The Historical Development of the Successful Dialogues in Mental Health Model
Abstract
1. Introduction
2. Materials and Methods
2.1. The Context of the Study: La Verneda-Sant Martí Adult School
2.2. Data Collection
2.3. Document Analysis
2.4. In-Depth Communicative Interviews
2.5. Data Analysis
3. Results
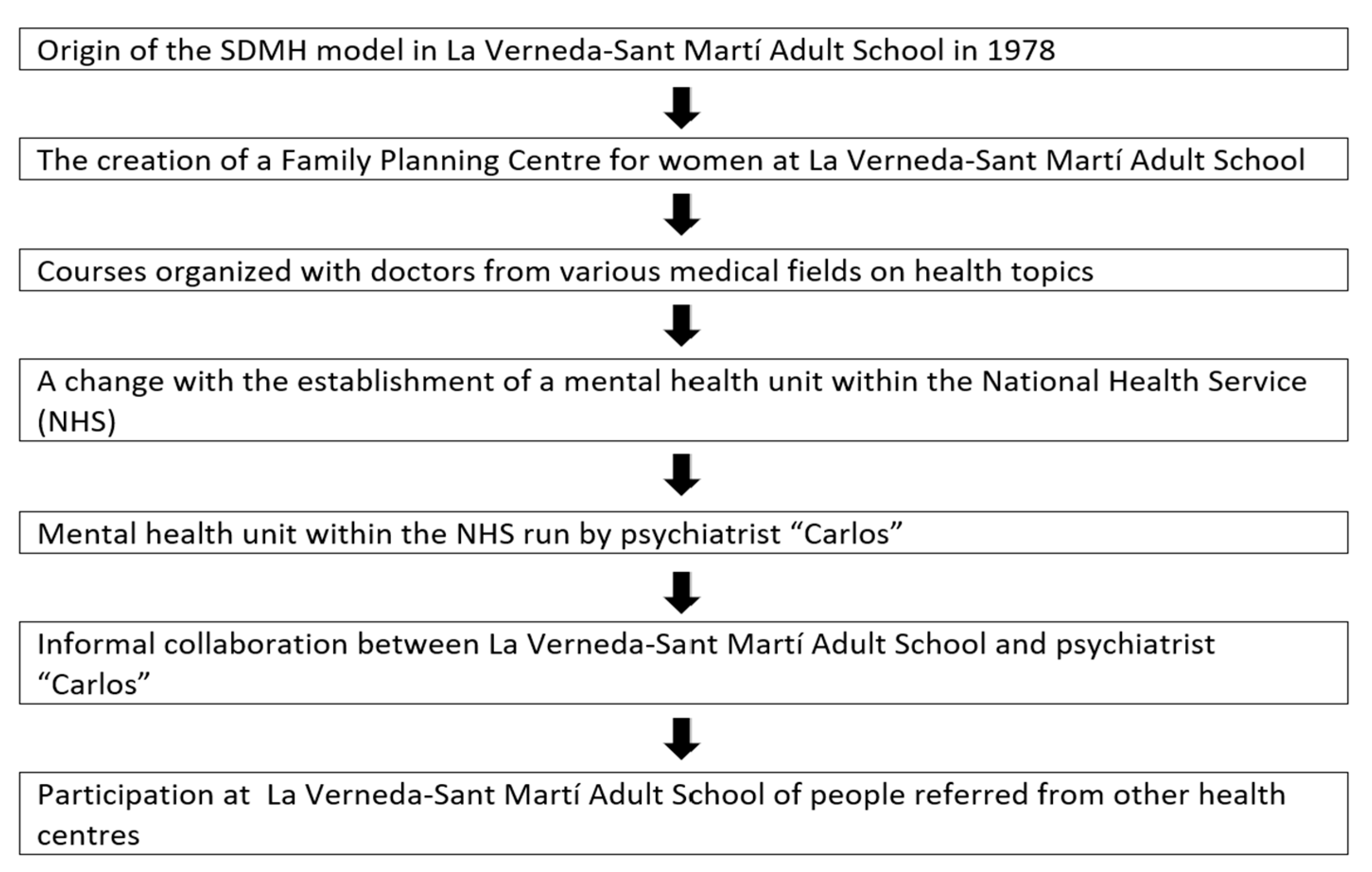
3.1. Co-Creation as the Seed for the Development of the SDMH Model
“From the outset, educators were attentive, listening to the conversations of participants of the adult school with mental health issues and the dialogues that supported them, contributing to opening these collaborations with health professionals.”.(Raquel)
“Yes, those of us who were working there did talk about mental health directly because we saw it very clearly. At that time (when I started working in the school), we were already talking about it in those terms. It’s not something we analyse and think about now, no. At that time, we were aware of what we were doing and understood the importance of it.”(Raquel)
“In the same building, there was the adult school, the library, the childcare centre, and the women’s health centre. A doctor from the public health system volunteered her time in that family planning space, undertaking highly committed volunteer work.”(Julia)
“We did so many things. I recall developing a course, although I don’t remember the title, with the doctor who volunteered at the school. At the time, I was teaching biology at the school, and we conducted a health program, so we had numerous dialogues with her and “the other women” (participants in the school) about mental health and health issues. We did this health programme for several years. That was in the early 1980s.”(Julia)
“We then had a long-standing relationship with Carlos’s Psychiatry Group. He was a very famous psychiatrist. Then, the psychiatrist and mental health group, who were in Sant Martí, sent people with mental health issues to the school. It lasted for many years, and we had a really smooth relationship. We knew it because people came and told us, ‘The Carlos group recommended that I come here.’ That is why a few years ago, Carlos was the town crier for the Verneda festivities.”(Julia)
“The school is highly regarded. I have met people who said they came to the school on the recommendation of their primary care doctor, not a mental health professional or the Carlos team. Even people from Granollers—I recall one participant who came from there because his doctor had recommended it.”.(Raquel)
3.2. The Origins of SDMH Detached from Psychiatric Intervention
“This group was marked by a kind of ideological ferment, blending elements of anti-psychiatry and Marxist psychoanalysis. I was among them, part of that circle. However, we soon positioned ourselves in opposition to the idea of anti-psychiatry. David Cooper, closely associated with Foucault, was one of its leading proponents. In his book, The Death of the Family, for instance, Cooper advanced arguments that we now view as emancipatory, but which were not perceived as such at the time. Moreover, it was particularly troubling that both Cooper and Foucault supported the decriminalisation of rape and the defence of pederastia. We were unequivocally and radically opposed to these ideas.”(Marcos)
“The leader of this group was Miguel [pseudonym], a highly democratic and progressive figure who was expelled from the university in 1968 as a result of a democratic movement against Franco. He later went on to work in a mental health institution in 1973. Marcos notes that, while Miguel did not establish a formal movement, he did initiate a critical reflection on mental health practice, effectively leading the broader process of collective engagement. Dialogic approach to psychiatry was therefore developed in those alternative environments of the time, and in strong collaboration with dialogic social and educational movements that focused on the improvement of the living conditions of all people.”(Marcos)
