Spanish Translation and Cultural Adaptation of the Wolf Motor Function Test for Survivors of Acquired Brain Injury
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Wolf Motor Function Test (WMFT)
2.4. Administration Procedure
- Test set-up: Adequate space was arranged in the test room to ensure the participant’s comfort, as well as proper chair and recording positions. It was essential that we ensure that the tested movement was clearly visible. As specified in the original version of the test, the administration was performed first with the less-affected UL and then with the most-affected UL.
- Instructions: General instructions were provided prior to the test administration. Each item was described and demonstrated twice: the first demonstration was performed slowly to familiarise the participant with the task, while the second demonstration was faster to show the required speed. Participants were not allowed to practice the tasks before the test commenced.
- Execution: The test was administered in a quiet environment to minimise distractions. Participants were encouraged to complete each task as quickly as possible and to achieve the highest weight as possible in the strength tasks. A second trial of the task was only allowed if the participant performed the task incorrectly, if there was a distraction or interruption, if the assessor made an error in preparation or timing, or if an object was dropped on the floor for more than 5 s. A second trial was not permitted if the assessor believed the participant could perform the task better or faster.
- Scoring: The time taken to complete each task was recorded using a stopwatch. The FA score was determined by an expert panel after viewing the recorded sessions, as specified in the instructions. The panel followed the Functional Ability Scale (FAS) and the scoring guidelines for each task.
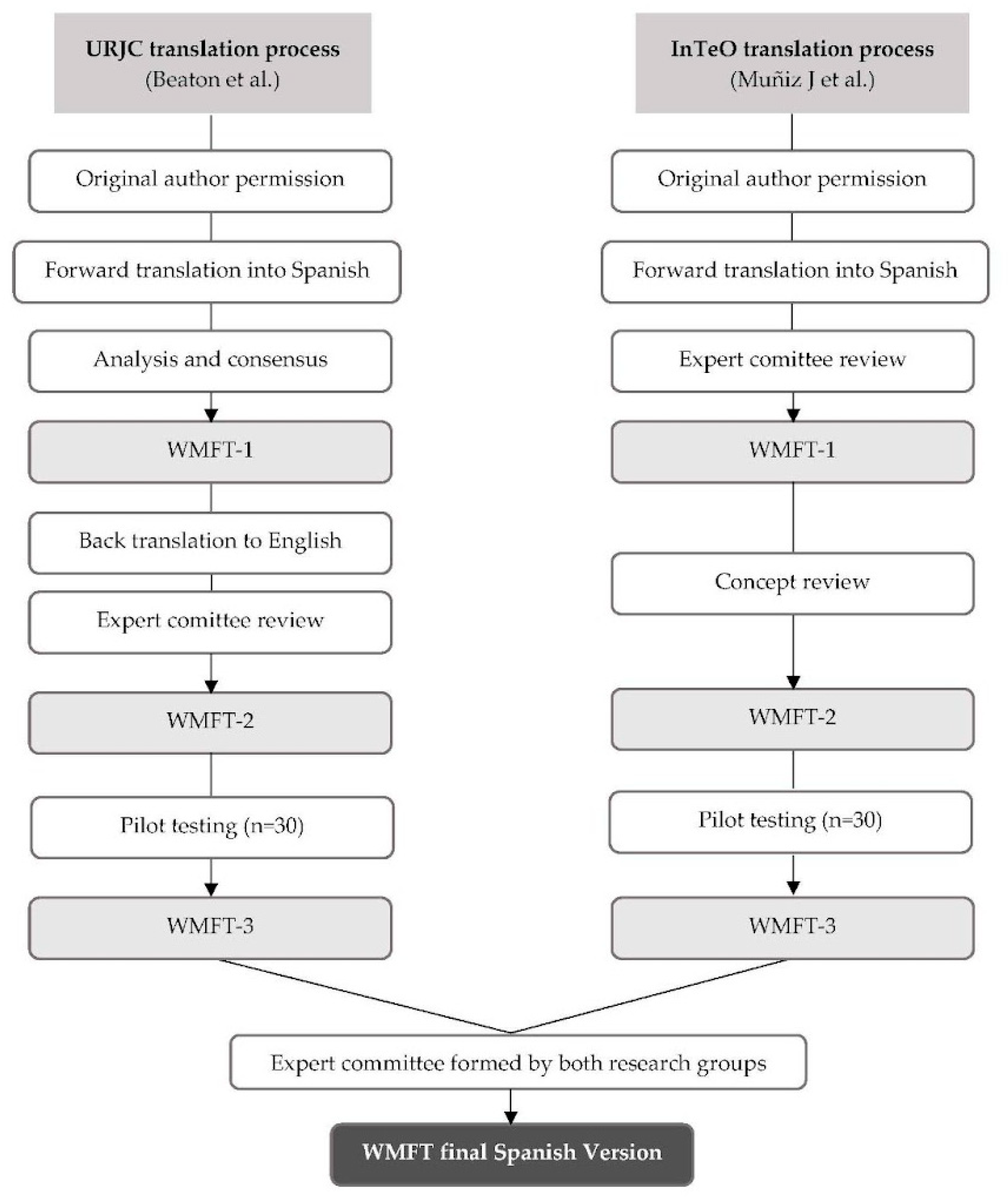
2.5. Process of Translation and Cultural Adaptation of the WMFT into Spanish
- Translation into Spanish: The test was translated by two native Spanish-speaking translators, resulting in translations T1 and T2.
