’Riordan, M.; Stone, V.; Jones, R.; Plaisted, K. Recognition of faux pas by normally developing children and children with asperger syndrome or high-functioning autism. J. Autism Dev. Disord. 1999, 29, 407–418. [Google Scholar] [CrossRef]
- Baron-Cohen, S.; Wheelwright, S.; Hill, J.; Raste, Y.; Plumb, I. The “reading the mind in the eyes” test revised version: A study with normal adults, and adults with asperger syndrome or high-functioning autism. J. Child Psychol. Psychiatry 2001, 42, 241–251. [Google Scholar] [CrossRef]
- Kuypers, K.P.C. Emotional empathic responses to dynamic negative affective stimuli is gender-dependent. Front. Psychol. 2017, 8, 1491. [Google Scholar] [CrossRef]
- van Donkersgoed, R.J.M.; de Jong, S.; aan het Rot, M.; Wunderink, L.; Lysaker, P.H.; Hasson-Ohayon, I.; Aleman, A.; Pijnenborg, G.H.M. Measuring empathy in schizophrenia: The empathic accuracy task and its correlation with other empathy measures. Schizophr. Res. 2019, 208, 153–159. [Google Scholar] [CrossRef]
- Zaki, J.; Bolger, N.; Ochsner, K. It takes two: The interpersonal nature of empathic accuracy. Psychol. Sci. 2008, 19, 399–404. [Google Scholar] [CrossRef]
- Wever, M.C.M.; van Houtum, L.A.E.M.; Janssen, L.H.C.; Spruit, I.M.; Tollenaar, M.S.; Rot, M.A.H.; Elzinga, B.M. Eyes on you: Ensuring empathic accuracy or signalling empathy? Int. J. Psychol. 2022, 57, 743–752. [Google Scholar] [CrossRef]
- Di Girolamo, M.; Giromini, L.; Winters, C.L.; Serie, C.M.B.; de Ruiter, C. The questionnaire of cognitive and affective empathy: A comparison between paper-and-pencil versus online formats in italian samples. J. Pers. Assess 2019, 101, 159–170. [Google Scholar] [CrossRef]
- McKenzie, K.; Russell, A.; Golm, D.; Fairchild, G. Empathic accuracy and cognitive and affective empathy in young adults with and without autism spectrum disorder. J. Autism Dev. Disord. 2022, 52, 2004–2018. [Google Scholar] [CrossRef]
- Davis, M.H. The effects of dispositional empathy on emotional reactions and helping: A multidimensional approach. J. Personal. 1983, 51, 167–184. [Google Scholar] [CrossRef]
- Horan, W.P.; Reise, S.P.; Kern, R.S.; Lee, J.; Penn, D.L.; Green, M.F. Structure and correlates of self-reported empathy in schizophrenia. J. Psychiatr. Res. 2015, 66–67, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Reniers, R.L.E.P.; Corcoran, R.; Drake, R.; Shryane, N.M.; Völlm, B.A. The QCAE: A questionnaire of cognitive and affective empathy. J. Pers. Assess 2011, 93, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Lindeman, M.; Koirikivi, I.; Lipsanen, J. Pictorial empathy test (PET): An easy-to-use method for assessing affective empathic reactions. Eur. J. Psychol. Assess. 2018, 34, 421–431. [Google Scholar] [CrossRef]
- Baliyan, S.; Cimadevilla, J.M.; Bustillos, A.; Escamilla, J.C.; Leiman, M.; Sandi, C.; Venero, C. Cultural adaptation, validation, and psychometric description of the pictorial empathy test (PET) in the spanish population. Eur. J. Psychol. Assess. 2023, 39, 141–152. [Google Scholar] [CrossRef]
- Monzel, M.; Keidel, K.; Reuter, M. Is it really empathy? the potentially confounding role of mental imagery in self-reports of empathy. J. Res. Personal. 2023, 103, 104354. [Google Scholar] [CrossRef]
- Fekih-Romdhane, F.; Amouchi, G.; Ali, A.M.; Cheour, M.; Hallit, S. Psychometric validation of an arabic-language version of the pictorial empathy test (PET) and the single-item empathy scale (SITES) for adults. Res. Sq. 2024. [Google Scholar] [CrossRef]
- Sandor, S. Mediator effects of cognitive and affective empathy on the relationship between schizotypal symptoms and social anxiety/avoidance levels. Neuropsychiatr. Invest. 2022, 60, 52–63. [Google Scholar] [CrossRef]
- Chuang, S.P.; Wu, J.Y.W.; Wang, C.S. Metacognitive beliefs, cognitive functioning, psychiatric symptoms and empathy in people with schizophrenia. Neuropsychiatr. Dis. Treat. 2021, 17, 2209–2217. [Google Scholar] [CrossRef]
- Jeong, D.; Aggarwal, S.; Robinson, J.; Kumar, N.; Spearot, A.; Park, D.S. Exhaustive or exhausting? evidence on respondent fatigue in long surveys. J. Dev. Econ. 2023, 161, 102992. [Google Scholar] [CrossRef]
