Arthroscopic Management of Medial or Rotational Ankle Instability: A Comprehensive Review of Current Evidence
Abstract
1. Introduction
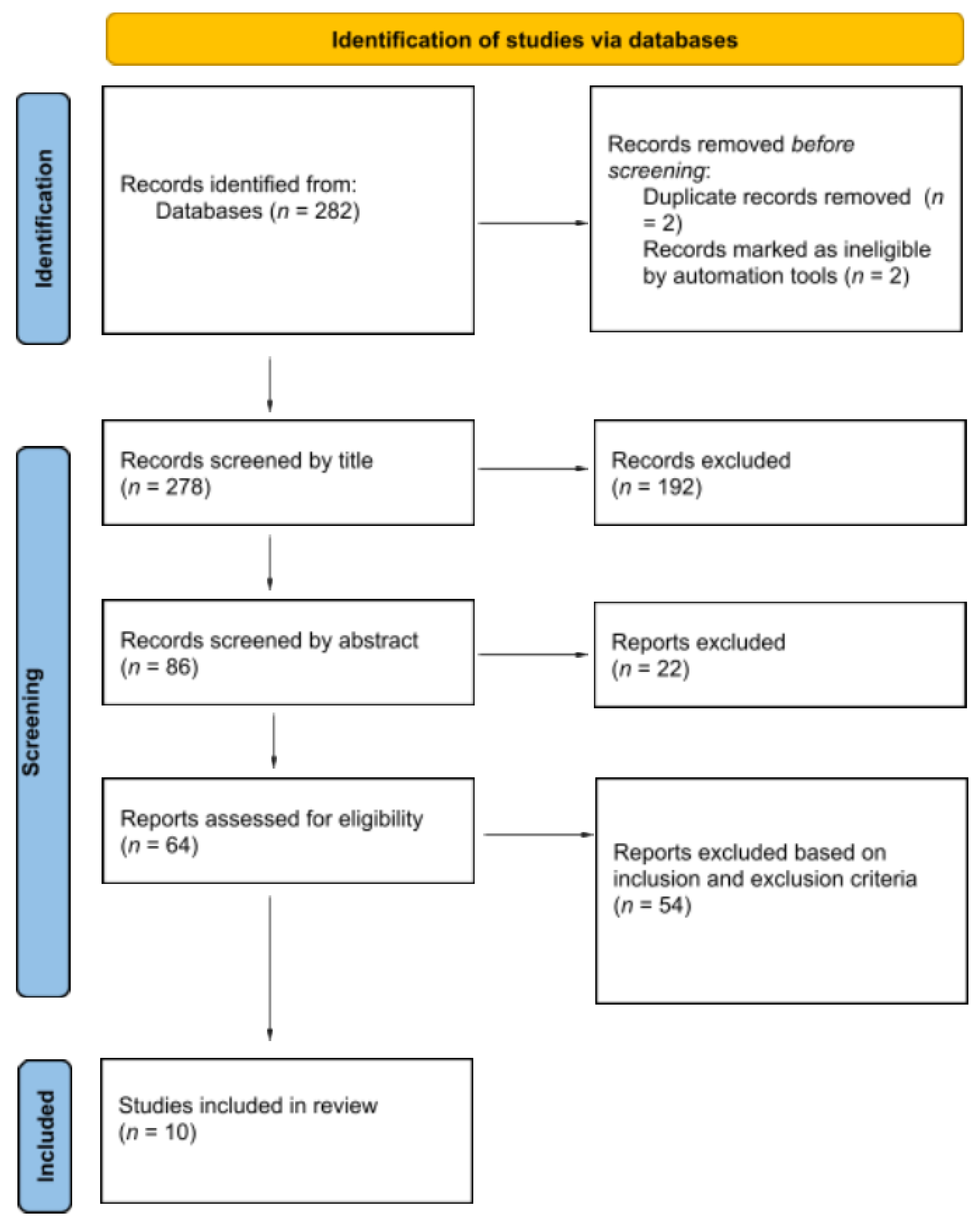
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Analysis
2.4. Extracted Variables and Outcomes
3. Results
3.1. Patient Demographics
3.2. Diagnosis and Cause of Instability
3.3. Associated Conditions
3.4. Management
3.5. Surgical Treatment and Additional Procedures
3.6. Post-Operative Protocol
3.7. Clinical Outcomes
3.8. Complications
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ATFL | Anterior talofibular ligament |
| CFL | Calcaneofibular ligament |
| CAI | Chronic ankle instability |
| RAI | Rotational ankle instability |
| MCL | Medial collateral ligament |
| MRI | Magnetic resonance imaging |
| AOFAS | American Orthopaedic Foot and Ankle Society |
| PROMs | Patient-reported outcome measures |
| EQ-5D | EuroQol-5 Dimensions |
| FAAM | Foot and Ankle Ability Measure |
| MINORS | Methodological Index for Non-Randomized Studies |
| ROM | Range of motion |
| IRB | Institutional Review Board |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analyses |
References
- Camacho, L.D.; Roward, Z.T.; Deng, Y.; Latt, L.D. Surgical Management of Lateral Ankle Instability in Athletes. J Athl Train. 2019, 54, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Mandarakas, M.; Pourkazemi, F.; Sman, A.; Burns, J.; Hiller, C.E. Systematic review of chronic ankle instability in children. J. Foot Ankle Res. 2014, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Van Rijn, R.M.; Van Os, A.G.; Bernsen, R.M.D.; Luijsterburg, P.A.; Koes, B.W.; Bierma-Zeinstra, S.M.A. What Is the Clinical Course of Acute Ankle Sprains? A Systematic Literature Review. Am. J. Med. 2008, 121, 324–331.e7. [Google Scholar] [CrossRef]
- DiGiovanni, B.F.; Partal, G.; Baumhauer, J.F. Acute ankle injury and chronic lateral instability in the athlete. Clin. Sports Med. 2004, 23, 1–19. [Google Scholar] [CrossRef]
- Chan, K.W.; Ding, B.C.; Mroczek, K.J. Acute and chronic lateral ankle instability in the athlete. Bull. NYU Hosp. Jt. Dis. 2011, 69, 17–26. [Google Scholar]
- Lauge-Hansen, N. Fractures of the ankle. III. Genetic roentgenologic diagnosis of fractures of the ankle. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1954, 71, 456–471. [Google Scholar] [PubMed]
- Gerber, J.P.; Williams, G.N.; Scoville, C.R.; Arciero, R.A.; Taylor, D.C. Persistent Disability Associated with Ankle Sprains: A Prospective Examination of an Athletic Population. Foot Ankle Int. 1998, 19, 653–660. [Google Scholar] [CrossRef]
- Ribbans, W.J.; Garde, A. Tibialis Posterior Tendon and Deltoid and Spring Ligament Injuries in the Elite Athlete. Foot Ankle Clin. 2013, 18, 255–291. [Google Scholar] [CrossRef]
- Hertel, J. Functional Anatomy, Pathomechanics, and Pathophysiology of Lateral Ankle Instability. J. Athl. Train. 2002, 37, 364–375. [Google Scholar]
