A Pilot Randomized Controlled Trial to Examine the Impact of a Therapy Dog Intervention on Depression, Mood, and Anxiety in Hospitalized Older Adults
Abstract
1. Introduction
2. Materials and Methods
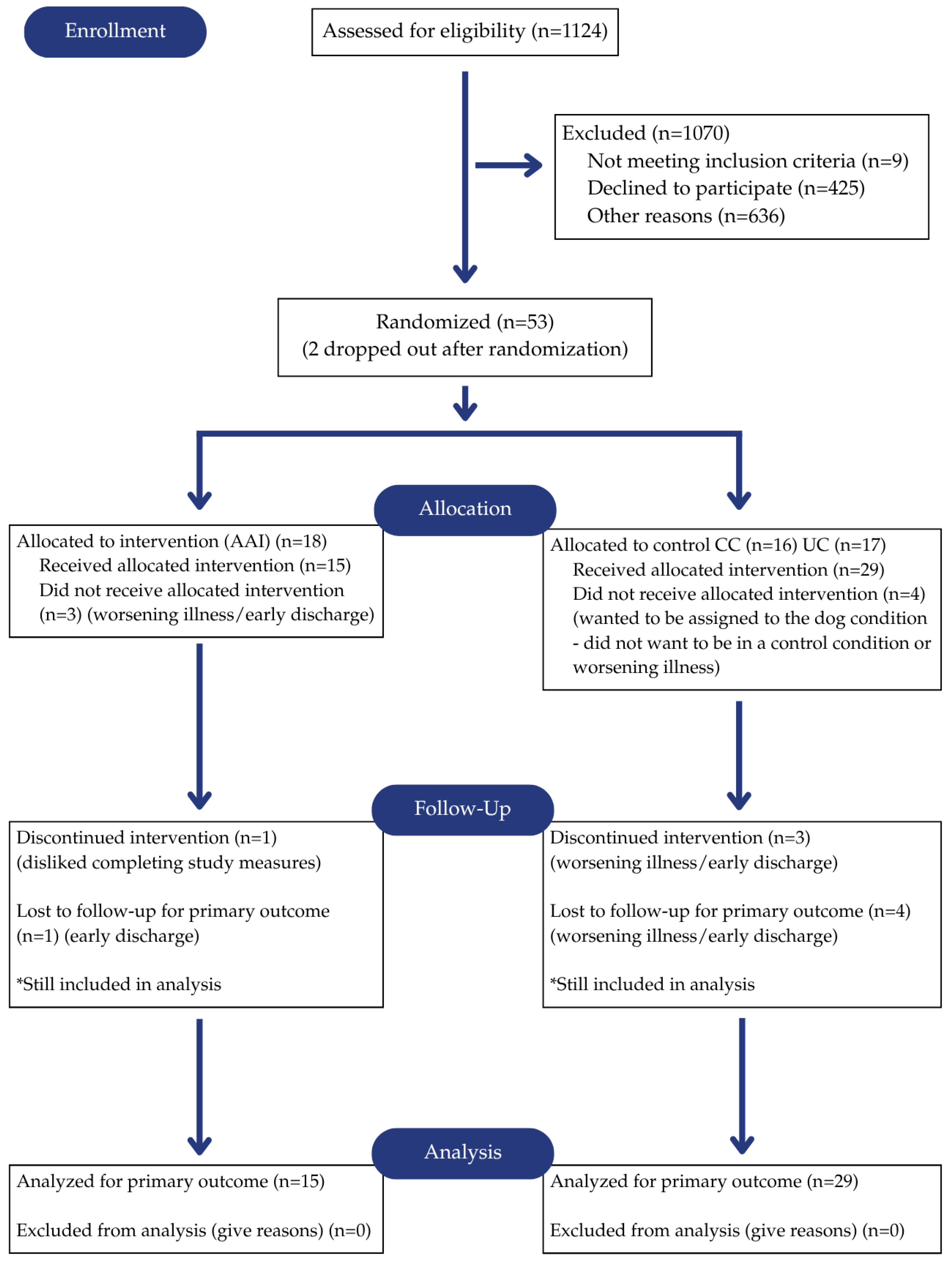
2.1. Design
2.2. Participants
2.3. Therapy Dogs and Handlers
2.4. Measures
2.5. Procedure
- (1)
- Animal-Assisted Interaction (AAI; n = 15): A Dogs on Call dog and handler team participated in a non-scripted interaction with these participants, a procedure repeated on three consecutive days. To facilitate the fidelity and consistency of treatment delivery, the handler was provided in advance with specific discussion topics, such as sports, the weather, or animals. The same dog/handler team may or may not participate in multiple visits to the same patient. The assignment of dog/handler teams was based purely on their availability.
