The Effectiveness and Safety of Tai Chi on Knee Pain: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Registration
2.2. Data Sources and Searches
2.3. Inclusion/Exclusion
2.3.1. Types of Studies
2.3.2. Participants
2.3.3. Types of Interventions
2.3.4. Types of Comparisons
2.3.5. Types of Outcome Measures
2.4. Study Selection
2.5. Data Extraction
2.6. Assessment of Risk of Bias (ROB)
2.7. Safety Assessment
2.8. Data Analyses
3. Results
3.1. Study Selection and Description
3.2. Participants
3.3. Intervention
3.4. Control Interventions
3.5. Outcomes
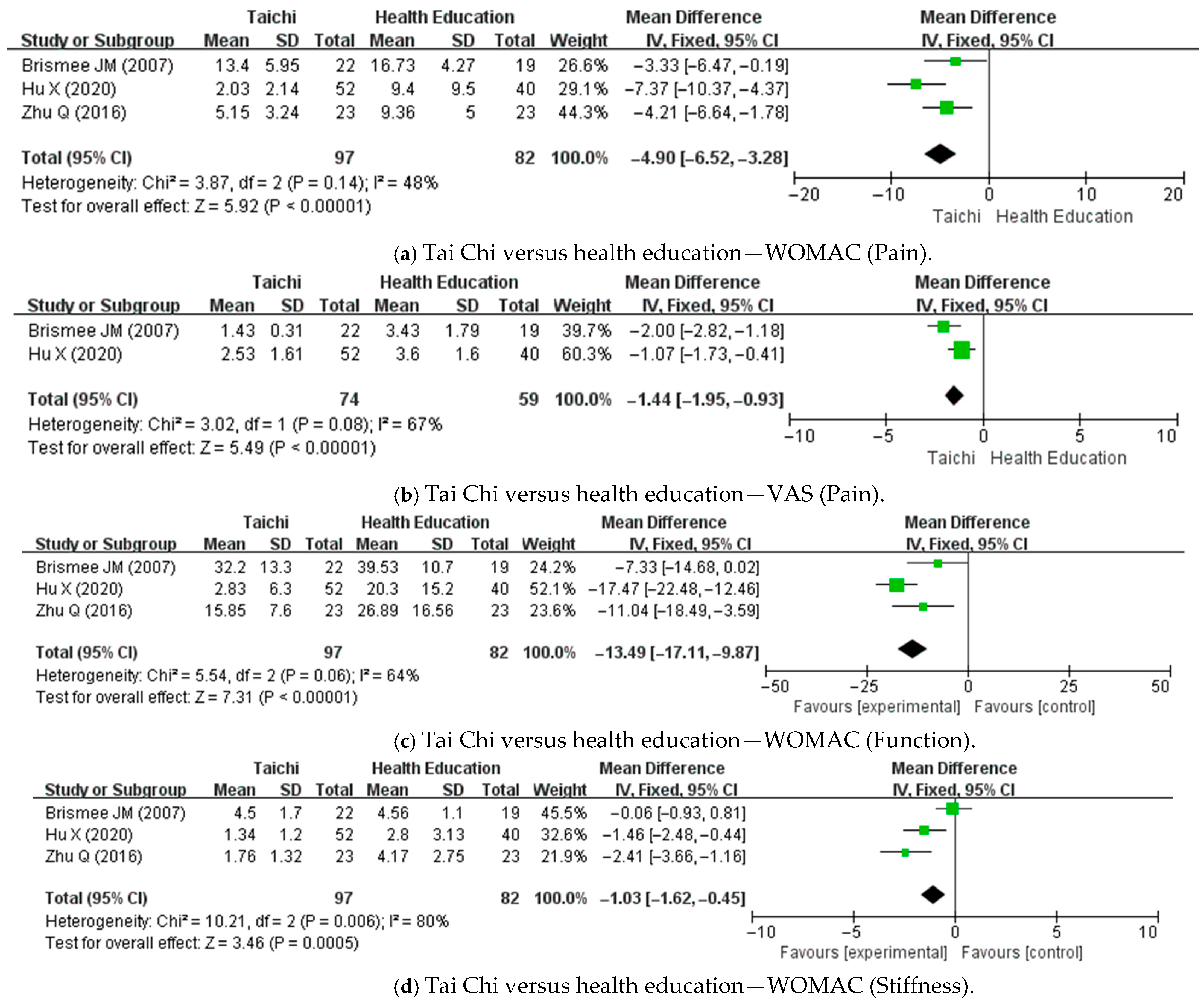
3.5.1. Tai Chi Versus Health Education
3.5.2. Tai Chi Versus No Intervention
3.5.3. Tai Chi Versus Stretching and Health Education
3.5.4. Tai Chi Versus Physical Therapy
3.5.5. Tai Chi Versus Resistance Training
3.6. Safety of Tai Chi
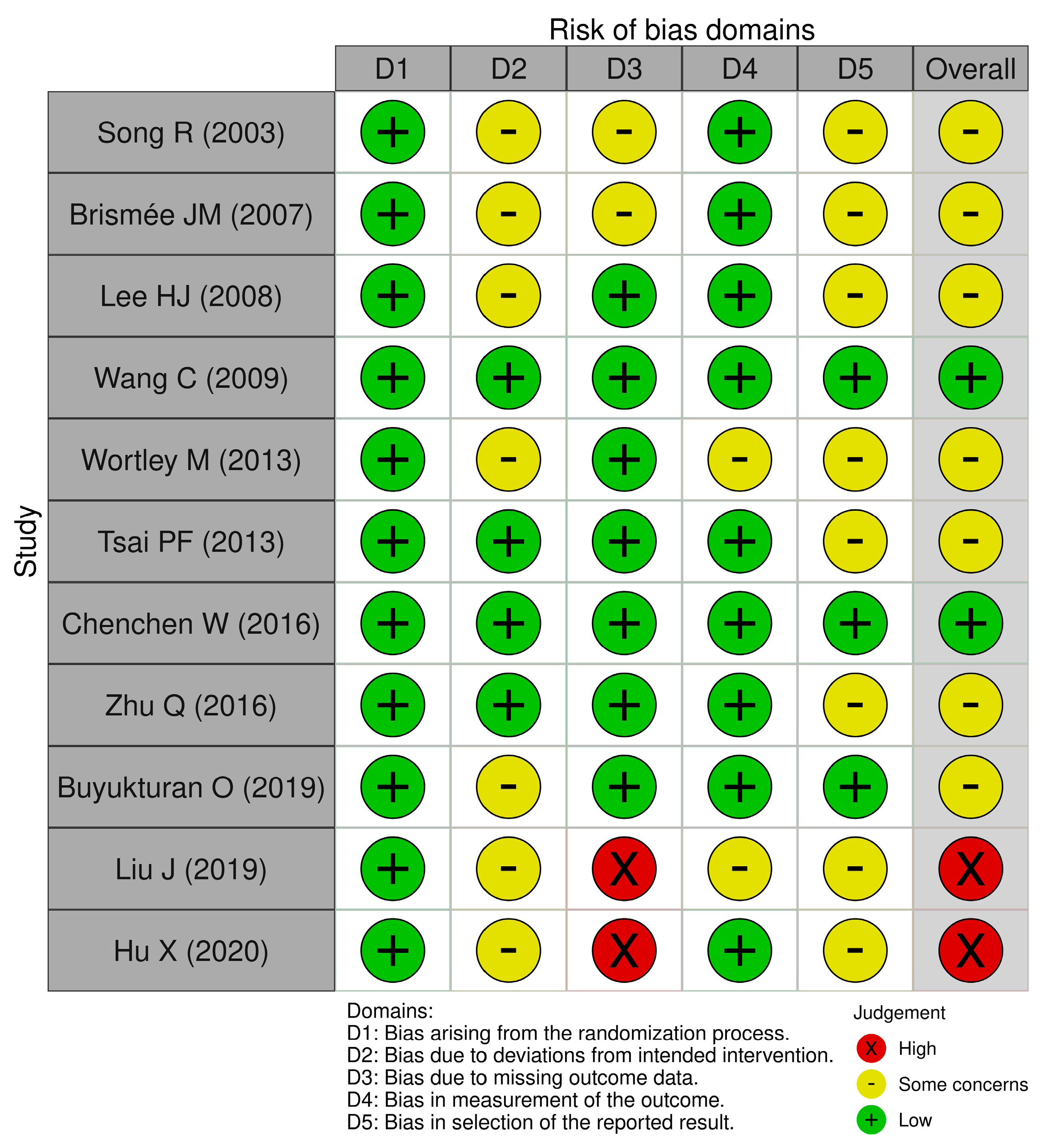
3.7. Assessment for ROB
4. Discussion
4.1. Main Findings
4.2. Limitations of the Review
4.3. Implications for Future Studies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lan, C.; Chen, S.-Y.; Lai, J.-S.; Wong, A.-M.-K. Tai Chi Chuan in medicine and health promotion. Evid. Based Complement. Altern. Med. 2013, 2013, 502131. [Google Scholar] [CrossRef] [PubMed]
- Maisel, E. Tai Chi for Health; Pickle Partners Publishing: Merseyside, UK, 2016; pp. 8–9. [Google Scholar]
- Wen, Z.-H. An interpretation of movement beauty of Chinese martial arts from the perspective of Zhouyi. J. Shenyang Sport Univ. 2019, 38, 128–135. [Google Scholar]
- Yeh, G.Y.; Wang, C.; Wayne, P.M.; Phillips, R.S. The effect of Tai Chi exercise on blood pressure: A systematic review. Prev. Cardiol. 2008, 11, 82–89. [Google Scholar] [CrossRef]
- Kwok, J.C.; Hui-Chan, C.W.; Tsang, W.W. Effects of aging and Tai Chi on finger-pointing toward stationary and moving visual targets. Arch. Phys. Med. Rehabil. 2010, 91, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Ho, R.T.H.; Wan, A.H.Y.; Au-Yeung, F.S.W.; Lo, P.H.Y.; Siu, P.J.C.Y.; Wong, C.P.K.; Ng, W.Y.H.; Cheung, I.K.M.; Ng, S.M.; Chan, C.L.W.; et al. The psychophysiological effects of Tai Chi and exercise in residential schizophrenic patients: A three-arm randomized controlled trial. BMC Complement. Altern. Med. 2014, 14, 364. [Google Scholar] [CrossRef] [PubMed]
- Ghandali, E.; Moghadam, S.T.; Hadian, M.R.; Olyaei, G.; Jalaie, S.; Sajjadi, E. The effect of Tai Chi exercises on postural stability and control in older patients with knee osteoarthritis. J. Bodyw. Mov. Ther. 2017, 21, 594–598. [Google Scholar] [CrossRef]
- Winser, S.J.; Tsang, W.W.; Krishnamurthy, K.; Kannan, P. Does Tai Chi improve balance and reduce falls incidence in neurological disorders? A systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 1157–1168. [Google Scholar] [CrossRef]
- Yang, Y.; Wang, Y.; Wang, S.; Shi, P.; Wang, C. The effect of Tai Chi on cardiorespiratory fitness for coronary disease rehabilitation: A systematic review and meta-analysis. Front. Physiol. 2017, 8, 1091. [Google Scholar] [CrossRef]
