Economic Evaluations of Rehabilitation Interventions: A Scoping Review with Implications for Return to Work Programs
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Sources
2.3. Data Extraction
3. Results
3.1. Study Characteristics and Intervention Type
3.2. Economic Outcomes
3.3. Return to Work Implication
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| RTW | Return To Work |
| CEA | Cost-Effectiveness Analysis |
| CUA | Cost Utility Analysis |
| BIA | Budget Impact Analysis |
| LMICs | Low- and Middle-Income Countries |
| ICERs | Incremental Cost-Effectiveness Ratios |
| QALY | Quality-Adjusted Life Years |
| CHEERS | Consolidated Health Economic Evaluation Reporting Standards |
| PRISMA-ScR | Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews |
| O-ACT | Outpatient Acceptance and Commitment Therapy |
Appendix A
| Section | Item | Prisma-ScR Checklist Item | Reported on Page |
|---|---|---|---|
| Title | |||
| Title | 1 | Identify the report as a scoping review. | Title page |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary that includes (as applicable) background, objectives, eligibility criteria, sources of evidence, charting methods, results, and conclusions that relate to the review questions and objectives. | Abstract |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. Explain why the review questions/objectives lend themselves to a scoping review approach. | 1–2 |
| Objectives | 4 | Provide an explicit statement of the questions and objectives being addressed with reference to their key elements (e.g., population or participants, concepts, and context) or other relevant key elements used to conceptualize the review questions and/or objectives. | 2 |
| Methods | |||
| Protocol and registration | 5 | Indicate whether a review protocol exists; state if and where it can be accessed (e.g., a web address); and, if available, provide registration information, including the registration number. | Not applicable |
| Eligibility criteria | 6 | Specify characteristics of the sources of evidence used as eligibility criteria (e.g., years considered, language, and publication status) and provide a rationale. | 3 |
| Information sources | 7 | Describe all information sources in the search (e.g., databases with dates of coverage and contact with authors to identify additional sources), as well as the date the most recent search was executed. | 3 |
| Search | 8 | Present the full electronic search strategy for at least 1 database, including any limits used, such that it could be repeated. | 3 |
| Selection of sources of evidence | 9 | State the process for selecting sources of evidence (i.e., screening and eligibility) included in the scoping review. | 3 |