- Gribble, P.A.; Delahunt, E.; Bleakley, C.; Caulfield, B.; Docherty, C.; Fourchet, F.; Fong, D.; Hertel, J.; Hiller, C.E.; Kaminski, T.W.; et al. Selection Criteria for Patients With Chronic Ankle Instability in Controlled Research: A Position Statement of the International Ankle Consortium. J. Orthop. Sports Phys. Ther. 2013, 43, 585–591. [Google Scholar] [CrossRef]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef] [PubMed]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.H.; Morris, B.L.; Saengsin, J.; Tourné, Y.; Guillo, S.; Guss, D.; DiGiovanni, C.W. Diagnosis and Treatment of Chronic Lateral Ankle Instability: Review of Our Biomechanical Evidence. J. Am. Acad. Orthop. Surg. 2021, 29, 3–16. [Google Scholar] [CrossRef]
- Hintermann, B.; Boss, A.; Schäfer, D. Arthroscopic Findings in Patients with Chronic Ankle Instability. Am. J. Sports Med. 2002, 30, 402–409. [Google Scholar] [CrossRef] [PubMed]
- Alparslan, L.; Chiodo, C. Lateral Ankle Instability: MR Imaging of Associated Injuries and Surgical Treatment Procedures. Semin. Musculoskelet. Radiol. 2008, 12, 346–358. [Google Scholar] [CrossRef]
- Crim, J.R.; Beals, T.C.; Nickisch, F.; Schannen, A.; Saltzman, C.L. Deltoid Ligament Abnormalities in Chronic Lateral Ankle Instability. Foot Ankle Int. 2011, 32, 873–878. [Google Scholar] [CrossRef]
- Hintermann, B.; Knupp, M.; Pagenstert, G.I. Deltoid Ligament Injuries: Diagnosis and Management. Foot Ankle Clin. 2006, 11, 625–637. [Google Scholar] [CrossRef]
- Schäfer, D.; Hintermann, B. Arthroscopic assessment of the chronic unstable ankle joint. Knee Surg. Sports Traumatol. Arthrosc. 1996, 4, 48–52. [Google Scholar] [CrossRef]
- Buchhorn, T.; Sabeti-Aschraf, M.; Dlaska, C.E.; Wenzel, F.; Graf, A.; Ziai, P. Combined Medial and Lateral Anatomic Ligament Reconstruction for Chronic Rotational Instability of the Ankle. Foot Ankle Int. 2011, 32, 1122–1126. [Google Scholar] [CrossRef]
- Caputo, A.M.; Lee, J.Y.; Spritzer, C.E.; Easley, M.E.; DeOrio, J.K.; Nunley, J.A.; DeFrate, L.E. In Vivo Kinematics of the Tibiotalar Joint After Lateral Ankle Instability. Am. J. Sports Med. 2009, 37, 2241–2248. [Google Scholar] [CrossRef]
- Vega, J.; Dalmau-Pastor, M. Anatomic Basis of Ankle Instability. Tech. Foot Ankle Surg. 2023, 22, 9–13. [Google Scholar] [CrossRef]
- Kim, J.G.; Gwak, H.C.; Lee, M.J.; Yoo, J.W.; Park, J.Y.; Yun, K.H.; Lee, Y.K. Arthroscopic Deltoid Repair: A Technical Tip. J. Foot Ankle Surg. 2017, 56, 1253–1256. [Google Scholar] [CrossRef]
- Vega, J.; Allmendinger, J.; Malagelada, F.; Guelfi, M.; Dalmau-Pastor, M. Combined arthroscopic all-inside repair of lateral and medial ankle ligaments is an effective treatment for rotational ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 132–140. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Mansur, N.S.B.; Lemos, A.V.K.C.; Baumfeld, D.S.; Baumfeld, T.S.; Prado, M.P.D.; Raduan, F.C.; Nery, C.A.S. Medial and Lateral Combined Ligament Arthroscopic Repair for Multidirectional Ankle Instability. Foot Ankle Orthop. 2021, 6, 2473011420986150. [Google Scholar] [CrossRef]
- Vega, J.; Malagelada, F.; Guelfi, M.; Dalmau-Pastor, M. Arthroscopic repair is an effective treatment for dynamic medial ankle instability secondary to posttraumatic and partial injury of the deltoid ligament deep fascicle. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3112–3120. [Google Scholar] [CrossRef]
- Seiça, E.C.; Mendes, D.; Sousa, M.R.; Vide, J. Deltoid ligament injuries: When and how to repair. Knee Surg Sports Traumatol. Arthrosc. 2024, 33, 1874–1883. [Google Scholar] [CrossRef]
