Vision-Based Assessment of Skeletal Muscle Decline: Correlating Gait Variance with SPPB Performance
Abstract
1. Introduction
2. Related Work
2.1. Preliminaries
2.2. Comparison of Equipment and Methods
3. Methodology
3.1. Data Description
3.1.1. Baseline Information
- Age: 60–80 years, 9 subjects, 47.4%; over 80 years, 10 subjects, 52.6%.
- Gender: 15 males, 78.9%; 4 females, 21.1%.
- Height: 145–155 cm, 5 subjects, 26.3%; 155–165 cm, 5 subjects, 26.3%; 165–175 cm, 8 subjects, 42.1%; 175 cm or above, 1 participant, 5.3%.
- Weight: 40–50 kg, 4 subjects, 21.1%; 50–60 kg, 5 subjects, 26.3%; 60–70 kg, 9 subjects, 47.4%; 85 kg or above, 1 participant, 5.3%. It is noteworthy that there were no subjects within the 70–85 kg range.
3.1.2. Score Distribution and Test Duration
3.1.3. Movement Distance Distribution
4. Proposed Method
4.1. Step 1: Pedestrian Movement Data Extraction and Analysis
4.2. Step 2: Calculate the Variance of Movement Distance and Construct a Comprehensive Indicator
4.3. Step 3: Construct a Comprehensive Indicator Through Principal Component Analysis (PCA)
4.4. Step 4: Correlation Analysis
5. Results and Discussion
5.1. Purpose and Overview
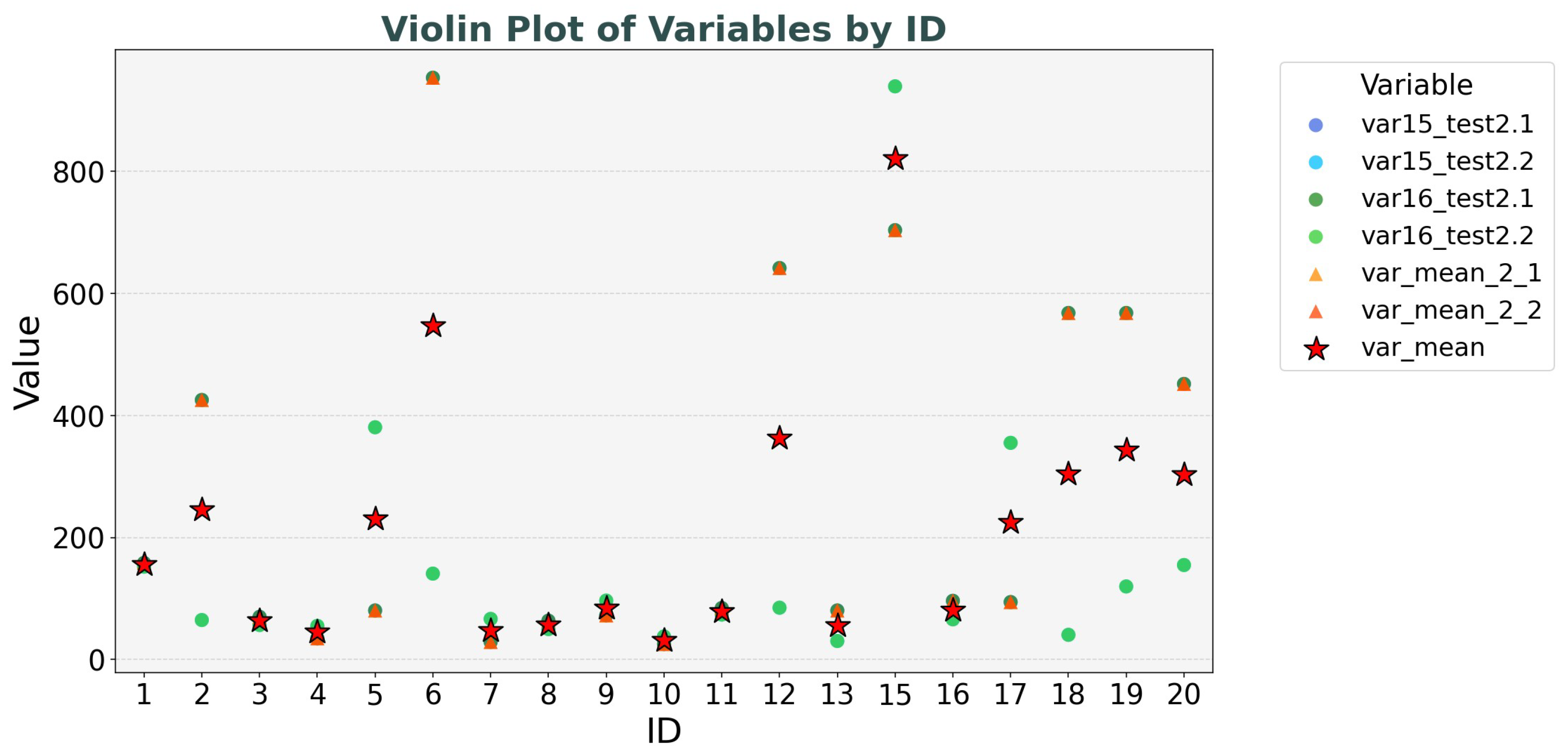
5.2. Result 1: The Relationship Between Comprehensive Indicators and Test 2 Duration in SPPB
- PC1 (Muscle-Control Reserve): The four variables var15_test2.1, var16_test2.1, var15_test2.2, and var16_test2.2 all exhibit a positive loading of 0.50 on PC1. This indicates a pattern of synchronous changes in relevant gait indicators across