- Analysis and consensus: Both translations were reviewed and analysed to reach a consensus on a single version (T1-2).
- Back translation to English: Native English-speaking translators, unaware of the original translation, independently translated T1-2 back into English (RT1 and RT2).
- Expert committee review: The committee, composed of four occupational therapists, two translators, and two researchers familiar with the tool, reviewed all the versions (T1, T2, T1-2, RT1, and RT2). After a thorough analysis, a prefinal Spanish version was selected.
- Pilot testing: The prefinal version was tested with a sample of 30 participants, who were interviewed about any difficulties in understanding the meaning of the questions and the responses. Incidents of incomplete or repeated responses were also noted (i.e., when all patients provide the same response to a specific question).
- Final revision: Errors and typographical mistakes were corrected, leading to the final version of the test, which was sent to the authors of the original version.
- Translation into Spanish: Two native Spanish-speaking translators independently translated the test, resulting in translations T1 and T2.
- First expert committee review: A committee of four occupational therapists with expertise in neurology and two methodologists met six times to review and unify the two translations. They made semantic and idiomatic adjustments to create the first Spanish version (WMFT-E-1).
- Concept review: Three neurorehabilitation experts conducted a content analysis and administered the test to identify any comprehension issues across the test’s instructions, resulting in the second version of the tool (WMFT-E-2).
- Pilot study: WMFT-E-2 was tested with a sample of participants with ABI. Participants were interviewed about any difficulties they encountered with the translated WMFT version. Evaluators also noted any questions that caused difficulty during the assessment, and the FA expert panel proposed changes to refine the administration and scoring instructions.
- Final version: Changes based on the pilot study feedback were incorporated, resulting in the final version of the test, which was translated and culturally adapted into Spanish (WMFT-E-3).
2.6. Pilot Testing of the Spanish Version of the WMFT
2.7. Ethical Considerations
2.8. Statistical Analysis
3. Results
3.1. Consensus-Based Revisions in the Cross-Cultural Adaptation of the WMFT
3.2. Sample Description
3.3. Pilot Testing Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| WMFT | Wolf Motor Function Test |
| ABI | Acquired Brain Injury |
| TBI | Traumatic Brain Injury |
| UL | Upper Limb |
| FA | Functional Ability |
| CAULIN | European evidence-based recommendations for clinical assessment of upper limb in neurorehabilitation |
| ICF | International Classification of Function |
| URJC | Rey Juan Carlos University |
| InTeO | Investigación en Terapia Ocupacional (Research in Occupational Therapy group) |
References
- Goldman, L.; Siddiqui, E.M.; Khan, A.; Jahan, S.; Rehman, M.U.; Mehan, S.; Sharma, R.; Budkin, S.; Kumar, S.N.; Sahu, A.; et al. Understanding Acquired Brain Injury: A review. Biomedicines 2022, 10, 2167. [Google Scholar] [CrossRef]
- Jolliffe, L.; Lannin, N.A.; Cadilhac, D.A.; Hoffmann, T. Systematic review of clinical practice guidelines to identify recommendations for rehabilitation after stroke and other acquired brain injuries. BMJ Open 2018, 8, e018791. [Google Scholar] [CrossRef]
- INE [Internet]. Enfermedades Crónicas Diagnosticadas por Sexo y Edad. Población con Discapacidad. Available online: https://www.ine.es/jaxi/Datos.htm?tpx=66954 (accessed on 10 December 2024).
