Leg Length Discrepancy After Total Hip Arthroplasty: A Review of Clinical Assessments, Imaging Diagnostics, and Medico-Legal Implications
Abstract
1. Introduction
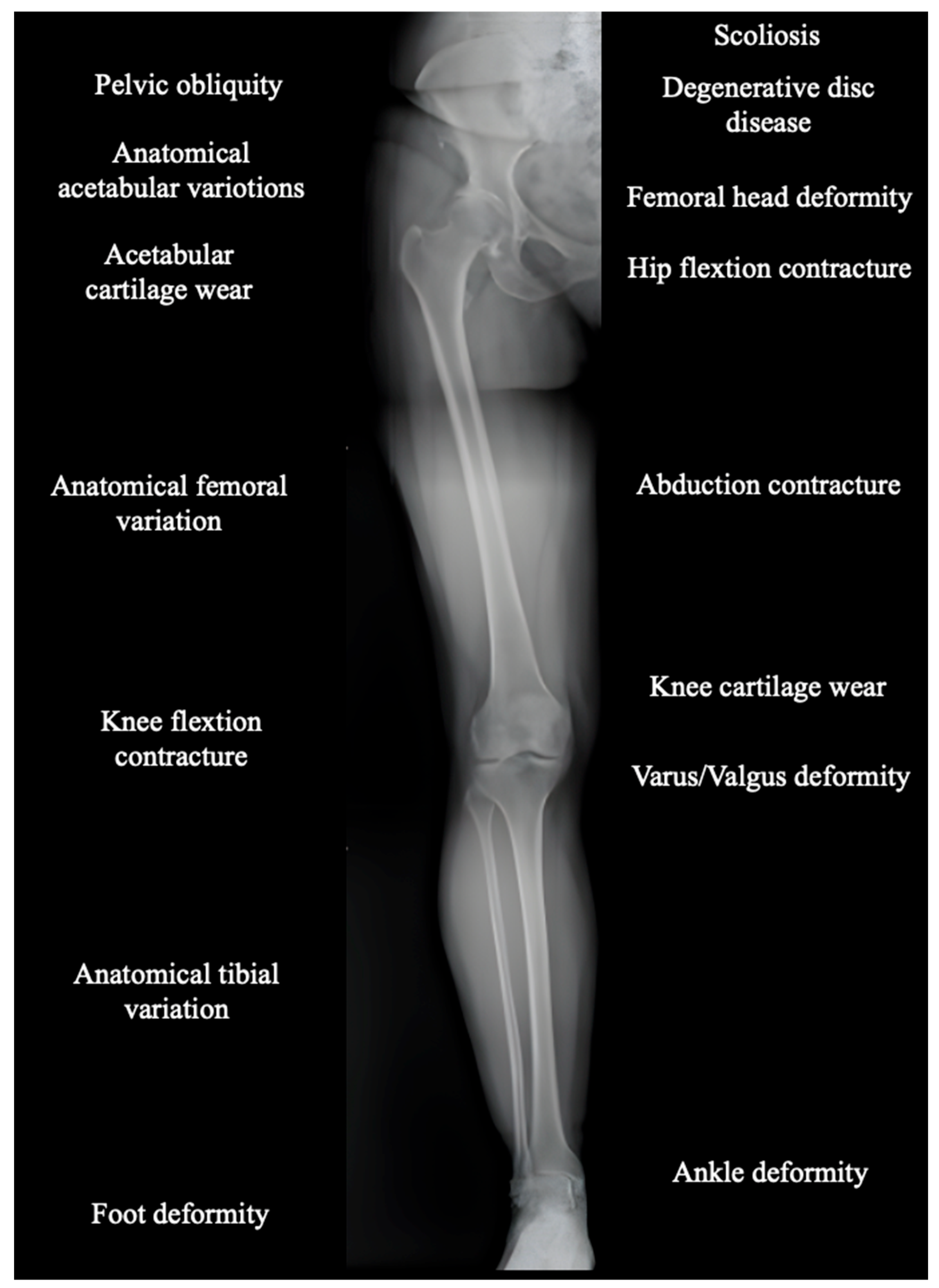
2. Anatomical and Functional Lower Limb Discrepancy: Definition and Assessment
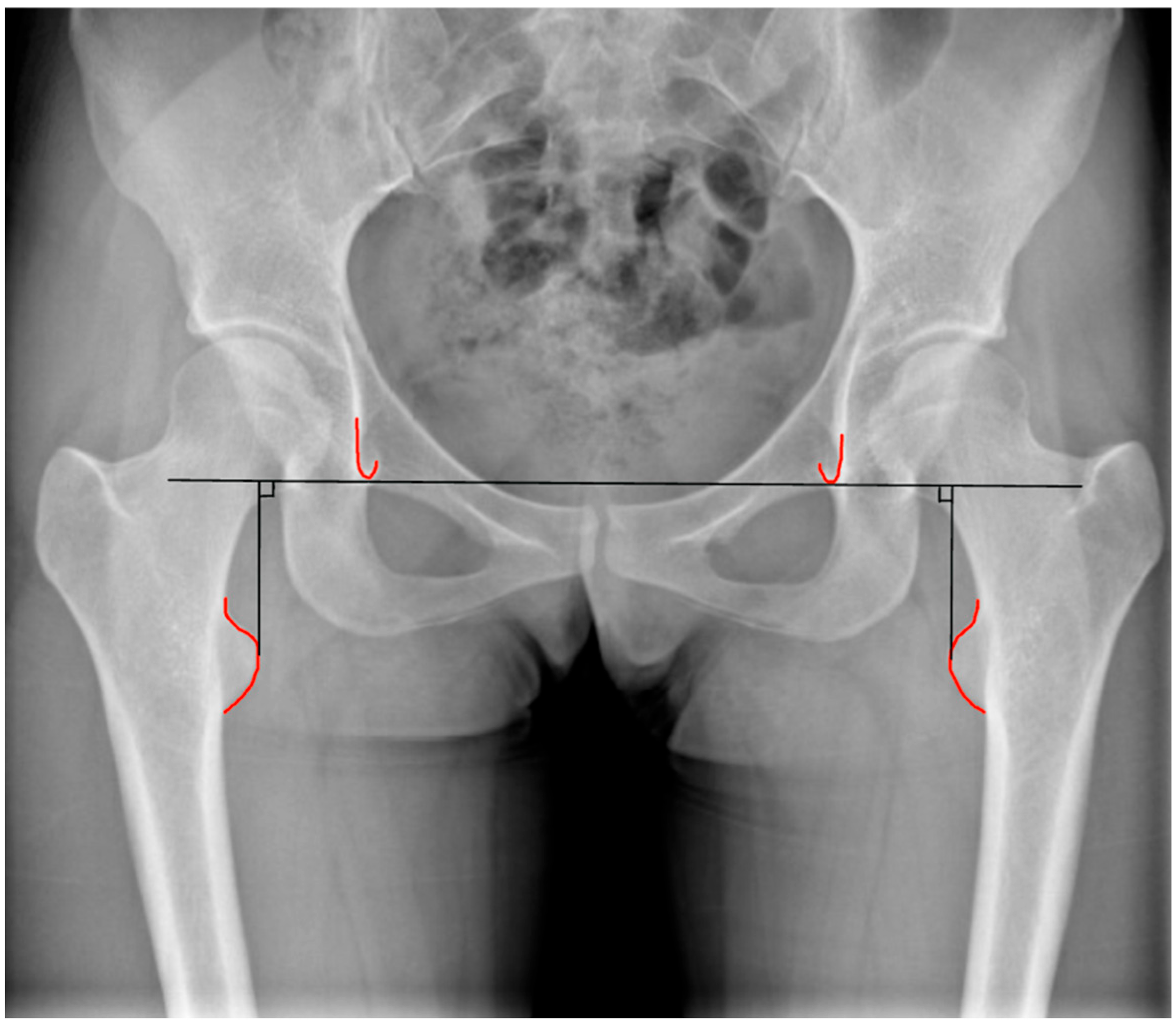
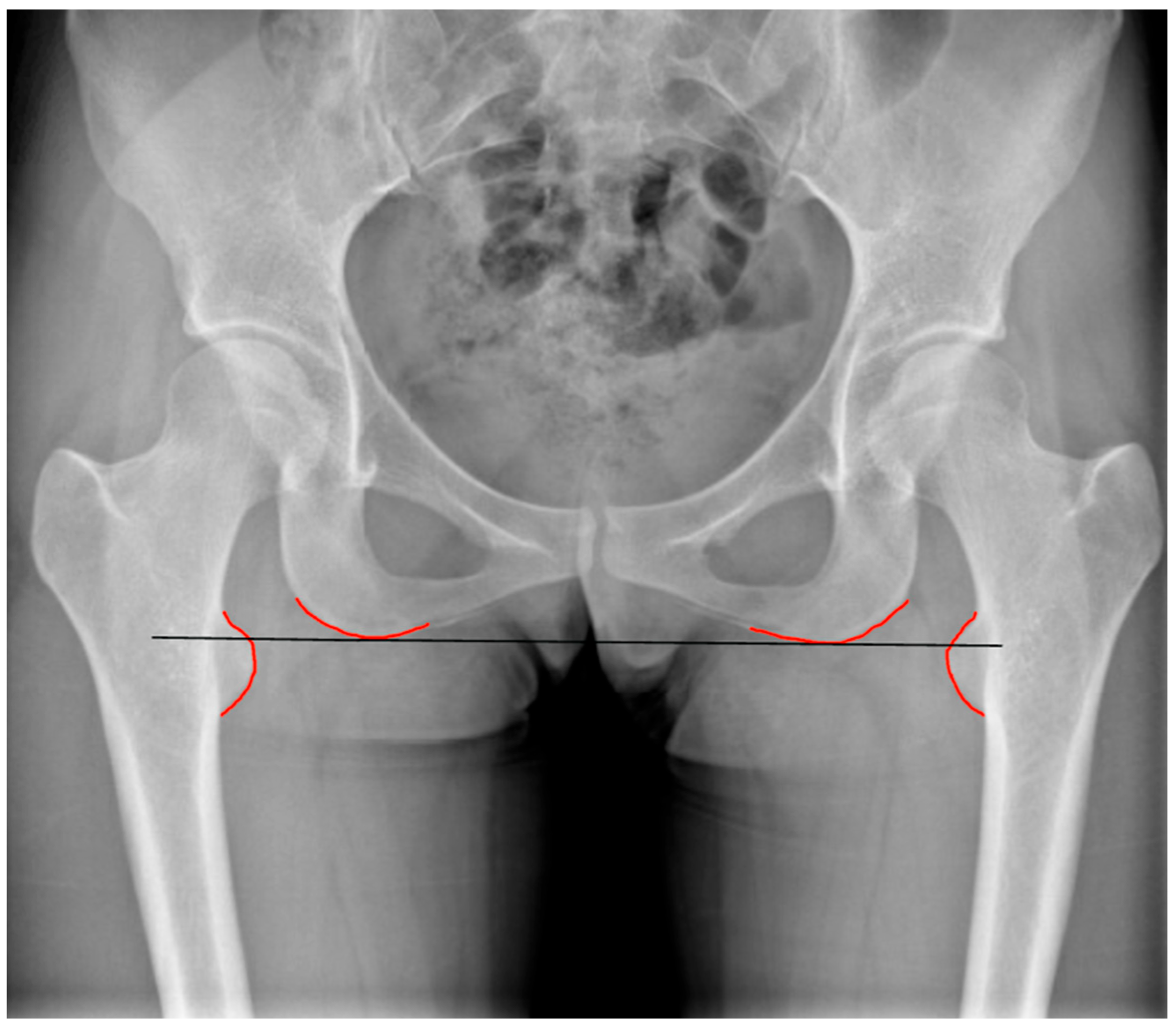
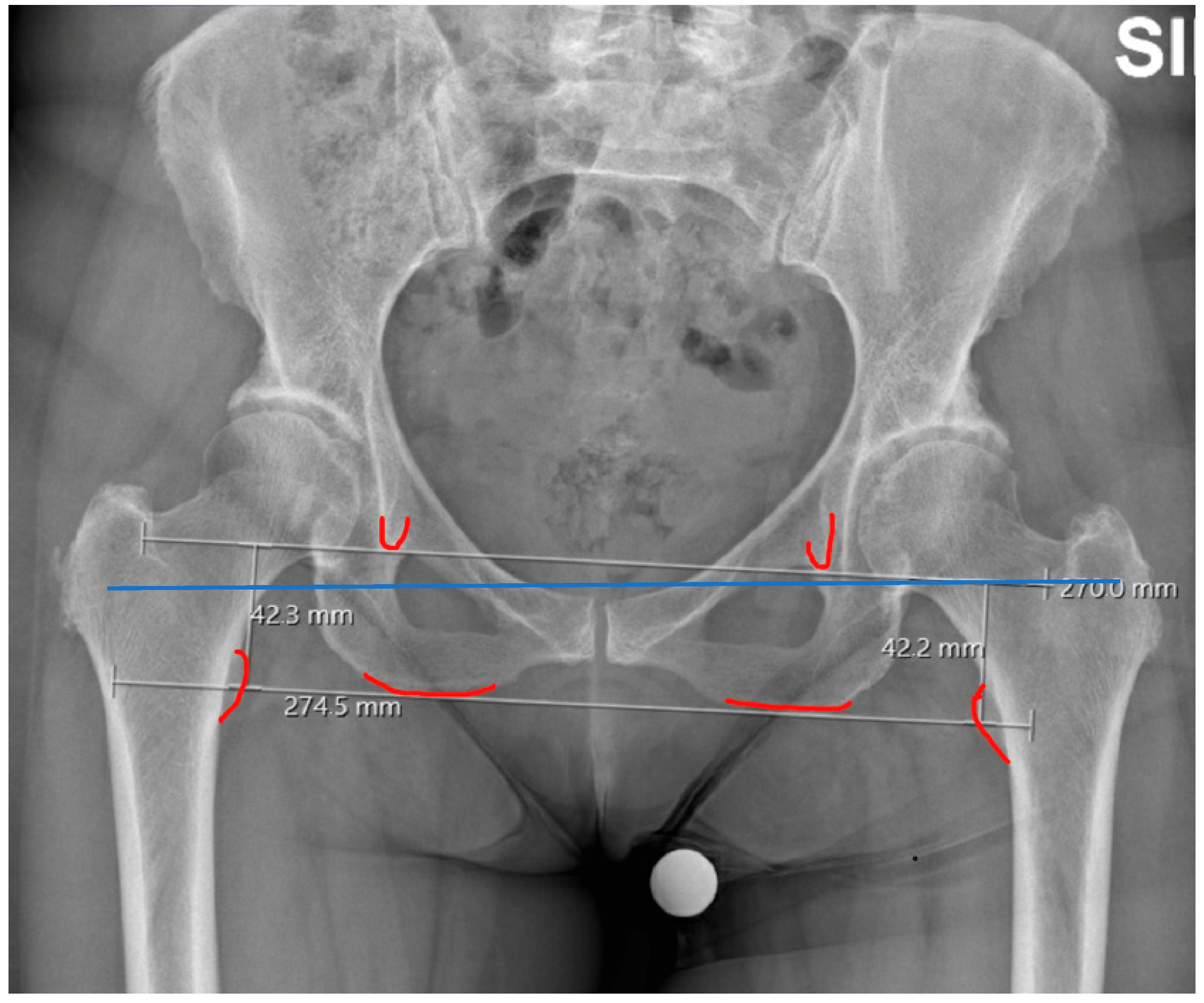
3. Lower Limb Discrepancy in THA
4. Preoperative Planning and Intraoperative Assessment
5. Clinical Relevance of Lower Limb Discrepancy
6. Medico-Legal Considerations
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Knight, S.R.; Aujla, R.; Biswas, S.P. Total Hip Arthroplasty—Over 100 years of operative history. Orthop. Rev. 2011, 3, e16. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Anderson, C.G.; Jang, S.J.; Brilliant, Z.R.; Mayman, D.J.; Vigdorchik, J.M.; Jerabek, S.A.; Sculco, P.K. Complication Rate After Primary Total Hip Arthroplasty Using the Posterior Approach and Enabling Technology: A Consecutive Series of 2888 Hips. J. Arthroplast. 2023, 38, S119–S123.e3. [Google Scholar] [CrossRef] [PubMed]
- Lecoanet, P.; Vargas, M.; Pallaro, J.; Thelen, T.; Ribes, C.; Fabre, T. Leg length discrepancy after total hip arthroplasty: Can leg length be satisfactorily controlled via anterior approach without a traction table? Evaluation in 56 patients with EOS 3D. Orthop. Traumatol. Surg. Res. 2018, 104, 1143–1148. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.S.; Dramis, A.; Board, T.N. Leg length discrepancy after total hip arthroplasty: A review of literature. Curr. Rev. Musculoskelet. Med. 2013, 6, 336–341. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gheewala, R.A.; Young, J.R.; Villacres Mori, B.; Lakra, A.; DiCaprio, M.R. Perioperative management of leg-length discrepancy in total hip arthroplasty: A review. Arch. Orthop. Trauma. Surg. 2023, 143, 5417–5423. [Google Scholar] [CrossRef] [PubMed]
