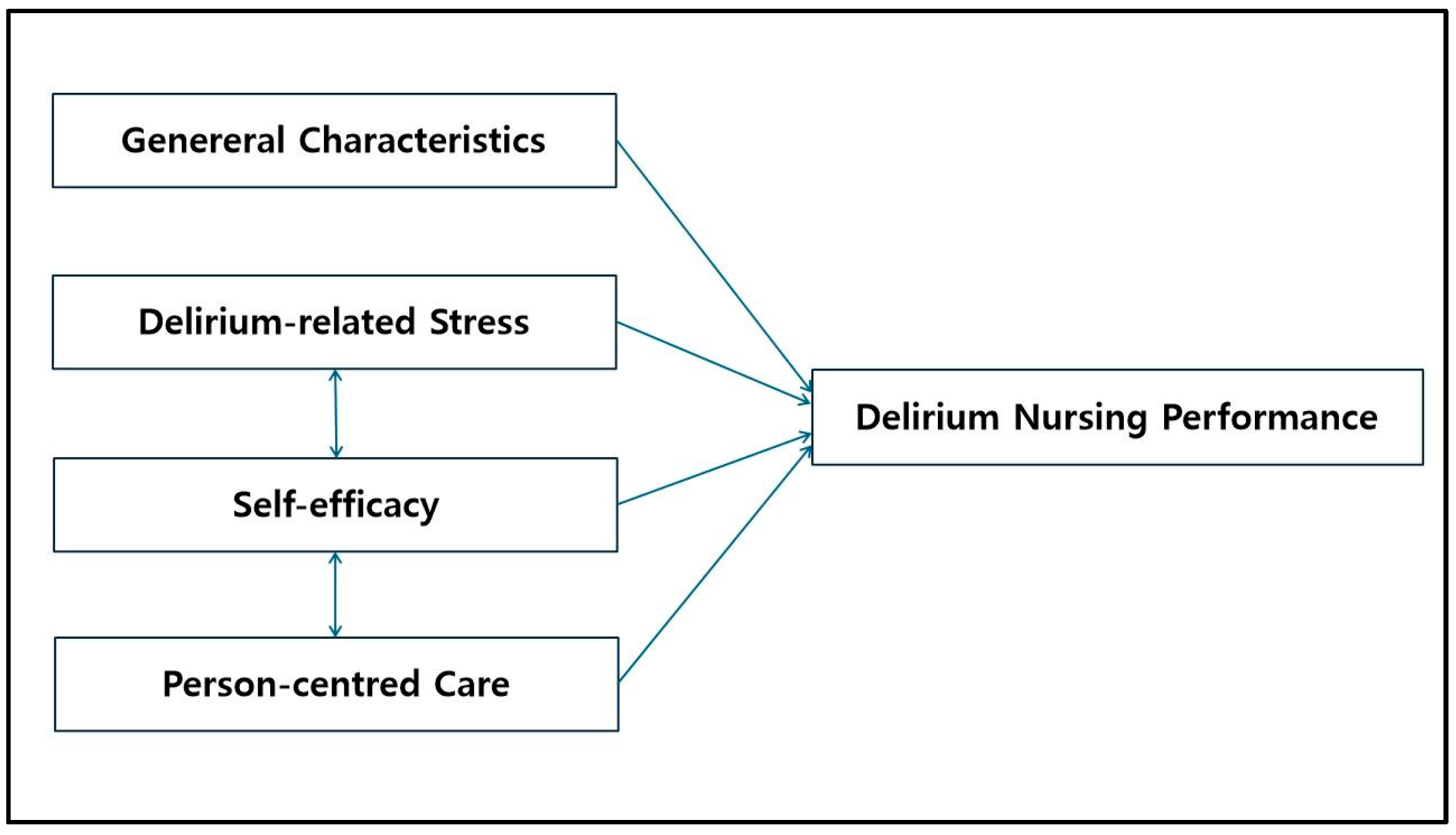
Impact of Delirium-Related Stress, Self-Efficacy, Person-Centred Care on Delirium Nursing Performance Among Nurses in Trauma Intensive Care Units: A Cross-Sectional Descriptive Survey Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Study Tools
2.3.1. General Characteristics
2.3.2. Delirium-Related Stress
2.3.3. Self-Efficacy
2.3.4. Person-Centred Care
2.3.5. Delirium Nursing Performance
2.4. Data Collection
2.5. Ethical Considerations
2.6. Data Analysis
3. Results
3.1. Differences in Delirium Nursing Performance According to Participants’ General Characteristics
3.2. Scores of Delirium-Related Stress, Self-Efficacy, Person-Centred Care, and Delirium Nursing Performance
3.3. Correlation of Delirium-Related Stress, Self-Efficacy, and Person-Centred Care with Delirium Nursing Performance in Participants
3.4. Factors Influencing Delirium Nursing Performance
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistics Korea. Status of Emergency Medical Treatment Outcomes for Severe Trauma (ICISS_2015 Based) Patients by Gender and Age. Available online: https://kosis.kr/statHtml/statHtml.do?orgId=411&tblId=DT_41104_3374&conn_path=I2 (accessed on 10 June 2024).
- Kim, N.Y.; Ryu, S.A.; Kim, Y.H. Factors related to delirium of intensive care unit patients in Korea: A systematic review. Iran. J. Public Health 2021, 50, 1526–1535. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Mo, L.; Hu, H.; Ou, Y.; Luo, J. Risk factors of postoperative delirium after cardiac surgery: A meta-analysis. J. Cardiothorac. Surg. 2021, 16, 113. [Google Scholar] [CrossRef]
- Denk, A.; Müller, K.; Schlosser, S.; Heissner, K.; Gülow, K.; Müller, M.; Schmid, S. Liver diseases as a novel risk factor for delirium in the ICU-Delirium and hepatic encephalopathy are two distinct entities. PLoS ONE 2022, 17, e0276914. [Google Scholar] [CrossRef]
- Roberson, S.W.; Patel, M.B.; Dabrowski, W.; Ely, E.W.; Pakulski, C.; Kotfis, K. Challenges of delirium management in patients with traumatic brain injury: From pathophysiology to clinical practice. Curr. Neuropharmacol. 2021, 19, 1519–1544. [Google Scholar] [CrossRef] [PubMed]
- Youn, S.H.; Son, H.S.; Kim, J.; Jung, K.; Moon, J.; Huh, Y.; Kim, Y. Trauma versus nontrauma intensive care unit nursing: A workload comparison. J. Trauma Nurs. 2020, 27, 346–350. [Google Scholar] [CrossRef] [PubMed]