different test phases and limb movements. From a biomechanical standpoint, when an individual has an adequate muscle reserve, it provides the material basis for flexible gait adjustments, leading to a more stable walking performance. Therefore, PC1 embodies the "basic support" role of muscles in gait regulation and reflects an individual’s potential to adjust gait as a whole based on muscle strength.The correlation between PC1 and duration is 0.24, suggesting a slight positive trend.
- PC2 (Learning-Fatigue Response): Statistically, variables in Test 2.1 phase (var15_test2.1, var16_test2.1) exhibit a positive loading of 0.50 on PC2, while variables in Test 2.2 phase (var15_test2.2, var16_test2.2) show a negative loading of −0.50, forming a cross-phase differential pattern. When the value of PC2 increases, the gait variance in Test 2.1 phase is significantly greater than that in Test 2.2. This is due to individual nervousness or conservative strategies during the initial test, leading to frequent gait adjustments. Conversely, when the value of PC2 decreases, the gait variance in Test 2.2 phase surpasses that in Test 2.1, indicating a decline in control ability caused by physical exhaustion and decreased attention due to repeated testing. Therefore, PC2 features the distinct response patterns of the neuromuscular system during repetitive tasks, either through learning-based optimization strategies or functional decline due to fatigue. The correlation between PC2 and duration is also 0.24, indicating a similar slight positive trend.