- Wylde, V.; Whitehouse, S.L.; Taylor, A.H.; Pattison, G.T.; Bannister, G.C.; Blom, A.W. Prevalence and functional impact of patient-perceived leg length discrepancy after hip replacement. Int. Orthop. 2009, 33, 905–909. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Basile, G.; Calori, G.M.; Bianco Prevot, L.; Fozzato, S.; Ragona, M.; Chiodi, B.; Montanari, E.; Amadei, F.; Leigheb, M.; Montana, A. The main causes of orthopedics and traumatology litigation in Italy: State of the art and review of the literature. Minerva Orthop. 2024, 75, 153–162. [Google Scholar] [CrossRef]
- Attarian, D.E.; Vail, T.P. Medicolegal aspects of hip and knee arthroplasty. Clin. Orthop. Relat. Res. 2005, 433, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C. Leg length discrepancy after primary total hip replacement. Musculoskelet. Surg. 2023, 107, 1–5. [Google Scholar] [CrossRef]
- Flecher, X.; Ollivier, M.; Argenson, J.N. Lower limb length and offset in total hip arthroplasty. Orthop. Traumatol. Surg. Res. 2016, 102 (Suppl. 1), S9–S20. [Google Scholar] [CrossRef] [PubMed]
- Meermans, G.; Malik, A.; Witt, J.; Haddad, F. Preoperative radiographic assessment of limb-length discrepancy in total hip arthroplasty. Clin. Orthop. Relat. Res. 2011, 469, 1677–1682. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tsai, C.J.; Yang, Z.Y.; Wu, T.Y.; Tsai, Y.T.; Wang, J.J.; Liaw, C.K. The Transverse Mechanical Axis of the Pelvis for Post-Operative Evaluation of Total Hip Arthroplasty. Biomedicines 2023, 11, 1397. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Moharrami, A.; Mirghaderi, P.; Hoseini Zare, N.; Moazen-Jamshidi, M.M.; Ebrahimian, M.; Mortazavi, S.M.J. Slight pelvic obliquity is normal in a healthy population: A cross-sectional study. J. Exp. Orthop. 2023, 10, 57. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hamad, M.N.; Livshetz, I.; Sood, A.; Patetta, M.; Gonzalez, M.H.; Amirouche, F.A. Effects of pelvic obliquity and limb position on radiographic leg length discrepancy measurement: A Sawbones model. J. Exp. Orthop. 2022, 9, 71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fujita, T.; Hamai, S.; Hara, D.; Kawahara, S.; Yamaguchi, R.; Ikemura, S.; Motomura, G.; Kawaguchi, K.; Nakashima, Y. Trendelenburg gait after total hip arthroplasty due to reduced muscle contraction of the hip abductors and extensors. J. Orthop. 2024, 59, 57–63. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sathappan, S.S.; Ginat, D.; Patel, V.; Walsh, M.; Jaffe, W.L.; Di Cesare, P.E. Effect of anaesthesia type on limb length discrepancy after total hip arthroplasty. J. Arthroplast. 2008, 23, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Love, B.R.T.; Wright, K. Leg length discrepancy after total hip replacement. Proceedings of Australian Orthopaedic association. J. Bone Jt. Surg. Br. 1983, 65, 103. [Google Scholar]
- Williamson, J.A.; Reckling, F.W. Limb length discrepancy and related problems following total hip replacement. Clin. Orthop. Relat. Res. 1978, 202, 135–138. [Google Scholar] [CrossRef]
- Abouelela, A.; Mubark, I.; Nagy, M.; Hind, J.; Jayakumar, N.; Ashwood, N.; Bindi, F. Limb Length Inequality in Patients After Primary Total Hip Arthroplasty: Analysis of Radiological Assessment and Influencing Risk Factors Based on a District General Hospital Experience of 338 Cases. Cureus 2021, 13, e19986. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Gallo, M.C.; Chung, B.C.; Tucker, D.W.; Piple, A.S.; Christ, A.B.; Lieberman, J.R.; Heckmann, N.D. Limb Length Discrepancy in Total Hip Arthroplasty: Is the Lesser Trochanter a Reliable Measure of Leg Length? J. Arthroplast. 2021, 36, 3593–3600. [Google Scholar] [CrossRef] [PubMed]
