The Effects of Patients’ Health Information Behaviors on Shared Decision-Making: Evaluating the Role of Patients’ Trust in Physicians
Abstract
1. Introduction
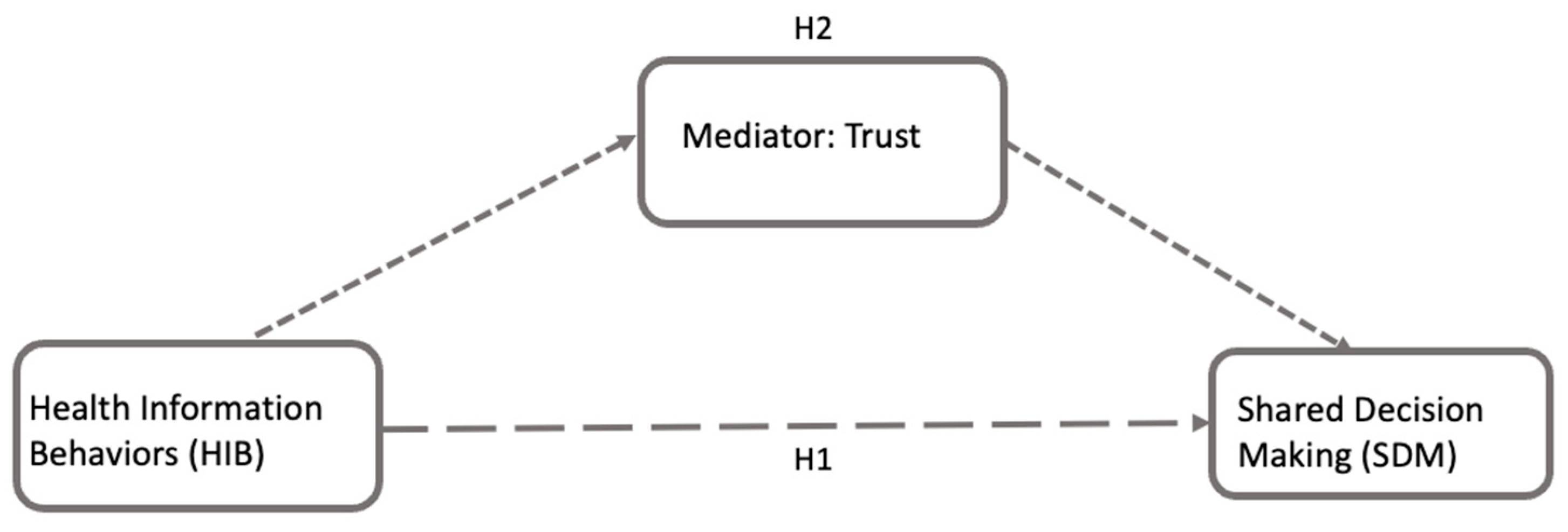
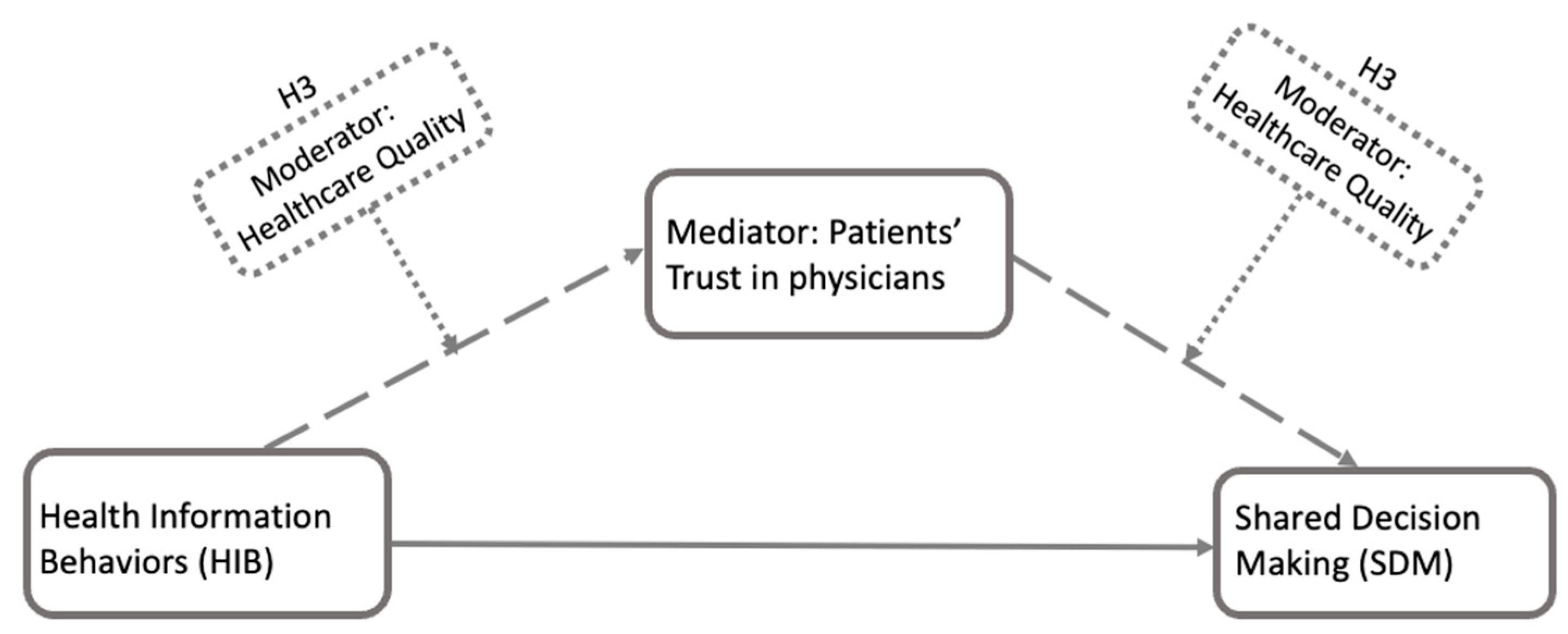
2. Theoretical Background and Hypothesis Development
2.1. Shared Decision-Making (SDM) and Health Information Behavior (HIB)
2.2. The Role of Patients’ Trust in Physicians
2.3. Robustness Checking
3. Materials and Methods
3.1. Data Descriptions
3.2. Measurements
3.2.1. Independent Variable (IV): Health Information Behavior (HIB)
3.2.2. Dependent Variable (DV): Shared Decision-Making (SDM)
3.2.3. Patients’ Trust in Physicians
- Concept 1: Trust in Information from Physicians (T1). Representing patients’ trust in the information provided by physicians, one survey question was selected from the survey: “In general, how much would you trust information about cancer from a doctor?” This was measured using a four-point Likert scale with options ranging from ‘A lot’ to ‘Not at all’. This question was intended to assess the level of confidence that patients have in their physician as a source of health information, focusing on the general trust patients have in their physicians.
- Concept 2: Trust in Information Sharing with Physicians (T2). Representing patients’ trust in sharing digital health-related data with their physicians, two questions were selected to represent this dimension of trust: (1) “Would you be willing to share health data from your wearable device with your health care provider?” and (2) “Have you shared health information from either an electronic monitoring device or smartphone with a health professional within the last 12 months?” These questions were measured using a binary scale, yes or no. The questions aimed to quantify the level to which patients are comfortable with and trust their physicians in handling and maintaining the confidentiality of their personal health information.
3.3. Data Analysis
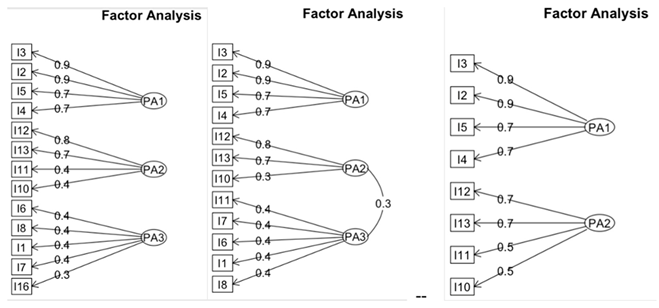
Exploratory Factor Analysis (EFA)
4. Results
4.1. Demographics
4.2. Factor Analysis
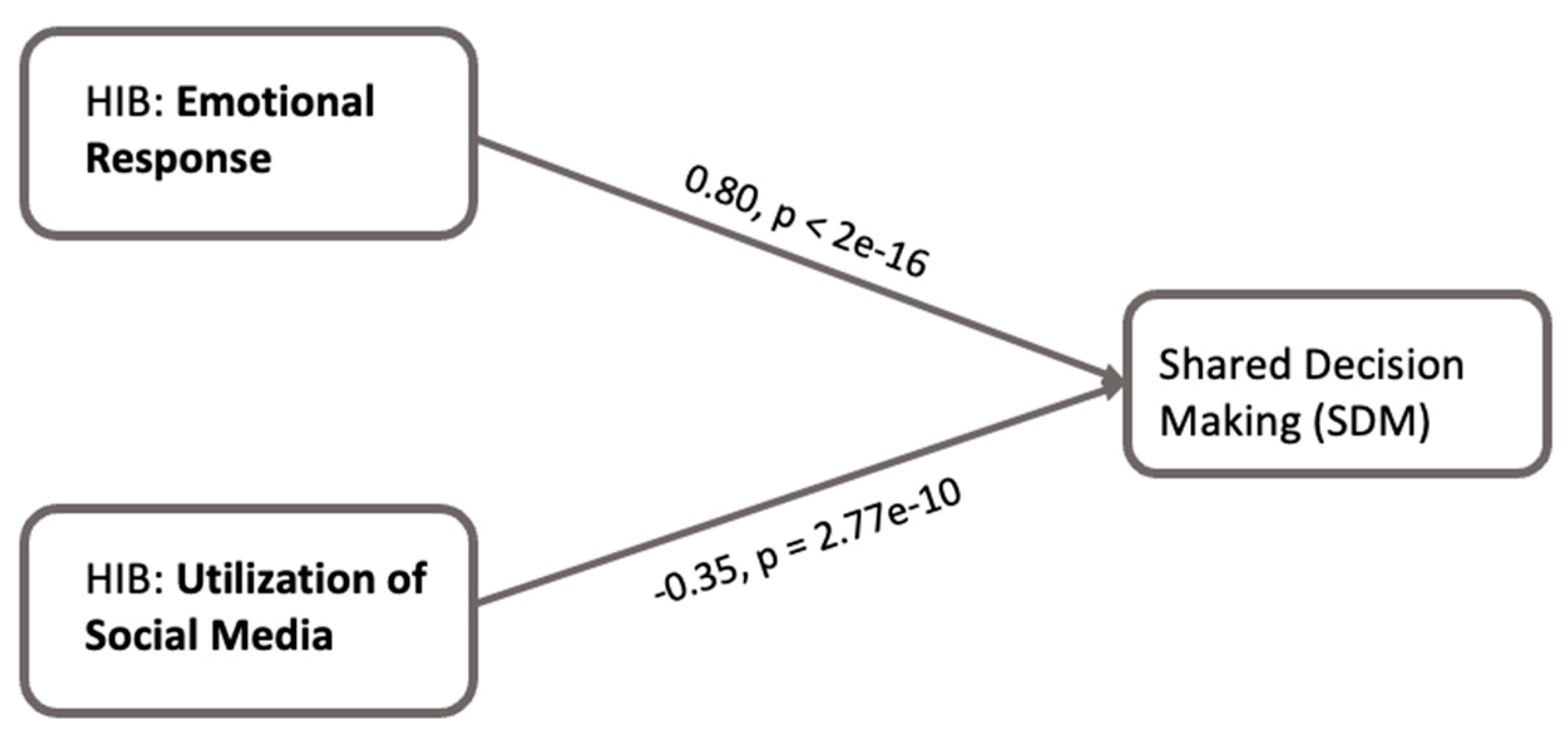
4.3. Linear Regression Analysis
4.4. Mediation Analysis
4.5. Patients’ Trust in Information Provided by Physicians (T1)
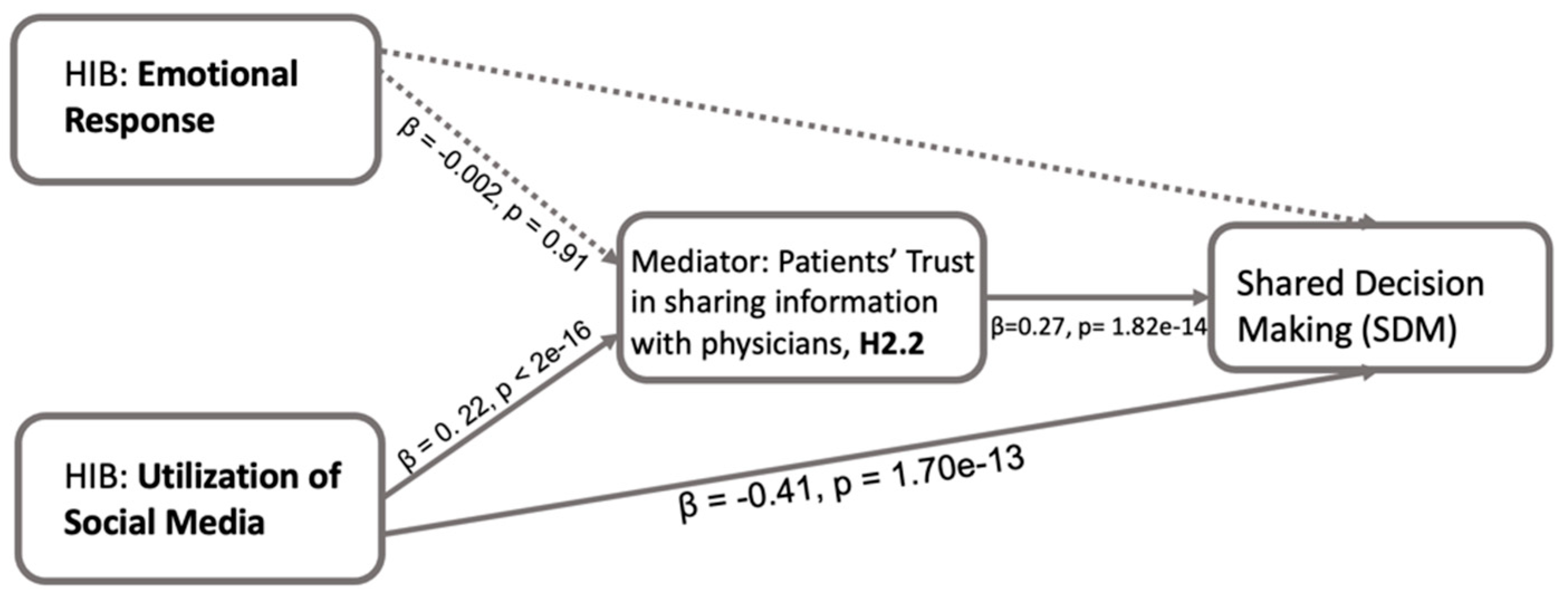
4.6. Patients’ Trust in Sharing Information with Physicians (T2)
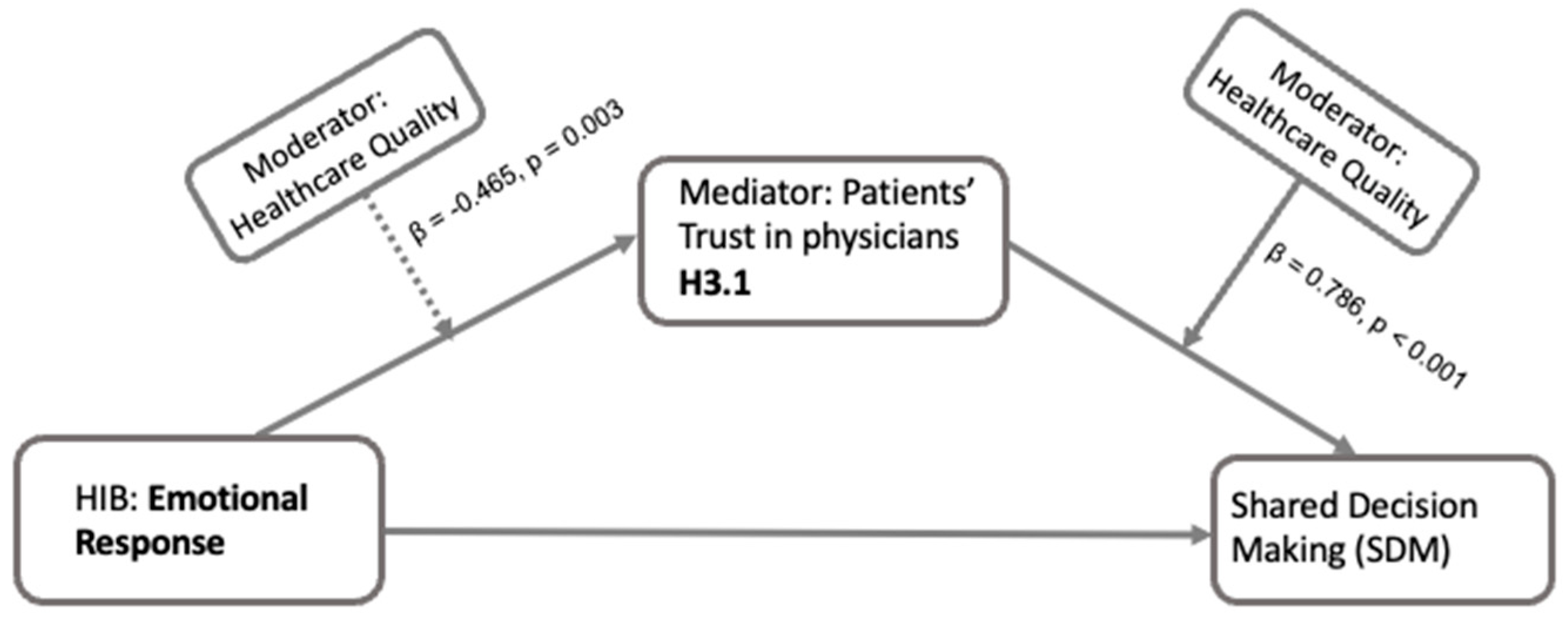
4.7. Moderated Mediation Analysis
5. Discussion
5.1. Mediating Effects of Trust
5.2. Trust and Patients’ Perceived Healthcare Quality
6. Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SDM | Shared decision-making |
| HIB | Health information behavior |
| HINTS | Health Information National Trends Survey |
| EFA | Exploratory factor analysis |
Appendix A. Description of Items Initially Representing HIB
