Beyond COVID-19 Infection: Cognitive and Emotional Pathways Between Posttraumatic Stress, Rumination, and Quality of Life in Hospitalized Patients
Abstract
1. Introduction
2. Methods
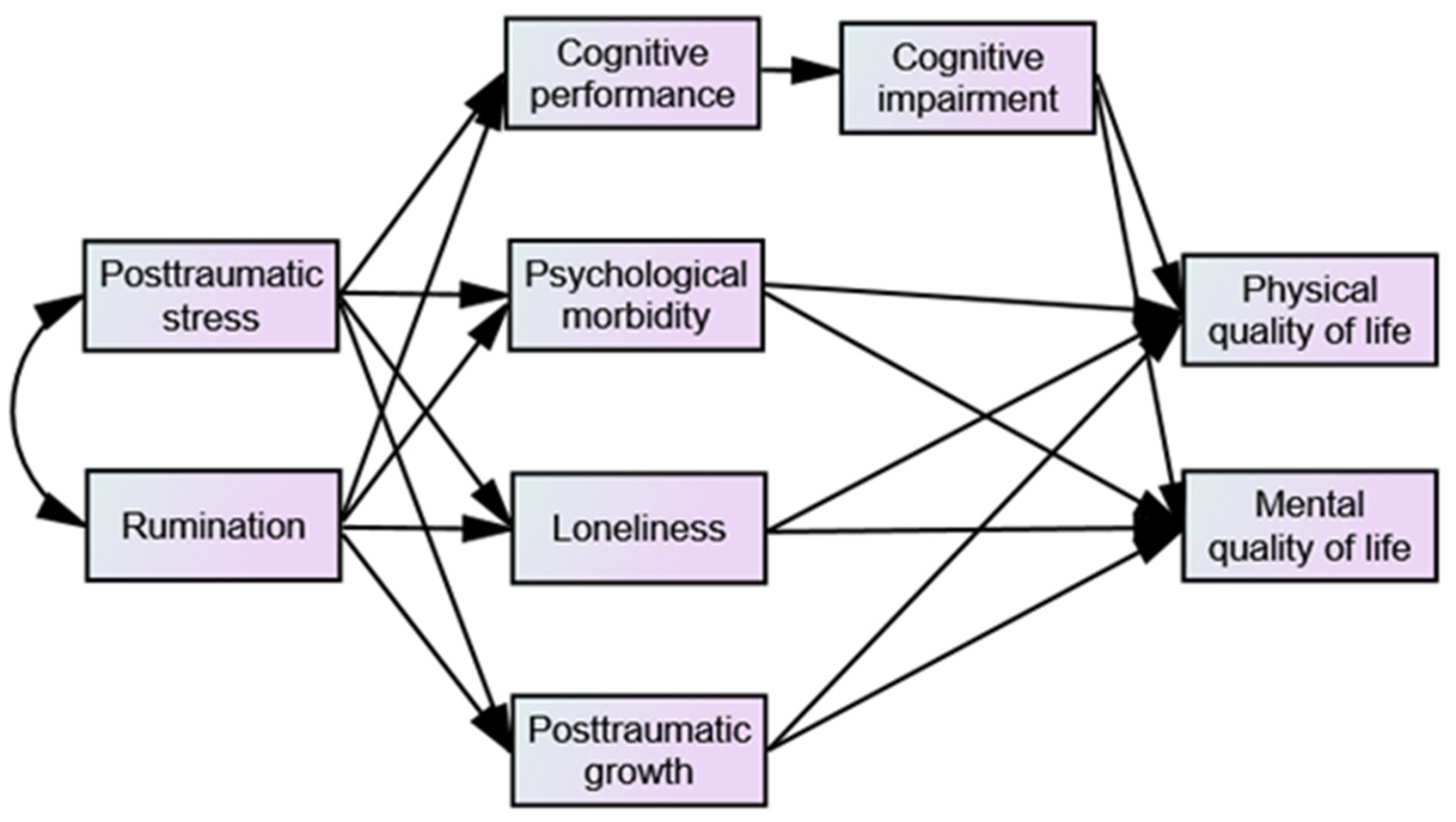
2.1. Conceptual Model
2.2. Study Design and Participants
2.3. Measures
2.4. Data Analysis
2.5. Sample Size
3. Results
3.1. Sample Characteristics
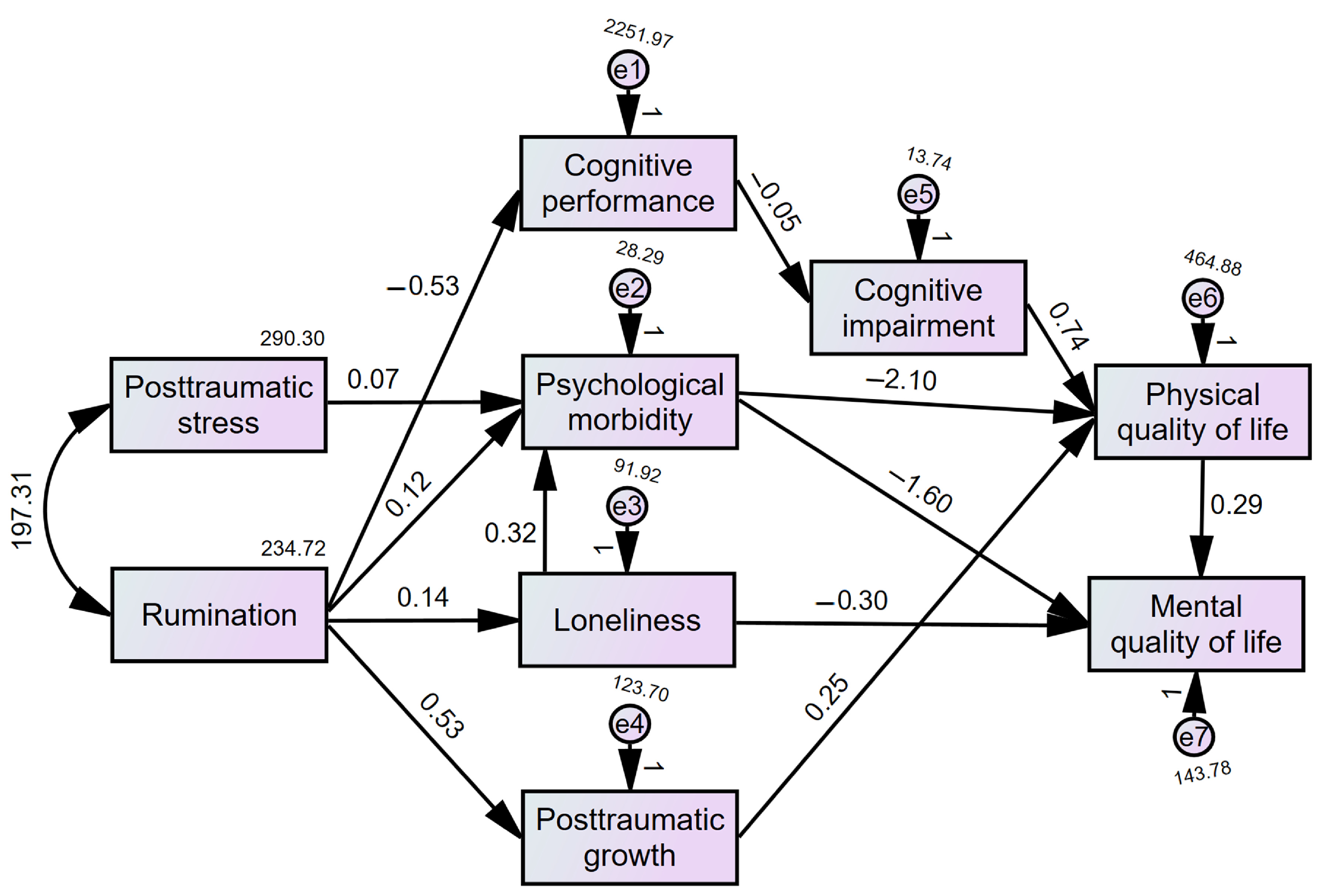
3.2. Path Analysis Model
3.3. The Moderating Role of Sex, Time Since Discharge, and ICU Admission
4. Discussion
Limitations and Future Studies
5. Conclusions and Implications
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mallah, S.I.; Ghorab, O.K.; Al-Salmi, S.; Abdellatif, O.S.; Tharmaratnam, T.; Iskandar, M.A.; Sefen, J.A.N.; Sidhu, P.; Atallah, B.; El-Lababidi, R.; et al. COVID-19: Breaking down a global health crisis. Ann. Clin. Microbiol. Antimicrob. 2021, 20, 35. [Google Scholar] [CrossRef]
- Worldometer. COVID-19 Coronavirus Pandemic: Portugal. Available online: https://www.worldometers.info/coronavirus/country/portugal/ (accessed on 13 April 2024).
- Ferreira, D.C.; Marques, R.C.; Nunes, A.M. The Portuguese Public Hospitals Performance Evolution before and during the SARS-CoV-2 Pandemic (2017–2022). Sustainability 2023, 15, 11572. [Google Scholar] [CrossRef]
- Medical Xpress. Portugal’s COVID-19 Crisis Slams Hospitals. 3 February 2021. Available online: https://medicalxpress.com/news/2021-02-portugal-covid-slams-hospitals.html (accessed on 13 April 2024).