- McArthur, K.; Krause, C.; Kwon, E.; Luo-Owen, X.; Cochran-Yu, M.; Swentek, L.; Burruss, S.; Turay, D.; Krasnoff, C.; Grigorian, A.; et al. Trauma and nontrauma damage-control laparotomy: The difference is delirium (data from the Eastern Association for the Surgery of Trauma SLEEP-TIME multicenter trial). J. Trauma Acute Care Surg. 2021, 91, 100–107. [Google Scholar] [CrossRef]
- Gravante, F.; Giannarelli, D.; Pucci, A.; Gagliardi, A.M.; Mitello, L.; Montagna, A.; Latina, R. Prevalence and risk factors of delirium in the intensive care unit: An observational study. Nurs. Crit. Care 2021, 26, 156–165. [Google Scholar] [CrossRef]
- Ali, M.A.; Hashmi, M.; Ahmed, W.; Raza, S.A.; Khan, M.F.; Salim, B. Incidence and risk factors of delirium in surgical intensive care unit. Trauma Surg. Acute Care Open 2021, 6, e000564. [Google Scholar] [CrossRef]
- Stollings, J.L.; Kotfis, K.; Chanques, G.; Pun, B.T.; Pandharipande, P.P.; Ely, E.W. Delirium in critical illness: Clinical manifestations, outcomes, and management. Intensive Care Med. 2021, 47, 1089–1103. [Google Scholar] [CrossRef]
- Alhalaiqa, F.; Masa’Deh, R.; Al Omari, O.; Shawashreh, A.; Khalifeh, A.H.; Gray, R. The impact of an educational programme on Jordanian intensive care nurses’ knowledge, attitudes, and practice regarding delirium and their levels of self-efficacy: A quasi-experimental design. Iran. J. Nurs. Midwifery Res. 2023, 28, 312–319. [Google Scholar] [CrossRef]
- Yang, Y.A. ICU Nurses’ Knowledge and Nursing Performance on Patients’ Symptoms of Delirium. Master’s Thesis, Catholic University, Seoul, Republic of Korea, 2006. [Google Scholar]
- Chow, S.K.Y.; Chan, S.C. Appraising the factors associated with delirium care behaviours and barriers to their assessment among clinical nurses: A cross-sectional study. Int. J. Environ. Res. Public Health 2024, 21, 1582. [Google Scholar] [CrossRef]
- Thomas, N.; Coleman, M.; Terry, D. Nurses’ experience of caring for patients with delirium: Systematic review and qualitative evidence synthesis. Nurs. Rep. 2021, 11, 164–174. [Google Scholar] [CrossRef] [PubMed]
- Ban, W.J.; Lee, J.M.; Nam, S.H. Influence of emergence delirium-related knowledge and nursing stress, practice, and confidence levels on the performance of recovery room nurses: A cross-sectional study. PLoS ONE 2024, 19, e0314575. [Google Scholar] [CrossRef]
- Wang, Y.; Li, L.; Tan, S.; Guan, Y.; Luo, X. Psychological stress and associated factors in caring for patients with delirium among intensive care unit nurses: A cross-sectional study. Aust. Crit. Care 2023, 36, 793–798. [Google Scholar] [CrossRef] [PubMed]