| I1. Have you ever looked for information about cancer from any source? (Yes/No) | I2. Based on the results of your most recent search for information about cancer, how much do you agree or disagree: It took a lot of effort to get the information you needed (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) |
| I3. Based on the results of your most recent search for information about cancer, how much do you agree or disagree: You felt frustrated during your search for the information (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I4. Based on the results of your most recent search for information about cancer, how much do you agree or disagree: You were concerned about the quality of the information (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) |
| I5. Based on the results of your most recent search for information about cancer, how much do you agree or disagree: The information you found was hard to understand (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I6. In the past 12 months have you used the Internet to look for health or medical information? (Yes/No) |
| I7. How confident are you that you can find helpful health resources on the Internet? (Very confident; Somewhat confident; A little confident; Not confident at all) | I8. In the past 12 months, have you used a health or wellness app on your tablet or smartphone? (Yes/No) |
| I9. In the last 12 months, have you used an electronic wearable device to monitor or track health or activity? For example, a Fitbit, AppleWatch or Garmin Vivofit (Yes/No) | I10. In the last 12 months, how often did you interact with people who have similar health or medical issues on social media or online forums? (Almost every day; At least once a week; A few times a month; Less than once a month; Never) |
| I11. In the last 12 months, how often did you watch a health-related video on a social media site (for example, YouTube)? (Almost every day; At least once a week; A few times a month; Less than once a month; Never) | I12. How much do you agree or disagree—I use information from social media to make decisions about my health (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) |
| I13. How much do you agree or disagree—I use information from social media in discussions with my health care provider (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I14. In the past 12 months, did you receive care from a doctor or health professional using telehealth? (Yes/No) |
| I15. Have you ever used an app like Apple Health Records or CommonHealth to combine your medical information from different patient portals or online medical records into one place? (Yes/No) | I16. How many times did you access your online medical record or patient portal in the last 12 months? (0; 1 to 2 times; 3 to 5 times; 6 to 9 times; 10 or more times; do not have an online medical record or patient portal) |