- Yang, G.-Y.; Sabag, A.; Hao, W.-L.; Zhang, L.-N.; Jia, M.-X.; Dai, N.; Zhang, H.; Ayati, Z.; Cheng, Y.-J.; Zhang, C.-H.; et al. Tai Chi for health and well-being: A bibliometric analysis of published clinical studies between 2010 and 2020. Complement. Ther. Med. 2021, 60, 102748. [Google Scholar] [CrossRef]
- Zhong, D.; Li, J.; Yang, H.; Li, Y.; Huang, Y.; Xiao, Q.; Liu, T.; Jin, R. Tai Chi for essential hypertension: A systematic review of randomized controlled trials. Curr. Hypertens. Rep. 2020, 22, 25. [Google Scholar] [CrossRef]
- Bunt, C.W.; Jonas, C.E.; Chang, J.G. Knee Pain in Adults and Adolescents: The Initial Evaluation. Am. Fam. Physician 2018, 98, 576–585. [Google Scholar] [PubMed]
- Nguyen, U.S.; Zhang, Y.; Zhu, Y.; Niu, J.; Zhang, B.; Felson, D.T. Increasing Prevalence of Knee Pain and Symptomatic Knee Osteoarthritis: Survey and Cohort Data. Ann. Intern. Med. 2011, 155, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Törnblom, M.; Haglund, E.; Bremander, A.; Nilsdotter, A.; Andersson, M.L.; Hettiarachchi, P.; Johansson, P.J.; Svartengren, M.; Aili, K. Associations between knee pain and knee-loading physical activities at work and leisure: A cross-sectional study based on accelerometer measurements. BMC Musculoskelet. Disord. 2025, 26, 345. [Google Scholar] [CrossRef]
- Zeng, C.Y.; Zhang, Z.R.; Tang, Z.M.; Hua, F.Z. Benefits and Mechanisms of Exercise Training for Knee Osteoarthritis. Front. Physiol. 2021, 12, 794062. [Google Scholar] [CrossRef]
- Seeley, M.K.; Lee, H.; Son, S.J.; Timmerman, M.; Lindsay, M.; Hopkins, J.T. A Review of the Relationships Between Knee Pain and Movement Neuromechanics. J. Sport Rehabil. 2021, 31, 684–693. [Google Scholar] [CrossRef]
- Thorstensson, C.; Andersson, M.; Jönsson, H.; Saxne, T.; Petersson, I. Natural course of knee osteoarthritis in middle-aged subjects with knee pain: 12-year follow-up using clinical and radiographic criteria. Ann. Rheum. Dis. 2009, 68, 1890–1893. [Google Scholar] [CrossRef]
- Philpot, L.M.; Schumann, M.E.; Ebbert, J.O. Social relationship quality among patients with chronic pain: A population-based sample. J. Patient Exp. 2020, 7, 316–323. [Google Scholar] [CrossRef]
- Sheng, J.; Liu, S.; Wang, Y.; Cui, R.; Zhang, X. The link between depression and chronic pain: Neural mechanisms in the brain. Neural Plast. 2017, 2017, 9724371. [Google Scholar] [CrossRef] [PubMed]
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.; Pandharipande, P.P.; Watson, P.; Weinhouse, G.; Nunnally, M.; Rochwerg, B.; et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [CrossRef]
- Nahin, R.L.; Boineau, R.; Khalsa, P.S.; Stussman, B.J.; Weber, W.J. Evidence-based evaluation of complementary health approaches for pain management in the United States. Mayo Clin. Proc. 2016, 91, 1292–1306. [Google Scholar] [CrossRef]
- Wang, Y.; Aaron, R.; Attal, N.; Colloca, L. An Update on Non-Pharmacological Interventions for Pain Relief. Cell Rep. Med. 2025, 6, 101940. [Google Scholar] [CrossRef] [PubMed]