- Nie, J.; Li, W.J.; Jiang, Z.Y. Self-efficacy of ICU nurses in delirium care: An analysis of the current status and influencing factors. BMC Nurs. 2024, 23, 773. [Google Scholar] [CrossRef]
- Koo, H.J.; Yang, J.H. Factors influencing performance of delirium care for postoperative delirium of elderly patients among recovery room nurses. J. Korean Acad. Soc. Nurs. Educ. 2016, 22, 387–395. [Google Scholar] [CrossRef]
- Chang, Y.L.; Hsieh, M.J.; Chang, Y.C.; Yeh, S.L.; Chen, S.W.; Tsai, Y.F. Self-efficacy of caring for patients in the intensive care unit with delirium: Development and validation of a scale for intensive care unit nurses. Aust. Crit. Care 2023, 36, 449–454. [Google Scholar] [CrossRef] [PubMed]
- Kvande, M.E.; Angel, S.; Højager Nielsen, A. Humanizing intensive care: A scoping review (HumanIC). Nurs. Ethics 2022, 29, 498–510. [Google Scholar] [CrossRef]
- Seo, M.H.; Kim, E.A.; Kim, H.R. How the nursing work environment moderates the relationship between clinical judgment and person-centered care among intensive care unit nurses. PLoS ONE 2025, 20, e0316654. [Google Scholar] [CrossRef]
- Park, Y.S. The Development and Effects of Evidence-Based Nursing Practice Guideline for the Nursing of Delirium in Cancer Patients. Ph.D. Thesis, Gyeongsang National University, Jinju, Republic of Korea, 2011. [Google Scholar]
- von der Lühe, V.; Roos, M.; Löbberding, M.; Scholten, N.; Müller, W.; Hellmich, M.; Simic, D.; Köpke, S.; Dichter, M.N. Expanded nursing roles to promote person-centred care for people with cognitive impairment in acute care (ENROLE-acute): Study protocol for a controlled clinical trial, process and economic evaluation. BMC Geriatr. 2023, 23, 858. [Google Scholar] [CrossRef]
- Youn, H.; Lee, M.; Jang, S.J. Person-centred care among intensive care unit nurses: A cross-sectional study. Intensive Crit. Care Nurs. 2022, 73, 103293. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.K. Person-centered care: An international dialogue. HERD 2021, 14, 30–37. [Google Scholar] [CrossRef]
- Morgan, S.; Yoder, L.H. A concept analysis of person-centered care. J. Holist. Nurs. 2012, 30, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Santana, M.J.; Manalili, K.; Jolley, R.J.; Zelinsky, S.; Quan, H.; Lu, M. How to practice person-centred care: A conceptual framework. Health Expect. 2018, 21, 429–440. [Google Scholar] [CrossRef]
