Respiratory Failure in Patients with Intracerebral Hemorrhage and Intraventricular Hemorrhage Extension: A Retrospective Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. An Evaluation of the Development of Respiratory Failure
2.3. Severity of IVH Extension and Estimation of ICH Volume
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICH | Intracerebral Hemorrhage |
| IVH | Intraventricular Hemorrhage |
| ABGA | Arterial Blood Gas Analysis |
| CT | Computed Tomography |
| SPSS | Statistical Package for Social Sciences |
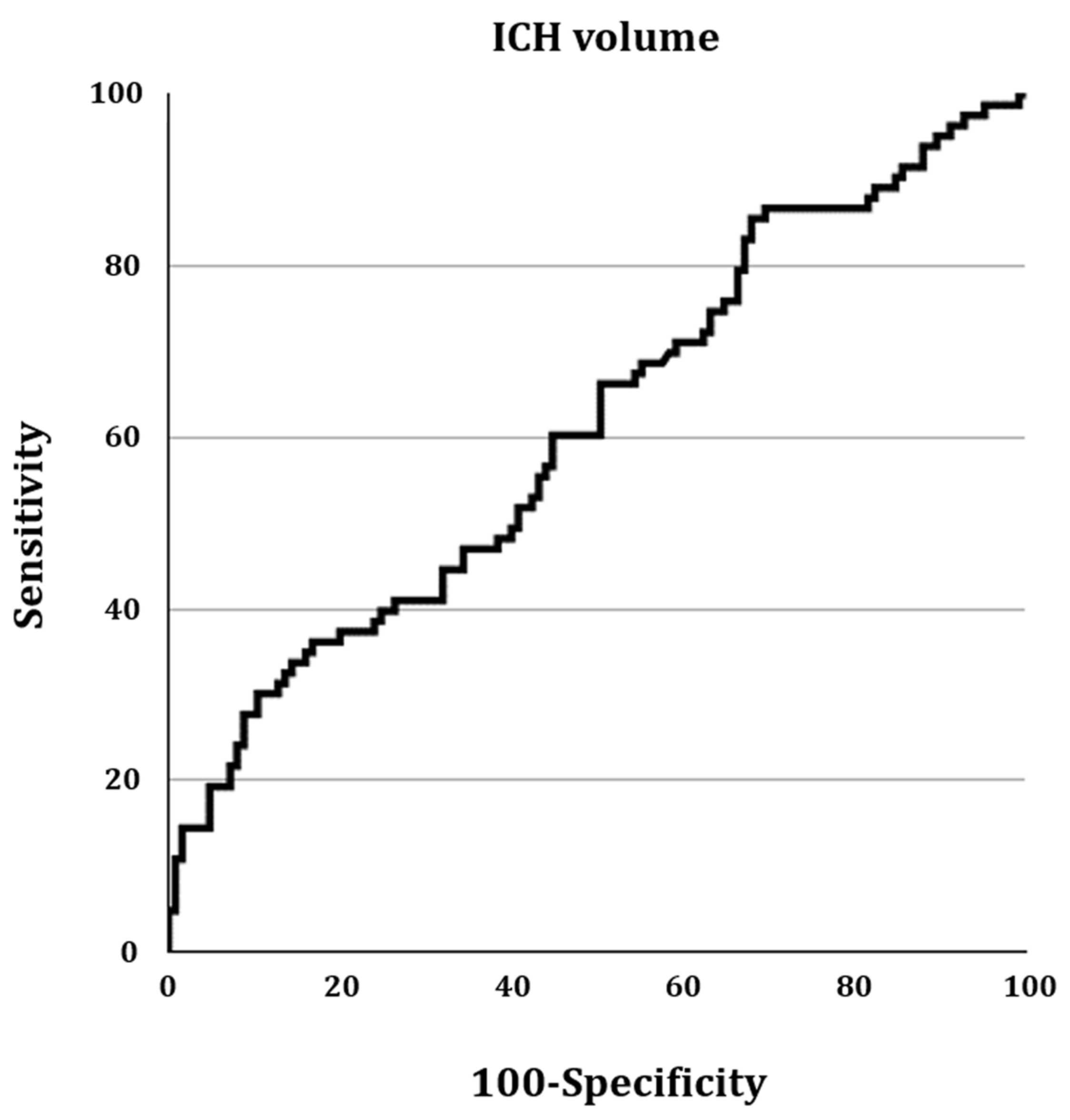
| ROC | Receiver Operating Characteristic |
References
- Li, X.; Zhang, L.; Wolfe, C.D.A.; Wang, Y. Incidence and Long-Term Survival of Spontaneous Intracerebral Hemorrhage Over Time: A Systematic Review and Meta-Analysis. Front. Neurol. 2022, 13, 819737. [Google Scholar] [CrossRef] [PubMed]
- Suthar, N.N.; Patel, K.L.; Saparia, C.; Parikh, A.P. Study of clinical and radiological profile and outcome in patients of intracranial hemorrhage. Ann. Afr. Med. 2016, 15, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Chang, M.C.; Kwak, S.G.; Park, D. Prediction of the motor prognosis with diffusion tensor imaging in hemorrhagic stroke: A meta-analysis. J. Integr. Neurosci. 2021, 20, 1011–1017. [Google Scholar] [CrossRef] [PubMed]
- Rochester, C.L.; Mohsenin, V. Respiratory complications of stroke. Semin. Respir. Crit. Care Med. 2002, 23, 248–260. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Gao, Y.; Wan, J.; Lan, X.; Han, X.; Zhu, S.; Zang, W.; Chen, X.; Ziai, W.; Hanley, D.F.; et al. Changes in motor function, cognition, and emotion-related behavior after right hemispheric intracerebral hemorrhage in various brain regions of mouse. Brain Behav. Immun. 2018, 69, 568–581. [Google Scholar] [CrossRef] [PubMed]