- Horesh, D.; Brown, A.D. Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychol. Trauma 2020, 12, 331–335. [Google Scholar] [CrossRef]
- Kaubisch, L.T.; Reck, C.; von Tettenborn, A.; Woll, C.F.J. The COVID-19 pandemic as a traumatic event and the associated psychological impact on families—A systematic review. J. Affect. Disord. 2022, 319, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef]
- Kira, I.A.; Shuwiekh, H.A.M.; Ashby, J.S.; Elwakeel, S.A.; Alhuwailah, A.; Sous, M.S.F.; Baali, S.B.A.; Azdaou, C.; Oliemat, E.M.; Jamil, H.J. The Impact of COVID-19 Traumatic Stressors on Mental Health: Is COVID-19 a New Trauma Type. Int. J. Ment. Health Addict. 2023, 21, 51–70. [Google Scholar] [CrossRef] [PubMed]
- Husky, M.M.; Pietrzak, R.H.; Marx, B.P.; Mazure, C.M. Research on Posttraumatic Stress Disorder in the Context of the COVID-19 Pandemic: A Review of Methods and Implications in General Population Samples. Chronic Stress 2021, 5, 24705470211051327. [Google Scholar] [CrossRef]
- COVID-19 Mental Disorders Collaborators. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet 2021, 398, 1700–1712. [Google Scholar] [CrossRef]
- Chen, Y.; Huang, X.; Zhang, C.; An, Y.; Liang, Y.; Yang, Y.; Liu, Z. Prevalence and predictors of posttraumatic stress disorder, depression, and anxiety among hospitalized patients with coronavirus disease 2019 in China. BMC Psychiatry 2021, 21, 80. [Google Scholar] [CrossRef]
- Lovik, A.; González-Hijón, J.; Kähler, A.K.; Valdimarsdóttir, U.A.; Frans, E.M.; Magnusson, P.K.E.; Pedersen, N.L.; Hall, P.; Czene, K.; Sullivan, P.F.; et al. Mental health indicators in Sweden over a 12-month period during the COVID-19 pandemic—Baseline data of the Omtanke2020 Study. J. Affect. Disord. 2023, 322, 108–117. [Google Scholar] [CrossRef]
- Hussain, N.; Samuelsson, C.M.; Drummond, A.; Persson, C.U. Prevalence of symptoms of anxiety and depression one year after intensive care unit admission for COVID-19. BMC Psychiatry 2024, 24, 170. [Google Scholar] [CrossRef]
- Nagarajan, R.; Krishnamoorthy, Y.; Basavarachar, V.; Dakshinamoorthy, R. Prevalence of post-traumatic stress disorder among survivors of severe COVID-19 infections: A systematic review and meta-analysis. J. Affect. Disord. 2022, 299, 52–59. [Google Scholar] [CrossRef]
- Becerra-Canales, B.; Campos-Martínez, H.M.; Campos-Sobrino, M.; Aquije-Cárdenas, G.A. Trastorno de estrés postraumático y calidad de vida del paciente post-COVID-19 en Atención Primaria [Post-traumatic stress and QoL of post-COVID-19 patients in primary care]. Aten. Primaria 2022, 54, 102460. [Google Scholar] [CrossRef] [PubMed]
- Egger, M.; Wimmer, C.; Stummer, S.; Reitelbach, J.; Bergmann, J.; Müller, F.; Jahn, K. Reduced health-related QoL, fatigue, anxiety and depression affect COVID-19 patients in the long-term after chronic critical illness. Sci. Rep. 2024, 14, 3016. [Google Scholar] [CrossRef]
- Juczyński, Z.; Kwiecińska, L.; Ogińska-Bulik, J. Ruminations as predictors of post-traumatic stress disorder after hospitalization for COVID-19. Ruminacje jako wyznaczniki zespołu stresu pourazowego po hospitalizacji z powodu COVID-19. Psychiatr. Pol. 2023, 57, 1011–1022. [Google Scholar] [CrossRef]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of Uncertainty and Mental Wellbeing: Serial Mediation by Rumination and Fear of COVID-19. Int. J. Ment. Health Addict. 2022, 20, 2731–2742. [Google Scholar] [CrossRef] [PubMed]
- Kang, H.S.; Kim, B.N. The Role of Event-Related Rumination and Perceived Social Support on Psychological Distress during the COVID-19 Pandemic: Results from Greater Daegu Region in South Korea. Psychiatry Investig. 2021, 18, 392–399. [Google Scholar] [CrossRef]