- Li, H.; Xue, X.; Tong, J.; Li, H.; Hua, Y. Deltoid ligament (DL) repair produced better results than DL nonrepair for the treatment for rotational ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 2015–2022. [Google Scholar] [CrossRef]
- Lewis, T.L.; Ayathamattam, J.; Vignaraja, V.; Dalmau-Pastor, M.; Ferreira, G.F.; Nunes, G.A.; Ray, R. Improvement in clinical outcomes following arthroscopic all-inside medial lateral ligament reconstruction for rotational ankle instability. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3090–3096. [Google Scholar] [CrossRef]
- Hintermann, B.; Valderrabano, V.; Boss, A.; Trouillier, H.H.; Dick, W. Medial Ankle Instability: An Exploratory, Prospective Study of Fifty-Two Cases. Am. J. Sports Med. 2004, 32, 183–190. [Google Scholar] [CrossRef]
- Vega, J.; Malagelada, F.; Guelfi, M.; Dalmau-Pastor, M. Arthroscopic anterior deltoid plication with bone anchor is an effective procedure to control residual talar anterior translation after lateral ligament repair. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 2178–2183. [Google Scholar] [CrossRef] [PubMed]
- Guelfi, M.; Vega, J.; Dalmau-Pastor, M.; Malagelada, F.; Pantalone, A. Arthroscopic treatment of ankle multiligamentous injuries provides similar clinical outcomes to the treatment of isolated lateral ligament injury at the 2-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 3082–3089. [Google Scholar] [CrossRef]
- Gentile, M.A.; Rigby, R.B.; Fleming, J.; Taylor, S.; Lamba, C. Chronic medial ankle instability medial drive through sign and surgical repair technique. Foot Ankle Surg. Tech. Rep. Cases. 2022, 2, 100225. [Google Scholar] [CrossRef]
- Bocchino, G.; Grassa, D.; Bove, A.; Salvini, M.; Kaplan, R.; Di Gialleonardo, E.; Forconi, F.; Maccauro, G.; Vitiello, R. The Effects of Kinesio Tape on Acute Ankle Sprain: A Systematic Review. J. Clin. Med. 2025, 14, 1440. [Google Scholar] [CrossRef]
- Hu, D.; Sun, H.; Wang, S.; Wang, H.; Zheng, X.; Tang, H.; Hou, H. Treatment and prevention of chronic ankle instability: An umbrella review of meta-analyses. Foot Ankle Surg. 2025, 31, 111–125. [Google Scholar] [CrossRef] [PubMed]
- Hamlyn, C.; Docherty, C.L.; Klossner, J. Orthotic Intervention and Postural Stability in Participants With Functional Ankle Instability After an Accommodation Period. J. Athl. Train. 2012, 47, 130–135. [Google Scholar] [CrossRef]
- Li, C.C.H.; Lui, T.H. Arthroscopic Deltoid Ligament Reconstruction in Rotational Ankle Instability. Arthrosc. Tech. 2023, 12, e1179–e1184. [Google Scholar] [CrossRef]
- Krogsgaard, M.R.; Palm, H.; Obionu, K.; Astrup, Y.; Lange, N.B.; Haak, T.; Dippmann, C. Good rate of satisfaction but suboptimal clinical outcome at long-term follow-up in a large series of patients who had operative stabilization of the deltoid ligament of the ankle. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1524–1530. [Google Scholar] [CrossRef]
- Kim, S.H.; Lee, S.H.; Cha, J.Y.; Choi, S.W.; Lee, Y.K. Arthroscopic Deltoid Ligament Repair as a Potential Alternative Treatment for Ankle Deltoid Ligament Injury. J. Clin. Med. 2025, 14, 1662. [Google Scholar] [CrossRef]