| I17. In the past 12 months have you used your online medical record or patient portal to look up test results? (Yes/No) | I18. In the past 12 months have you used your online medical record or patient portal to view clinical notes (a health care providers written notes that describe your visit)? (Yes/No) |
Appendix B. Comparison of Regression Coefficients and Fit Metrics Across Imputation Methods
| Model | T1_1 Coef | T1_2 Coef | T2_1 Coef | T2_2 Coef | RSE | Adj R2 |
| Original Data | 0.080 | 0.739 | 0.057 | 0.013 | — | — |
| KNN Imputation | 0.058 | 0.717 | 0.186 | 0.003 | 0.05 | 2.39 |
| MICE Imputation | 0.076 | 0.681 | 0.078 | 0.013 | 0.06 | 2.33 |
| Random Forest | 0.069 | 0.732 | 0.042 | 0.007 | 0.06 | 2.22 |
| Note: To ensure robustness in handling missing data, we evaluated three imputation strategies: Multiple Imputation using Chained Equations (MICE), Random Forest Imputation (missForest), and k-Nearest Neighbors Imputation (KNN). The coefficients across all four models show consistent directions and significance patterns. The KNN-imputed model shows the lowest Residual Standard Error (RSE = 0.05) and the highest Adjusted R2 (2.39), suggesting that it explains more variance with lower residual noise than other methods. Importantly, the core relationships between trust indicators and SDM remain stable across models, indicating that the imputation did not alter the key findings of the analysis. This supports the robustness of the results and validates the use of KNN for handling missing data. | ||||||
Appendix C. Controlled Demographic Information
| Variable | n | Percentage | |
| Birth gender | Male | 2353 | 37.64% |
| Female | 3899 | 62.36% | |
| Age | 18–34 | 966 | 15.45% |
| 35–49 | 1279 | 20.46% | |
| 50–64 | 1799 | 28.77% | |
| 65–74 | 1361 | 21.77% | |
| 75+ | 847 | 13.55% | |
| Education | Less than high school | 448 | 7.17% |
| High school graduate | 1210 | 19.35% | |
| Some college | 1672 | 26.74% | |
| Bachelor | 1808 | 28.92% | |
| Post-baccalaureate | 1114 | 17.82% | |
| Race | Hispanic | 1194 | 19.10% |
| Non-Hispanic White | 3203 | 51.23% | |
| Non-Hispanic Black | 1032 | 16.51% | |
| Non-Hispanic Asian | 626 | 10.01% | |
| Non-Hispanic other | 197 | 3.15% | |
| Ever Had Cancer | Yes | 1084 | 17.34% |
| No | 5168 | 82.66% |
Appendix D. Detailed Results of Factor Analysis
- Step 1: Determine Number of Factors to Extract
- Step 2: Factor analysis with fa() function from package GPArotation
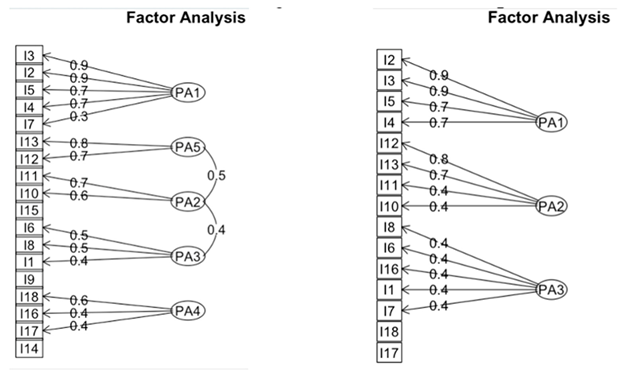
- Step 3: Refine the Factor Model with Iterative Process
References
- Elwyn, G.; Laitner, S.; Coulter, A.; Walker, E.; Watson, P.; Thomson, R. Implementing shared decision making in the NHS. BMJ 2010, 341, c5146. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, M.J.; Shulman, L.M.; Vandigo, J.; Mullins, C.D. Patient engagement and shared decision-making: What do they look like in neurology practice? Neurol. Clin. Pract. 2016, 6, 190–197. [Google Scholar] [CrossRef]