“Still under the Franco regime, a clandestine meeting took place, addressing various democratic issues, including mental health. At that weekend meeting, three people met and got to know each other through me, who were Miguel [pseudonym], Jesús [pseudonym] from the Basque Country, and Isabel [pseudonym], the doctor who would later establish the Family Planning Centre for women in conjunction with the La Verneda-Sant Martí Adult School.”(Marcos)
“We (Marcos, Andrés and Jesús) were inseparable friends since we were eight years old. Andrés, is a psychiatrist who has been responsible for child psychiatry at the National Health Service in the entire province of Bizkaia for years. He kept in touch, he was very attentive to dialogic psychiatry in Finland, sending me publications and materials, and used to say, ‘Hey, they’re doing what you said should also be done, in psychiatry.’ So, we’ve kept in touch. And in fact, together with Andrés, we’ve always had the idea of doing it in the Basque Country.”(Marcos)
“We did not follow up with participants to see whether or not they went to a psychiatrist; we did not do that. Some explained it, and if someone did not, we did not know and did not ask them. Holding respect for each person to explain whatever they wanted.”(Julia)
3.3. Types of Dialogues That Generate Social Impact on Mental Health
“In that context there was a fight in psychoanalysis between the most orthodox Freudians and the Lacanians, and there was quite a lot of controversy about mental health conceptions. The SDMH model within La Verneda-Sant Martí Adult School was not aimed to subscribe to one theoretical school of thought or another, but to analyse dialogues and investigate the characteristics that made them successful in improving mental health issues.”(Marcos)
“I don’t know if they knew about specific health problems because, to me, they were all the same; they weren’t labelled (…) They did not feel they were treated as ‘poor thing, they have this’, but rather as just one more among the others.”(Julia)
“The key, or what I have observed from different participants based on what they have told me, is ultimately the ‘dialogic learning’. Because when each one told me how important it was for them, they were describing almost a different principle of dialogic learning. For example, one mentioned the importance of meaning, of having something to get up for, because for her, volunteering made a lot of meaning. Or, for another, the topic of dialogue and being able to talk to other people and express what she was feeling was very important. For another, it was extremely important to be able to learn something she had never learned in her entire life, which was to read and write. For another, it was that people accepted her as she was, which is what we call equality of differences, etc. So, the fact that the school was based on dialogic learning was what also brought about this transformation in them and gave them a reason to get up every morning, because many of them said that they didn’t feel like getting up in the morning, and having a space like the school made them want to. And that saves lives.”(Raquel)
“What is specific to this school that you would not find elsewhere is the principles of dialogic learning. Meaning, transformation… these seven principles are like a whole, the dialogic, that it is dialogic and not just talking for the sake of talking (…) here there is real dialogue, you take an interest in the person, you ask them questions, and people know that it is totally genuine because you really mean it and it is not because you are paying someone, but because it is a source of feeling, of truth, and it is free.”(Raquel)
