Airway Ultrasound: A Narrative Review of Present Use and Future Applications in Anesthesia
Abstract
1. Introduction
2. Materials & Methods
3. Results
3.1. Airway Ultrasound: Principles and Techniques
3.2. Sonoanatomy of the Upper Airway
3.3. Airway Ultrasound in Specific Clinical Situations
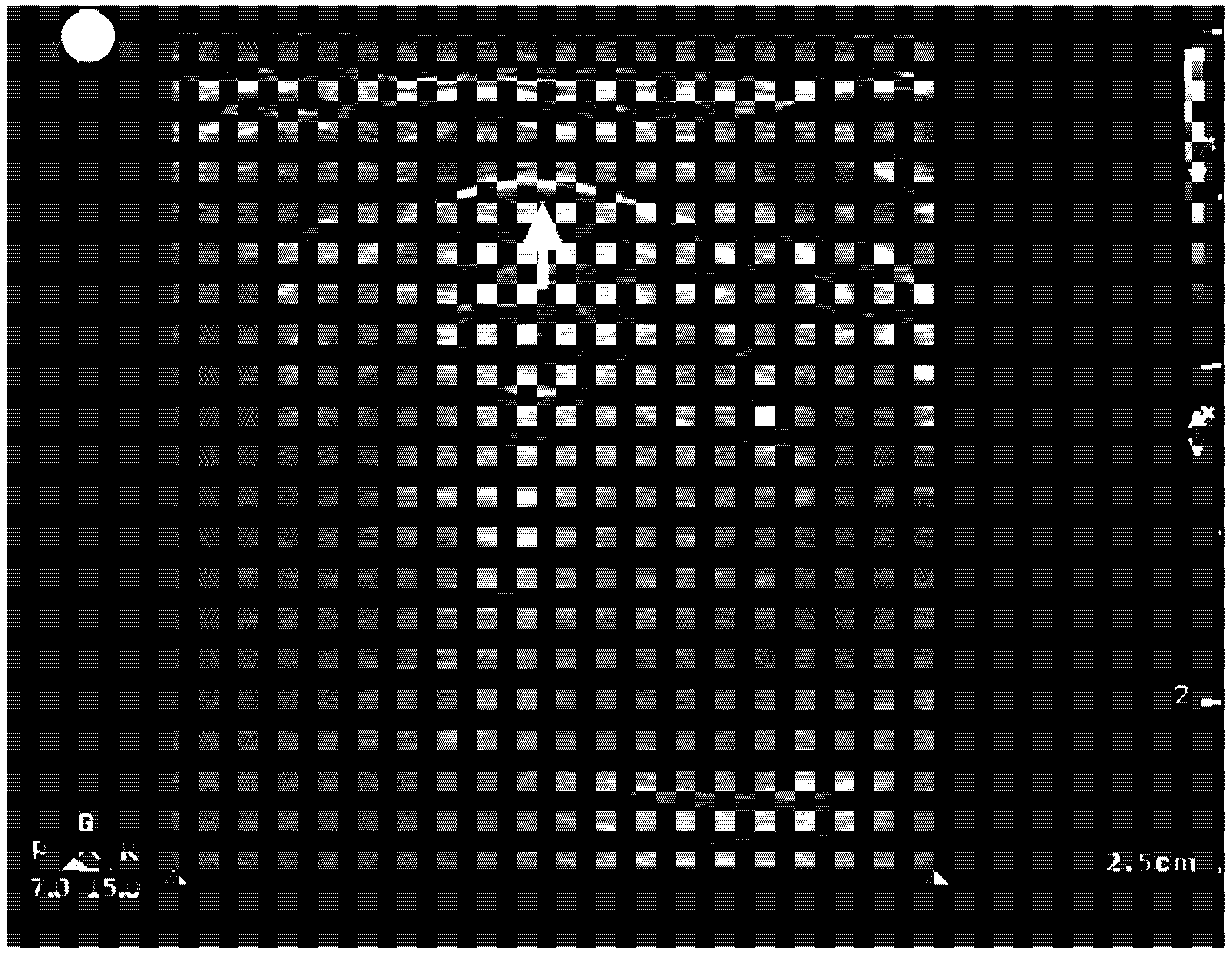
3.3.1. Assessment of Difficulty with Airway
3.3.2. Confirmation of Endotracheal Tube Position
3.3.3. Evaluation of Laryngeal Edema
3.3.4. Ultrasound to Aid in Emergent Cricothyroidotomy
3.3.5. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Turner, J.S.; Bucca, A.W.; Propst, S.L.; Ellender, T.J.; Sarmiento, E.J.; Menard, L.M.; Hunter, B.R. Association of Checklist Use in Endotracheal Intubation with Clinically Important Outcomes: A Systematic Review and Meta-analysis. JAMA Netw. Open 2020, 3, e209278. [Google Scholar] [CrossRef] [PubMed]
- Levitan, R.M.; Heitz, J.W.; Sweeney, M.; Cooper, R.M. The complexities of tracheal intubation with direct laryngoscopy and alternative intubation devices. Ann. Emerg. Med. 2011, 57, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Kwon, Y.S.; Lee, C.A.; Park, S.; Ha, S.O.; Sim, Y.S.; Baek, M.S. Incidence and outcomes of cricothyrotomy in the “cannot intubate, cannot oxygenate” situation. Medicine 2019, 98, e17713. [Google Scholar] [CrossRef]
- Roth, D.; Pace, N.L.; Lee, A.; Hovhannisyan, K.; Warenits, A.-M.; Arrich, J.; Herkner, H. Airway physical examination tests for detection of difficult airway management in apparently normal adult patients. Cochrane Database Syst. Rev. 2018, 5, CD008874. [Google Scholar] [CrossRef]
- Heidegger, T.; Pandit, J.J. Difficult Airway Management: From the Power of Prediction to the Art of Management. Anesth. Analg. 2025, 140, 290–294. [Google Scholar] [CrossRef]
- Yentis, S.M. Predicting difficult intubation–worthwhile exercise or pointless ritual? Anaesthesia 2002, 57, 105–109. [Google Scholar] [CrossRef] [PubMed]
- Sotoodehnia, M.; Rafiemanesh, H.; Mirfazaelian, H.; Safaie, A.; Baratloo, A. Ultrasonography indicators for predicting difficult intubation: A systematic review and meta-analysis. BMC Emerg. Med. 2021, 21, 76. [Google Scholar] [CrossRef]
- Carsetti, A.; Sorbello, M.; Adrario, E.; Donati, A.; Falcetta, S. Airway Ultrasound as Predictor of Difficult Direct Laryngoscopy: A Systematic Review and Meta-analysis. Anesth. Analg. 2022, 134, 740–750. [Google Scholar] [CrossRef]
- Gomes, S.H.; Simões, A.M.; Nunes, A.M.; Pereira, M.V.; Teoh, W.H.; Costa, P.S.; Kristensen, M.S.; Teixeira, P.M.; Pêgo, J.M. Useful Ultrasonographic Parameters to Predict Difficult Laryngoscopy and Difficult Tracheal Intubation—A Systematic Review and Meta-Analysis. Front. Med. 2021, 8, 671658. [Google Scholar] [CrossRef]