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021, 20, 795–820. [Google Scholar] [CrossRef]
- Huertas Hoyas, E.; Pedrero Pérez, E.J.; Águila Maturana, A.M.; García López-Alberca, S.; González Alted, C. Functionality predictors in acquired brain damage. Neurologia 2014, 30, 339–346. [Google Scholar] [CrossRef]
- Marshall, S.; Teasell, R.; Bayona, N.; Lippert, C.; Chundamala, J.; Villamere, J.; Mackie, D.; Cullen, N.; Bayley, M. Motor impairment rehabilitation post acquired brain injury. Brain Inj. 2007, 21, 133–160. [Google Scholar] [CrossRef]
- Lawrence, E.S.; Coshall, C.; Dundas, R.; Stewart, J.; Rudd, A.G.; Howard, R.; Wolfe, C.D. Estimates of the prevalence of acute stroke impairments and disability in a multiethnic population. Stroke 2001, 32, 1279–1284. [Google Scholar] [CrossRef]
- Wolf, T.J.; Baum, C.M.; Lee, D.; Hammel, J. The development of the improving participation after stroke self-management program (IPASS): An exploratory randomized clinical study. Top. Stroke Rehabil. 2016, 23, 284–292. [Google Scholar] [CrossRef]
- Alt Murphy, M.; Resteghini, C.; Feys, P.; Lamers, I. An overview of systematic reviews on upper extremity outcome measures after stroke. BMC Neurol. 2015, 15, 29. [Google Scholar] [CrossRef]
- Prieto-Botella, D.; Sánchez-Pérez, A.; Sánchez-Moreno, S.; Hurtado-Pomares, M.; Peral-Gómez, P.; Espinosa-Sempere, C.; Juárez-Leal, I.; Fernández-Pires, P.; Valera-Gran, D.; Navarrete-Muñoz, E.-M. Identification and use of assessment tools in Spanish occupational therapists: An exploratory study. Healthcare 2022, 10, 1902. [Google Scholar] [CrossRef] [PubMed]
- Prange-Lasonder, G.B.; Alt Murphy, M.; Lamers, I.; Hughes, A.-M.; Buurke, J.H.; Feys, P.; Keller, T.; Klamroth-Marganska, V.; Tarkka, I.M.; Timmermans, A.; et al. European evidence-based recommendations for clinical assessment of upper limb in neurorehabilitation (CAULIN): Data synthesis from systematic reviews, clinical practice guidelines and expert consensus. J. Neuroeng. Rehabil. 2021, 18, 162. [Google Scholar] [CrossRef] [PubMed]
- Madroñero-Miguel, B.; Cuesta-García, C. Spanish consensus of occupational therapists on upper limb assessment tools in stroke. Br. J. Occup. Ther. 2023, 86, 648–658. [Google Scholar] [CrossRef]
- Duff, S.V.; He, J.; Nelsen, M.A.; Lane, C.J.; Rowe, V.T.; Wolf, S.L.; Dromerick, A.W.; Winstein, C.J. Interrater reliability of the Wolf Motor Function Test-Functional Ability Scale: Why it matters. Neurorehabil. Neural Repair 2014, 29, 436–443. [Google Scholar] [CrossRef]
- Wolf, S.L.; Catlin, P.A.; Ellis, M.; Archer, A.L.; Morgan, B.; Piacentino, A. Assessing wolf motor function test as outcome measure for research in patients after stroke. Stroke 2001, 32, 1635–1639. [Google Scholar] [CrossRef]
- Bürge, E.; Kupper, D.; Badan Bâ, M.; Leemann, B.; Berchtold, A. Qualities of a French version of the Wolf Motor Function Test: A multicenter study. Ann. Phys. Rehabil. Med. 2013, 56, 288–299. [Google Scholar] [CrossRef]