- Emanuel, E.J.; Emanuel, L.L. Four models of the physician-patient relationship. JAMA 1992, 267, 2221–2226. [Google Scholar] [CrossRef]
- Driever, E.M.; Tolhuizen, I.M.; Duvivier, R.J.; Stiggelbout, A.M.; Brand, P.L.P. Why do medical residents prefer paternalistic decision making? An interview study. BMC Med. Educ. 2022, 22, 155. [Google Scholar] [CrossRef]
- Niu, Z.; Bhurosy, T.; Heckman, C. Cancer Survivors’ Emotional Well-being: Roles of Internet Information Seeking, Patient-centered Communication, and Social Support. J. Health Commun. 2021, 26, 514–522. [Google Scholar] [CrossRef]
- Luo, A.; Yu, Z.; Liu, F.; Xie, W. The Chain Mediating Effect of the Public’s Online Health Information-Seeking Behavior on Doctor-Patient Interaction. Front. Public Health 2022, 10, 874495. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; McKee, M.; Torbica, A.; Stuckler, D. Systematic Literature Review on the Spread of Health-related Misinformation on Social Media. Soc. Sci. Med. 2019, 240, 112552. [Google Scholar] [CrossRef]
- Bin Naeem, S.; Kamel Boulos, M.N. COVID-19 Misinformation Online and Health Literacy: A Brief Overview. Int. J. Environ. Res. Public Health 2021, 18, 8091. [Google Scholar] [CrossRef] [PubMed]
- Chegini, Z.; Islam, S.M.S. Shared-decision-making Behavior in Hospitalized Patients: Investigating the Impact of Patient’s Trust in Physicians, Emotional Support, Informational Support, and Tendency to Excuse Using a Structural Equation Modeling Approach. J. Patient Exp. 2021, 8, 23743735211049661. [Google Scholar] [CrossRef]
- Wang, H.; Jia, J.; Fan, Y.; Chen, H.; Lou, Y.; Wang, X.; Huang, X. Impact of inpatient self-efficacy and trust in physicians on inpatient satisfaction with medical services: The mediating role of patient participation in medical decision-making. Front. Psychol. 2024, 15, 1364319. [Google Scholar] [CrossRef]
- Entwistle, V. Trust and shared decision-making: An emerging research agenda. Health Expect. 2004, 7, 271–273. [Google Scholar] [CrossRef] [PubMed]
- Hesse, B.W.; Nelson, D.E.; Kreps, G.L.; Croyle, R.T.; Arora, N.K.; Rimer, B.K.; Viswanath, K. Trust and Sources of Health Information: The Impact of the Internet and Its Implications for Health Care Providers: Findings From the First Health Information National Trends Survey. Arch. Intern. Med. 2005, 165, 2618–2624. [Google Scholar] [CrossRef] [PubMed]
- Lambert, S.D.; Loiselle, C.G. Health information seeking behavior. Qual. Health Res. 2007, 17, 1006–1019. [Google Scholar] [CrossRef]
- Zimmerman, M.S.; Shaw, G. Health information seeking behaviour: A concept analysis. Health Info. Libr. J. 2020, 37, 173–191. [Google Scholar] [CrossRef] [PubMed]
- Resnicow, K.; Catley, D.; Goggin, K.; Hawley, S.; Williams, G.C. Shared Decision Making in Health Care: Theoretical Perspectives for Why It Works and For Whom. Med. Decis. Mak. 2022, 42, 755–764. [Google Scholar] [CrossRef]