- Jasty, M.; Webster, W.; Harris, W. Management of limb length inequality during total hip replacement. Clin. Orthop. Relat. Res. 1996, 333, 165–171. [Google Scholar] [CrossRef]
- Cuckler, J.M. Limb length and stability in total hip replacement. Orthopedics 2005, 28, 951–953. [Google Scholar] [CrossRef] [PubMed]
- Edeen, J.; Sharkey, P.F.; Alexander, A.H. Clinical significance of leg-length inequality after total hip arthroplasty. Am. J. Orthop. 1995, 24, 347–351. [Google Scholar] [PubMed]
- Alfuth, M.; Fichter, P.; Knicker, A. Leg length discrepancy: A systematic review on the validity and reliability of clinical assessments and imaging diagnostics used in clinical practice. PLoS ONE 2021, 16, e0261457. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Reinbacher, P.; Smolle, M.A.; Friesenbichler, J.; Draschl, A.; Leithner, A.; Maurer-Ertl, W. Pre-operative templating in THA using a short stem system: Precision and accuracy of 2D versus 3D planning method. J. Orthop. Traumatol. 2022, 23, 16. [Google Scholar] [CrossRef]
- Charnley, J. Low Friction Arthroplasty of the Hip: Theory and Practice; Springer: New York, NY, USA, 1979. [Google Scholar]
- Tassinari, L.; Di Martino, A.; Brunello, M.; Rossomando, V.; Traina, F.; Faldini, C. Leg length discrepancy after total hip arthroplasty performed by direct anterior approach: A systematic review comparing surgical approaches and strategies for prevention. EFORT Open Rev. 2024, 9, 733–744. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Takigami, I.; Itokazu, M.; Itoh, Y.; Matsumoto, K.; Yamamoto, T.; Shimizu, K. Limb-length measurement in total hip arthroplasty using a calipers dual pin retractor. Bull. NYU Hosp. Jt. Dis. 2008, 66, 107–110. [Google Scholar] [PubMed]
- Sarin, V.K.; Pratt, W.R.; Bradley, G.W. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J. Arthroplast. 2005, 20, 887–891. [Google Scholar] [CrossRef] [PubMed]