- Berardi, A.; Dhrami, L.; Tofani, M.; Valente, D.; Sansoni, J.; Galeoto, G. Cross-cultural adaptation and validation in the Italian population of the wolf motor function test in patients with stroke. Funct. Neurol. 2018, 33, 229–253. [Google Scholar]
- Adhikari, S.P.; Tretriluxana, J.; Chaiyawat, P. Reliability and validity of the Nepali Wolf motor function test following cross-cultural adaptation. Kathmandu Univ. Med. J. (KUMJ) 2016, 14, 3–8. [Google Scholar]
- Pereira, N.D.; Michaelsen, S.M.; Menezes, I.S.; Ovando, A.C.; Lima, R.C.M.; Teixeira-Salmela, L.F. Reliability of the Brazilian version of the Wolf Motor Function Test in adults with hemiparesis. Rev. Bras. Fisioter. 2011, 15, 257–265. [Google Scholar] [CrossRef]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Muñiz, J.; Elosua, P.; Hambleton, R.K.; International Test Commission. International Test Commission Guidelines for test translation and adaptation: Second edition. Psicothema 2013, 25, 151–157. [Google Scholar] [CrossRef]
- Hernández, A.; Hidalgo, M.D.; Hambleton, R.K.; Gómez-Benito, J. International Test Commission guidelines for test adaptation: A criterion checklist. Psicothema 2020, 32, 390–398. [Google Scholar] [CrossRef]
- Epstein, J.; Osborne, R.H.; Elsworth, G.R.; Beaton, D.E.; Guillemin, F. Cross-cultural adaptation of the Health Education Impact Questionnaire: Experimental study showed expert committee, not back-translation, added value. J. Clin. Epidemiol. 2013, 68, 360–369. [Google Scholar] [CrossRef]
- Epstein, J.; Santo, R.M.; Guillemin, F. A review of guidelines for cross-cultural adaptation of questionnaires could not bring out a consensus. J. Clin. Epidemiol. 2014, 68, 435–441. [Google Scholar] [CrossRef]
- Cruchinho, P.; López-Franco, M.D.; Capelas, M.L.; Almeida, S.; Bennett, P.M.; Miranda da Silva, M.; Teixeira, G.; Nunes, E.; Lucas, P.; Gaspar, F. Translation, cross-cultural adaptation, and validation of measurement instruments: A practical guideline for novice researchers. J. Multidiscip. Healthc. 2024, 17, 2701–2728. [Google Scholar] [CrossRef]
- Sousa, V.D.; Rojjanasrirat, W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. J. Eval. Clin. Pract. 2010, 17, 268–274. [Google Scholar] [CrossRef]
- Scott, K.; Ummer, O.; LeFevre, A.E. The devil is in the detail: Reflections on the value and application of cognitive interviewing to strengthen quantitative surveys in global health. Health Policy Plan. 2021, 36, 982–995. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, J.; Hayward, K.S.; Kwakkel, G.; Ward, N.S.; Wolf, S.L.; Borschmann, K.; Krakauer, J.W.; Boyd, L.A.; Carmichael, S.T.; Corbett, D.; et al. Agreed definitions and a shared vision for new standards in stroke recovery research: The Stroke Recovery and Rehabilitation Roundtable taskforce. Int. J. Stroke 2017, 12, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Trabassi, D.; Castiglia, S.F.; Bini, F.; Marinozzi, F.; Ajoudani, A.; Lorenzini, M.; Chini, G.; Varrecchia, T.; Ranavolo, A.; De Icco, R.; et al. Optimizing Rare Disease Gait Classification through Data Balancing and Generative AI: Insights from Hereditary Cerebellar Ataxia. Sensors 2024, 24, 3613. [Google Scholar] [CrossRef] [PubMed]