- Tedeschi, R.G.; Shakespeare-Finch, J.; Taku, K.; Calhoun, L.G. Posttraumatic Growth: Theory, Research, and Applications; Routledge: New York, NY, USA, 2018. [Google Scholar]
- Bovero, A.; Balzani, S.; Tormen, G.; Malandrone, F.; Carletto, S. Factors Associated with Post-Traumatic Growth during the COVID-19 Pandemic: A Systematic Review. J. Clin. Med. 2023, 13, 95. [Google Scholar] [CrossRef]
- Adjorlolo, S.; Adjorlolo, P.; Andoh-Arthur, J.; Ahiable, E.K.; Kretchy, I.A.; Osafo, J. Post-Traumatic Growth and Resilience among Hospitalized COVID-19 Survivors: A Gendered Analysis. Int. J. Environ. Res. Public Health 2022, 19, 10014. [Google Scholar] [CrossRef]
- Pietrzak, R.H.; Tsai, J.; Southwick, S.M. Association of Symptoms of Posttraumatic Stress Disorder with Posttraumatic Psychological Growth Among US Veterans During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e214972. [Google Scholar] [CrossRef]
- Wu, X.; Kaminga, A.C.; Dai, W.; Deng, J.; Wang, Z.; Pan, X.; Liu, A. The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. J. Affect. Disord. 2019, 243, 408–415. [Google Scholar] [CrossRef] [PubMed]
- Ernst, M.; Niederer, D.; Werner, A.M.; Czaja, S.J.; Mikton, C.; Ong, A.D.; Rosen, T.; Brähler, E.; Beutel, M.E. Loneliness before and during the COVID-19 pandemic: A systematic review with meta-analysis. Am. Psychol. 2022, 77, 660–677. [Google Scholar] [CrossRef] [PubMed]
- Sankaran, S. The Loneliness Epidemic and How It Affects Hospitalized Patients. In Health Equity in Hospital Medicine; Sankaran, S., Ed.; Springer Nature: Heidelberg, Germany, 2023; pp. 113–117. [Google Scholar] [CrossRef]
- Madden, R.; Ahmed, R.; Cloonan, J.; May, E.; Chambers, H.; Briggs, R. 347 Loneliness Amonst Older Inpatients in the Context of COVID-Related Visiting Restrictions. Age Ageing 2022, 51, afac218.304. [Google Scholar] [CrossRef]
- Sipowicz, K.; Pietras, T.; Mosiołek, A.; Sobstyl, M.; Ring, M.; Kamecki, K.; Stefańczyk, I.; Kosmalski, M. The sense of loneliness and meaning in life in post-COVID convalescents—A preliminary study. Front. Psychiatry 2023, 14, 1296385. [Google Scholar] [CrossRef]
- Hawkley, L.C. Loneliness and health. Nat. Rev. Dis. Primers 2022, 8, 22. [Google Scholar] [CrossRef]
- Crivelli, L.; Palmer, K.; Calandri, I.; Guekht, A.; Beghi, E.; Carroll, W.; Frontera, J.; García-Azorín, D.; Westenberg, E.; Winkler, A.S.; et al. Changes in cognitive functioning after COVID-19: A systematic review and meta-analysis. Alzheimer’s Dement. 2022, 18, 1047–1066. [Google Scholar] [CrossRef]
- Vasilevskaya, A.; Mushtaque, A.; Tsang, M.Y.; Alwazan, B.; Herridge, M.; Cheung, A.M.; Tartaglia, M.C. Sex and age affect acute and persisting COVID-19 illness. Sci. Rep. 2023, 13, 6029. [Google Scholar] [CrossRef]
- Jaywant, A.; Vanderlind, W.M.; Alexopoulos, G.S.; Fridman, C.B.; Perlis, R.H.; Gunning, F.M. Frequency and profile of objective cognitive deficits in hospitalized patients recovering from COVID-19. Neuropsychopharmacology 2021, 46, 2235–2240. [Google Scholar] [CrossRef]
- Wood, G.K.; Sargent, B.F.; Ahmad, Z.U.; Tharmaratnam, K.; Dunai, C.; Egbe, F.N.; Martin, N.H.; Facer, B.; Pendered, S.L.; Rogers, H.C.; et al. Posthospitalization COVID-19 cognitive deficits at 1 year are global and associated with elevated brain injury markers and gray matter volume reduction. Nat. Med. 2025, 31, 245–257. [Google Scholar] [CrossRef]
- Ariza, M.; Cano, N.; Segura, B.; Bejar, J.; Barrué, C.; NAUTILUS Project Collaborative Group; Cortés, C.U.; Junqué, C.; Garolera, M. Cognitive and emotional predictors of QoL and functioning after COVID-19. Ann. Clin. Transl. Neurol. 2024, 11, 302–320. [Google Scholar] [CrossRef]