- Gudykunst, W.B.; Ting-Toomey, S. Culture and affective communication. Am. Behav. Sci. 1988, 31, 384–400. [Google Scholar] [CrossRef]
- Al-Amrani, S.N. The impact of arab collectivist culture on willingness to communicate in A second language: A critical review. SSRN Electron. J. 2021. [CrossRef]
- Safiri, S.; Noori, M.; Nejadghaderi, S.A.; Shamekh, A.; Sullman, M.J.M.; Collins, G.S. The burden of schizophrenia in the middle east and north africa region, 1990–2019. Sci Rep. 2024, 14, 9720. [Google Scholar] [CrossRef] [PubMed]
- Balkhi, B.; Alshayban, D.; Alotaibi, N.M. Impact of healthcare expenditures on healthcare outcomes in the middle east and north africa (MENA) region: A cross-country comparison, 1995–2015. Front. Public Health 2021, 8, 624962. [Google Scholar] [CrossRef]
- Kassir, G.; Hayek, S.E.; Charara, R.; Cherro, M.; Itani, H.; Khoury, J.E. Predictors of admission to an assertive outreach service for psychosis in lebanon. PLoS Glob. Public Health 2022, 2, e0001428. [Google Scholar] [CrossRef]
- Meyer, L.; Lakatos, P.; He, Y. Language dysfunction in schizophrenia: Assessing neural tracking to characterize the underlying disorder(s)? Front. Neurosci. 2021, 15, 640502. [Google Scholar] [CrossRef]
- Haddad, C.; Abboche, E.; Hallit, S.; Haddad, G.; Hachem, D.; Zoghbi, M. Factors associated with length of stay in hospitalized psychiatric patients: A monocentric retrospective study in lebanon. Discov. Public Health 2024, 21, 63. [Google Scholar] [CrossRef]
- Association, A.P. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publishing: Washington, WA, USA, 2013; Available online: https://books.google.com.lb/books/about/Diagnostic_and_Statistical_Manual_of_Men.html?id=-JivBAAAQBAJ&redir_esc=y (accessed on 16 January 2025).
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef]
- Hallit, S.; Obeid, S.; Haddad, C.; Kazour, F.; Kazour, G. Validation of the arabic version of the PANSS scale among lebanese schizophrenic patients. J. Psychopathol. 2017, 23, 60–66. [Google Scholar]
- Jones, S.H.; Thornicroft, G.; Coffey, M.; Dunn, G. A brief mental health outcome scale-reliability and validity of the global assessment of functioning (GAF). Br. J. Psychiatry 1995, 166, 654–659. [Google Scholar] [CrossRef]
- Bagby, R.M.; Parker, J.D.; Taylor, G.J. The twenty-item toronto alexithymia scale--I. item selection and cross-validation of the factor structure. J. Psychosom Res. 1994, 38, 23–32. [Google Scholar] [CrossRef] [PubMed]
- El Frenn, Y.; Akel, M.; Hallit, S.; Obeid, S. Couple’s Satisfaction among Lebanese adults: Validation of the Toronto Alexithymia Scale and Couple Satisfaction Index-4 scales, association with attachment styles and mediating role of alexithymia. BMC Psychol. 2022, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Mundfrom, D.J.; Shaw, D.G.; Ke, T.L. Minimum sample size recommendations for conducting factor analyses. Int. J. Test. 2005, 5, 159–168. [Google Scholar] [CrossRef]
- Hu, L.; Bentler, P.M. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Chen, F.F. Sensitivity of goodness of fit indexes to lack of measurement invariance. Struct. Equ. Model. A Multidiscip. J. 2007, 14, 464–504. [Google Scholar] [CrossRef]
- Vandenberg, R.J.; Lance, C.E. A review and synthesis of the measurement invariance literature: Suggestions, practices, and recommendations for organizational research. Organ. Res. Methods 2000, 3, 4–70. [Google Scholar] [CrossRef]
- Swami, V.; Todd, J.; Azzi, V.; Malaeb, D.; El Dine, A.S.; Obeid, S.; Halli, S. Psychometric properties of an arabic translation of the functionality appreciation scale (FAS) in lebanese adults. Body Image. 2022, 42, 361–369. [Google Scholar] [CrossRef]
- Joseph, F.H., Jr.; Sarstedt, M.; Ringle, C.M.; Gudergan, S.P. Advanced Issues in Partial Least Squares Structural Equation Modeling; SAGE Publications: Thousand Oaks, CA, USA, 2017; Available online: https://books.google.com.lb/books/about/Advanced_Issues_in_Partial_Least_Squares.html?hl=id&id=-f1rDgAAQBAJ&redir_esc=y (accessed on 16 January 2025).