| Instructions | Problem | Solution |
|---|---|---|
| Objects | Objects used were culturally appropriate for the Spanish context, but the units of force were different. | The units of force were changed from pound (lbs.) to kilograms (kg). |
| General information | The original text lacked a structure that facilitated comprehension. | The instructions were reorganised into a logical sequence to enhance understanding. This restructuring clarified the purpose of the test, the administration process, the scoring method, and the recording procedures. |
| Individual tasks instructions | Instructions were complex. | Images were incorporated to enhance the clarity and understanding of the instructions. |
| Instructions | Problem | Solution |
|---|---|---|
| Language | The language used was not inclusive. The terms “paciente” (patient) and “evaluador” (evaluator) were used, and the terms “extremidad superior no afectada” (unaffected upper extremity) and “extremidad superior afectada” (affected upper extremity) were used to describe the limbs. | “Patient” and “evaluator” were replaced with “persona evaluada” (participant) and “persona evaluadora” (assessor) to ensure inclusivity. “Extremidad superior no afectada” (unaffected upper extremity) and “extremidad superior afectada” (affected upper extremity) were replaced with “extremidad superior menos afectada” (less-affected UL) and “extremidad superior más afectada” (most-affected UL) for greater clarity and sensitivity. |
| Objects | List of objects was presented without accompanying images. | An image was included to illustrate the required objects. |
| General information | The text was excessively lengthy, complex, and repetitive, making it difficult to read. | Repetitive instructions were unified and reorganised to enhance clarity and facilitate comprehension. |
| Some evaluators were not prepared to understand the instructions. | The requirement was added: “To be an evaluator, you should have knowledge about UL biomechanics and anatomy”. | |
| The double instruction (slow and fast) and the demonstration were eliminated. | It was clarified that the instruction and demonstration could be repeated as needed. | |
| Individual tasks instructions | The instructions presented significant challenges in terms of comprehension. | Terminology was unified, and items were organised into a consistent structure, making the administration process faster. |
| The instruction was reiterated twice, first at a slow pace and then at a faster pace. | The repeated instruction was removed to streamline the process. | |
| Filming position | The movement was not clearly visible. | The camera position was modified to ensure better visibility of the movement. |
| Print instructions | The information was lengthy and irrelevant to the context in Spain. | All information, except the template dimensions, was eliminated. |
| URJC Sample | InTeO Sample | Total Sample | |
|---|---|---|---|
| (n = 30) | (n = 30) | (n = 60) | |
| Sex, n (%) | |||
| Women | 9 (30) | 13 (43.3) | 22 (36.7) |