| Data charting process | 10 | Describe the methods of charting data from the included sources of evidence (e.g., calibrated forms or forms that have been tested by the team before their use and whether data charting was conducted independently or in duplicate) and any processes for obtaining and confirming data from investigators. | 3 |
| Data items | 11 | List and define all variables for which data were sought and any assumptions and simplifications made. | 3 |
| Critical appraisal of individual sources of evidence | 12 | If performed, provide a rationale for conducting a critical appraisal of included sources of evidence; describe the methods used and how this information was used in any data synthesis (if appropriate). | Not applicable |
| Synthesis of results | 13 | Describe the methods of handling and summarizing the data that were charted. | 3 |
| Results | |||
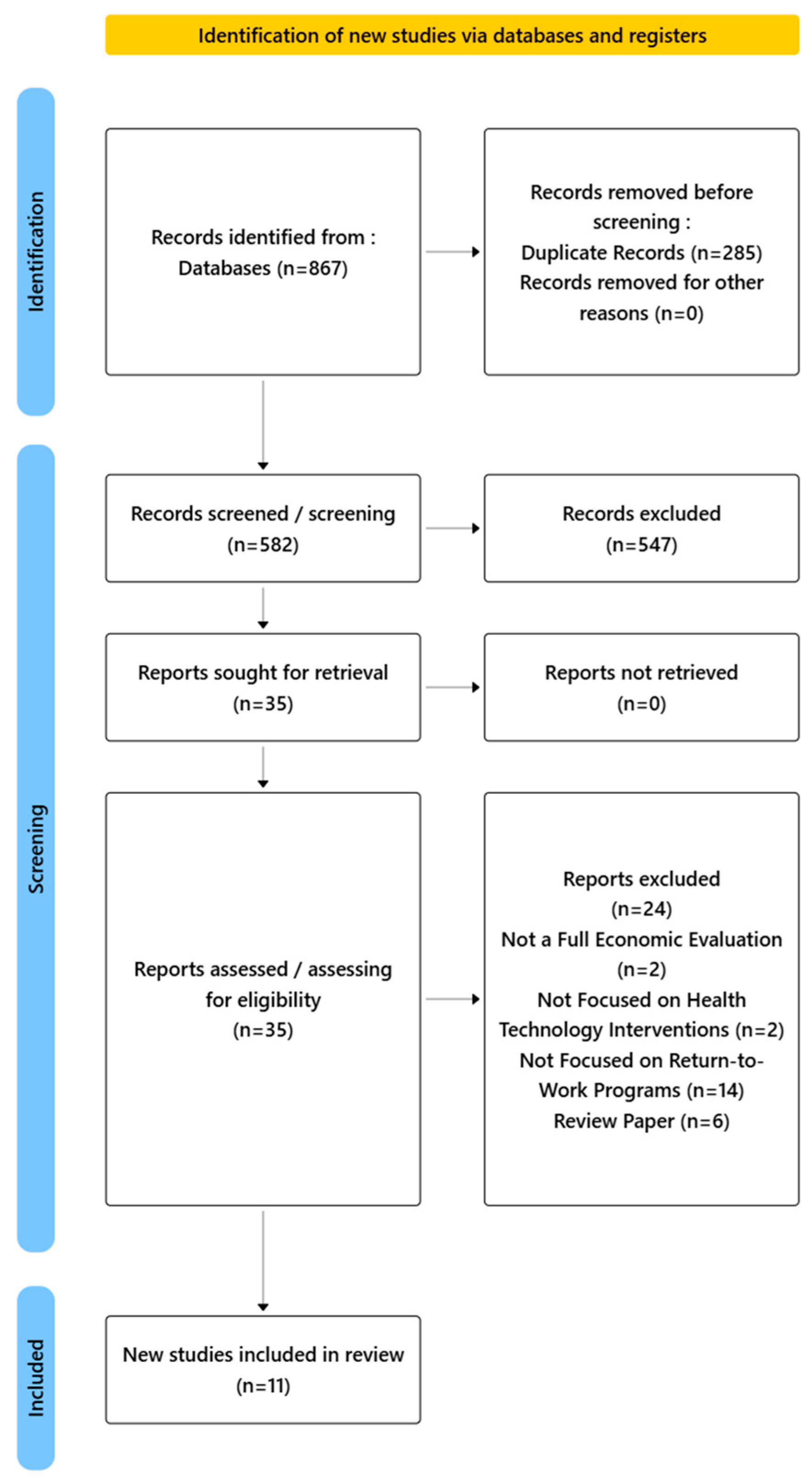
| Selection of sources of evidence | 14 | Give number of sources of evidence screened, assessed for eligibility, included in the review, with reasons for exclusion at each stage, ideally using a flow diagram. | 4, Figure 1 |
| Characteristics of sources of evidence | 15 | For each source of evidence, present characteristics for which data were charted and provide the citations. | 5, Table 1 |
| Critical appraisal of the sources of evidence | 16 | If performed, present the data of the critical appraisal of the included sources of evidence (see item 12). | Not applicable |
| Results of individual sources of evidence | 17 | For each included source of evidence, present the relevant data that were charted that relate to the review questions and objectives. | 4–10 |
| Synthesis of results | 18 | Summarize and/or present the charting results as they relate to the review questions and objectives. | 4–10 |
| Discussion | |||
| Summary of evidence | 19 | Summarize the main results (including an overview of concepts, themes, and types of evidence available), link to the review questions and objectives, and consider the relevance to key groups. | 10–13 |
| Limitations | 20 | Discuss the limitations of the scoping review process. | 12 |
| Conclusions | 21 | Provide a general interpretation of the results with respect to the review questions and objectives, as well as potential implications and/or next steps. | 13 |
| Funding | |||
| Funding | 22 | Describe sources of funding for the included sources of evidence, as well as sources of funding for the scoping review. Describe the role of the funders of the scoping review. | 13 |
References
- Treger, I.; Kosto, A.; Vadas, D.; Friedman, A.; Lutsky, L.; Kalichman, L. Crafting the Future of Community-Based Medical Rehabilitation: Exploring Optimal Models for Non-Inpatient Rehabilitation Services through a Narrative Review. Int. J. Environ. Res. Public Health 2024, 21, 1332. [Google Scholar] [CrossRef]