“In specific cases, there were girls who had been victims of trafficking, people with neurodiversities, people with autism, schizophrenia, etc. Sometimes we coordinated with other entities and sometimes we didn’t. In other words, you could detect a specific case and maybe that person had schizophrenia, but you didn’t call it schizophrenia, first because you didn’t know, and second because you didn’t have to know. At the school, we have always tried to treat each person in the best way possible for them; we didn’t need a label (…) And how do you find out what they need? Through dialogue. Taking each person into account, encouraging those who speak less to speak more, ensuring they can speak, that they have their space, etc. And all of that is part of working on the whole issue of mental health.”(Raquel)
“At one point, we had more than 100 cases in specific cases. Then one day I asked one of them, ‘But why do you come here from so far away?’ And it really stuck with me, because she said, ‘Because here they treat us like people.’ That really stuck with me.”(Julia)
“In class, mental health was always taken into account through dialogue, mutual respect, and also, I believe, through the interrelationships between friends, such as if one was feeling unwell, another would call her, etc. We didn’t call it a health programme, but it was already happening. It was happening through attendance, relationships, dialogue, providing a much better life, having friends, a good atmosphere, parties, etc. These things also improved the problem of loneliness.”(Julia)
“A lady who had Alzheimer’s and didn’t have a place in a day centre came to the new readers’ class and other classes, and the school adapted, not only in terms of dialoguing and creating meaning, making friends and discussing topics, but also in terms of welcoming everyone, all her needs.”(Raquel)
“My experience is that it happens in any space (at school), because ultimately, the school is imbued with dialogic learning in all areas. (…) are activities that bring them to life because they are imbued with dialogic learning. Also in dialogic gatherings, of course, I think that’s where it happens most, but in literacy classes I have also found people who have experienced this process of transformation (…) this space of freedom.”(Raquel)
3.4. Dialogic Literary Gatherings (DLGs) as a Successful Action in the SDMH Model
“In the very first DLG, there were already two people with serious mental health problems. And the very fact that they were listened to, even by people with university degrees, in this case professionals, because the participants did not hold any academic degrees, the fact that they were taken seriously and listened to what they had to say, was a point of self-esteem that helped them. We never suggested that this was going to solve their mental health problems. In other words, it was a valuable aid to them, but it needed to be supplemented by professional psychiatric care. DLG was never intended as an alternative to psychiatry or as an opposition to mental health institutions. On the contrary, it was always intended as complementary and, moreover, in dialogue with those institutions. In fact, we never suggested that ‘medical intervention’ in the sense of medication or other interventions should be stopped.”(Marcos)
“Regarding the dialogic gatherings, during a school session, a woman explained in front of everyone, and there were many of us, how badly she had been, and how she participated in the dialogic gatherings, and how she improved. She was one of the pioneers who later brought dialogic gatherings to the healthcare centre.”(Julia)