| Men | 21 (70) | 17 (56.7) | 38 (63.3) |
| Age, mean (SD) | 64 (11.9) | 58 (15.9) | 61 (14.2) |
| Education level, n (%) | |||
| ≤Primary education | 13 (43.3) | 13 (43.3) | 26 (43.3) |
| >Primary education | 17 (56.7) | 17 (56.7) | 34 (56.7) |
| Patient with a caregiver, n (%) | |||
| Yes | 2 (6.7) | 8 (26.7) | 10 (16.7) |
| No | 28 (93.3) | 22 (73.3) | 50 (83.3) |
| Most-affected UL, n (%) | |||
| Left | 11 (36.7) | 16 (53.3) | 27 (45.0) |
| Right | 19 (63.3) | 14 (46.7) | 33 (55.0) |
| Type of ABI, n (%) | |||
| Non-TBI | 30 (100) | 25 (83.4) | 55 (91.7) |
| TBI | - | 3 (10.0) | 3 (5.0) |
| Other | - | 2 (6.6) | 2 (3.3) |
| Months from ABI onset to the test session, median (IQR) | 1.6 (1.0, 1.4) | 5.6 (3.3, 14.7) | 2 (1.2, 5.5) |
| URJC Sample | InTeO Sample | Total Sample | ||||
|---|---|---|---|---|---|---|
| Tasks (Time) | Left UL (n = 19) | Right UL (n = 11) | Left UL (n = 14) | Right UL (n = 16) | Left UL (n = 33) | Right UL (n = 27) |
| 1. Forearm to table (side) | 0.7 (0.6; 0.8) | 0.7 (0.6; 0.7) | 0.9 (0.8; 1.2) | 1.0 (0.7; 1.3) | 0.8 (0.7; 0.9) | 0.7 (0.7; 1.1) |
| 2. Forearm to box (side) | 0.9 (0.9; 1.0) | 0.9 (0.8; 0.9) | 1.3 (1.1; 1.5) | 1.1 (0.9; 1.4) | 1.0 (0.9; 1.3) | 0.9 (0.8; 1.2) |
| 3. Extend elbow (side) | 0.9 (0.8; 1.0) | 0.9 (0.8; 1.2) | 1.3 (0.9; 1.6) | 1.0 (0.8; 1.3) | 1.0 (0.9; 1.3) | 0.9 (0.8; 1.2) |
| 4. Extend elbow (weight) | 1.1 (1.0; 1.2) | 1.0 (1.0; 1.5) | 1.0 (0.9; 1.6) | 0.9 (0.7; 1.4) | 1.1 (1.0; 1.3) | 1.0 (0.9; 1.5) |
| 5. Hand to table (front) | 0.7 (0.6; 0.8) | 0.7 (0.6; 0.8) | 1.0 (0.8; 1.2) | 0.9 (0.8; 1.1) | 0.8 (0.7; 1.0) | 0.8 (0.7; 1.0) |
| 6. Hand to box (front) | 0.9 (0.8; 1.0) | 1.0 (0.8; 1.3) | 1.0 (0.7; 1.2) | 0.8 (0.7; 1.0) | 0.9 (0.7; 1.0) | 0.9 (0.7; 1.1) |
| 7. Weight to box, in kg | 4.5 (3.5; 5.5) | 5.0 (4.3; 5.0) | 5.0 (4.1; 6.1) | 5.0 (3.9; 7.0) | 5.0 (3.5; 5.5) | 5.0 (4.0; 5.3) |
| 8. Reach and retrieve | 1.1 (1.0; 1.4) | 1.3 (1.0; 1.5) | 1.1 (0.9; 1.4) | 1.1 (0.9; 1.6) | 1.1 (1.0; 1.4) | 1.1 (0.9; 1.6) |
| 9. Lift can | 1.7 (1.4; 1.9) | 1.7 (1.2; 1.8) | 1.5 (1.4; 2.0) | 1.7 (1.3; 2.0) | 1.6 (1.4; 1.9) | 1.6 (1.3; 1.9) |
| 10. Lift pencil | 1.6 (1.1; 2.0) | 1.6 (1.2; 1.8) | 1.6 (1.3; 1.9) | 1.5 (1.1; 1.8) | 1.6 (1.3; 1.9) | 1.6 (1.2; 1.8) |
| 11. Lift paper clip | 1.9 (1.8; 2.0) | 1.9 (1.6; 2.0) | 1.6 (1.4; 1.8) | 1.5 (1.3; 2.4) | 1.8 (1.5; 2.0) | 1.7 (1.4; 2.3) |
| 12. Stack checkers | 3.9 (3.4; 4.3) | 4.0 (3.7; 4.3) | 3.7 (3.1; 4.5) | 3.9 (3.3; 4.2) | 3.8 (3.2; 4.3) | 4.0 (3.4; 4.3) |
| 13. Flip cards | 6.0 (5.4; 6.7) | 6.0 (5.2; 7.0) | 7.4 (5.7; 9.8) | 5.6 (4.7; 9.3) | 6.1 (5.6; 8.6) | 5.8 (4.9; 8.8) |
| 14. Grip strength, in kg | 38.3 (27.9; 40.1) | 28.0 (25.3; 35.4) | 29.3 (23.3; 37.3) | 31.6 (20.3; 38.0) | 35.6 (24.0; 39.5) | 29.3 (21.9; 37.1) |
| 15. Turn key in lock | 6.4 (5.9; 8.6) | 7.3 (6.3; 9.9) | 5.1 (4.0; 5.7) | 4.9 (4.2; 11.6) | 5.9 (5.1; 7.2) | 6.4 (4.7; 11.2) |
| 16. Fold towel | 8.3 (7.1; 13.4) | 8.0 (6.4; 9.9) | 6.7 (5.3; 7.6) | 7.6 (4.6; 9.7) | 7.4 (6.4; 9.2) | 7.8 (5.8; 9.2) |