5.3. Result 2: The Relationship Between Comprehensive Indicators and SPPB Test 2 Scores
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Thies, S.B.; Bates, A.; Costamagna, E.; Kenney, L.; Granat, M.; Webb, J.; Howard, D.; Baker, R.; Dawes, H. Are older people putting themselves at risk when using their walking frames? BMC Geriatr. 2020, 20, 90. [Google Scholar] [CrossRef]
- Montero-Odasso, M.; Van Der Velde, N.; Martin, F.C.; Petrovic, M.; Tan, M.P.; Ryg, J.; Aguilar-Navarro, S.; Alexander, N.B.; Becker, C.; Blain, H.; et al. World guidelines for falls prevention and management for older adults: A global initiative. Age Ageing 2022, 51, afac205. [Google Scholar] [CrossRef] [PubMed]
- Lauretani, F.; Ticinesi, A.; Gionti, L.; Prati, B.; Nouvenne, A.; Tana, C.; Meschi, T.; Maggio, M. Short-Physical Performance Battery (SPPB) score is associated with falls in older outpatients. Aging Clin. Exp. Res. 2019, 31, 1435–1442. [Google Scholar] [CrossRef] [PubMed]
- Martini, E.; Boldo, M.; Aldegheri, S.; Valè, N.; Filippetti, M.; Smania, N.; Bertucco, M.; Picelli, A.; Bombieri, N. Enabling gait analysis in the telemedicine practice through portable and accurate 3D human pose estimation. Comput. Methods Programs Biomed. 2022, 225, 107016. [Google Scholar] [CrossRef]
- Luo, J.; Tjahjadi, T. View and clothing invariant gait recognition via 3D human semantic folding. IEEE Access 2020, 8, 100365–100383. [Google Scholar] [CrossRef]
- Sarapata, G.; Dushin, Y.; Morinan, G.; Ong, J.; Budhdeo, S.; Kainz, B.; O’Keeffe, J. Video-based activity recognition for automated motor assessment of Parkinson’s disease. IEEE J. Biomed. Health Inform. 2023, 27, 5032–5041. [Google Scholar] [CrossRef]
- Wang, Z.; Deligianni, F.; Voiculescu, I.; Yang, G.Z. A single RGB camera based gait analysis with a mobile tele-robot for healthcare. In Proceedings of the 2021 43rd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Virtual, 1–5 November 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 6933–6936. [Google Scholar]
- Silva, J.; Atalaia, T.; Abrantes, J.; Aleixo, P. Gait Biomechanical Parameters Related to Falls in the Elderly: A Systematic Review. Biomechanics 2024, 4, 165–218. [Google Scholar] [CrossRef]
- Wang, H.; Su, B.; Lu, L.; Jung, S.; Qing, L.; Xie, Z.; Xu, X. Markerless gait analysis through a single camera and computer vision. J. Biomech. 2024, 165, 112027. [Google Scholar] [CrossRef]
- Mehta, D.; Sridhar, S.; Sotnychenko, O.; Rhodin, H.; Shafiei, M.; Seidel, H.P.; Xu, W.; Casas, D.; Theobalt, C. Vnect: Real-time 3d human pose estimation with a single rgb camera. ACM Trans. Graph. (TOG) 2017, 36, 1–14. [Google Scholar] [CrossRef]
- D’Antonio, E.; Taborri, J.; Mileti, I.; Rossi, S.; Patané, F. Validation of a 3D markerless system for gait analysis based on OpenPose and two RGB webcams. IEEE Sens. J. 2021, 21, 17064–17075. [Google Scholar] [CrossRef]
- Muñoz-Ospina, B.; Alvarez-Garcia, D.; Clavijo-Moran, H.J.C.; Valderrama-Chaparro, J.A.; García-Peña, M.; Herrán, C.A.; Urcuqui, C.C.; Navarro-Cadavid, A.; Orozco, J. Machine learning classifiers to evaluate data from gait analysis with depth cameras in patients with Parkinson’s disease. Front. Hum. Neurosci. 2022, 16, 826376. [Google Scholar] [CrossRef] [PubMed]
- Yoon, D.H.; Kim, J.H.; Lee, K.; Cho, J.S.; Jang, S.H.; Lee, S.U. Inertial measurement unit sensor-based gait analysis in adults and older adults: A cross-sectional study. Gait Posture 2024, 107, 212–217. [Google Scholar] [CrossRef] [PubMed]
- Lafontaine, V.; Lapointe, P.; Bouchard, K.; Gagnon, J.M.; Dallaire, M.; Gaboury, S.; da Silva, R.A.; Beaulieu, L.D. An open vibration and pressure platform for fall prevention with a reinforcement learning agent. Pers. Ubiquitous Comput. 2021, 25, 7–19. [Google Scholar] [CrossRef]