- Rogers, C.E.; Larkey, L.K.; Keller, C. A Review of Clinical Trials of Tai Chi and Qigong in Older Adults. West. J. Nurs. Res. 2009, 31, 245–279. [Google Scholar] [CrossRef]
- Kang, H.; Yang, M.; Li, M.; Xi, R.; Sun, Q.; Lin, Q. Effects of different parameters of Tai Chi on the intervention of chronic low back pain: A meta-analysis. PLoS ONE 2024, 19, e0306518. [Google Scholar] [CrossRef] [PubMed]
- Kong, L.J.; Lauche, R.; Klose, P.; Bu, J.H.; Yang, X.C.; Guo, C.Q.; Dobos, G.; Cheng, Y.W. Tai Chi for chronic pain conditions: A systematic review and meta-analysis of randomized controlled trials. Sci. Rep. 2016, 6, 25325. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Moher, D. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Gilbert, A.; Piccinin, C.; Velikova, G.; Groenvold, M.; Kuliś, D.; Blazeby, J.M.; Bottomley, A. Linking the European Organisation for Research and Treatment of Cancer Item Library to the Common Terminology Criteria for Adverse Events. J. Clin. Oncol. 2022, 40, 3770–3780. [Google Scholar] [CrossRef]
- Song, R.; Lee, E.O.; Lam, P.; Bae, S.C. Effects of Tai Chi exercise on pain, balance, muscle strength, and perceived difficulties in physical functioning in older women with osteoarthritis: A randomized clinical trial. J. Rheumatol. 2003, 30, 2039–2044. [Google Scholar]
- Brismée, J.M.; Paige, R.L.; Chyu, M.C.; Boatright, J.D.; Hagar, J.M.; McCaleb, J.A.; Quintela, M.M.; Feng, D.; Xu, K.T.; Shen, C.L. Group and home-based Tai Chi in elderly subjects with knee osteoarthritis: A randomized controlled trial. Clin. Rehabil. 2007, 21, 99–111. [Google Scholar] [CrossRef]
- Lee, H.J.; Park, H.J.; Chae, Y.; Kim, S.Y.; Kim, S.N.; Kim, S.T.; Kim, J.H.; Yin, C.S.; Lee, H. Tai Chi Qigong for the quality of life of patients with knee osteoarthritis: A pilot, randomized, waiting-list controlled trial. Clin. Rehabil. 2009, 23, 504–511. [Google Scholar] [CrossRef]
- Wang, C.; Schmid, C.H.; Hibberd, P.L.; Kalish, R.; Roubenoff, R.; Rones, R.; McAlindon, T. Tai Chi is effective in treating knee osteoarthritis: A randomized controlled trial. Arthritis Rheum. 2009, 61, 1545–1553. [Google Scholar] [CrossRef]
- Wortley, M.; Zhang, S.; Paquette, M.; Byrd, E.; Baumgartner, L.; Klipple, G.; Krusenklaus, J.; Brown, L. Effects of resistance and Tai Ji training on mobility and symptoms in knee osteoarthritis patients. J. Sport Health Sci. 2013, 2, 209–214. [Google Scholar] [CrossRef]
- Tsai, P.F.; Chang, J.Y.; Beck, C.; Kuo, Y.F.; Keefe, F.J. A pilot cluster-randomized trial of a 20-week Tai Chi program in elders with cognitive impairment and osteoarthritic knee: Effects on pain and other health outcomes. J. Pain Symptom Manag. 2013, 45, 660–669. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Schmid, C.H.; Iversen, M.D.; Harvey, W.F.; Fielding, R.A.; Driban, J.B.; Price, L.L.; Wong, J.B.; Reid, K.F.; Rones, R.; et al. Comparative effectiveness of Tai Chi versus physical therapy for knee osteoarthritis: A randomized trial. Ann. Intern. Med. 2016, 165, 77–86. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Huang, L.; Wu, X.; Wang, L.; Zhang, Y.; Fang, M.; Liu, Y.; Li, J.X. Effects of Tai Ji Quan training on gait kinematics in older Chinese women with knee osteoarthritis: A randomized controlled trial. J. Sport Health Sci. 2016, 5, 297–303. [Google Scholar] [CrossRef] [PubMed]