| 17. Lift basket | 3.6 (3.0; 3.9) | 3.2 (3.0; 3.6) | 2.6 (2.1; 3.1) | 2.8 (2.2; 3.3) | 3.1 (2.6; 3.7) | 3.0 (2.6; 3.6) |
| Total | 39.9 (35.2; 49.5) | 41.7 (35.9; 44.8) | 41.1 (33.3; 47.0) | 40.0 (33.0; 69.8) | 39.9 (34.2; 48.8) | 40.6 (33.3; 53.8) |
| Tasks | URJC Sample | InTeO Sample | Total Sample | |||
|---|---|---|---|---|---|---|
| Left UL (n = 11) | Right UL (n = 19) | Left UL (n = 16) | Right UL (n = 14) | Left UL (n = 27) | Right UL (n = 33) | |
| 1. Forearm to table (side) | ||||||
| Time | 1.8 (1.3; 2.5) | 2.0 (1.6; 2.8) | 1.3 (0.9; 1.6) | 1.3 (1.0; 1.6) | 1.4 (1.0; 2.1) | 1.6 (1.3;2.2) |
| FA | 4.0 (4.0; 4.0) | 4.0 (3.5; 4.0) | 5.0 (4.0; 5.0) | 5.0 (4.0; 5.0) | 4.0 (4.0; 5.0) | 4.5 (4.0; 5.0) |
| 2. Forearm to box (side) | ||||||
| Time | 1.9 (1.9; 2.6) | 2.0 (1.9; 2.2) | 1.5 (1.1; 2.0) | 2.0 (1.6; 2.3) | 1.8 (1.3; 2.4) | 2.0 (1.7; 2.2) |
| FA | 4.0 (3.5; 4.0) | 4.0 (3.5; 4.0) | 4.0 (4.0; 5.0) | 4.0 (4.0; 4.0) | 4.0 (4.0; 4.0) | 4.0 (4.0; 4.0) |
| 3. Extend elbow (side) | ||||||
| Time | 2.3 (2.0; 3.6) | 2.4 (1.9; 3.5) | 1.4 (1.0; 1.8) | 1.6 (1.3; 1.9) | 1.9 (1.3; 2.6) | 2.0 (1.7; 2.6) |
| FA | 3.0 (3.0; 3.5) | 4.0 (3.0; 4.0) | 4.0 (3.0; 5.0) | 4.0 (4.0; 5.0) | 3.0 (3.0; 4.0) | 4.0 (3.0; 4.0) |
| 4. Extend elbow (weight) | ||||||
| Time | 3.3 (3.0; 4.3) | 3.0 (2.7; 3.8) | 1.2 (0.9; 1.2) | 1.3 (1.1; 2.0) | 2.2 (1.1; 3.8) | 2.7 (1.5; 3.2) |
| FA | 3.0 (3.0; 3.5) | 4.0 (3.0; 4.0) | 4.0 (3.8; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 4.0) | 4.0 (3.0; 4.0) |
| 5. Hand to table (front) | ||||||
| Time | 1.2 (1.0; 1.4) | 1.2 (1.0; 1.8) | 1.1 (0.9; 1.4) | 1.3 (1.1;1.6) | 1.1 (0.9; 1.4) | 1.2 (1.0; 1.7) |
| FA | 4.0 (4.0; 4.0) | 4.0 (4.0; 4.0) | 4.5 (3.8; 5.0) | 4.5 (4.0; 5.0) | 4.0 (4.0; 5.0) | 4.0 (4.0; 5.0) |
| 6. Hand to box (front) | ||||||
| Time | 2.0 (1.9; 2.0) | 1.9 (1.3; 2.2) | 1.0 (0.8; 1.4) | 1.1 (0.9; 1.6) | 1.4 (0.9; 1.9) | 1.6 (1.1; 2.0) |
| FA | 3.0 (3.0; 4.0) | 4.0 (3.0; 4.0) | 4.0 (4.0; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 4.5) | 4.0 (3.0; 4.0) |
| 7. Weight to box, in kg | 3.0 (2.3; 3.5) | 3.5 (2.8; 3.8) | 3.5 (2.4; 7.0) | 3.5 (2.0; 4.0) | 3.0 (2.3; 4.8) | 3.5 (2.0; 4.0) |
| 8. Reach and retrieve | ||||||
| Time | 1.9 (1.6; 2.0) | 2.0 (1.9; 2.1) | 1.4 (1.2; 1.7) | 1.4 (1.2; 2.3) | 1.6 (1.3; 2.0) | 1.9 (1.4; 2.1) |
| FA | 4.0 (3.5; 4.0) | 4.0 (3.5; 4.0) | 4.0 (3.0; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 4.5) | 4.0 (4.0; 4.0) |
| 9. Lift can | ||||||
| Time | 2.9 (2.5; 3.1) | 2.9 (2.5; 3.4) | 2.5 (1.7; 3.0) | 2.7 (2.1; 3.6) | 2.6 (2.0; 3.1) | 2.8 (2.4; 3.5) |
| FA | 3.0 (3.0; 4.0) | 4.0 (3.0; 4.0) | 4.0 (4.0; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 4.5) | 4.0 (3.0; 4.0) |
| 10. Lift pencil | ||||||
| Time | 5.0 (2.9; 6.6) | 5.0 (4.1; 5.3) | 2.0 (1.6; 2.4) | 2.4 (1.8; 3.2) | 2.7 (2.0; 4.8) | 4.1 (2.4; 5.2) |
| FA | 3.0 (3.0; 4.0) | 3.0 (3.0; 3.0) | 4.5 (4.0; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 5.0) | 3.0 (3.0; 4.0) |
| 11. Lift paper clip | ||||||
| Time | 8.5 (7.5; 10.5) | 8.7 (7.0; 10.7) | 2.5 (1.6; 3.6) | 3.3 (2.1; 4.0) | 4.6 (2.5; 8.9) | 6.2 (3.6; 9.5) |