- Berner, K.; Cockcroft, J.; Morris, L.D.; Louw, Q. Concurrent validity and within-session reliability of gait kinematics measured using an inertial motion capture system with repeated calibration. J. Bodyw. Mov. Ther. 2020, 24, 251–260. [Google Scholar] [CrossRef]
- Choi, A.; Kim, T.H.; Yuhai, O.; Jeong, S.; Kim, K.; Kim, H.; Mun, J.H. Deep learning-based near-fall detection algorithm for fall risk monitoring system using a single inertial measurement unit. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 2385–2394. [Google Scholar] [CrossRef]
- Han, X.; Guffanti, D.; Brunete, A. A Comprehensive Review of Vision-Based Sensor Systems for Human Gait Analysis. Sensors 2025, 25, 498. [Google Scholar] [CrossRef]
- Le, V.T.; Tran-Trung, K.; Hoang, V.T. A comprehensive review of recent deep learning techniques for human activity recognition. Comput. Intell. Neurosci. 2022, 2022, 8323962. [Google Scholar] [CrossRef]
- Cedeno-Moreno, R.; Malagon-Barillas, D.L.; Morales-Hernandez, L.A.; Gonzalez-Hernandez, M.P.; Cruz-Albarran, I.A. Computer Vision System Based on the Analysis of Gait Features for Fall Risk Assessment in Elderly People. Appl. Sci. 2024, 14, 3867. [Google Scholar] [CrossRef]
- Boldo, M.; Di Marco, R.; Martini, E.; Nardon, M.; Bertucco, M.; Bombieri, N. On the reliability of single-camera markerless systems for overground gait monitoring. Comput. Biol. Med. 2024, 171, 108101. [Google Scholar] [CrossRef]
- Lim, Z.K.; Connie, T.; Goh, M.K.O.; Saedon, N.I.B. Fall risk prediction using temporal gait features and machine learning approaches. Front. Artif. Intell. 2024, 7, 1425713. [Google Scholar] [CrossRef]
- Drover, D.; Howcroft, J.; Kofman, J.; Lemaire, E.D. Faller classification in older adults using wearable sensors based on turn and straight-walking accelerometer-based features. Sensors 2017, 17, 1321. [Google Scholar] [CrossRef] [PubMed]
- Eichler, N.; Raz, S.; Toledano-Shubi, A.; Livne, D.; Shimshoni, I.; Hel-Or, H. Automatic and efficient fall risk assessment based on machine learning. Sensors 2022, 22, 1557. [Google Scholar] [CrossRef] [PubMed]
- Chen, B.; Chen, C.; Hu, J.; Sayeed, Z.; Qi, J.; Darwiche, H.F.; Little, B.E.; Lou, S.; Darwish, M.; Foote, C.; et al. Computer vision and machine learning-based gait pattern recognition for flat fall prediction. Sensors 2022, 22, 7960. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.W.; Choi, J.Y.; Ha, E.J.; Choi, J.H. Human pose estimation using mediapipe pose and optimization method based on a humanoid model. Appl. Sci. 2023, 13, 2700. [Google Scholar] [CrossRef]
- Van Criekinge, T.; Saeys, W.; Truijen, S.; Vereeck, L.; Sloot, L.H.; Hallemans, A. A full-body motion capture gait dataset of 138 able-bodied adults across the life span and 50 stroke survivors. Sci. Data 2023, 10, 852. [Google Scholar] [CrossRef]
- Lyu, Z.; Wang, L.; Gao, X.; Ma, Y. The identification of elderly people with high fall risk using machine learning algorithms. Healthcare 2022, 11, 47. [Google Scholar] [CrossRef]
- Manssor, S.A.; Sun, S.; Elhassan, M.A. Real-time human recognition at night via integrated face and gait recognition technologies. Sensors 2021, 21, 4323. [Google Scholar] [CrossRef]
- Kidziński, Ł.; Yang, B.; Hicks, J.L.; Rajagopal, A.; Delp, S.L.; Schwartz, M.H. Deep neural networks enable quantitative movement analysis using single-camera videos. Nat. Commun. 2020, 11, 4054. [Google Scholar] [CrossRef]
- Lee, D.; Soon, J.; Choi, G.; Kim, K.; Bahn, S. Identification of the Visually Prominent Gait Parameters for Forensic Gait Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2467. [Google Scholar] [CrossRef]