- Hosmer, D.W., Jr.; Lemeshow, S.; Sturdivant, R.X. Applied Logistic Regression; John Wiley & Sons: Hoboken, NJ, USA, 2013; Available online: https://books.google.com.lb/books/about/Applied_Logistic_Regression.html?id=64JYAwAAQBAJ&redir_esc=y (accessed on 12 January 2025).
- Brown, T.A. Confirmatory Factor Analysis for Applied Research, 2nd ed.; The Guilford Press: New York, NY, USA, 2015; Available online: https://psycnet.apa.org/record/2015-10560-000 (accessed on 12 January 2025).
- Taber, K.S. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res. Sci. Educ. 2018, 48, 1273–1296. [Google Scholar] [CrossRef]
- Kenny, D.A.; McCoach, D.B. Effect of the number of variables on measures of fit in structural equation modeling. Struct. Equ. Model. A Multidiscip. J. 2003, 10, 333–351. [Google Scholar] [CrossRef]
- Kenny, D.A.; Kaniskan, B.; McCoach, D.B. The performance of RMSEA in models with small degrees of freedom. Sociol. Methods Res. 2015, 44, 486–507. [Google Scholar] [CrossRef]
- Lai, K.; Green, S.B. The problem with having two watches: Assessment of fit when RMSEA and CFI disagree. Multivar. Behav. Res. 2016, 51, 220–239. [Google Scholar] [CrossRef]
- Ahad, A.A.; Sanchez-Gonzalez, M.; Junquera, P. Understanding and addressing mental health stigma across cultures for improving psychiatric care: A narrative review. Cureus 2023, 15, e39549. [Google Scholar] [CrossRef]
- Shanbour-Srour, K.; Goldberg, T.; Kurman, J. Exploring the relationship between cultural orientations and empathy among arab-palestinian teachers in israel: A mixed-method study. J. Cross-Cult. Psychol. 2025, 56, 450–469. [Google Scholar] [CrossRef]
- El Halabi, S.; Founouni, Z.N.; Arawi, T. Social construction of arab masculinity and its effects on mental health. In Handbook of Healthcare in the Arab World, Laher I, ed.; Springer International Publishing: Cham, Switzerland, 2019; pp. 1–11. [Google Scholar] [CrossRef]
- Beadle, J.N.; de la Vega, C.E. Impact of aging on empathy: Review of psychological and neural mechanisms. Front. Psychiatry 2019, 10, 331. [Google Scholar] [CrossRef]
- Yang, H.; Shi, H.; Ni, K.; Wang, Y.; Cheung, E.F.C.; Chan, R.C.K. Exploring the links between alexithymia, empathy and schizotypy in college students using network analysis. Cogn. Neuropsychiatry 2020, 25, 245–253. [Google Scholar] [CrossRef] [PubMed]
- Castellini, G.; Merola, G.P.; Baccaredda Boy, O.; Vincenzoa, P.; Bernardoa, B.; Emanuelea, C.; Eleonoraa, R.; Valentinab, B.; Sandrob, S.; Benedetta, N.; et al. Emotional dysregulation, alexithymia and neuroticism: A systematic review on the genetic basis of a subset of psychological traits. Psychiatr. Genet. 2023, 33, 79–101. [Google Scholar] [CrossRef] [PubMed]
- Frattaroli, N.; Geljic, M.; Runkowska, D.; Darke, H.; Reddyhough, C.; Mills, T.; Mitchell, M.; Hill, R.; Carter, O.; Sundram, S. Cognitive and perceptual impairments in schizophrenia extend to other psychotic disorders but not schizotypy. Schizophr. Res. Cogn. 2022, 30, 100266. [Google Scholar] [CrossRef] [PubMed]