- (2)
- Conversational Control (CC; n = 15): The handler visited the participant alone, without their dog, for a non-scripted interaction as instructed for the AAI condition. The sessions were also repeated on three consecutive days.
- (3)
- Usual Care (UC; n = 14): No additional interventions were provided to participants in the UC condition beyond their usual hospital care. Participants rested or engaged in a quiet activity during the 20 min intervention period.
3. Results
3.1. Satisfaction
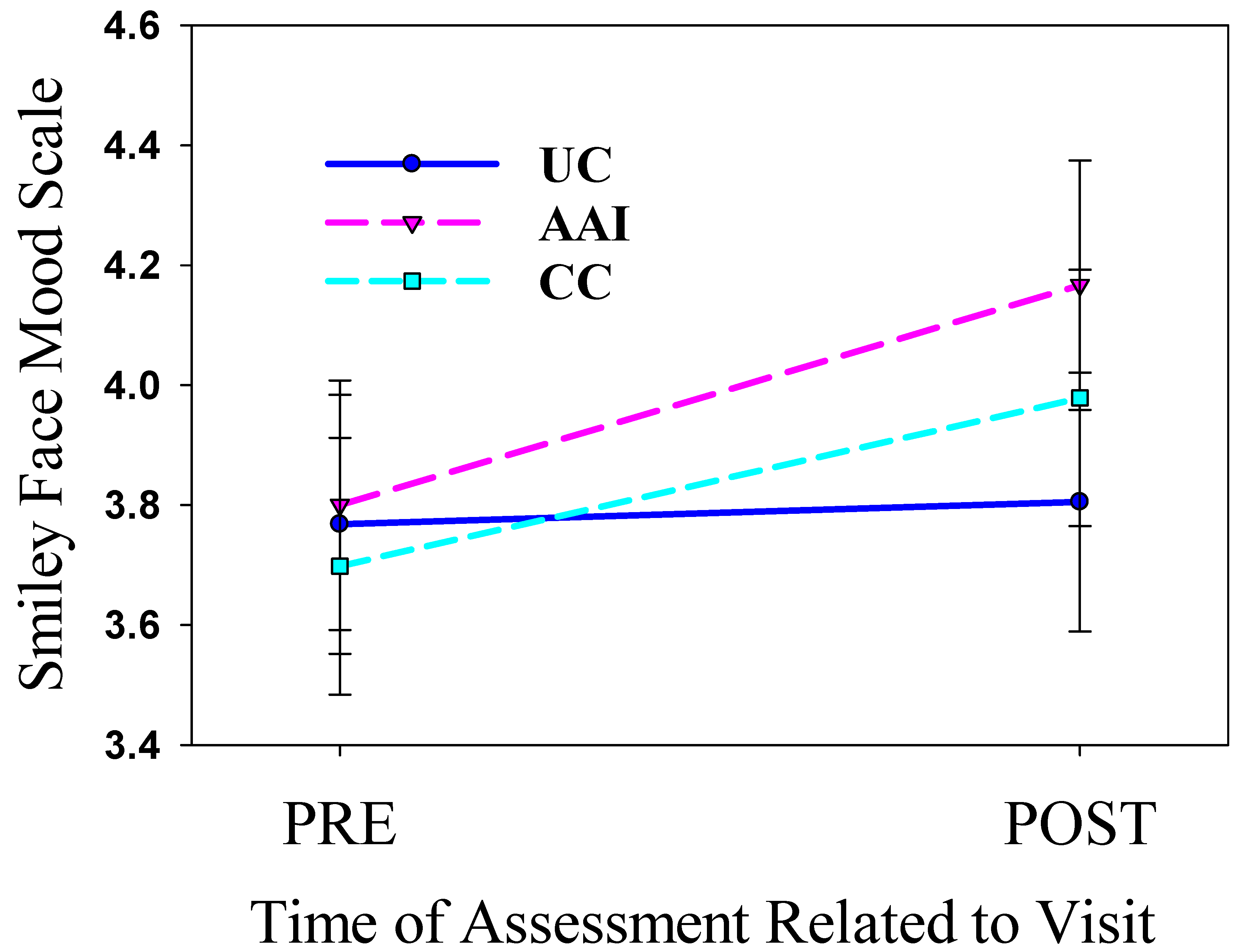
3.2. Intervention Period—Mood
3.3. Intervention Period—Amount of Anxiety
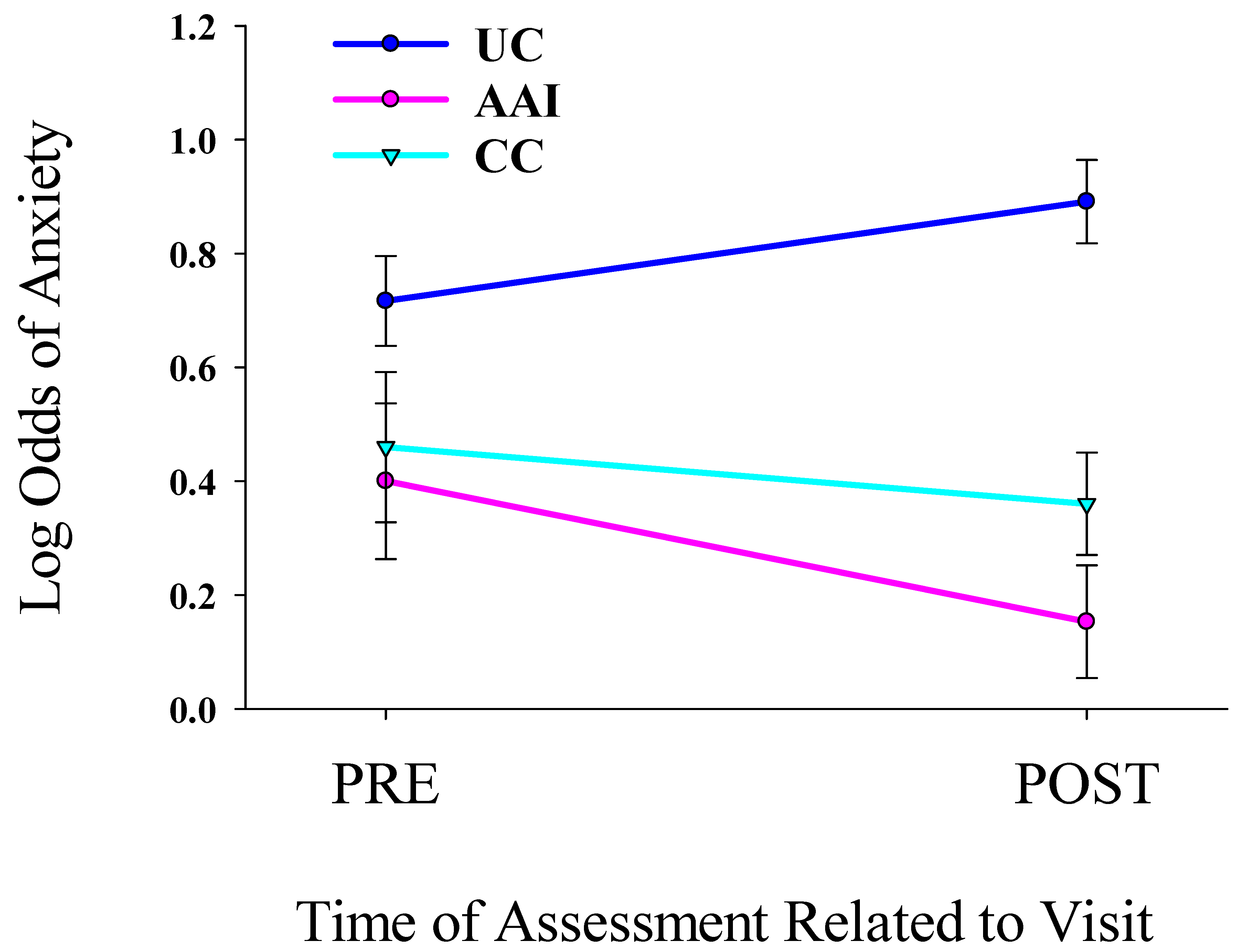
3.4. Intervention Period—Presence of Anxiety
3.5. Study Duration: Baseline to Day 5 and 1 and 6 Months—Amount of Anxiety
3.6. Study Duration: Baseline to Day 5 and 1 and 6 Months—Depression
3.7. Study Duration: Baseline to Day 5 and 1 and 6 Months—Quality of Life
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAI | Animal-Assisted Intervention |
| CC | Conversational Control condition—Handler Only |
| UC | Usual Care Condition |
| DoC | Dogs on Call |
| VCU | Virginia Commonwealth University |
| VCUH | Virginia Commonwealth University Health System |
| BIMS | Brief Interview for Mental Status |
| CESD | Center for Epidemiological Studies, Depression |
| STAI | State Trait Anxiety Inventory |
| HRQOL | Health Related Quality of Life |
References
- United Nations Department of Economic and Social Affairs, Population Division. World Population Prospects 2024: Summary of Results. 11 July 2024. (UN DESA/POP/2024/TR/NO. 9). Available online: https://population.un.org/wpp/ (accessed on 12 July 2025).