- Szewczyk, W.; Fitzpatrick, A.L.; Fossou, H.; Gentile, N.L.; Sotoodehnia, N.; Vora, S.B.; West, T.E.; Bertolli, J.; Cope, J.R.; Lin, J.S.; et al. Long COVID and recovery from Long COVID: QoL impairments and subjective cognitive decline at a median of 2 years after initial infection. BMC Infect. Dis. 2024, 24, 1241. [Google Scholar] [CrossRef]
- O’Dowd, A. COVID-19: Third of people infected have long term symptoms. BMJ 2021, 373, n1626. [Google Scholar] [CrossRef]
- Scott, S.B.; Graham-Engeland, J.E.; Engeland, C.G.; Smyth, J.M.; Almeida, D.M.; Katz, M.J.; Lipton, R.B.; Mogle, J.A.; Munoz, E.; Ram, N.; et al. The Effects of Stress on Cognitive Aging, Physiology and Emotion (ESCAPE) Project. BMC Psychiatry 2015, 15, 146. [Google Scholar] [CrossRef]
- Lopes, A.; Rocha, J. Convergent Validity of Impact of Event Scale-Revised and Impact of Event Scale-6 Portuguese Versions. Master’s Thesis, Instituto Superior de Ciências da Saúde–Norte (CESPU), Paredes, Portugal, 2013. [Google Scholar]
- Ramos, C.; Figueiras, L.; Lopes, M.; Leal, I.; Tedeschi, R. Inventário de ruminação relacionada com o acontecimento: Qualidades psicométricas na população portuguesa [Event-Related Rumination Inventory: Psychometric Properties on a Portuguese Sample]. Psicol. Saúde Doenças 2015, 16, 299–310. [Google Scholar] [CrossRef]
- Cavaco, S.; Gonçalves, A.; Pinto, C.; Almeida, E.; Gomes, F.; Moreira, I.; Fernandes, J.; Teixeira-Pinto, A. Trail Making Test: Regression-based norms for the portuguese population. Arch. Clin. Neuropsychol. 2013, 28, 189–198. [Google Scholar] [CrossRef]
- Freitas, S.; Simões, M.R.; Martins, C.; Vilar, M.; Santana, I. Estudos de adaptação do Montreal Cognitive Assessment (MoCA) para a população portuguesa [Adaptation studies of the Montreal Cognitive Assessment (MoCA) to the portuguese population]. Aval. Psicol. 2010, 9, 345–357. [Google Scholar]
- Pais-Ribeiro, J.; Silva, I.; Ferreira, T.; Martins, A.; Meneses, R.; Baltar, M. Validation study of a Portuguese version of the Hospital Anxiety and Depression Scale. Psychol. Health Med. 2007, 12, 225–237. [Google Scholar] [CrossRef] [PubMed]
- Carmichael, J.; Spitz, G.; Gould, K.R.; Johnston, L.; Samiotis, A.; Ponsford, J. Bifactor analysis of the Hospital Anxiety and Depression Scale (HADS) in individuals with traumatic brain injury. Sci. Rep. 2023, 13, 8017. [Google Scholar] [CrossRef]
- Gibbons, C.J.; Mills, R.J.; Thornton, E.W.; Ealing, J.; Mitchell, J.D.; Shaw, P.J.; Talbot, K.; Tennant, A.; Young, C.A. Rasch analysis of the hospital anxiety and depression scale (HADS) for use in motor neurone disease. Health Qual. Life Outcomes 2021, 9, 82. [Google Scholar] [CrossRef]
- Faustino, B.; Lopes, P.; Oliveira, J.; Campaioli, G.; Rondinone, M.; Bomfim, H.; Germano, L. Psychometric and Rash Analysis of the UCLA Loneliness Scale-16 in a Portuguese Sample of Older Adults. Psychol. Stud. 2019, 64, 140–146. [Google Scholar] [CrossRef]
- Lamela, D.; Figueiredo, B.; Bastos, A.; Martins, H. Posttraumatic Growth Inventory Short Form-Portuguese Version (Portuguese PTGI-SF, PTGI-SF); [Database Record]; APA PsycTests: Washington, DC, USA, 2013. [Google Scholar] [CrossRef]
- Ferreira, P.L.; Ferreira, L.N.; Pereira, L.N. Medidas sumário física e mental de estado de saúde para a população portuguesa [Physical and mental summary measures of health state for the portuguese population]. Rev. Port. Saúde Pública 2012, 30, 163–171. [Google Scholar]
- Hair, J.F.; Black, W.; Babin, B.; Anderson, R. Multivariate Data Analysis: A Global Perspective; Pearson Education: London, UK, 2020. [Google Scholar]
- Soper, D.S. A-priori Sample Size Calculator for Hierarchical Multiple Regression [Software]. 2019. Available online: http://www.danielsoper.com/statcalc (accessed on 6 January 2025).