| FA | 3.0 (2.0; 3.0) | 2.0 (1.0; 3.0) | 4.5 (3.8; 5.0) | 4.0 (4.0; 5.0) | 4.0 (3.0; 5.0) | 3.0 (2.0; 4.0) |
| 12. Stack checkers | ||||||
| Time | 10.8 (9.5; 13.5) | 9.6 (8.4; 12.2) | 7.4 (3.6; 12.8) | 6.2 (5.2; 7.4) | 10.6 (6.2; 13.5) | 8.5 (5.9; 11.0) |
| FA | 3.0 (3.0; 3.0) | 3.0 (3.0; 3.0) | 4.0 (2.0; 5.0) | 4.0 (4.0; 4.8) | 3.0 (3.0; 4.5) | 3.0 (3.0; 4.0) |
| 13. Flip cards | ||||||
| Time | 18.6 (14.1; 20.7) | 17.5 (11.5; 20.5) | 7.3 (5.4; 19.1) | 6.2 (5.2; 7.4) | 13.8 (6.7; 20.0) | 11.5 (9.8; 18.9) |
| FA | 3.0 (3.0; 3.0) | 3.0 (3.0; 3.0) | 3.0 (3.0; 4.0) | 3.0 (3.0; 3.8) | 3.0 (3.0; 3.5) | 3.0 (3.0; 3.0) |
| 14. Grip strength, in kg | 10.0 (8.0; 12.5) | 12.5 (8.8; 13.3) | 19.0 (10.2; 26.6) | 20.2 (12.5; 30.6) | 12.5 (9.1; 23.0) | 12.5 (9.0; 18.3) |
| 15. Turn key in lock | ||||||
| Time | 20.5 (19.1; 23.0) | 17.4 (16.1; 22.9) | 8.8 (4.7; 21.3) | 6.0 (5.4; 7.6) | 18.3 (7.3; 23.0) | 14.3 (6.5; 18.7) |
| FA | 3.0 (3.0; 3.0) | 3.0 (3.0; 3.0) | 3.5 (3.0; 4.0) | 3.0 (3.0; 4.0) | 3.0 (3.0; 4.0) | 3.0 (3.0; 4.0) |
| 16. Fold towel | ||||||
| Time | 12.3 (10.8; 17.4) | 15.4 (9.6; 17.5) | 8.3 (4.9; 9.8) | 7.7 (5.7; 29.1) | 9.9 (7.7; 12.4) | 10.4 (7.9; 16.0) |
| FA | 4.0 (3.0; 4.0) | 4.0 (3.0; 4.0) | 4.0 (4.0; 5.0) | 4.0 (4.5; 5.0) | 4.0 (3.0; 4.0) | 4.0 (3.0; 4.0) |
| 17. Lift basket | ||||||
| Time | 9.6 (7.7; 22.9) | 8.2 (6.5; 16.8) | 3.2 (2.2; 4.9) | 3.5 (3.0; 4.3) | 5.3 (2.9; 17.5) | 5.3 (3.5; 8.3) |
| FA | 4.0 (3.5; 4.0) | 4.0 (3.0; 4.0) | 4.0 (3.8; 5.0) | 4.0 (3.3; 4.0) | 4.0 (3.5; 4.0) | 4.0 (3.0; 4.0) |
| Total | ||||||
| Time | 113.0 (93.0; 125.8) | 98.8 (84.7; 109.5) | 120.1 (34.9; 212.9) | 51.3 (45.1; 60.3) | 112.95 (65.9; 181.4) | 79.4 (57.1; 101.7) |
| FA | 51.0 (50.0; 52.0) | 52.0 (51.0; 54.4) | 69.5 (56.0; 76.25) | 66.5 (61.8; 70.25) | 54.0 (50.0; 66.5) | 54.0 (51.0; 61.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Casaña-Escriche, E.; Sánchez-Cabeza, Á.; Huertas Hoyas, E.; Valera-Gran, D.; Navarrete-Muñoz, E.-M. Spanish Translation and Cultural Adaptation of the Wolf Motor Function Test for Survivors of Acquired Brain Injury. Healthcare 2025, 13, 1969. https://doi.org/10.3390/healthcare13161969
Casaña-Escriche E, Sánchez-Cabeza Á, Huertas Hoyas E, Valera-Gran D, Navarrete-Muñoz E-M. Spanish Translation and Cultural Adaptation of the Wolf Motor Function Test for Survivors of Acquired Brain Injury. Healthcare. 2025; 13(16):1969. https://doi.org/10.3390/healthcare13161969
Chicago/Turabian StyleCasaña-Escriche, Empar, Ángel Sánchez-Cabeza, Elisabet Huertas Hoyas, Desirée Valera-Gran, and Eva-María Navarrete-Muñoz. 2025. "Spanish Translation and Cultural Adaptation of the Wolf Motor Function Test for Survivors of Acquired Brain Injury" Healthcare 13, no. 16: 1969. https://doi.org/10.3390/healthcare13161969
APA StyleCasaña-Escriche, E., Sánchez-Cabeza, Á., Huertas Hoyas, E., Valera-Gran, D., & Navarrete-Muñoz, E.-M. (2025). Spanish Translation and Cultural Adaptation of the Wolf Motor Function Test for Survivors of Acquired Brain Injury. Healthcare, 13(16), 1969. https://doi.org/10.3390/healthcare13161969