- Borowy, C.S.; Mukhdomi, T. Sonography Physical Principles and Instrumentation. In StatPearls [Internet]; StatPearls Publishing: St.Petersburg, FL, USA, 2023. [Google Scholar]
- Bakhru, R.N.; Schweickert, W.D. Intensive care ultrasound: I. Physics, equipment, and image quality. Ann. Am. Thorac. Soc. 2013, 10, 540–548. [Google Scholar] [CrossRef]
- Sidebotham, D.; Merry, A.F.; Legget, M.E.; Wright, I.G. Practical Perioperative Transoesophageal Echocardiography; Oxford University Press: Oxford, UK, 2018; pp. 13–21. [Google Scholar]
- Garg, R.; Gupta, A. Ultrasound: A promising tool for contemporary airway management. World J. Clin. Cases 2015, 3, 926–929. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Bellinger, R.; Shedd, A.; Wolfshohl, J.; Walker, J.; Healy, J.; Taylor, J.; Chao, K.; Yen, Y.-H.; Tzeng, C.-F.T.; et al. Point-of-care ultrasound in airway evaluation and management: A comprehensive review. Diagnostics 2023, 13, 1541. [Google Scholar] [CrossRef] [PubMed]
- Kadadi, S.; Gadkari, C.; Pundkar, A. A Comparison of Airway Ultrasound and Clinical Parameters for Predicting Difficult Laryngoscopy in the Emergency Department: A Study Protocol. Cureus 2024, 16, e69543. [Google Scholar] [CrossRef] [PubMed]
- Singh, M.; Chin, K.J.; Chan, V.W.; Wong, D.T.; Prasad, G.A.; Yu, E. Use of sonography for airway assessment: An observational study. J. Ultrasound Med. 2010, 29, 79–85. [Google Scholar] [CrossRef]
- Shan, T.; Tan, Q.; Wu, D.; Bao, H.; Ge, D.; Han, L.; Su, C.; Ju, Y. Ultrasound-guided superior laryngeal nerve block: A randomized comparison between parasagittal and transverse approach. BMC Anesthesiol. 2024, 24, 269. [Google Scholar] [CrossRef]
- Pinto, J.; Cordeiro, L.; Pereira, C.; Gama, R.; Fernandes, H.; Assunção, J. Predicting difficult laryngoscopy using ultrasound measurement of distance from skin to epiglottis. J. Crit. Care 2016, 33, 26–31. [Google Scholar] [CrossRef]
- Zheng, Z.; Wang, X.; Du, R.; Wu, Q.; Chen, L.; Ma, W. Effectiveness of ultrasonic measurement for the hyomental distance and distance from skin to epiglottis in predicting difficult laryngoscopy in children. Eur. Radiol. 2023, 33, 7849–7856. [Google Scholar] [CrossRef]
- Kalezić, N.; Lakićević, M.; Miličić, B.; Stojanović, M.; Sabljak, V.; Marković, D. Hyomental distance in the different head positions and hyomental distance ratio in predicting difficult intubation. Bosn. J. Basic Med Sci. 2016, 16, 232–236. [Google Scholar] [CrossRef]