- Büyükturan, Ö.; Büyükturan, B.; Kurt, E.E.; Yetiş, M. Effects of Tai Chi on partial anterior cruciate ligament injury: A single-blind, randomized-controlled trial. Turk. J. Phys. Med. Rehabil. 2019, 65, 160–168. [Google Scholar] [CrossRef]
- Liu, J.; Chen, L.; Chen, X.; Hu, K.; Tu, Y.; Lin, M.; Huang, J.; Liu, W.; Wu, J.; Qiu, Z.; et al. Modulatory effects of different exercise modalities on the functional connectivity of the periaqueductal gray and ventral tegmental area in patients with knee osteoarthritis: A randomised multimodal magnetic resonance imaging study. Br. J. Anaesth. 2019, 123, 506–518. [Google Scholar] [CrossRef]
- Hu, X.; Lai, Z.; Wang, L. Effects of Tai Chi exercise on knee and ankle proprioception among individuals with knee osteoarthritis. Res. Sports Med. 2020, 28, 268–278. [Google Scholar] [CrossRef]
- Ye, Y.; Liu, A. The Effectiveness of Tai Chi for Knee Osteoarthritis: An Overview of Systematic Reviews. Int. J. Gen. Med. 2023, 16, 4499–4514. [Google Scholar] [CrossRef]
- Hu, L.; Wang, Y.; Liu, X.; Ji, X.; Ma, Y.; Man, S.; Hu, Z.; Cheng, J.; Huang, F. Tai Chi Exercise Can Ameliorate Physical and Mental Health of Patients with Knee Osteoarthritis: Systematic Review and Meta-Analysis. Clin. Rehabil. 2021, 35, 64–79. [Google Scholar] [CrossRef]
- Cui, H.; Wang, Q.; Pedersen, M.; Wang, Q.; Lv, S.; James, D.; Larkey, L. The Safety of Tai Chi: A Meta-Analysis of Adverse Events in Randomized Controlled Trials. Contemp. Clin. Trials 2019, 82, 85–92. [Google Scholar] [CrossRef]
- Yang, F.; Liu, W. Knee Joint Biomechanics of Simplified 24 Tai Chi Forms and Association with Pain in Individuals with Knee Osteoarthritis: A Pilot Study. Osteoarthr. Cartil. Open 2021, 3, 100149. [Google Scholar] [CrossRef] [PubMed]
- Xing, H.; Su, X.; Liu, Y.; Chen, Y.; Ju, Y.; Kang, Z.; Sun, W.; Yao, F.; Yao, L.; Gong, L. Prediction of Knee Joint Pain in Tai Chi Practitioners: A Cross-Sectional Machine Learning Approach. BMJ Open 2023, 13, e067036. [Google Scholar] [CrossRef]
- Song, R.; Lee, E.O.; Lam, P.; Bae, S.C. Effects of a Sun-Style Tai Chi Exercise on Arthritic Symptoms, Motivation and the Performance of Health Behaviors in Women with Osteoarthritis. J. Korean Acad. Nurs. 2007, 37, 249–256. [Google Scholar] [CrossRef] [PubMed]
- Li, J.Y.; Zhang, Y.F.; Smith, G.S.; Xue, C.J.; Luo, Y.N.; Chen, W.H.; Skinner, C.J.; Finkelstein, J. Quality of Reporting of Randomized Clinical Trials in Tai Chi Interventions—A Systematic Review. Evid.-Based Complement. Alternat. Med. 2011, 2011, 383245. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef] [PubMed]