- Lee, S.B.; Shin, S.J. Effects of clinical nurses critical reflection competency, professional pride, and person-centered care practice on patient safety management activities. J. Korean Crit. Care Nurs. 2023, 16, 87–98. [Google Scholar] [CrossRef]
- Shin, J.Y.; Jang, E.H. Influence of person-centered perioperative nursing and patient safety competency on patient safety management activities among operating room nurses: A descriptive survey study. Korean J. Adult Nurs. 2023, 35, 97–106. [Google Scholar] [CrossRef]
- Joo, Y.S.; Jang, Y.S. Predictors of person-centered care among nurses in adult intensive care units. J. Korean Clin. Nurs. Res. 2022, 28, 34–44. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Kim, Y.T. ICU Nurse’s Stressors and the Relationship Between the Degree of Social Support. Master’s Thesis, Hanyang University, Seoul, Republic of Korea, 1989. [Google Scholar]
- Cheraghi, F.; Hassani, P.; Yaghmaei, F.; Alavi-Majed, H. Developing a valid and reliable self-efficacy in clinical performance scale. Int. Nurs. Rev. 2009, 56, 214–221. [Google Scholar] [CrossRef]
- Jung, Y.J. Effects of Intensive Care Unit Syndrome Knowledge, Job Stress, and Self-Efficacy on Nursing Activities Among ICU Nurses. Master’s Thesis, Ewha Womans University, Seoul, Republic of Korea, 2019. [Google Scholar]
- Lee, J.J. Development of Person Centered Nursing Assessment Tool (PCNAT). Ph.D. Thesis, Daegu Catholic University, Daegu, Republic of Korea, 2018. [Google Scholar]
- Yoo, H.J.; Shim, J. Effects of a person-centred care intervention in an intensive care unit: Using mixed methods to examine nurses’ perspectives. J. Nurs. Manag. 2020, 28, 1295–1304. [Google Scholar] [CrossRef]
- Shin, S.; Moon, H. The effects of resilience, client-centered communication competency, and positive nursing organizational culture on person-centered nursing in general hospital nurses. Korean Int. Soc. 2023, 7, 509–536. [Google Scholar] [CrossRef]
- Jang, B.J.; Yeom, H.A. Relationships among delirium knowledge, self-efficacy, and nursing performance of hospice palliative care nurses. Korean J. Hosp. Palliat. Care 2018, 21, 65–74. [Google Scholar] [CrossRef]
- Kang, J.S.; Song, H.J. Factors affecting the performance of nurses in delirium care. J. Korean Crit. Care Nurs. 2019, 12, 13–21. [Google Scholar] [CrossRef]
- Huang, H.; Zhang, X.; Tu, L.; Peng, W.; Wang, D.; Chong, H.; Wang, Z.; Du, H.; Chen, H. Inclusive leadership, self-efficacy, organization-based self-esteem, and intensive care nurses’ job performance: A cross-sectional study using structural equation modeling. Intensive Crit. Care Nurs. 2025, 87, 103880. [Google Scholar] [CrossRef] [PubMed]