“As part of this project, DLG were implemented in health centres in four different countries: a residence for people with mental health problems in Greece, a centre for people with mental health problems in Romania, some of them with psychotic disorders, a primary care centre in Spain, and an NGO working with adults with mental health problems in the Netherlands. People from these countries were trained and then moderated DLG in these institutions. An online course was also created, which is still open and continues to train more people in more contexts to implement DLG.”(Erin)
“In these DLG with mental health patients, we have read books by Saramago, Federico Garcia Lorca, and we have dialogued Kafka’s The Metamorphosis. Romeo and Juliet, among others, has also been read.”(Erin)
“There were two issues here: one was that they [psychiatrists and doctors] saw that it was beneficial and helped their mental health patients with their medical treatment. Also, in many cases, when the therapy they were receiving was private, it was because they were people who did not have the resources to pay for it, so the aim was to reduce the cost as much as possible. One way therapists could reduce the cost for these individuals was to complement their work with ours, which was provided free of charge to the patients. We did this for five years, from 1978 to 1982.”(Marcos)
“On the final conference of this project, when we shared the mental health results of these DLG, some participants shared the positive impacts these DLG had had on themselves, highlighting the creation of friendships and support networks, increased self-esteem, increased respect and solidarity, and increased autonomy.”(Erin)
“There was also a health centre director, someone who was working at the public health agency and her boss, and they explained the impacts they had seen on health and that they believed this should be expanded. They appreciated that we provided scientific evidence and also the voices of participants on the impact that DLG has on them. In fact, we had meetings because they wanted to provide training in different health centres so that DLG could be implemented and psychologists or social workers could be trained to do so.”(Erin)
3.5. Clarifying Errors
“Montse and Nuria were trained in the SDMH model by its co-founder Marcos and implemented it very well when following exactly the scientific bases of the model, always with the guidance of the founder. Later, both wrote that they had created a dialogic approach to ‘psychiatric rehabilitation’, attributing this name to the excellent results obtained by the SDMH model, which never presented itself as psychiatric. To practice psychiatry, it is compulsory to first hold a university degree in medicine, and neither the founders of SDMH nor those two academics hold a degree in medicine. This model [SDMH] conducts a social dialogic collaboration with psychiatry for the overcoming of mental health issues, but only psychiatry decides the treatments, and only psychiatrists do psychiatry.”(Raquel)
“This meeting was held in a famous Café on 19th June 2015 at 17.30 h. Montse said that she was delighted and expressed to what extent Andres appreciated Marcos. (…). Later in 2016, on the 3rd of November, Marcos and Montse agreed to submit a project on mental health with Andres to the official call for research proposals, focused on the implementation of DLGs. On the 14th of July 2017, they commented that the proposal was not considered for evaluation due to an involuntary formal mistake not related to its content. Montse clarified that her head of the research group was worrying a lot for this mistake.”(Olivia)