- Park, J.; Lee, J.; Lee, J.; Kim, Y. The Effects of Physical Activity on Health Outcomes among Korean Adults: Using Data from the Korea National Health and Nutrition Examination Survey. J. Korean Med. Sci. 2020, 35, e138. [Google Scholar] [CrossRef]
- Paffenbarger, R.S.; Hyde, R.T.; Wing, A.L.; Hsieh, C.C. Physical Activity, All Cause Mortality, and Longevity of College Alumni. N. Engl. J. Med. 1986, 314, 605–613. [Google Scholar] [CrossRef]
- Lloyd, M.; Skelton, D.A.; Mead, G.E.; Williams, B.; van Wijck, F. Physical Fitness Interventions for Nonambulatory Stroke Survivors: A Mixed Methods Systematic Review and Meta Analysis. Brain Behav. 2018, 8, e01000. [Google Scholar] [CrossRef]
- Messier, S.P.; Glasser, J.L.; Ettinger, W.H., Jr.; Craven, T.E.; Miller, M.E. Declines in Strength and Balance in Older Adults with Chronic Knee Pain: A 30 Month Longitudinal, Observational Study. Arthritis Rheum. 2002, 47, 141–148. [Google Scholar] [CrossRef]
- Li, L.; Guo, S.; Ding, B.; Zhang, J. Effectiveness of Tai Chi Exercise on Balance, Falls, and Motor Function in Older Adults: A Meta Analysis. Front. Med. 2024, 11, 1486746. [Google Scholar] [CrossRef]

| First Author (Year) | Patient(s), Sample Size | Experimental Group (Intervention, Regimen) | Control Group (Intervention, Regimen) | Outcome Measurements | Main Result | Adverse Events |
|---|---|---|---|---|---|---|
| Song R (2003) [29], South Korea | Knee pain patients with knee osteoarthritis n = 43 | Tai Chi n = 22; total of 36 sessions (three times a week for 12 weeks) | No intervention, n = 21 | 1. WOMAC score (1) Joint pain (2) Joint stiffness (3) Physical function 2. Function scale (1) Balance (2) Cardiovascular functioning 3. Muscle strength (1) Abdominal muscle strength (2) Knee muscle strength | 1. (1) p < 0.05 (2) p < 0.05 (3) p < 0.01 2. (1) p < 0.01 (2) NS 3. (1) p < 0.01 (2) NS | n.r. |
| Brismée JM (2007) [30], United States | Knee pain patients with knee osteoarthritis n = 31 | Tai Chi n = 18; total of 18 sessions (three times a week for 6 weeks) | Health education n = 13; total of 18 sessions (three times a week for 6 weeks) | 1. VAS for knee pain 2. WOMAC score (1) Overall (2) Pain (3) Stiffness (4) Function 3. Function scale (knee ROM) | 1. p < 0.05 2. (1) p < 0.05 (2) p < 0.05 (3) NS (4) p < 0.05 3. NS | (E) Minor muscle soreness and foot and knee pain after first session. No AEs were observed during the remaining sessions. (C) None. |
| Lee HJ (2008) [31], South Korea | Knee pain patients with knee osteoarthritis n = 41 | Tai Chi n = 28; total of 16 sessions (twice a week for 8 weeks) | No intervention n = 13 | 1. WOMAC score (1) Total (2) Pain (3) Stiffness (4) Physical function 2. Functional scale (6 min walking test) 3. Quality of life (SF-36) (1) Total (2) Physical health (3) Mental health | 1. (1) NS (2) p < 0.05 (3) NS (4) NS 2. p < 0.001 3. (1) p < 0.05 (2) p < 0.05 (3) p < 0.05 | n.r. |