- Caplan, Z.U.S. Older Population Grew From 2010 to 2020 at Fastest Rate Since 1880 to 1890. 25 May 2023. Available online: https://www.census.gov/library/stories/2023/05/2020-census-united-states-older-population-grew.html (accessed on 12 July 2025).
- World Health Organization. Ageing and Health. 2 October 2022. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health#:~:text=The%20pace%20of%20population%20ageing,from%2012%25%20to%2022%25 (accessed on 12 July 2025).
- Tenchov, R.; Sasso, J.M.; Wang, X.; Qiongqiong, A.Z. Aging hallmarks and progression and age-related diseases: A landscape view of research advancement. ACH Chem. Neurosci. 2024, 15, 1–30. [Google Scholar] [CrossRef] [PubMed]
- United States Surgeon General. Our Epidemic of Loneliness and Isolation: The U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community. 2023. Available online: https://www.hhs.gov/sites/default/files/surgeon-general-social-connection-advisory.pdf (accessed on 12 July 2025).
- Kwong, A.S.F.; Pearson, R.M.; Adams, M.J.; Northstone, K.; Tilling, K.; Smith, D.; Fawns-Ritchie, C.; Bould, H.; Warne, N.; Zammit, S.; et al. Mental health before and during the COVID-19 pandemic in two longitudinal UK population cohorts. Br. J. Psychiatry 2021, 218, 334–343. [Google Scholar] [CrossRef]
- Cai, H.; Jin, Y.; Liu, R.; Zhang, Q.; Su, Z.; Ungvari, G.S. Global prevalence of depression in older adults: A systematic review and meta-analysis of epidemiological surveys. Asian J. Psychiatry 2023, 80, 103417. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, P.; Chitnis, A.; Louie, D.; Suthoff, E.; Chen, S.Y.; Maitland, J. The economic burden of adults with major depressive disorder in the United States (2019). Adv. Ther. 2023, 40, 4460–4479. [Google Scholar] [CrossRef]
- Gee, N.R.; Mueller, M.K. A systematic review of research on pet ownership and animal interactions among older adults. Anthrozoös 2019, 32, 183–207. [Google Scholar] [CrossRef]
- Manville, K.; Coulson, M.; Mulqueen, M.A.; Neller, K.; Searing, C.; Welland, S. Effects of canine assisted intervention on mental health of higher education students: A systematic review. Hum. Anim. Interact. 2022, 12, 111–145. [Google Scholar]
- Gee, N.R.; Mueller, M.; Curl, A. Human-animal interaction and older adults: An overview. Front. Psychol. 2017, 8, 1461. [Google Scholar] [CrossRef]
- Gee, N.R.; Townsend, L.; Findling, R. (Eds.) The Role of Companion Animals in the Treatment of Mental Disorders; American Psychiatric Association: Washington, DC, USA, 2023. [Google Scholar]
- Ko, H.J.; Youn, C.H.; Kim, S.H.; Kim, S.Y. Effect of pet insects on the psychological health of community-dwelling elderly people: A single-blinded, randomized, controlled trial. Gerontology 2016, 62, 200–209. [Google Scholar] [CrossRef]
- Colombo, G.; Buono, M.D.; Smania, K.; Raviola, R.; De Leo, D. Pet therapy and institutionalized elderly: A study on 144 cognitively unimpaired subjects. Arch. Gerontol. Geriatr. 2006, 42, 207–216. [Google Scholar] [CrossRef]
- Travers, C.; Perkins, J.; Rand, J.; Bartlett, H.; Morton, J. An evaluation of dog-assisted therapy for residents of aged care facilities with dementia. Anthrozoos 2013, 26, 213–225. [Google Scholar] [CrossRef]
- Borgi, M.; Collacchi, B.; Giuliani, A.; Cirulli, F. Dog visiting programs for managing depressive symptoms in older adults: A meta-analysis. Gerontologist 2020, 60, e66–e75. [Google Scholar] [CrossRef]