- Waddell, A.; Lennox, A.; Spassova, G.; Bragge, P. Barriers and facilitators to shared decision-making in hospitals from policy to practice: A systematic review. Implement. Sci. 2021, 16, 74. [Google Scholar] [CrossRef]
- Bujnowska-Fedak, M.M.; Waligóra, J.; Mastalerz-Migas, A. The Internet as a Source of Health Information and Services. Adv. Exp. Med. Biol. 2019, 1211, 1–16. [Google Scholar] [CrossRef]
- Bussey, L.G.; Sillence, E. The role of internet resources in health decision-making: A qualitative study. Digit. Health 2019, 5, 2055207619888073. [Google Scholar] [CrossRef]
- Krist, A.H.; Tong, S.T.; Aycock, R.A.; Longo, D.R. Engaging patients in decision-making and behavior change to promote prevention. Stud. Health Technol. Inf. 2017, 240, 284–302. [Google Scholar] [CrossRef]
- Sepucha, K.R.; Atlas, S.J.; Chang, Y.; Freiberg, A.; Malchau, H.; Mangla, M.; Rubash, H.; Simmons, L.H.; Cha, T. Informed, Patient-Centered Decisions Associated with Better Health Outcomes in Orthopedics: Prospective Cohort Study. Med. Decis. Mak. 2018, 38, 1018–1026. [Google Scholar] [CrossRef]
- Goold, S.D. Trust, Distrust and Trustworthiness. J. Gen. Intern. Med. 2002, 17, 79–81. [Google Scholar] [CrossRef]
- Hall, M.A.; Camacho, F.; Dugan, E.; Balkrishnan, R. Trust in the Medical Profession: Conceptual and Measurement Issues. Health Serv. Res. 2002, 37, 1419–1439. [Google Scholar] [CrossRef] [PubMed]
- Mayer, R.C.; Davis, J.H.; Schoorman, F.D. An Integrative Model of Organizational Trust. Acad. Manag. Rev. 1995, 20, 709–734. [Google Scholar] [CrossRef]
- Kao, A.C.; Green, D.C.; Davis, N.A.; Koplan, J.P.; Cleary, P.D. Patients’ Trust in Their Physicians. J. Gen. Intern. Med. 1998, 13, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Iott, B.E.; Campos-Castillo, C.; Anthony, D.L. Trust and Privacy: How Patient Trust in Providers is Related to Privacy Behaviors and Attitudes. AMIA Annu. Symp. Proc. 2020, 2019, 487–493. [Google Scholar] [PubMed]
- Asan, O.; Yu, Z.; Crotty, B.H. How clinician-patient communication affects trust in health information sources: Temporal trends from a national cross-sectional survey. PLoS ONE 2021, 16, e0247583. [Google Scholar] [CrossRef]
- Kraetschmer, N.; Sharpe, N.; Urowitz, S.; Deber, R.B. How does trust affect patient preferences for participation in decision-making? Health Expect. 2004, 7, 317–326. [Google Scholar] [CrossRef]
- Peek, M.E.; Gorawara-Bhat, R.; Quinn, M.T.; Odoms-Young, A.; Wilson, S.C.; Chin, M.H. Patient trust in physicians and shared decision-making among African-Americans with diabetes. Health Commun. 2013, 28, 616–623. [Google Scholar] [CrossRef]
- Graham, J.L.; Shahani, L.; Grimes, R.M.; Hartman, C.; Giordano, T.P. The Influence of Trust in Physicians and Trust in the Healthcare System on Linkage, Retention, and Adherence to HIV Care. AIDS Patient Care STDS 2015, 29, 661–667. [Google Scholar] [CrossRef]