- Stenum, J.; Hsu, M.M.; Pantelyat, A.Y.; Roemmich, R.T. Clinical gait analysis using video-based pose estimation: Multiple perspectives, clinical populations, and measuring change. PLoS Digit. Health 2024, 3, e0000467. [Google Scholar] [CrossRef]
- Ota, M.; Tateuchi, H.; Hashiguchi, T.; Ichihashi, N. Verification of validity of gait analysis systems during treadmill walking and running using human pose tracking algorithm. Gait Posture 2021, 85, 290–297. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Nava, I.H.; Valentín-Coronado, L.M.; Garcia-Constantino, M.; Favela, J. Gait activity classification on unbalanced data from inertial sensors using shallow and deep learning. Sensors 2020, 20, 4756. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.Y.; Ha, E.; Son, M.; Jeon, J.H.; Kim, J.W. Human Joint Angle Estimation Using Deep Learning-Based Three-Dimensional Human Pose Estimation for Application in a Real Environment. Sensors 2024, 24, 3823. [Google Scholar] [CrossRef]
- Yamamoto, M.; Shimatani, K.; Ishige, Y.; Takemura, H. Verification of gait analysis method fusing camera-based pose estimation and an IMU sensor in various gait conditions. Sci. Rep. 2022, 12, 17719. [Google Scholar] [CrossRef]
- Zarkou, A.; Lee, S.C.; Prosser, L.A.; Jeka, J.J. Foot and ankle somatosensory deficits affect balance and motor function in children with cerebral palsy. Front. Hum. Neurosci. 2020, 14, 45. [Google Scholar] [CrossRef]
- Arita, S.; Nishiyama, D.; Taniguchi, T.; Fukui, D.; Yamanaka, M.; Yamada, H. Feature selection to classify lameness using a smartphone-based inertial measurement unit. PLoS ONE 2021, 16, e0258067. [Google Scholar] [CrossRef]
- Hatamzadeh, M.; Busé, L.; Chorin, F.; Alliez, P.; Favreau, J.D.; Zory, R. A kinematic-geometric model based on ankles’ depth trajectory in frontal plane for gait analysis using a single RGB-D camera. J. Biomech. 2022, 145, 111358. [Google Scholar] [CrossRef]
- Nishiyama, D.; Arita, S.; Fukui, D.; Yamanaka, M.; Yamada, H. Accurate fall risk classification in elderly using one gait cycle data and machine learning. Clin. Biomech. 2024, 115, 106262. [Google Scholar] [CrossRef]
- Nakano, N.; Sakura, T.; Ueda, K.; Omura, L.; Kimura, A.; Iino, Y.; Fukashiro, S.; Yoshioka, S. Evaluation of 3D markerless motion capture accuracy using OpenPose with multiple video cameras. Front. Sport. Act. Living 2020, 2, 50. [Google Scholar] [CrossRef]
- Anitha, G.; Priya, S.B. Vision Based Real Time Monitoring System for Elderly Fall Event Detection Using Deep Learning. Comput. Syst. Sci. Eng. 2022, 42, 87–103. [Google Scholar] [CrossRef]
- Barzyk, P.; Boden, A.S.; Howaldt, J.; Stürner, J.; Zimmermann, P.; Seebacher, D.; Liepert, J.; Stein, M.; Gruber, M.; Schwenk, M. Steps to Facilitate the Use of Clinical Gait Analysis in Stroke Patients: The Validation of a Single 2D RGB Smartphone Video-Based System for Gait Analysis. Sensors 2024, 24, 7819. [Google Scholar] [CrossRef] [PubMed]
- Lonini, L.; Moon, Y.; Embry, K.; Cotton, R.J.; McKenzie, K.; Jenz, S.; Jayaraman, A. Video-based pose estimation for gait analysis in stroke survivors during clinical assessments: A proof-of-concept study. Digit. Biomark. 2022, 6, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Parashar, A.; Shekhawat, R.S.; Ding, W.; Rida, I. Intra-class variations with deep learning-based gait analysis: A comprehensive survey of covariates and methods. Neurocomputing 2022, 505, 315–338. [Google Scholar] [CrossRef]






| Papers | Equipment Used | Privacy Protection | Camera Capture Method | Quantity of Equipment Used |
|---|---|---|---|---|