- Bertuccelli, M.; Ciringione, L.; Rubega, M.; Bisiacchi, P.; Masiero, S.; Del Felice, A. Cognitive impairment in people with previous COVID-19 infection: A scoping review. Cortex 2022, 154, 212–230. [Google Scholar] [CrossRef]
- Panagea, E.; Messinis, L.; Petri, M.C.; Liampas, I.; Anyfantis, E.; Nasios, G.; Patrikelis, P.; Kosmidis, M. Neurocognitive Impairment in Long COVID: A Systematic Review. Arch. Clin. Neuropsychol. 2025, 40, 125–149. [Google Scholar] [CrossRef]
- Mertens, L.; Tamm, G.; Hoorelbeke, K. Ruminative thinking styles differentially relate to posttraumatic stress versus growth following trauma exposure. Psychol. Trauma 2025. [Google Scholar] [CrossRef]
- Silva, J.; Martins, S.; Ferreira, A.R.; Fernandes, J.; Vieira, T.; Fontes, L.; Reis, N.; Braga, A.; Coimbra, I.; Paiva, J.A.; et al. Depression and health-related quality of life in critical COVID-19 survivors. Eur. Psychiatry 2022, 65, S377. [Google Scholar] [CrossRef]
- Kolakowsky-Hayner, S.A.; Goldin, Y.; Kingsley, K.; Alzueta, E.; Arango-Lasprilla, J.C.; Perrin, P.B.; Baker, F.C.; Ramos-Usuga, D.; Constantinidou, F. Psychosocial Impacts of the COVID-19 Quarantine: A Study of Gender Differences in 59 Countries. Medicina 2021, 57, 789. [Google Scholar] [CrossRef]
- Gorenshtein, A.; Leibovitch, L.; Liba, T.; Stern, S.; Stern, Y. Gender Disparities in Neurological Symptoms of Long COVID: A Systematic Review and Meta-Analysis. Neuroepidemiology 2024, 1–15, advance online publication. [Google Scholar] [CrossRef]
- Wollast, R.; Lüders, A.; Nugier, A.; Guimond, S.; Phillips, J.B.; Sutton, R.M.; Douglas, K.M.; Sengupta, N.K.; Lemay, E.P.; Zand, S.; et al. Gender inequality and cultural values in explaining gender differences in positive and negative emotions: A comparison of 24 countries during the COVID-19 pandemic. Curr. Psychol. 2025, 44, 7584–7602. [Google Scholar] [CrossRef]
- Gough, B.; Novikova, I. Mental Health, Men and Culture: How Do Sociocultural Constructions of Masculinities Relate to Men’s Mental Health Help-Seeking Behaviour in the WHO European Region? WHO Regional Office for Europe: Copenhagen, Denmark, 2020. [Google Scholar]
- Bi, Y.; Xiao, Y.; Pan, X.; Zhang, Y.; Yang, Q.; Hu, L. Long-term post-traumatic stress symptoms in COVID-19 survivors and its risk factors: A two-year longitudinal cohort study. Psychiatry Res. 2023, 329, 115523. [Google Scholar] [CrossRef]
- Taquet, M.; Skorniewska, Z.; De Deyn, T.; Hampshire, A.; Trender, W.R.; Hellyer, P.J.; Chalmers, J.D.; Ho, L.P.; Horsley, A.; Marks, M.; et al. Cognitive and psychiatric symptom trajectories 2-3 years after hospital admission for COVID-19: A longitudinal, prospective cohort study in the UK. Lancet Psychiatry 2024, 11, 696–708. [Google Scholar] [CrossRef]
- Cheetham, N.J.; Penfold, R.; Giunchiglia, V.; Bowyer, V.; Sudre, C.H.; Canas, L.S.; Deng, J.; Murray, B.; Kerfoot, E.; Antonelli, M.; et al. The effects of COVID-19 on cognitive performance in a community-based cohort: A COVID symptom study biobank prospective cohort study. eClinicalMedicine 2023, 62, 102086. [Google Scholar] [CrossRef]
- O’Connor, D.B.; Wilding, S.; Ferguson, E.; Cleare, S.; Wetherall, K.; McClelland, H.; Melson, A.J.; Niedzwiedz, C.; O’Carroll, R.E.; Platt, S.; et al. Effects of COVID-19-related worry and rumination on mental health and loneliness during the pandemic: Longitudinal analyses of adults in the UK COVID-19 mental health & wellbeing study. J. Ment. Health 2023, 32, 1122–1133. [Google Scholar] [CrossRef] [PubMed]