- Aarskog, N.K.; Hunskar, I.; Bruvik, F. Animal-assisted interventions with dogs and robotic animals for residents of with dementia in nursing homes: A systematic review. Phys. Occup. Ther. Geriatr. 2019, 37, 77–93. [Google Scholar] [CrossRef]
- Chang, S.J.; Lee, J.; An, H.; Hong, W.H.; Lee, J.Y. Animal-assisted therapy as an intervention for older adults: A systematic review and meta-analysis to guide evidence-based practice. Worldviews Evid.-Based Nurs. 2021, 18, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Berry, A.; Borgi, M.; Terranova, L.; Chiarotti, F.; Alleva, E.; Cirulli, F. Developing effective animal- assisted intervention programs involving visiting dogs for institutionalized geriatric patients: A pilot study. Psychogeriatrics 2012, 12, 143–150. [Google Scholar] [CrossRef] [PubMed]
- Phelps, K.A.; Miltenberger, R.G.; Jens, T.; Wadeson, H. An investigation of the effects of dog visits on depression, mood, and social interaction in elderly individuals living in a nursing home. Behav. Interv. 2018, 23, 181–200. [Google Scholar] [CrossRef]
- Saha, S.; Lim, C.C.W.; Cannon, D.L.; Burton, L.; Bremner, M.; Cosgrove, P.; Huo, Y.; McGrath, J.J. Co-morbidity between mood and anxiety disorders: A systematic review and meta-analysis. Depress. Anxiety 2021, 38, 286–306. [Google Scholar] [CrossRef]
- Lamers, F.; van Oppen, P.; Comijs, H.C.; Smit, J.H.; Spinhoven, P.; van Balkom, A.J.L.M.; Nolen, W.A.; Zitman, F.G.; Beekman, A.T.F.; Penninx, B. Comorbidity patterns of anxiety and depressive disorders in a large cohort study: The Netherlands Study of Depression and Anxiety (NESDA). J. Clin. Psychiatry 2011, 72, 341. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Abate, S.V. Chapter 10: Animal-assisted therapy for cardiac conditions. In Animal Assisted Therapy Use Application by Condition; Altschuler, E., Ed.; Academic Press: Cambridge, MA, USA, 2023; pp. 147–164. [Google Scholar] [CrossRef]
- Özdemir, S.T.; Özer, S. The effect of animal assisted rehabilitation practices on symptoms of Alzheimer’s patients: Systematic review and meta-analysis. Geriatr. Nurs. 2025, 63, 521–527. [Google Scholar] [CrossRef]
- LeRoux, M.; Kemp, R. Effect of a companion dog on depression and anxiety levels of elderly residents in a long-term care facility. Psychogeriatrics 2009, 9, 23–26. [Google Scholar] [CrossRef]
- Barker, S.B.; Pandurangi, A.K.; Best, A.M. Effects of animal-assisted therapy on patients’ anxiety, fear, and depression before ECT. J. ECT 2003, 19, 38–44. [Google Scholar] [CrossRef]
- Schattner, A. The spectrum of hospitalization-associated harm in the elderly. Eur. J. Intern. Med. 2023, 115, 29–33. [Google Scholar] [CrossRef]
- Townsend, L.; Gee, N.R.; Friedmann, E.; Mueller, M.; Barker, S. Recruitment feasibility for a randomized controlled pilot study of animal-assisted intervention for hospitalized older adults. J. Ageing Longev. 2024, 4, 404–416. [Google Scholar] [CrossRef]
- Gee, N.R.; Townsend, L.; Friedmann, E.; Barker, S.; Mueller, M. A pilot randomized controlled trial to examine the impact of a therapy dog intervention on loneliness in hospitalized older adults. Innov. Aging. 2024, 8, igae085. [Google Scholar] [CrossRef] [PubMed]
- Hopewell, S.; Chan, A.-W.; Collins, G.S.; Hróbjartsson, A.; Moher, D.; Schulz, K.F.; Tunn, R.; Aggarwal, R.; Berkwits, M.; A Berlin, J.; et al. CONSORT 2025 Statement: Updated guideline for reporting randomised trials. BMJ 2025, 388, e081123. [Google Scholar] [CrossRef] [PubMed]
- Center for Human-Animal Interaction. Dogs on Call Program. Available online: https://chai.vcu.edu/programs--services/dogs-on-call/ (accessed on 17 July 2025).