- Stretz, C.; Gao, C.; Greer, D.M.; Loomis, C.; Gilmore, E.J.; Kundishora, A.J.; Matouk, C.C.; Hwang, D.Y. Intracerebral Hemorrhage with Intraventricular Extension-Getting the Prognosis Right Early. Front. Neurol. 2017, 8, 418. [Google Scholar] [CrossRef] [PubMed]
- Witsch, J.; Falcone, G.J.; Leasure, A.C.; Matouk, C.; Endres, M.; Sansing, L.; Woo, D.; Sheth, K.N. Intracerebral Hemorrhage with Intraventricular Extension Associated with Loss of Consciousness at Symptom Onset. Neurocrit. Care 2021, 35, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Vingerhoets, F.; Bogousslavsky, J. Respiratory dysfunction in stroke. Clin. Chest Med. 1994, 15, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, K.; Kawakami, K.; Onimaru, H.; Okada, Y.; Yokota, S.; Koshiya, N.; Oku, Y.; Iizuka, M.; Koizumi, H. The respiratory control mechanisms in the brainstem and spinal cord: Integrative views of the neuroanatomy and neurophysiology. J. Physiol. Sci. 2017, 67, 45–62. [Google Scholar] [CrossRef] [PubMed]
- Benarroch, E.E. Brainstem respiratory chemosensitivity: New insights and clinical implications. Neurology 2007, 68, 2140–2143. [Google Scholar] [CrossRef] [PubMed]
- Mirabile, V.S.; Shebl, E.; Sankari, A.; Burns, B. Respiratory Failure in Adults; StatPearls: Treasure Island, FL, USA, 2025. Available online: https://www.ncbi.nlm.nih.gov/books/NBK526127/ (accessed on 11 June 2023).