| “Video-Based Activity Recognition for Automated Motor Assessment of Parkinson’s Disease” Sarapata et al. [6] | Consumer-grade handheld devices (e.g., tablets), OpenPose | Privacy is considered. Measures: Obtained informed consent from subjects and followed ethical committee approvals; only used the 2D coordinate data of human joint positions (stick-figure data) extracted by OpenPose, without directly using the original video data. | Static (fixed-camera) | One camera; auxiliary pose estimation tools |
| “A Single RGB Camera Based Gait Analysis with a Mobile Tele-robot for Healthcare” Wang et al. [7] | Dual robot system, iPad, Intel RealSense D415 | Whether privacy is considered and specific measures were not clearly mentioned. It is not stated whether only stick-figure data is used, and the use of original video data may be involved, so privacy protection is questionable. | Dynamic (mobile robot camera) | One RGB-D camera; one iPad; one mobile tele-robot |
| “Computer Vision System Based on the Analysis of Gait Features for Fall Risk Assessment in Elderly People” Cedeno-Moreno et al. [19] | IDS UI-3130CP-M-GL R2 monochrome camera, treadmill | Privacy is considered. Measures: Approved by the ethics committee and obtained informed consent; used the key-point data (stick-figure data) extracted for gait feature analysis, without directly using the original video data. | Static (treadmill recording) | One monochrome camera; one treadmill |
| “On the reliability of single-camera markerless systems for overground gait monitoring” Boldo et al. [20] | W Intel RealSense D415, Vicon MX 13 infrared cameras | Privacy is considered. Measures: Obtained ethical approval and informed consent; used the human joint key-point data (stick-figure data) extracted by OpenPose, without directly using the original video data. | Static (overground walking) | One RGB-D camera; eight infrared cameras |
| “Fall risk prediction using temporal gait features and machine learning approaches” Lim et al. [21] | Two fixed cameras, Mendeley public dataset (inertial sensor data) | Privacy is considered. Measures: Approved by the ethics committee, obtained informed consent, and anonymized the data; used the 26 human key-point data (stick-figure data) extracted by AlphaPose, without directly using the original video data. | Static (TUG test) | Two cameras; public dataset used; no additional hardware |
| Our study | One fixed camera | Privacy is considered. During data collection, privacy protection is ensured by capturing only the human keypoint data through the camera, without recording actual video footage. | Static (fixed-camera) | One camera |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tong, Z.; Chen, S.; Yamaguchi, Y.; Nakamura, M.; Yen, H.-Y.; Lee, S.-C. Vision-Based Assessment of Skeletal Muscle Decline: Correlating Gait Variance with SPPB Performance. Healthcare 2025, 13, 1405. https://doi.org/10.3390/healthcare13121405
Tong Z, Chen S, Yamaguchi Y, Nakamura M, Yen H-Y, Lee S-C. Vision-Based Assessment of Skeletal Muscle Decline: Correlating Gait Variance with SPPB Performance. Healthcare. 2025; 13(12):1405. https://doi.org/10.3390/healthcare13121405
Chicago/Turabian StyleTong, Zhaozhen, Sinan Chen, Yuko Yamaguchi, Masahide Nakamura, Hsin-Yen Yen, and Shu-Chun Lee. 2025. "Vision-Based Assessment of Skeletal Muscle Decline: Correlating Gait Variance with SPPB Performance" Healthcare 13, no. 12: 1405. https://doi.org/10.3390/healthcare13121405
APA StyleTong, Z., Chen, S., Yamaguchi, Y., Nakamura, M., Yen, H.-Y., & Lee, S.-C. (2025). Vision-Based Assessment of Skeletal Muscle Decline: Correlating Gait Variance with SPPB Performance. Healthcare, 13(12), 1405. https://doi.org/10.3390/healthcare13121405