- Papadopoulos, D.V.; Koulouvaris, P.; Aggelidakis, G.C.; Tsantes, A.G.; Lykissas, M.G.; Mavrodontidis, A. Intraoperative measurement of limb lengthening during total hip arthroplasty. Indian. J. Orthop. 2017, 51, 162–167. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lambers, A.P.; Marley, M.A.; Jennings, R.; Bucknill, A. Accuracy of Leg Length and Offset Measurements During Total Hip Arthroplasty Using an Imageless Navigation System. Cureus 2023, 15, e38689. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ogawa, K.; Kabata, T.; Maeda, T.; Kajino, Y.; Tsuchiya, H. Accurate leg length measurement in total hip arthroplasty: A comparison of computer navigation and a simple manual measurement device. Clin. Orthop. Surg. 2014, 6, 153–158. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Halawi, M.J.; Jongbloed, W.; Baron, S.; Savoy, L.; Williams, V.J.; Cote, M.P. Patient Dissatisfaction After Primary Total Joint Arthroplasty: The Patient Perspective. J. Arthroplast. 2019, 34, 1093–1096. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, S.; Kernohan, G.; Fitzpatrick, C.; Hill, J.; Beverland, D. Perception of imposed leg length inequality in normal subjects. Hip Int. 2010, 20, 505–511. [Google Scholar] [CrossRef]
- Rannisto, S.; Okuloff, A.; Uitti, J.; Paananen, M.; Rannisto, P.H.; Malmivaara, A.; Karppinen, J. Leg-length discrepancy is associated with low back pain among those who must stand while working. BMC Musculoskelet. Disord. 2015, 16, 110. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Applebaum, A.; Nessim, A.; Cho, W. Overview and Spinal Implications of Leg Length Discrepancy: Narrative Review. Clin. Orthop. Surg. 2021, 13, 127–134. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kim, C.; Nevitt, M.; Guermazi, A.; Niu, J.; Clancy, M.; Tolstykh, I.; Jungmann, P.M.; Lane, N.E.; Segal, N.A.; Harvey, W.F.; et al. Brief Report: Leg Length Inequality and Hip Osteoarthritis in the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheumatol. 2018, 70, 1572–1576. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Röder, C.; Vogel, R.; Burri, L.; Dietrich, D.; Staub, L.P. Total hip arthroplasty: Leg length inequality impairs functional outcomes and patient satisfaction. BMC Musculoskelet. Disord. 2012, 13, 95. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Parvizi, J.; Sharkey, P.F.; Bissett, G.A.; Rothman, R.H.; Hozack, W.J. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J. Bone Jt. Surg. Am. 2003, 85, 2310–2317. [Google Scholar] [CrossRef]
- Keršič, M.; Dolinar, D.; Antolič, V.; Mavčič, B. The impact of leg length discrepancy on clinical outcome of total hip arthroplasty: Comparison of four measurement methods. J. Arthroplast. 2014, 29, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Schöner, L.; Steinbeck, V.; Busse, R.; Marques, C.J. Satisfied with the worst health outcomes or unsatisfied with the best: Explaining the divergence between good patient-reported outcomes and low satisfaction and vice versa among knee arthroplasty patients—A retrospective cohort study. J. Orthop. Surg. Res. 2025, 20, 88. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Hofmann, A.A.; Skrzynski, M.C. Leg length inequality and nerve palsy in total hip arthroplasty: A lawyer awaits! Orthopaedics 2000, 23, 943–944. [Google Scholar] [CrossRef] [PubMed]
- Majeed, H. Litigations in trauma and orthopaedic surgery: Analysis and outcomes of medicolegal claims during the last 10 years in the United Kingdom National Health Service. EFORT Open Rev. 2021, 6, 152–159. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ingravallo, F.; Cerquetti, I.; Vignatelli, L.; Albertini, S.; Bolcato, M.; Camerlingo, M.; Corbi, G.; De Leo, D.; De Nicolò, A.; De Stefano, F.; et al. Medico-legal assessment of personal damage in older people: Report from a multidisciplinary consensus conference. Int. J. Leg. Med. 2020, 134, 2319–2334. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cruz-Medel, I.; Rodrigues-de-Souza, D.P.; Alburquerque-Sendín, F. Comprehensive Analysis of Pelvic Asymmetries in Low Back Pain, Scoliosis, Post-Traumatic Pelvic Dysfunctions and Obstetric Changes: A Narrative Review Focused on Clinical Relevance. Symmetry 2024, 16, 1304. [Google Scholar] [CrossRef]
- Kokubu, Y.; Kawahara, S.; Ayabe, Y.; Motomura, G.; Hamai, S.; Hara, T.; Nakashima, Y. Evaluation of Leg Length Difference on Perioperative Radiographs of Total Hip Arthroplasty Considering Lower Limb Malposition. Cureus 2024, 16, e70790. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Coble, T.J.; Jestus, J.W.; Bell, J.A.; Weller, W.J.; Calandruccio, J.H. Maintaining Professionalism in the Difficult Patient Interaction. Orthop. Clin. N. Am. 2025, 56, 59–66. [Google Scholar] [CrossRef] [PubMed]
- Sabharwal, S.; Kumar, A. Methods for assessing leg length discrepancy. Clin. Orthop. Relat. Res. 2008, 466, 2910–2922. [Google Scholar] [CrossRef]
- Hardwick-Morris, M.; Wigmore, E.; Twiggs, J.; Miles, B.; Jones, C.W.; Yates, P.J. Leg length discrepancy assessment in total hip arthroplasty: Is a pelvic radiograph sufficient? Bone Jt. Open. 2022, 3, 960–968. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wu, J.; Zhuang, X.; Lin, C.; He, L.; Zhang, R. Does the use of intraoperative measurement reduce limb length discrepancies after total hip arthroplasty? BMC Musculoskelet. Disord. 2023, 24, 648. [Google Scholar] [CrossRef]
- Basile, G. The autobiographical narrative as a damage assessment means: Injuries to profound subjective sensitivities—Personalization and objectivization of medicolegal relevance. Clin. Ter. 2022, 173, 585–589. [Google Scholar] [CrossRef] [PubMed]