| Variables | Categories | n | % | Delirium Nursing Performance | |
|---|---|---|---|---|---|
| M ± SD | t/F (p) | ||||
| Sex | Female | 134 | 78.8 | 3.80 ± 0.42 | 0.05 (0.957) |
| Male | 36 | 21.2 | 3.80 ± 0.50 | ||
| Age (years) | <30 | 107 | 62.9 | 3.80 ± 0.44 | 0.01 (0.994) |
| 30∼40 | 51 | 30.0 | 3.80 ± 0.46 | ||
| ≥40 | 12 | 7.1 | 3.79 ± 0.42 | ||
| Marital status | Unmarried | 134 | 76.1 | 3.79 ± 0.44 | −0.72 (0.473) |
| Married | 42 | 23.9 | 3.86 ± 0.44 | ||
| Educational status | ≤Bachelors | 153 | 90.0 | 3.79 ± 0.43 | −0.78 (0.439) |
| ≥Masters | 17 | 10.0 | 3.87 ± 0.55 | ||
| Religion | No | 131 | 77.1 | 3.78 ± 0.42 | −0.84 (0.400) |
| Yes | 39 | 22.9 | 3.85 ± 0.50 | ||
| Total clinical experience (years) | <3 | 46 | 27.1 | 3.78 ± 0.48 | 0.59 (0.625) |
| 3∼5 | 37 | 21.8 | 3.85 ± 0.43 | ||
| 5∼10 | 57 | 33.5 | 3.82 ± 0.45 | ||
| ≥10 | 30 | 17.6 | 3.72 ± 0.39 | ||
| Experience in the trauma intensive care unit (years) | <3 | 68 | 40.0 | 3.76 ± 0.48 | 0.72 (0.488) |
| 3∼5 | 53 | 31.2 | 3.86 ± 0.40 | ||
| ≥5 | 49 | 28.8 | 3.79 ± 0.43 | ||
| Work shift type | 3 shifts | 162 | 95.3 | 3.81 ± 0.44 | 1.08 (0.281) |
| 2 shifts, full-time | 8 | 4.7 | 3.64 ± 0.37 | ||
| Presence of nursing guidelines for delirium care | Yes | 65 | 38.2 | 3.87 ± 0.42 | 1.59 (0.113) |
| None | 105 | 61.8 | 3.75 ± 0.45 | ||
| Use of a delirium assessment tool | Used | 94 | 55.3 | 3.84 ± 0.46 | 1.51 (0.133) |
| Not used | 76 | 44.7 | 3.74 ± 0.41 | ||
| Delirium-related education experience | Yes | 103 | 60.6 | 3.83 ± 0.43 | 1.29 (0.198) |
| No | 67 | 39.4 | 3.75 ± 0.45 | ||
| Variables | Number of Items | Mean | Scale Range | ||
|---|---|---|---|---|---|
| M ± SD | Min | Max | |||
| Delirium-related stress | 20 | 57.42 ± 13.73 | 12.55 | 93.00 | 0–100 |
| Self-efficacy | 37 | 3.82 ± 0.40 | 2.84 | 5.00 | 1–5 |
| Person-centred care | 25 | 3.85 ± 0.39 | 2.84 | 5.00 | 1–5 |
| Cooperative relationship | 7 | 3.82 ± 0.43 | 2.86 | 5.00 | 1–5 |
| Holism | 4 | 3.67 ± 0.53 | 2.25 | 5.00 | 1–5 |
| Respect | 5 | 4.03 ± 0.49 | 2.80 | 5.00 | 1–5 |
| Individualisation | 5 | 4.01 ± 0.43 | 2.80 | 5.00 | 1–5 |
| Empowerment | 4 | 3.68 ± 0.58 | 2.25 | 5.00 | 1–5 |
| Delirium nursing performance | 25 | 3.80 ± 0.44 | 2.80 | 4.88 | 1–5 |
| Variables | 1. DS | 2. SE | 3. PCC | 4. DNP | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | 3.1 | 3.2 | 3.3 | 3.4 | 3.5 | ||||