- Tansey, P.J.; Castillo, I.; Panchbhavi, V.K. A Novel All-Inside Knotless Arthroscopic Deltoid Ligament Repair. Tech. Foot Ankle Surg. 2024, 23, 1–5. [Google Scholar] [CrossRef]
- Aicale, R.; Maffulli, N. Rotational ankle instability: A current concept review. J. Orthop. Surg. 2023, 31, 10225536231182347. [Google Scholar] [CrossRef] [PubMed]
- Loozen, L.; Veljkovic, A.; Younger, A. Deltoid ligament injury and repair. J. Orthop. Surg. 2023, 31, 10225536231182345. [Google Scholar] [CrossRef] [PubMed]
- Gonzalez, T.A.; Macaulay, A.A.; Ehrlichman, L.K.; Drummond, R.; Mittal, V.; DiGiovanni, C.W. Arthroscopically Assisted Versus Standard Open Reduction and Internal Fixation Techniques for the Acute Ankle Fracture. Foot Ankle Int. 2016, 37, 554–562. [Google Scholar] [CrossRef] [PubMed]
- Schrempf, J.; Baumbach, S.; Abdelatif, N.M.N.; Polzer, H.; Böcker, W. A systematic review on how to diagnose deltoid ligament injuries—Are we missing a uniform standard? BMC Musculoskelet. Disord. 2024, 25, 782. [Google Scholar] [CrossRef]
| Study Aspect | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Types of studies | 1. Therapeutic clinical studies evaluating arthroscopic lateral ankle ligament repair 2. Studies with retrospective or prospective design 3. Randomized and quasi-randomized controlled trials 4. Studies reporting preoperative and postoperative outcome scores 5. Minimum 12-month follow-up for all included patients 6. Published in peer-reviewed journals 7. Written in English 8. Full-text available | 1. Review articles 2. Case reports 3. Technique articles 4. Cadaveric studies 5. Animal studies 6. In vivo basic science studies |
| Types of participants | 1. Adult patients (≥18 years old) diagnosed with medial or rotational ankle instability 2. Patients undergoing arthroscopic ligament repair as primary or combined procedure | 1. Pediatric populations (<18 years old) 2. Patients treated non-operatively 3. Cases involving experimental or non-standard interventions |
| Types of interventions | 1. Arthroscopic surgical procedures for the treatment of medial ankle instability (including deltoid ligament repair or combined repairs) | 1. Open or hybrid procedures without an arthroscopic component 2. Non-surgical interventions 3. Experimental techniques not supported by outcome data |
| Authors | Type of Study | Number of Patients | Number of Ankles | Male | Female | Mean Age (Year) | Follow-Up (Month) |
|---|---|---|---|---|---|---|---|
| Mansur et al. [25] | Retrospective | 29 | 30 | 14 | 15 | 38 | 14.8 |
| Vega et al. [26] | Retrospective | 7 | 7 | ns | ns | 23 | 34 |
| Vega et al. [23] | Retrospective | 13 | 13 | 12 | 1 | 32 | 35 |
| Buchhorn et al. [19] | Prospective | 81 | 81 | 30 | 51 | 31.9 | 12 |
| Seiça et al. [27] | Retrospective | 39 | 39 | 23 | 16 | 40.1 | 21.3 |
| Li et al. [28] | Retrospective | 24 | 24 | 20 | 4 | 33 | 28 |
| Lewis et al. [29] | Prospective | 12 | 12 | 6 | 6 | 33.9 | 21 |
| Hintermann et al. [30] | Prospective | 51 | 52 | 27 | 25 | 36.4 | 52 |
| Vega et al. [31] | Prospective | 8 | 8 | 7 | 1 | 31 | 22 |
| Guelfi et al. [32] | Prospective | 25 | 25 | 16 | 9 | 27 | 24 |
| Total | 289 | 291 | 155 | 128 | 32.6 | 26.4 |
| Authors | Conservative Approach (Yes/No) | Duration of Conservative Approach (Month) | Surgical Approach | Additional Surgery | AOFAS SCORE | Complications |