| Wang C (2009) [32], United States | Knee pain patients with knee osteoarthritis n = 40 | Tai Chi n = 20; total of 24 sessions (twice a week for 12 weeks) | Stretching and health education n = 20; total of 24 sessions (twice a week for 12 weeks) | 1. WOMAC score (1) Pain (2) Stiffness (3) Function 2. VAS for pain 3. Functional scale (1) 6 Minute Walk Test (2) Balance score (3) Chair stand time 4. Quality of life (SF-36) (1) Physical health (2) Mental health 5. Depressive scale (CES-D) 6. Self-Efficacy Score | 1. (1) p < 0.001 (2) p < 0.05 (3) p < 0.01 2. p < 0.01 3. (1) NS (2) NS (3) p < 0.001 4. (1) p < 0.01 (2) NS 5. p < 0.01 6. p < 0.05 | (E) One participant in the Tai Chi group reported an increase in knee pain at 2 weeks. This was resolved following the modification of that participant’s Tai Chi Technique. (C) None. |
| Wortley M (2013) [33], United States | Knee Pain patients with knee osteoarthritis n = 31 | (E) Tai Chi n = 12; total of 20 sessions (two times a week for 10 weeks) | (C1) Resistance training n = 13; total of 20 sessions (two times a week for 10 weeks) (C2) No intervention n = 6 | 1. WOMAC score (1) Pain (2) Physical function (3) Stiffness 2. Functional scale (1) 6 min walking test (2) Time up and go test (3) Stair climb and descent test | 1. (1) p < 0.01 in (C1), NS in (E) and (C2) (2) p < 0.05 in (C1), NS in (E) and (C2) (3) p < 0.05 in (E), p < 0.001 in (C1) and NS in (C2) 2. (1) NS in (E), (C1) and (C2) (2) p < 0.001 in (E), p < 0.01 in (C1) and NS in (C2) (3) NS in (E), (C1) and (C2) | n.r. |
| Tsai PF (2013) [34], United States | Knee pain patients with knee osteoarthritis n = 55 | Tai Chi n = 28; total of 60 sessions (three times a week for 20 weeks) | Health education n = 27; 60 sessions (three times a week for 20 weeks) | 1. WOMAC score (1) Pain score (2) Physical function (3) Stiffness 2. Function scale (sit to stand test) 3. MMSE score | 1. (1) p < 0.01 (2) NS (3) p < 0.05 2. NS 3. NS | No AEs occurred in (E) and (C). |
| Chenchen W (2016) [35], United States | Knee pain patients with knee osteoarthritis n = 204 | Tai Chi n = 106; total of 24 sessions (two times a week for 12 weeks) | Physical therapy n = 98; total of 24-48 sessions (2-4 sessions a week for 12 weeks) | 1. WOMAC score (1) Pain (2) Physical function (3) Stiffness 2. Function scale (physical function) 3. Depression scale (BDI) 4. Medication use 5. Quality of life (SF-36) | 1. (1) NS (2) NS (3) NS 2. NS 3. p < 0.01 4. NS 5. p < 0.05 | No AEs occurred in (E) and (C). |
| Zhu Q (2016) [36], China | Knee pain patients with knee osteoarthritis n = 46 | Tai Chi n = 23; total of 72 sessions (three times a week for 24 weeks) | Health education n = 23; total of 24 sessions (once a week for 24 weeks) | 1. WOMAC score (1) Pain (2) Physical function (3) Stiffness 2. Function scale (SPPB) | 1. (1) p < 0.01 (2) p < 0.01 (3) p < 0.001 2. p < 0.001 | No AEs occurred in (E) and (C). |
| Buyukturan O (2019) [37], Turkey | Knee pain patients with partial anterior cruciate ligament injury n = 58 | Tai Chi n = 29; total of 24 sessions (three times a week for 8 weeks) | No intervention n = 29 | 1. VAS for pain 2. Function scale (Lysholm Knee Scale) 3. Muscle strength (Biodex System 4-Pro) (1) Extension PT 60°/sec (2) Flexion PT 60°/sec (3) Extension PT 180°/sec (4) Flexion PT 180°/sec 4. Proprioception scale | 1. p < 0.01 2. NS 3. (1) p < 0.05 (2) NS (3) p < 0.05 (4) NS 4. p < 0.001 | n.r. |