- Ollila, H.; Pihlaja, R.; Koskinen, S.; Tuulio-Henriksson, A.; Salmela, V.; Tiainen, M.; Hokkanen, L.; Hästbacka, J. Long-term cognitive functioning is impaired in ICU-treated COVID-19 patients: A comprehensive controlled neuropsychological study. Crit. Care 2022, 26, 223. [Google Scholar] [CrossRef]
- Pihlaja, R.E.; Kauhanen, L.S.; Ollila, H.S.; Tuulio-Henriksson, A.S.; Koskinen, S.K.; Tiainen, M.; Salmela, V.R.; Hästbacka, J.; Hokkanen, L.S. Associations of subjective and objective cognitive functioning after COVID-19: A six-month follow-up of ICU, ward, and home-isolated patients. Brain Behav. Immun. Health 2023, 27, 100587. [Google Scholar] [CrossRef]
- Schröder, D.; Stölting, A.; Müllenmeister, C.; Behrens, G.M.N.; Klawitter, S.; Klawonn, F.; Cook, A.; Wegner, N.; Wetzke, M.; Schmachtenberg, T.; et al. Improvement in quality of life and cognitive function in Post-COVID syndrome after online occupational therapy: Results from a randomized controlled pilot study. PLoS ONE 2025, 20, e0312714. [Google Scholar] [CrossRef]
| Sociodemographic Variables | Patients | |
|---|---|---|
| n (%)/M ± SD | ||
| Sex | Women | 88 (34.10) |
| Men | 170 (65.90) | |
| Age | 61.41 ± 10.86 | |
| ≤49 | 32 (12.40) | |
| 50–59 | 59 (22.90) | |
| 60–69 | 98 (38.00) | |
| 70–75 | 69 (26.70) | |
| Marital status | Married/non-marital partnership | 162 (62.80) |
| Single/divorced/widowed | 96 (37.20) | |
| Education | ≤Primary education | 101 (39.20) |
| ≤Secondary education | 121 (46.90) | |
| ≤University degree | 36 (13.90) | |
| Professional situation | Employed | 96 (37.20) |
| Unemployed | 24 (9.30) | |
| Retired | 138 (53.50) | |
| Clinical Variables | ||
| Hospitalization main diagnosis | COVID-19 | 194 (75.20) |
| Other | 64 (24.80) | |
| Intensive care unit admission | Yes | 60 (23.30) |
| No | 198 (76.70) | |
| Cohort | I | 120 (46.50) |
| II | 138 (53.50) | |
| Discharge duration (days) | 629.27 (259.33) | |
| Psychological Variables | Min.–Max. | M ± SD |
| Posttraumatic stress (IES-R) | 0.00–82.00 | 13.90 (17.07) |
| Rumination (ERRI) | 0.00–60.00 | 16.54 (15.35) |
| Cognitive performance (TMT-A time) | 26.00–375.00 | 83.81 (48.25) |
| Cognitive impairment (MoCA) | 8.00–29.00 | 20.24 (4.43) |
| Psychological morbidity (HADS) | 0.00–34.00 | 9.38 (7.10) |
| Loneliness (UCLA) | 16.00–63.00 | 24.89 (9.83) |
| Posttraumatic growth (PTGI) | 0.00–50.00 | 17.95 (13.79) |
| Physical QoL (SF-12) | 0.00–100.00 | 58.01 (26.20) |
| Mental QoL (SF-12) | 6.25–100.00 | 68.62 (21.85) |
| Path | b (SE) | Z Value | p | β |
|---|---|---|---|---|
| Posttraumatic stress (IES-R) → Psych. morbidity (HADS) | 0.074 (0.030) | 2.490 | 0.013 | 0.178 |
| Rumination (ERRI) → Cognitive performance (TMT-A) | −0.535 (0.193) | −2.767 | 0.006 | −0.170 |
| Rumination (ERRI) → Psych. morbidity (HADS) | 0.122 (0.033) | 3.651 | <0.001 | 0.263 |
| Rumination (ERRI) → Loneliness (UCLA) | 0.135 (0.039) | 3.464 | <0.001 | 0.211 |
| Rumination (ERRI) → Posttraumatic growth (PTGI) | 0.528 (0.045) | 11.658 | <0.001 | 0.588 |
| Loneliness (UCLA) → Psych. morbidity (HADS) | 0.318 (0.035) | 9.180 | <0.001 | 0.438 |
| Cognitive performance (TMT-A) → Cognitive impairment (MoCA) | −0.050 (0.005) | −10.397 | <0.001 | −0.544 |
| Cognitive impairment (MoCA) → Physical QoL (SF-12) | 0.737 (0.305) | 2.416 | 0.016 | 0.125 |