- Khullar, D.; Prasad, K.; Neprash, H.; Poplau, S.; Brown, R.L.; Williams, E.S.; Audi, C.; Linzer, M. Factors associated with patient trust in their clinicians: Results from the Healthy Work Place Study. Health Care Manag. Rev. 2022, 47, 289. [Google Scholar] [CrossRef]
- Chawłowska, E.; Staszewski, R.; Jóźwiak, P.; Lipiak, A.; Zawiejska, A. Development and Validation of a Health Behaviour Scale: Exploratory Factor Analysis on Data from a Multicentre Study in Female Primary Care Patients. Behav. Sci. 2022, 12, 378. [Google Scholar] [CrossRef] [PubMed]
- van Buuren, S.; Groothuis-Oudshoorn, K. mice: Multivariate Imputation by Chained Equations in R. J. Stat. Softw. 2011, 45, 1–67. [Google Scholar] [CrossRef]
- Birkhäuer, J.; Gaab, J.; Kossowsky, J.; Hasler, S.; Krummenacher, P.; Werner, C.; Gerger, H. Trust in the health care professional and health outcome: A meta-analysis. PLoS ONE 2017, 12, e0170988. [Google Scholar] [CrossRef]
- Ichikawa, T.; Kishida, D.; Shimojima, Y.; Yajima, N.; Oguro, N.; Yoshimi, R.; Sakurai, N.; Hidekawa, C.; Sada, K.; Miyawaki, Y.; et al. Impact of online health information-seeking behavior on shared decision-making in patients with systemic lupus erythematosus: The TRUMP2-SLE project. Lupus 2023, 32, 1258–1266. [Google Scholar] [CrossRef]
- Rodríguez-Fuertes, A.; Reinares-Lara, P.; Garcia-Henche, B. Incorporation of the emotional indicators of the patient journey into healthcare organization management. Health Expect. 2023, 26, 297–306. [Google Scholar] [CrossRef] [PubMed]
- Lu, Q.; Schulz, P.J. How Physicians Tackle Internet-Misinformed Patients: Going Beyond Traditional Patient-Centered Communication—A Study Protocol. Adv. Med. Educ. Pract. 2023, 14, 983–988. [Google Scholar] [CrossRef]
- Song, M.; Elson, J.; Nguyen, T.; Obasi, S.; Pintar, J.; Bastola, D. Exploring trust dynamics in health information systems: The impact of patients’ health conditions on information source preferences. Front. Public Health 2024, 12, 1478502. [Google Scholar] [CrossRef]
- Papadimitriou, C.; Clayman, M.L.; Mallinson, T.; Weaver, J.A.; Guernon, A.; Meehan, A.J.; Kot, T.; Ford, P.; Ideishi, R.; Prather, C.; et al. A New Process Model for Relationship-Centred Shared Decision-Making in Physical Medicine and Rehabilitation Settings. Health Expect. 2024, 27, e14162. [Google Scholar] [CrossRef] [PubMed]
- Abidova, A.; da Silva, P.A.; Moreira, S. The mediating role of patient satisfaction and perceived quality of healthcare in the emergency department. Medicine 2021, 100, e25133. [Google Scholar] [CrossRef]
- Walker, D.M.; Johnson, T.; Ford, E.W.; Huerta, T.R. Trust Me, I’m a Doctor: Examining Changes in How Privacy Concerns Affect Patient Withholding Behavior. J. Med. Internet Res. 2017, 19, e2. [Google Scholar] [CrossRef]