- Huh, J.; Shin, H.-Y.; Kim, S.-H.; Yoon, T.-K.; Kim, D.-K. Diagnostic predictor of difficult laryngoscopy: The hyomental distance ratio. Anesth. Analg. 2009, 108, 544–548. [Google Scholar] [CrossRef]
- Petrișor, C.; Trancă, S.; Szabo, R.; Simon, R.; Prie, A.; Bodolea, C. Clinical versus Ultrasound Measurements of Hyomental Distance Ratio for the Prediction of Difficult Airway in Patients with and without Morbid Obesity. Diagnostics 2020, 10, 140. [Google Scholar] [CrossRef]
- Osman, A.; Sum, K.M. Role of upper airway ultrasound in airway management. J. Intensiv. Care 2016, 4, 52. [Google Scholar] [CrossRef] [PubMed]
- Sotoodehnia, M.; Khodayar, M.; Jalali, A.; Momeni, M.; Safaie, A.; Abdollahi, A. Prediction of difficult laryngoscopy/difficult intubation cases using upper airway ultrasound measurements in emergency department: A prospective observational study. BMC Emerg. Med. 2023, 23, 78. [Google Scholar] [CrossRef]
- Petrisor, C.; Szabo, R.; Constantinescu, C.; Prie, A.; Hagau, N. Ultrasound-based assessment of hyomental distances in neutral, ramped, and maximum hyperextended positions, and derived ratios, for the prediction of difficult airway in the obese population: A pilot diagnostic accuracy study. Anaesthesiol. Intensiv. Ther. 2018, 50, 110–116. [Google Scholar] [CrossRef]
- Rudingwa, P.; Yadav, N.K.; Mishra, S.K.; Pannerselvam, S. Ultrasound measurement of anterior neck soft tissue and tongue thickness to predict difficult laryngoscopy—An observational analytical study. Indian J. Anaesth. 2019, 63, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, S.; Zeger, W.; Schmier, C.; Crum, T.; Craven, A.; Frrokaj, I.; Pang, H.; Shostrom, V. Pilot study to determine the utility of point-of-care ultrasound in the assessment of difficult laryngoscopy. Acad. Emerg. Med. 2011, 18, 754–758. [Google Scholar] [CrossRef]
- Zheng, J.; Wu, J.; Dong, J.; Ding, Y. Role of anterior neck soft tissue quantifications by ultrasound in predicting difficult laryngoscopy. Med Sci. Monit. 2014, 20, 2343–2350. [Google Scholar] [CrossRef]
- Furia, J.S.; Nadkarni, M.M. Ultrasound-based assessment of tongue thickness for prediction of difficult laryngoscopy and intubation. J. Anaesthesiol. Clin. Pharmacol. 2024, 40, 235–241. [Google Scholar] [CrossRef] [PubMed]
- Yao, W.; Wang, B. Can tongue thickness measured by ultrasonography predict difficult tracheal intubation? Br. J. Anaesth. 2017, 118, 601–609. [Google Scholar] [CrossRef]
- Wang, B.; Yao, W.; Xue, Q.; Wang, M.; Xu, J.; Chen, Y.; Zhang, Y. Nomograms for predicting difficult airway based on ultrasound assessment. BMC Anesthesiol. 2022, 22, 23. [Google Scholar] [CrossRef]