- McQuarrie, A.M.; Smith, S.D.; Jakobson, L.S. Alexithymia and sensory processing sensitivity account for unique variance in the prediction of emotional contagion and empathy. Front. Psychol. 2023, 14, 1072783. [Google Scholar] [CrossRef]
- Moriguchi, Y.; Decety, J.; Ohnishi, T.; Maeda, M.; Mori, T.; Nemoto, K.; Matsuda, H.; Komakiet, G. Empathy and judging other’s pain: An fMRI study of alexithymia. Cereb. Cortex 2007, 17, 2223–2234. [Google Scholar] [CrossRef]
- Aslan, G.; Bakan, A.B.; Yildiz, M. An investigation of the relationship between alexithymia and empathy tendency in university students receiving health education. Perspect. Psychiatr. Care 2021, 57, 709–716. [Google Scholar] [CrossRef]
- Wang, W.; Zhou, Y.; Liu, R.; Wei, S.; Xu, H.; Wang, J.; Wang, L.; Trinh, T.H.; Wu, H.E.; Wang, D.; et al. Association between empathy and clinical symptoms in chronic schizophrenia: A large sample study based on chinese han population. J. Psychiatr. Res. 2021, 139, 106–112. [Google Scholar] [CrossRef]
- Taha, S.M.; Abdelraof, A.I.; El-Monshed, A.H.; Amr, M.; Elhay, E.S.A. Insight and empathy in schizophrenia: Impact on quality of life and symptom severity. Arch Psychiatr. Nurs. 2024, 52, 60–68. [Google Scholar] [CrossRef]
- Lincoln, T.M.; Mehl, S.; Kesting, M.; Rief, W. Negative symptoms and social cognition: Identifying targets for psychological interventions. Schizophr. Bull. 2011, 37 (Suppl. 2), 23. [Google Scholar] [CrossRef]
- Fakhoury, W.K.; Wright, D.; Wallace, M. Prevalence and extent of distress of adverse effects of antipsychotics among callers to a united kingdom national mental health helpline. Int. Clin. Psychopharmacol. 2001, 16, 153–162. [Google Scholar] [CrossRef]
- Meng, Q.; Li, R.; Hou, F.; Zhang, Q. Effects of chlorpromazine on sleep quality, clinical and emotional measures among patients with schizophrenia. Clin. Neurol. Neurosurg. 2018, 165, 134–138. [Google Scholar] [CrossRef]
- Read, J.; Williams, J. Positive and negative effects of antipsychotic medication: An international online survey of 832 recipients. Curr. Drug Saf. 2019, 14, 173–181. [Google Scholar] [CrossRef] [PubMed]
| Variables | N (%) |
|---|---|
| Sex | |
| Males | 72 (63.7%) |
| Females | 41 (36.3%) |
| Level of Education | |
| Elementary | 27 (23.9%) |
| Complementary | 42 (37.2%) |
| High school | 30 (26.5%) |
| University education | 14 (12.4%) |
| Mean ± SD | |
| Age (years) | 57.52 ± 10.35 [min = 33; max = 76] |
| Age of schizophrenia onset | 25.33 ± 7.71 [min = 13; max = 48] |
| Length of hospitalization (years) | 3.69 ± 4.82 [min = 0.01; max = 32] |
| Length of illness (years) | 32.04 ± 11.59 [min = 6; max = 61] |
| Affective empathy | 19.98 ± 7.70 [min = 7; max = 34] |
| PANSS | 90.27 ± 28.08 [min = 30; max = 156] |
| GAF | 71.59 ± 25.40 [min = 20; max = 100] |
| Alexithymia | 53.58 ± 13.82 [min = 30; max = 90] |
| Model | CFI | RMSEA | SRMR | Model Comparison | ΔCFI | ΔRMSEA | ΔSRMR |
|---|---|---|---|---|---|---|---|