- Yang, X.; Parton, J.; Lewis, D.; Yang, N.; Hudnall, M. Effect of Patient-Physician Relationship on Withholding Information Behavior: Analysis of Health Information National Trends Survey (2011–2018) Data. J. Med. Internet Res. 2020, 22, e16713. [Google Scholar] [CrossRef]
- Musbahi, A.; Brown, L.R.; Reddy, A.; Viswanath, Y.K.S.; Rao, M.; Gopinath, B.R. Systematic review of online patient resources to support shared decision making for bariatric surgery. Int. J. Surg. 2020, 74, 34–38. [Google Scholar] [CrossRef] [PubMed]
- Muhammed T, S.; Mathew, S.K. The disaster of misinformation: A review of research in social media. Int. J. Data Sci. Anal. 2022, 13, 271–285. [Google Scholar] [CrossRef]
- Ismail, N.; Kbaier, D.; Farrell, T.; Kane, A. The Experience of Health Professionals with Misinformation and Its Impact on Their Job Practice: Qualitative Interview Study. JMIR Form. Res. 2022, 6, e38794. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.S.-L.; Goonawardene, N. Internet Health Information Seeking and the Patient-Physician Relationship: A Systematic Review. J. Med. Internet Res. 2017, 19, e9. [Google Scholar] [CrossRef] [PubMed]
- Smailhodzic, E.; Hooijsma, W.; Boonstra, A.; Langley, D.J. Social media use in healthcare: A systematic review of effects on patients and on their relationship with healthcare professionals. BMC Health Serv. Res. 2016, 16, 442. [Google Scholar] [CrossRef]
- Lewandowski, R.; Goncharuk, A.G.; Cirella, G.T. Restoring patient trust in healthcare: Medical information impact case study in Poland. BMC Health Serv. Res. 2021, 21, 865. [Google Scholar] [CrossRef]
- Jain, R.; Jain, Y. The importance of physical examination in primary health care provided by NPHW is being threatened in COVID-19 times. J. Fam. Med. Prim. Care 2021, 10, 19–21. [Google Scholar] [CrossRef]



| Emotional Response During Health Information Behavior | Utilization of Social Media During Health Information Behavior |
|---|---|
| I2. Based on the results of your most recent search for information about cancer, how much do you agree or disagree: It took a lot of effort to get the information you needed (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I10. In the last 12 months, how often did you interact with people who have similar health or medical issues on social media or online forums? (Almost every day; At least once a week; A few times a month; Less than once a month; Never) |
| (I3–5). Based on the results of your most recent search for information about cancer, how much do you agree or disagree: I3. You felt frustrated during your search for the information (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I11. In the last 12 months, how often did you watch a health-related video on a social media site (for example, YouTube)? (Almost every day; At least once a week; A few times a month; Less than once a month; Never) |