- De Luis-Cabezón, N.; Ly-Liu, D.; Renedo-Corcostegui, P.; Santaolalla-Montoya, F.; de Maturana, A.Z.-L.; Herrero-Herrero, J.C.; Martínez-Hurtado, E.; De Frutos-Parra, R.; Bilbao-Gonzalez, A.; Fernandez-Vaquero, M.A. A new score for airway assessment using clinical and ultrasound parameters. Front. Med. 2024, 11, 1334595. [Google Scholar] [CrossRef]
- Chou, H.-C.; Tseng, W.-P.; Wang, C.-H.; Ma, M.H.-M.; Wang, H.-P.; Huang, P.-C.; Sim, S.-S.; Liao, Y.-C.; Chen, S.-Y.; Hsu, C.-Y.; et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation 2011, 82, 1279–1284. [Google Scholar] [CrossRef] [PubMed]
- Adi, O.; Chuan, T.W.; Rishya, M. A feasibility study on bedside upper airway ultrasonography compared to waveform capnography for verifying endotracheal tube location after intubation. Crit. Ultrasound J. 2013, 5, 7. [Google Scholar] [CrossRef] [PubMed]
- Chou, E.H.; Dickman, E.; Tsou, P.-Y.; Tessaro, M.; Tsai, Y.-M.; Ma, M.H.-M.; Lee, C.-C.; Marshall, J. Ultrasonography for confirmation of endotracheal tube placement: A systematic review and meta-analysis. Resuscitation 2015, 90, 97–103. [Google Scholar] [CrossRef]
- Kuriyama, A.; Jackson, J.L.; Kamei, J. Performance of the cuff leak test in adults in predicting post-extubation airway complications: A systematic review and meta-analysis. Crit. Care 2020, 24, 640. [Google Scholar] [CrossRef]
- Pluijms, W.A.; van Mook, W.N.; Wittekamp, B.H.; Bergmans, D.C. Postextubation laryngeal edema and stridor resulting in respiratory failure in critically ill adult patients: Updated review. Crit. Care 2015, 19, 295. [Google Scholar] [CrossRef]
- Schick, M.; Grether-Jones, K. Point-of-Care Sonographic Findings in Acute Upper Airway Edema. West J. Emerg. Med. 2016, 17, 825–829. [Google Scholar] [CrossRef]
- Aytac, B.G.; Soyal, O.B. Ultrasonographic evaluation of the postoperative airway edema after robotic prostatectomy: A single center observational study. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 8505–8513. [Google Scholar] [CrossRef] [PubMed]
- Cook, T.M.; Woodall, N.; Harper, J.; Benger, J. Fourth National Audit Project. Major complications of airway management in the UK: Results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 2: Intensive care and emergency departments. Br. J. Anaesth. 2011, 106, 632–642. [Google Scholar] [CrossRef]
- Watanabe, H.; Nakazawa, H.; Tokumine, J.; Yorozu, T. Real-time vs. static ultrasound-guided needle cricothyroidotomy: A randomized crossover simulation trial. Sci. Rep. 2025, 15, 8112. [Google Scholar] [CrossRef]
- Dotson, M.; Thompson, S.; Singh, G.P.; Area, S. Comparison of Point-of-Care Ultrasound Guidance and the Traditional Approach in Performing Simulated Emergent Cricothyroidotomy Among Emergency Medicine Physicians, Residents, and Students. Cureus 2024, 16, e71015. [Google Scholar] [CrossRef]