| Configural | 0.966 | 0.082 | 0.044 | ||||
| Metric | 0.967 | 0.073 | 0.043 | Configural vs. metric | 0.001 | 0.009 | 0.001 |
| Scalar | 0.977 | 0.056 | 0.046 | Metric vs. scalar | 0.010 | 0.017 | 0.003 |
| Mean ± SD | F | df1, df2 | p | Effect Size | |
|---|---|---|---|---|---|
| Level of Education | 0.13 | 3, 109 | 0.944 | 0.003 | |
| Elementary | 21.33 ± 9.16 | ||||
| Complementary | 22.07 ± 8.03 | ||||
| Secondary school | 22.60 ± 7.01 | ||||
| University education | 21.93 ± 5.27 |
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |
|---|---|---|---|---|---|---|---|
| 1. Affective empathy | 1 | ||||||
| 2. Age | 0.09 | 1 | |||||
| 3. Age of schizophrenia onset | −0.17 | 0.17 | 1 | ||||
| 4. Duration of Hospital Stay | 0.06 | 0.07 | −0.17 | 1 | |||
| 5. Duration of the disease | 0.17 | 0.73 *** | −0.46 *** | 0.04 | 1 | ||
| 6. PANSS | 0.10 | 0.05 | 0.05 | 0.04 | −0.004 | 1 | |
| 7. GAF | −0.12 | −0.13 | −0.03 | 0.05 | −0.08 | −0.68 *** | 1 |
| 8. Alexithymia | −0.46 *** | −0.01 | 0.08 | −0.14 | −0.04 | 0.09 | −0.03 |
| Unstandardized Beta | Standardized Beta | p | 95% CI | |
|---|---|---|---|---|
| Sex (females vs. males *) | −3.41 | −0.21 | 0.026 | −6.40; −0.42 |
| Age of schizophrenia onset | −0.07 | −0.07 | 0.471 | −0.25; 0.12 |
| Length of illness | 0.04 | 0.06 | 0.553 | 0.09; 0.16 |
| General functioning | −0.05 | −0.17 | 0.051 | −0.10; 0.001 |
| Alexithymia | −0.21 | −0.37 | <0.001 | −0.30; −0.11 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kerbage, G.; Akkari, C.; Hachem, N.; El Murr, M.; El Mir, R.; Abou Atme, C.; Haddad, G.; Abou Khalil, R.; El Hayek, E.; Harb, F.; et al. Psychometric Properties of the Arabic Version of the Pictorial Empathy Test for Assessing Affective Empathic Reactions in Patients with Schizophrenia. Healthcare 2025, 13, 2022. https://doi.org/10.3390/healthcare13162022
Kerbage G, Akkari C, Hachem N, El Murr M, El Mir R, Abou Atme C, Haddad G, Abou Khalil R, El Hayek E, Harb F, et al. Psychometric Properties of the Arabic Version of the Pictorial Empathy Test for Assessing Affective Empathic Reactions in Patients with Schizophrenia. Healthcare. 2025; 13(16):2022. https://doi.org/10.3390/healthcare13162022
Chicago/Turabian StyleKerbage, Georges, Camille Akkari, Nagham Hachem, Michelle El Murr, Rita El Mir, Cyril Abou Atme, Georges Haddad, Rony Abou Khalil, Elissar El Hayek, Frederic Harb, and et al. 2025. "Psychometric Properties of the Arabic Version of the Pictorial Empathy Test for Assessing Affective Empathic Reactions in Patients with Schizophrenia" Healthcare 13, no. 16: 2022. https://doi.org/10.3390/healthcare13162022
APA StyleKerbage, G., Akkari, C., Hachem, N., El Murr, M., El Mir, R., Abou Atme, C., Haddad, G., Abou Khalil, R., El Hayek, E., Harb, F., Hallit, S., & Fekih-Romdhane, F. (2025). Psychometric Properties of the Arabic Version of the Pictorial Empathy Test for Assessing Affective Empathic Reactions in Patients with Schizophrenia. Healthcare, 13(16), 2022. https://doi.org/10.3390/healthcare13162022