| I4. You were concerned about the quality of the information (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I12. How much do you agree or disagree—I use information from social media to make decisions about my health (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) |
| I5. The information you found was hard to understand (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) | I13. How much do you agree or disagree—I use information from social media in discussions with my health care provider (Strongly agree; Somewhat agree; Somewhat disagree; Strongly disagree) |
| Mediator | HIB Dimension | Effect on SDM | Coefficient (β) | p-Value | Mediation Effect | Moderated Mediation |
|---|---|---|---|---|---|---|
| Trust in Physicians (H2.1) | Emotional Response | Direct Effect | 0.683 | <2 × 10−16 | Partial Mediation (Proportion Mediated: 14.9%) | Significant (β = −0.079, p = 0.004) |
| Indirect Effect | 0.120 | <2 × 10−16 | ||||
| Total Effect | 0.803 | <2 × 10−16 | ||||
| Utilization of Social Media | Direct Effect | −0.315 | <2 × 10−16 | Partial Mediation (Proportion Mediated: 9.53%) | Not significant (β = 0.061, p = 0.103) | |
| Indirect Effect | −0.033 | 0.0084 | ||||
| Total Effect | −0.348 | <2 × 10−16 | ||||
| Trust in Information Sharing (H2.2) | Emotional Response | Direct Effect | - | - | - | - |
| Indirect Effect | - | - | - | - | ||
| Total Effect | - | - | - | - | ||
| Utilization of Social Media | Direct Effect | −0.409 | <2 × 10−16 | Partial Mediation (Proportion Mediated: −17.52%) | Significant (β = 0.087, p = 0.013) | |
| Indirect Effect | 0.061 | <2 × 10−16 | ||||
| Total Effect | −0.348 | <2 × 10−16 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, M.; Elson, J.; Haas, C.; Obasi, S.N.; Sun, X.; Bastola, D. The Effects of Patients’ Health Information Behaviors on Shared Decision-Making: Evaluating the Role of Patients’ Trust in Physicians. Healthcare 2025, 13, 1238. https://doi.org/10.3390/healthcare13111238
Song M, Elson J, Haas C, Obasi SN, Sun X, Bastola D. The Effects of Patients’ Health Information Behaviors on Shared Decision-Making: Evaluating the Role of Patients’ Trust in Physicians. Healthcare. 2025; 13(11):1238. https://doi.org/10.3390/healthcare13111238
Chicago/Turabian StyleSong, Mingming, Joel Elson, Christian Haas, Sharon N. Obasi, Xinyu Sun, and Dhundy Bastola. 2025. "The Effects of Patients’ Health Information Behaviors on Shared Decision-Making: Evaluating the Role of Patients’ Trust in Physicians" Healthcare 13, no. 11: 1238. https://doi.org/10.3390/healthcare13111238
APA StyleSong, M., Elson, J., Haas, C., Obasi, S. N., Sun, X., & Bastola, D. (2025). The Effects of Patients’ Health Information Behaviors on Shared Decision-Making: Evaluating the Role of Patients’ Trust in Physicians. Healthcare, 13(11), 1238. https://doi.org/10.3390/healthcare13111238