- Barker, S.B.; Holloway, R.; Barker, R.T. Animal-Assisted Interventions in Health Care Settings; Purdue University Press: West Lafayette, Indiana, 2019. [Google Scholar]
- Townsend, L.; Towsley, N.; Gee, N.R. “Dogs on Call”: A Community-Engaged Human Subjects Training with Hospital Based Therapy Dog Teams. J. Empir. Res. Hum. Res. Ethics 2023, 18, 363–371. [Google Scholar] [CrossRef]
- Chodosh, J.; Edelen, M.O.; Buchanan, J.L.; Yosef, J.A.; Ouslander, J.G.; Berlowitz, D.R.; Streim, J.E.; Saliba, D. Nursing Home Assessment of Cognitive Impairment: Development and testing of a Brief Instrument of Mental Status. J. Am. Geriatr. Soc. 2008, 56, 2069–2075. [Google Scholar] [CrossRef]
- Brown, D.W.; Balluz, L.S.; Giles, W.H.; Beckles, G.L.; Moriarty, D.G.; Ford, E.S.; Mokdad, A.H. Diabetes mellitus and health-related quality of life among older adults: Findings from the behavioral risk factor surveillance system (BRFSS). Diabetes Res. Clin. Pract. 2004, 65, 105–115. [Google Scholar] [CrossRef]
- Dominick, K.L.; Ahern, F.M.; Gold, C.H.; Heller, D.A. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clin. Exp. Res. 2002, 14, 499–508. [Google Scholar] [CrossRef]
- American Psychological Association. APA Dictionary of Psychology: Anxiety. Available online: https://dictionary.apa.org/anxiety (accessed on 17 July 2025).
- Julian, L.R. Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Res. 2011, 63, S467–S472. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zsido, A.N.; Teleki, S.A.; Csokasi, K.; Rozsa, S.; Bandi, S.A. Development of the short version of the Spielberger state—Trait anxiety inventory. Psychiatry Res. 2020, 291, 113223. [Google Scholar] [CrossRef]
- American Psychological Association. APA Dictionary of Psychology: Depression. Available online: https://dictionary.apa.org/depression (accessed on 17 July 2025).
- Andresen, E.M.; Malmgren, J.A.; Carter, W.B.; Patrick, D.L. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am. J. Prev. Med. 1994, 10, 77–84. [Google Scholar] [CrossRef]
- Radloff, L.S. The CES-D scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977, 1, 385–401. [Google Scholar] [CrossRef]
- Pérez-Sáez, E.; Cabrero-Montes, E.M.; Llorente-Cano, M.; González-Ingelmo, E. A pilot study on the impact of a pottery workshop on the well-being of people with dementia. Dementia 2018, 19, 2056–2072. [Google Scholar] [CrossRef] [PubMed]
- Julious, S.A. Sample size of 12 per group rule of thumb for a pilot study. Pharm. Stat. 2005, 4, 287–291. [Google Scholar] [CrossRef]
- Correia-Caeiro, C.; Romero, T.; Guo, K.; Mills, D.S. Older adults Looking at dog pictures—Psychobiological effects. Acta Psychol. 2025, 258, 105221. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gee, N.R.; Townsend, L.; Friedmann, E.; Barker, S.; Mueller, M. A Pilot Randomized Controlled Trial to Examine the Impact of a Therapy Dog Intervention on Depression, Mood, and Anxiety in Hospitalized Older Adults. Healthcare 2025, 13, 1819. https://doi.org/10.3390/healthcare13151819
Gee NR, Townsend L, Friedmann E, Barker S, Mueller M. A Pilot Randomized Controlled Trial to Examine the Impact of a Therapy Dog Intervention on Depression, Mood, and Anxiety in Hospitalized Older Adults. Healthcare. 2025; 13(15):1819. https://doi.org/10.3390/healthcare13151819
Chicago/Turabian StyleGee, Nancy R., Lisa Townsend, Erika Friedmann, Sandra Barker, and Megan Mueller. 2025. "A Pilot Randomized Controlled Trial to Examine the Impact of a Therapy Dog Intervention on Depression, Mood, and Anxiety in Hospitalized Older Adults" Healthcare 13, no. 15: 1819. https://doi.org/10.3390/healthcare13151819
APA StyleGee, N. R., Townsend, L., Friedmann, E., Barker, S., & Mueller, M. (2025). A Pilot Randomized Controlled Trial to Examine the Impact of a Therapy Dog Intervention on Depression, Mood, and Anxiety in Hospitalized Older Adults. Healthcare, 13(15), 1819. https://doi.org/10.3390/healthcare13151819