|---|---|---|---|---|---|---|
| Mansur et al. [25] | Yes | 6 | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | Microfracture for osteochondral lesion of the talus peroneal tendoscopy Lateral internal bracing syndesmosis fixation | 91.9 | 1 peri-implant fracture 1 transient paresthesia 1 superficial infection 1 scar retraction |
| Vega et al. [26] | Yes | ns | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | Chondral talar lesion debridement [1] Osteophyte resection [5] Hindfoot endoscopy [3] | 100 | None |
| Vega et al. [23] | Yes | ns | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | Osteochondral talar lesion debridement and microfracture [2] Osteophyte resection [1] Posterior endoscopy [2] | 100 | None |
| Buchhorn et al. [19] | Yes | ns | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | ns | 94.1 | 4 delayed wound healing 1 hyperesthesia |
| Seiça et al. [27] | Yes | ns | 10: Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique; 10: Retensioning procedures | ns | 86.9 | 1 superficial wound dehiscence 4 ROM limitation 1 skin retraction 1 dysesthesia |
| Li et al. [28] | Yes | 6 | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | ns | 98 | None |
| Lewis et al. [29] | Yes | ns | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique | ns | ns | None |
| Hintermann et al. [30] | Yes | 7.1 | Arthroscopic all-inside medial and lateral ligament repair with a knotless suture anchor technique, augmentation with plantaris tendon graft if needed | Calcaneal lengthening osteotomy | 91.6 | None |
| Vega et al. [31] | Yes | 3 | Arthroscopic anterior deltoid plication with a bony anchor | Synovectomy and osteophyte resection [2] | 100 | None |
| Guelfi et al. [32] | Yes | 6 | Arthroscopic all-inside lateral and medial ligament repair with a knotless suture anchor technique | ATFL repaired with a knotless anchor | ns | None |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barbieri, C.; Bocchino, G.; Grassa, D.; Di Costa, D.; Gabrielli, E.; Forconi, F.; Maccauro, G.; Vitiello, R. Arthroscopic Management of Medial or Rotational Ankle Instability: A Comprehensive Review of Current Evidence. Healthcare 2025, 13, 1398. https://doi.org/10.3390/healthcare13121398
Barbieri C, Bocchino G, Grassa D, Di Costa D, Gabrielli E, Forconi F, Maccauro G, Vitiello R. Arthroscopic Management of Medial or Rotational Ankle Instability: A Comprehensive Review of Current Evidence. Healthcare. 2025; 13(12):1398. https://doi.org/10.3390/healthcare13121398
Chicago/Turabian StyleBarbieri, Chiara, Guido Bocchino, Daniele Grassa, Doriana Di Costa, Elena Gabrielli, Fabrizio Forconi, Giulio Maccauro, and Raffaele Vitiello. 2025. "Arthroscopic Management of Medial or Rotational Ankle Instability: A Comprehensive Review of Current Evidence" Healthcare 13, no. 12: 1398. https://doi.org/10.3390/healthcare13121398
APA StyleBarbieri, C., Bocchino, G., Grassa, D., Di Costa, D., Gabrielli, E., Forconi, F., Maccauro, G., & Vitiello, R. (2025). Arthroscopic Management of Medial or Rotational Ankle Instability: A Comprehensive Review of Current Evidence. Healthcare, 13(12), 1398. https://doi.org/10.3390/healthcare13121398