“Marcos and Montse planned to do a research on mental health in collaboration with the work and contract of one doctoral student who would like to take this focus on a dissertation. The first candidate for doing this work had another professional plan. Then a clinical psychology student [Nuria] wanted to apply for a predoctoral contract and Marcos proposed to Montse to tell Nuria whether she would like to do it. Nuria accepted enthusiastically and seriously followed a profound and long training on the scientific bases of the SDMH model. Later, she was in charge of the training of professionals of an excellent institution for mental health patients. The institution published the details of this training, all of them based on the concepts and practices created by the founders of the SDMH. Then, the DLG were followed by 25 patients reading and dialoguing about the book The Metamorphosis by Kafka. After the difficult acceptance of her research group first (including Nuria herself), and the professionals later, to begin with this book, when they saw the positive results, all of them were extraordinarily satisfied.”(Olivia)
“From the adult school, it was understood that any intervention related to mental health attempting to present it as from psychiatry would have been an intrusion and completely reckless. Professionals and participants in La Verneda-Sant Martí School never accepted it being called dialogic psychiatry.”(Julia)
“We always approached it as a dialogic model of mental health. What was the focus of the dialogic model? Because there have been many dialogues in mental health. The goal was to ensure that the dialogues established were not predetermined by philosophies, ideologies, or specific concepts. Instead, they were established based on scientific criteria that we later came to refer to as social impact. In other words, those types of dialogues that were shown to best overcome mental health problems.”(Marcos)
“They have made the mistake of claiming to have created a model of dialogic psychiatry but this is not accurate. This is something they have said, and from our perspective, it is not the case. Dialogic psychiatry is practised by authorized professionals of psychiatry, our collaboration with them is only providing dialogues which are very successful in mental health, like the DLG and others.”(Marcos)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wynter, R.; Smith, L. Introduction: Historical contexts to communicating mental health. Med. Humanit. 2017, 43, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Uscamayta Ayvar, M.J.; Sanchez Garrafa, R.; Escobar, J.I.; de Erausquin, G.A. The Concept of Mania in Traditional Andean Culture. Am. J. Psychiatry 2019, 176, 338–340. [Google Scholar] [CrossRef]
- Kendler, K.S. From many to one to many—The search for causes of psychiatric illness. JAMA Psychiatry 2019, 76, 1085–1091. [Google Scholar] [CrossRef] [PubMed]
- Breuer, J.; Freud, S. Studies on Hysteria; Standard Edition; Strachey, J., Translator; Hogarth Press: London, UK, 1955; Volume 2. [Google Scholar]
- Directorate-General for Research and Innovation. Monitoring the Impact of EU Framework Programmes: Expert Report; Publications Office of the European Union: Luxembourg, 2018; ISBN 9789279934711. [Google Scholar]
- Flecha, R. The Dialogic Society: The Sociology Scientists and Citizens Like and Use; Hipatia Press: London, UK, 2022; Available online: https://hipatiapress.com/index/en/2022/12/04/the-dialogic-society-2/ (accessed on 15 March 2025).
- Lebron, A.; Valls, R.; Flecha, R. Successful Dialogues in Mental Health (SDMH). [Internet]. 1979. Available online: https://archive.org/details/successful-dialogs-in-mental-health (accessed on 10 March 2025).
- Lebron, A.; Valls, R.; Flecha, R. Dialogic Gatherings in Mental Health (DGMH). 1979. Available online: https://archive.org/details/dialogic-gatherings-in-mental-health (accessed on 10 March 2025).