| Liu J (2019) [38], China | Knee pain patients with knee osteoarthritis n = 52 | Tai Chi n = 28; total of 60 sessions (five times a week for 12 weeks) | Health education n = 24; total of 60 sessions (five times a week for 12 weeks) | 1. KOOS score (1) Pain (2) Symptoms (3) Daily living (4) Sport (5) Quality of life 2. Serum biomarker (1) BDNF (2) IFN-g (3) PD-1 (4) TIM-3 3. Functional connectivity changes in brain regions (1) PAG (2) VTA | 1. (1) p < 0.01 (2) NS (3) NS (4) p < 0.01 (5) p < 0.01 2. (1) NS (2) p < 0.01 (3) p < 0.01 (4) NS (3) p < 0.01 3. (1) Tai Chi decreased right PAG rsFC with the medial orbital prefrontal cortex, and the decreased rsFC was associated with improvements in knee pain (2) There was also a significantly decreased rsFC between the left VTA and the medial orbital prefrontal cortex in the Tai Chi group | No AEs occurred in (E) and (C). |
| Hu X (2020) [39], China | Knee pain patients with knee osteoarthritis n = 92 | Tai Chi n = 52; total of 72 sessions (three times a week for 24 weeks) | Health education n = 40; total of 24 sessions (once a week for 24 weeks) | 1. VAS for pain 2. WOMAC score (1) Pain (2) Physical function (3) Stiffness 3. Proprioception scale (1) Plantarflexion of ankle (2) Dorsiflexion of ankle (3) Varus of ankle (4) Valgus of ankle (5) Flexion of knee (6) Extension of knee | 1. NS 2. (1) NS (2) p < 0.05 (3) NS 3. (1) p < 0.05 (2) p < 0.05 (3) p < 0.05 (4) NS (5) p < 0.05 (6) NS | n.r. |
| Program Name | Details of Program | |
|---|---|---|
| Song R (2003) [29] | 12-form Tai Chi from Sun-style Tai Chi | 20 min; 12-form Tai Chi from Sun-style Tai Chi (1) Warm-up exercise (2) Tai chi movement (3) Cool-down exercise |
| Brismée JM (2007) [30] | 24-form Tai Chi from Yang-style Tai Chi | 40 min; 24-form Tai Chi from Yang-style Tai Chi (1) Warm-up exercise for 5 min (2) Tai Chi movement for 30 min (3) Cool-down exercise for 5 min |
| Lee HJ (2008) [31] | 18-form Tai Chi | 60 min; 18-form Tai Chi (1) Warm-up exercise for 10 min (2) Tai Chi movement for 50 min - Raising the arms; - Opening the chest; - Painting a rainbow; - Separating the clouds; - Rolling the arms in a horse-riding stance; - Rowing the boat; - Carry ball in front of the shoulders; - Looking at the moon; - Pushing palms; - Cloud hands in a horse-riding stance; - Scooping the sea and searching the sky; - Pushing waves; - Flying dove spreads its wings; - Punching in horse stance; - Flying like wild geese; - Rotating wheel; - Stepping whilst bouncing a ball; - Balancing chi. |
| Wang C (2009) [32] | 10-form Tai Chi from Yang-style Tai Chi | 60 min; 10-form Tai Chi from Yang-style Tai Chi (1) Self-massage and a review of Tai Chi principles for 10 min (2) Tai Chi movement for 30 min (3) Breathing technique for 10 min (4) Relaxation for 10 min |