| r (p) | |||||||||
| 1. DS | 1 | ||||||||
| 2. SE | 0.12 (0.112) | 1 | |||||||
| 3. PCC | −0.05 (0.535) | 0.47 (<0.001) | 1 | ||||||
| 3.1. Cooperative relationship | −0.12 (0.108) | 0.37 (<0.001) | 0.84 (<0.001) | 1 | |||||
| 3.2. Holism | 0.03 (0.731) | 0.32 (<0.001) | 0.71 (<0.001) | 0.51 (<0.001) | 1 | ||||
| 3.3. Respect | −0.08 (0.318) | 0.37 (<0.001) | 0.85 (<0.001) | 0.65 (<0.001) | 0.49 (<0.001) | 1 | |||
| 3.4. Individualisation | 0.08 (0.302) | 0.48 (<0.001) | 0.84 (<0.001) | 0.63 (<0.001) | 0.47 (<0.001) | 0.71 (<0.001) | 1 | ||
| 3.5. Empowerment | 0.06 (0.461) | 0.33 (<0.001) | 0.77 (<0.001) | 0.50 (<0.001) | 0.44 (<0.001) | 0.57 (<0.001) | 0.60 (<0.001) | 1 | |
| 4. DNP | −0.01 (0.905) | 0.41 (<0.001) | 0.51 (<0.001) | 0.32 (<0.001) | 0.37 (<0.001) | 0.44 (<0.001) | 0.46 (<0.001) | 0.49 (<0.001) | 1 |
| B | SE | β | t (p) | |
|---|---|---|---|---|
| Constant | 1.11 | 0.33 | 3.41 (<0.001) | |
| Person-centred care | 0.46 | 0.08 | 0.41 | 5.53 (<0.001) |
| Self-Efficacy | 0.24 | 0.08 | 0.22 | 2.96 (0.004) |
| F (p) | 34.82 (<0.001) | |||
| R2 (Adjusted R2) | 0.294 (0.286) | |||
| Tolerance | 0.41–0.51 | |||
| Variance inflation factor | 1.28 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seong, G.-H.; Park, H.-R. Impact of Delirium-Related Stress, Self-Efficacy, Person-Centred Care on Delirium Nursing Performance Among Nurses in Trauma Intensive Care Units: A Cross-Sectional Descriptive Survey Study. Healthcare 2025, 13, 1243. https://doi.org/10.3390/healthcare13111243
Seong G-H, Park H-R. Impact of Delirium-Related Stress, Self-Efficacy, Person-Centred Care on Delirium Nursing Performance Among Nurses in Trauma Intensive Care Units: A Cross-Sectional Descriptive Survey Study. Healthcare. 2025; 13(11):1243. https://doi.org/10.3390/healthcare13111243
Chicago/Turabian StyleSeong, Ga-Hee, and Hyung-Ran Park. 2025. "Impact of Delirium-Related Stress, Self-Efficacy, Person-Centred Care on Delirium Nursing Performance Among Nurses in Trauma Intensive Care Units: A Cross-Sectional Descriptive Survey Study" Healthcare 13, no. 11: 1243. https://doi.org/10.3390/healthcare13111243
APA StyleSeong, G.-H., & Park, H.-R. (2025). Impact of Delirium-Related Stress, Self-Efficacy, Person-Centred Care on Delirium Nursing Performance Among Nurses in Trauma Intensive Care Units: A Cross-Sectional Descriptive Survey Study. Healthcare, 13(11), 1243. https://doi.org/10.3390/healthcare13111243