- Padrós-Cuxart, M.; Crespo-López, A.; Lopez de Aguileta, G.; Jarque-Mur, C. Impact on mental health and well-being of the Dialogic Literary Gathering among women in a primary healthcare centre. Int. J. Qual. Stud. Health Well-Being 2024, 19, 2370901. [Google Scholar] [CrossRef] [PubMed]
- Zubiri-Esnaola, H.; Racionero-Plaza, S.; Fernández-Villardón, A.; Carbonell, S. “It was very liberating”: Dialogic literary gatherings supporting mental health literacy. Community Ment. Health J. 2023, 59, 869–880. [Google Scholar] [CrossRef]
- Flecha, R.; Soler, M. Communicative methodology: Successful actions and dialogic democracy. Curr. Sociol. 2014, 62, 232–242. [Google Scholar] [CrossRef]
- Puigvert, L. Preventive socialization of gender violence: Moving forward using the communicative methodology of research. Qual. Inq. 2014, 20, 839–843. [Google Scholar] [CrossRef]
- Flecha, R. Sharing Words: Theory and Practice of Dialogic Learning; Rowman & Littlefield: Lanham, ML, USA, 2000. [Google Scholar]
- Aroca, M.S. Voices inside schools—La Verneda-Sant Martí: A school where people dare to dream. Harv. Educ. Rev. 1999, 69, 320–336. [Google Scholar] [CrossRef]
- Flecha, R. Successful Educational Actions for Inclusion and Social Cohesion in Europe; Springer: Cham, Switzerland, 2014. [Google Scholar] [CrossRef]
- Ruiz-Eugenio, L.; Soler-Gallart, M.; Racionero-Plaza, S.; Padrós, M. Dialogic literary gatherings: A systematic review of evidence to overcome social and educational inequalities. Educ. Res. Rev. 2023, 39, 100534. [Google Scholar] [CrossRef]
- López de Aguileta, A.; Salceda, M.; Girbés-Peco, S.; Peña-Axt, J.C.; Soler-Gallart, M. Democratizing Taste on Classical Music for All. Qual. Res. Educ. 2023, 12, 236–251. [Google Scholar] [CrossRef]
- Puigvert, L. Female University Students Respond to Gender Violence through Dialogic Feminist Gatherings. Int. Multidiscip. J. Soc. Sci. 2016, 5, 183. [Google Scholar] [CrossRef]
- Olabarria, A.; Zubiri-Esnaola, H.; Santiago-Garabieta, M.; Álvarez-Guerrero, G. Dialogic Pedagogical Gatherings to Foster Pre-Service Teachers Self-Efficacy in Addressing School Violence. Multidiscip. J. Educ. Res. 2025, 15, 22–42. [Google Scholar] [CrossRef]
- Ministerio de Sanidad y Consumo (Spain). Mental Health Strategy of the National Health System; Strategy approved by the Interterritorial Council of the National Health System on December 11, 2006; Ministerio de Sanidad y Consumo: Madrid, Spain, 2007. Available online: https://www.sanidad.gob.es/areas/calidadAsistencial/estrategias/saludMental/docs/ESTRATEGIA_SALUD_MENTAL_SNS_PAG_WEB.pdf (accessed on 15 March 2025).
- Cin, A.D.; de Mesones, J.; Tizón, J. La Mina District of Barcelona. Cities 1995, 12, 87–95. [Google Scholar] [CrossRef]
- Stanwell-Smith, R. Mad, bad and dangerous to know? History and mental health. Perspect. Public Health 2019, 139, 110. [Google Scholar] [CrossRef] [PubMed]
- Szmukler, G. Involuntary Detention and Treatment: Are We Edging toward a “Paradigm Shift”? Schizophr. Bull. 2020, 46, 231–235. [Google Scholar] [CrossRef]
- Malla, A.; Joober, R.; Garcia, A. “Mental illness is like any other medical illness”: A critical examination of the statement and its impact on patient care and society. J. Psychiatry Neurosci. 2015, 40, 147–150. [Google Scholar] [CrossRef]
- Cooper, D. (Ed.) Psychiatry and Anti-Psychiatry, 1st ed.; Routledge: London, UK, 2013; ISBN 9781136438455. [Google Scholar]
- Seikkula, J. Psykoosi—Psyykenlääkkeet—Psykologia. Psykologia 1984, 19, 102–107. [Google Scholar]