- Graeb, D.A.; Robertson, W.D.; Lapointe, J.S.; Nugent, R.A.; Harrison, P.B. Computed tomographic diagnosis of intraventricular hemorrhage. Etiology and prognosis. Radiology 1982, 143, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Jang, S.H.; Choi, B.Y.; Chang, C.H.; Kim, S.H.; Chang, M.C. Prediction of motor outcome based on diffusion tensor tractography findings in thalamic hemorrhage. Int. J. Neurosci. 2013, 123, 233–239. [Google Scholar] [CrossRef] [PubMed]
- Bisson, D.A.; Flaherty, M.L.; Shatil, A.S.; Gladstone, D.; Dowlatshahi, D.; Carrozzella, J.; Zhang, L.; Hill, M.D.; Demchuck, A.; Aviv, R.I. Original and Modified Graeb Score Correlation with Intraventricular Hemorrhage and Clinical Outcome Prediction in Hyperacute Intracranial Hemorrhage. Stroke 2020, 51, 1696–1702. [Google Scholar] [CrossRef] [PubMed]
- Trifan, G.; Arshi, B.; Testai, F.D. Intraventricular Hemorrhage Severity as a Predictor of Outcome in Intracerebral Hemorrhage. Front. Neurol. 2019, 10, 217. [Google Scholar] [CrossRef] [PubMed]
- Maramattom, B.V.; Weigand, S.; Reinalda, M.; Wijdicks, E.F.; Manno, E.M. Pulmonary complications after intracerebral hemorrhage. Neurocrit. Care 2006, 5, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Broderick, J.P.; Adams, H.P., Jr.; Barsan, W.; Feinberg, W.; Feldmann, E.; Grotta, J.; Kase, C.; Krieger, D.; Mayberg, M.; Tilley, B.; et al. Guidelines for the management of spontaneous intracerebral hemorrhage: A statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke 1999, 30, 905–915. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.; Chuchalin, A.; Gusev, E.; Martynov, M.; Shogenova, L.; Panin, A. The syndrome of respiratory failure in acute stroke patients. Eur. Respir. J. 2020, 56, 2009. [Google Scholar] [CrossRef]
| Total (n = 208) | RF Group (n = 83) | Non-RF Group (n =125) | p-Value | 95% CI (Lower Limit, Upper Limit) | |
|---|---|---|---|---|---|
| Age (years), mean ± SD | 58.4 ± 13.0 | 58.2 ± 11.5 | 58.8 ± 13.9 | 0.782 | −3.123, 4.145 |
| Sex (M:F) | 110:98 | 43:40 | 67:58 | 0.800 | |
| Graeb scale score, mean ± SD | 6.3 ± 3.0 | 6.6 ± 2.9 | 6.2 ± 3.0 | 0.324 | −1.253, 0.417 |
| ICH volume (mL), mean ± SD | 32.6 ± 34.2 | 42.0 ± 42.5 | 26.4 ± 25.7 | 0.003 | −25.905, −5.331 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, M.C.; Lee, M.Y.; Kwak, S.G.; Lee, A.Y. Respiratory Failure in Patients with Intracerebral Hemorrhage and Intraventricular Hemorrhage Extension: A Retrospective Study. Healthcare 2025, 13, 1876. https://doi.org/10.3390/healthcare13151876
Chang MC, Lee MY, Kwak SG, Lee AY. Respiratory Failure in Patients with Intracerebral Hemorrhage and Intraventricular Hemorrhage Extension: A Retrospective Study. Healthcare. 2025; 13(15):1876. https://doi.org/10.3390/healthcare13151876
Chicago/Turabian StyleChang, Min Cheol, Michael Y. Lee, Sang Gyu Kwak, and Ah Young Lee. 2025. "Respiratory Failure in Patients with Intracerebral Hemorrhage and Intraventricular Hemorrhage Extension: A Retrospective Study" Healthcare 13, no. 15: 1876. https://doi.org/10.3390/healthcare13151876
APA StyleChang, M. C., Lee, M. Y., Kwak, S. G., & Lee, A. Y. (2025). Respiratory Failure in Patients with Intracerebral Hemorrhage and Intraventricular Hemorrhage Extension: A Retrospective Study. Healthcare, 13(15), 1876. https://doi.org/10.3390/healthcare13151876