| Wortley M (2013) [33] | 12-form Tai Chi from Yang-style Tai Chi | 60 min; 12-form Tai Chi from Yang-style Tai Chi (1) The program began by learning the first two movements during the first session and then adding a new movement during each session for the first 5 weeks. (2) In each training session of the first few weeks, sufficient time was provided for practicing the new and previously learned movements. (3) During the last 5 weeks, participants also practiced the movements in the opposite direction to the original direction in order to similarly “load” both lower limbs. |
| Tsai PF (2013) [34] | 12-form Tai Chi from Sun-style Tai Chi | Tai Chi started at 20 min per session and gradually increased to 40 min per session; 12-form Tai Chi from Sun-style Tai Chi (1) Stage 1 (30 sessions in the first 10 weeks) enabled them to learn the forms (2) Stage 2 (30 sessions in the second 10 weeks) enabled them to rehearse the forms |
| Chenchen W (2016) [35] | Developed classical Yang-style Tai Chi | 60 min; developed classical Yang-style Tai Chi (1) Warm-up exercise (2) Review of Tai Chi principles (3) Tai Chi movement (4) Breathing techniques (5) Relaxation methods |
| Zhu Q (2016) [36] | 8-form Tai Chi | 60 min; 8-form Tai Chi (1) Withdraw and push (2) Fan through the back (3) Wave hands like clouds (4) Lift hand (5) Brush knee and twist steps (6) Step back to repulse monkey (7) Fair lady works at shuttles (8) Golden pheasant stands with one leg (right and left) |
| Buyukturan O (2019) [37] | 10-form Tai Chi from Yang-style Tai Chi | 60 min; 10-form Tai Chi from Yang-style Tai Chi (1) Warm-up exercise and a review of Tai Chi principles and techniques (2) Tai Chi movement (3) Breathing techniques (4) Various relaxation methods |
| Liu J (2019) [38] | 24-form Tai Chi from Yang-Style Tai Chi | 60 min; 24-form Tai Chi from Yang-style Tai Chi (1) Warm-up exercise for 10 min (2) Tai Chi movement for 30 min (3) Breathing techniques for 10 min (4) Relaxation for 10 min |
| Hu X (2020) [39] | Tai Chi | 60 min; Tai Chi (1) Warm-up exercise for 5 min (2) Tai Chi movement for 50 min (3) Cool-down for 5 min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, H.; Sung, S.-H.; Lee, S. The Effectiveness and Safety of Tai Chi on Knee Pain: A Systematic Review and Meta-Analysis. Healthcare 2025, 13, 1615. https://doi.org/10.3390/healthcare13131615
Lee H, Sung S-H, Lee S. The Effectiveness and Safety of Tai Chi on Knee Pain: A Systematic Review and Meta-Analysis. Healthcare. 2025; 13(13):1615. https://doi.org/10.3390/healthcare13131615
Chicago/Turabian StyleLee, Hyunggon, Soo-Hyun Sung, and Sangnam Lee. 2025. "The Effectiveness and Safety of Tai Chi on Knee Pain: A Systematic Review and Meta-Analysis" Healthcare 13, no. 13: 1615. https://doi.org/10.3390/healthcare13131615
APA StyleLee, H., Sung, S.-H., & Lee, S. (2025). The Effectiveness and Safety of Tai Chi on Knee Pain: A Systematic Review and Meta-Analysis. Healthcare, 13(13), 1615. https://doi.org/10.3390/healthcare13131615