- Seikkula, J. From Monologue to Dialogue in Consultation with Larger Systems. Hum. Syst. 1995, 6, 21–42. [Google Scholar]
- Florence, A.C. A abordagem Open Dialogue: História, princípios e evidências/The Open Dialogue approach: History, principles and evidence. Rev. Polis Psique 2018, 8, 191. [Google Scholar] [CrossRef]
- Bergström, T.; Seikkula, J.; Alakare, B.; Mäki, P.; Köngäs-Saviaro, P.; Taskila, J.J.; Tolvanen, A.; Aaltonen, J. The Family-Oriented Open Dialogue Approach in the Treatment of First-Episode Psychosis: Nineteen-Year Outcomes. Psychiatry Res. 2018, 270, 168–175. [Google Scholar] [CrossRef]
- Valtanen, K. The Psychiatrist’s Role in Implementing an Open Dialogue Model of Care. Aust. N. Z. J. Fam. Ther. 2019, 40, 319–329. [Google Scholar] [CrossRef]
- Seikkula, J.; Alakare, B.; Aaltonen, J. Open dialogue in psychosis I: An introduction and case illustration. J. Constr. Psychol. 2001, 14, 247–265. [Google Scholar] [CrossRef]
- Dialogic Minds. Dialogic Minds: Transferring Dialogic Literary Gatherings to Mental Health Across Europe (Erasmus + Project No. 2020-1-ES01-KA204-083054). 2020–2023. Available online: https://www.dialogicminds.eu/project-outputs/ (accessed on 20 March 2025).
- United Nations Universal Declaration of Human Rights|United Nations. Available online: http://legal.un.org/avl/pdf/ha/udhr/udhr_e.pdf (accessed on 20 March 2025).
- Crespo-López, A.; Valls-Carol, R.; Giner-Gota, E. The co-creation and implementation of a protocol for the prevention of gender violence in a non-university adult educational center. Behav. Sci. 2025, 15, 406. [Google Scholar] [CrossRef]
- Flecha, A.; García, R.; Rudd, R. Using Health Literacy in School to Overcome Inequalities. Eur. J. Educ. 2011, 46, 209–218. [Google Scholar] [CrossRef]
| Pseudonym | Gender | Age Range | Profile |
|---|---|---|---|
| Julia | Woman | 70–75 | Educator at La Verneda-Sant Martí Adult School since 1979 and co-founder of ‘Successful Dialogues in Mental Health’ model. |
| Marcos | Man | 70–75 | Founder of La Verneda-Sant Martí Adult School and co-founder of ‘Successful Dialogues in Mental Health’ model. |
| Raquel | Woman | 40–45 | Educator at La Verneda-Sant Martí Adult School since January 2006. |
| Olivia | Woman | 25–30 | Educator at La Verneda-Sant Martí Adult School since 2021. |
| Erin | Woman | 30–35 | Coordinator of the Erasmus Project Dialogic Minds. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soler-Gallart, M.; Crespo-López, A.; López de Aguileta, G.; Ramis-Salas, M.; Oliver, E. The Historical Development of the Successful Dialogues in Mental Health Model. Healthcare 2025, 13, 1696. https://doi.org/10.3390/healthcare13141696
Soler-Gallart M, Crespo-López A, López de Aguileta G, Ramis-Salas M, Oliver E. The Historical Development of the Successful Dialogues in Mental Health Model. Healthcare. 2025; 13(14):1696. https://doi.org/10.3390/healthcare13141696
Chicago/Turabian StyleSoler-Gallart, Marta, Alba Crespo-López, Garazi López de Aguileta, Mimar Ramis-Salas, and Esther Oliver. 2025. "The Historical Development of the Successful Dialogues in Mental Health Model" Healthcare 13, no. 14: 1696. https://doi.org/10.3390/healthcare13141696
APA StyleSoler-Gallart, M., Crespo-López, A., López de Aguileta, G., Ramis-Salas, M., & Oliver, E. (2025). The Historical Development of the Successful Dialogues in Mental Health Model. Healthcare, 13(14), 1696. https://doi.org/10.3390/healthcare13141696