- Aubert, T.; Galanzino, G.; Gerard, P.; Le Strat, V.; Rigoulot, G.; Lhotellier, L. Accuracy of Preoperative 3D vs 2D Digital Templating for Cementless Total Hip Arthroplasty Using a Direct Anterior Approach. Arthroplast. Today 2023, 24, 101260. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sullivan, J.D. The medico-legal expertise: Solid medicine, sufficient legal and a measure of common sense. Mcgill J. Med. 2006, 9, 147–151. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bianco Prevot, L.; Tronconi, L.P.; Bolcato, V.; Accetta, R.; Di Mauro, L.; Basile, G. Leg Length Discrepancy After Total Hip Arthroplasty: A Review of Clinical Assessments, Imaging Diagnostics, and Medico-Legal Implications. Healthcare 2025, 13, 1358. https://doi.org/10.3390/healthcare13121358
Bianco Prevot L, Tronconi LP, Bolcato V, Accetta R, Di Mauro L, Basile G. Leg Length Discrepancy After Total Hip Arthroplasty: A Review of Clinical Assessments, Imaging Diagnostics, and Medico-Legal Implications. Healthcare. 2025; 13(12):1358. https://doi.org/10.3390/healthcare13121358
Chicago/Turabian StyleBianco Prevot, Luca, Livio Pietro Tronconi, Vittorio Bolcato, Riccardo Accetta, Lucio Di Mauro, and Giuseppe Basile. 2025. "Leg Length Discrepancy After Total Hip Arthroplasty: A Review of Clinical Assessments, Imaging Diagnostics, and Medico-Legal Implications" Healthcare 13, no. 12: 1358. https://doi.org/10.3390/healthcare13121358
APA StyleBianco Prevot, L., Tronconi, L. P., Bolcato, V., Accetta, R., Di Mauro, L., & Basile, G. (2025). Leg Length Discrepancy After Total Hip Arthroplasty: A Review of Clinical Assessments, Imaging Diagnostics, and Medico-Legal Implications. Healthcare, 13(12), 1358. https://doi.org/10.3390/healthcare13121358