| Psych. morbidity (HADS) → Physical QoL (SF-12) | −2.095 (0.198) | 10.580 | <0.001 | −0.572 |
| Psych. morbidity (HADS) → Mental QoL (SF-12) | −1.596 (0.140) | −11.418 | <0.001 | −0.519 |
| Loneliness (UCLA) → Mental QoL (SF-12) | −0.300 (0.089) | −3.353 | <0.001 | −0.135 |
| Posttraumatic growth (PTGI) → Physical QoL (SF-12) | 0.248 (0.102) | 2.430 | 0.015 | 0.131 |
| Physical QoL (SF-12) → Mental QoL (SF-12) | 0.293 (0.034) | 8.635 | <0.001 | 0.348 |
| Predictor | Indirect Effect | Outcome | β | CI95% |
|---|---|---|---|---|
| Posttraumatic stress (PTSS) | Psych. morbidity (HADS) | Physical QoL (SF-12) | −0.102 * | [−0.216, −0.003] |
| Posttraumatic stress (PTSS) | Psych. morbidity (HADS) | Mental QoL (SF-12) | −0.128 * | [−0.273, −0.002] |
| Rumination (ERRI) | Loneliness (UCLA) | Psych. morbidity (HADS) | 0.093 *** | [0.040, 0.159] |
| Rumination (ERRI) | Cognitive performance (TMT-A time) | Cognitive impairment (MoCA) | 0.093 *** | [0.046, 0.144] |
| Rumination (ERRI) | Cognitive performance (TMT-A time) → Cognitive impairment (MoCA) [Loneliness (UCLA)→] Psych. morbidity (HADS) | Physical QoL (SF-12) | −0.115 * | [−0.225, −0.012] |
| Rumination (ERRI) | Cognitive performance (TMT-A time) → Cognitive impairment (MoCA) → Physical QoL (SF-12) [Loneliness (UCLA) →] Psych. morbidity → Physical QoL (SF-12) | Mental QoL (SF-12) | −0.253 *** | [−0.359, −0.144] |
| Loneliness (UCLA) | Psych. morbidity (HADS) | Physical QoL (SF-12) | −0.251 *** | [−0.319, −0.187] |
| Loneliness (UCLA) | Psych. morbidity (HADS) | Mental QoL (SF-12) | −0.315 *** | [−0.391, −0.245] |
| Psych. morbidity (HADS) | Physical QoL (SF-12) | Mental QoL (SF-12) | −0.199 *** | [−0.262, −0.147] |
| Cognitive performance (TMT-A time) | Cognitive impairment (MoCA) | Physical QoL (SF-12) | −0.068 * | [−0.128, −0.010] |
| Cognitive performance (TMT-A time) | Cognitive impairment (MoCA) | Mental QoL (SF-12) | −0.024 * | [−0.045, −0.004] |
| Cognitive impairment (MoCA) | Physical QoL (SF-12) | Mental QoL (SF-12) | 0.044 * | [0.007, 0.081] |
| Posttraumatic growth (PTGI) | Physical QoL (SF-12) | Mental QoL (SF-12) | 0.046 * | [0.008, 0.087] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilaça, M.; Carvalho, S.; Leite, J.; Leite, F.; Pereira, M.G. Beyond COVID-19 Infection: Cognitive and Emotional Pathways Between Posttraumatic Stress, Rumination, and Quality of Life in Hospitalized Patients. Healthcare 2025, 13, 1655. https://doi.org/10.3390/healthcare13141655
Vilaça M, Carvalho S, Leite J, Leite F, Pereira MG. Beyond COVID-19 Infection: Cognitive and Emotional Pathways Between Posttraumatic Stress, Rumination, and Quality of Life in Hospitalized Patients. Healthcare. 2025; 13(14):1655. https://doi.org/10.3390/healthcare13141655
Chicago/Turabian StyleVilaça, Margarida, Sandra Carvalho, Jorge Leite, Fernanda Leite, and M. Graça Pereira. 2025. "Beyond COVID-19 Infection: Cognitive and Emotional Pathways Between Posttraumatic Stress, Rumination, and Quality of Life in Hospitalized Patients" Healthcare 13, no. 14: 1655. https://doi.org/10.3390/healthcare13141655
APA StyleVilaça, M., Carvalho, S., Leite, J., Leite, F., & Pereira, M. G. (2025). Beyond COVID-19 Infection: Cognitive and Emotional Pathways Between Posttraumatic Stress, Rumination, and Quality of Life in Hospitalized Patients. Healthcare, 13(14), 1655. https://doi.org/10.3390/healthcare13141655