- Siddiqui, N.; Yu, E.; Boulis, S.; You-Ten, K.E. Ultrasound Is Superior to Palpation in Identifying the Cricothyroid Membrane in Subjects with Poorly Defined Neck Landmarks: A Randomized Clinical Trial. Anesthesiology 2018, 129, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, H.; Uzawa, K.; Tokumine, J.; Lefor, A.K.; Motoyasu, A.; Yorozu, T. Airway ultrasound for patients anticipated to have a difficult airway: Perspective for personalized medicine. World J. Clin. Cases 2023, 11, 1951–1962. [Google Scholar] [CrossRef] [PubMed]
- Adi, O.; Fong, C.P.; Sum, K.M.; Ahmad, A.H. Usage of airway ultrasound as an assessment and prediction tool of a difficult airway management. Am. J. Emerg. Med. 2020, 42, 263.e1–263.e4. [Google Scholar] [CrossRef] [PubMed]










| Sonographic Predictor | Measurement Cut-Off | Sensitivity (%) | Specificity (%) | Additional Notes |
|---|---|---|---|---|
| Distance from Skin to Epiglottis (DSE) | >2.5–2.75 cm | 64.7 | 77.1 | Strong NPV; increased accuracy when combined with Mallampati (compared to clinical assessment alone) |
| Hyomental Distance Ratio (HMDR) | <1.2 | 88–95.2 | 60–69.2 | Superior to traditional clinical predictors; especially useful in obese patients. |
| Skin-to-Vocal Cord Distance (SVC) | >9.4 mm | 70 | 84 | Increased SVC correlates with difficult laryngoscopy, especially in high-BMI patients. |
| Skin-to-Hyoid Bone Distance (SHB) | 66–77 mm | 68 | 73 | |
| Tongue Thickness | >6.1 cm | 75 | 83 | Its high sensitivity and specificity make this measurement excellent for evaluating difficult intubation. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riveros-Perez, E.; Avella-Molano, B.; Rocuts, A. Airway Ultrasound: A Narrative Review of Present Use and Future Applications in Anesthesia. Healthcare 2025, 13, 1502. https://doi.org/10.3390/healthcare13131502
Riveros-Perez E, Avella-Molano B, Rocuts A. Airway Ultrasound: A Narrative Review of Present Use and Future Applications in Anesthesia. Healthcare. 2025; 13(13):1502. https://doi.org/10.3390/healthcare13131502
Chicago/Turabian StyleRiveros-Perez, Efrain, Bibiana Avella-Molano, and Alex Rocuts. 2025. "Airway Ultrasound: A Narrative Review of Present Use and Future Applications in Anesthesia" Healthcare 13, no. 13: 1502. https://doi.org/10.3390/healthcare13131502
APA StyleRiveros-Perez, E., Avella-Molano, B., & Rocuts, A. (2025). Airway Ultrasound: A Narrative Review of Present Use and Future Applications in Anesthesia. Healthcare, 13(13), 1502. https://doi.org/10.3390/healthcare13131502