- Wales, K.; Lang, D.; Rahja, M.; Somerville, L.; Laver, K.; Lannin, N.A. Economic Effects of Occupational Therapy Services for Adults in Acute and Subacute Care Settings: A Systematic Review. Am. J. Occup. Ther. 2022, 76, 7601180080. [Google Scholar] [CrossRef]
- Maccarone, M.C.; Masiero, S.; Papathanasiou, J.; Panayotov, K.; Kashilskah, Y.; Prokopidis, K.; Papanastasiou, C.; Tyllianakis, M.; Dionyssiotis, Y. Frailty Education: Promoting Geriatric Competencies among Physical Medicine and Rehabilitation Residents. Am. J. Phys. Med. Rehabil. 2023, 102, E137–E140. [Google Scholar] [CrossRef]
- Toledo, C.; Vera, A.; Leija, L.; Gutierrez, J. The Importance of Rehabilitation for COVID-19 Sequelae. In Proceedings of the 2021 Global Medical Engineering Physics Exchanges/Pan American Health Care Exchanges (GMEPE/PAHCE), Sevilla, Spain, 15–20 March 2021; IEEE: Piscataway, NJ, USA, 2021; pp. 1–5. [Google Scholar]
- Walsh, T.S.; Salisbury, L.G.; Merriweather, J.L.; Boyd, J.A.; Griffith, D.M.; Huby, G.; Kean, S.; Mackenzie, S.J.; Krishan, A.; Lewis, S.C.; et al. Increased Hospital-Based Physical Rehabilitation and Information Provision After Intensive Care Unit Discharge. JAMA Intern. Med. 2015, 175, 901. [Google Scholar] [CrossRef] [PubMed]
- Dibben, P.; Wood, G.; O’Hara, R. Do Return to Work Interventions for Workers with Disabilities and Health Conditions Achieve Employment Outcomes and Are They Cost Effective? A Systematic Narrative Review. Empl. Relat. 2018, 40, 999–1014. [Google Scholar] [CrossRef]
- Flemming, J.; Chojecki, D.; Tjosvold, L.; Paulden, M.; Armijo-Olivo, S. Quality of Reporting of Economic Evaluations in Rehabilitation Research: A Systematic Review. Disabil. Rehabil. 2022, 44, 2233–2240. [Google Scholar] [CrossRef] [PubMed]
- Mancuso, M.; Valentini, I.; Basile, M.; Bowen, A.; Fordell, H.; Laurita, R.; Möller, M.C.; Williams, L.J.; Zoccolotti, P. Cost-effectiveness of Neuropsychological Rehabilitation for Acquired Brain Injuries: Update of Stolwyk et al.’s (2019) Review. J. Neuropsychol. 2024, 19, 115–139. [Google Scholar] [CrossRef]
- Lathiere, T.; Jaubert, A.; Lewis, J.; David-Tchouda, S.; Beard, D.; Pinsault, N. The Health Economic Analysis of Surgery versus Rehabilitation in Non-Traumatic Musculoskeletal Shoulder Disorders: A Systematic Review of Trial-Based Studies. Clin. Rehabil. 2024, 39, 139–152. [Google Scholar] [CrossRef]
- Nagra, G.; Ezeugwu, V.E.; Bostick, G.P.; Branton, E.; Dennett, L.; Drake, K.; Durand-Moreau, Q.; Guptill, C.; Hall, M.; Ho, C.; et al. Return-to-Work for People Living with Long COVID: A Scoping Review of Interventions and Recommendations. medRxiv 2024. [Google Scholar] [CrossRef]
- Aagesen, M.; la Cour, K.; Møller, J.-J.K.; Stapelfeldt, C.M.; Hauken, M.A.; Pilegaard, M.S. Rehabilitation Interventions for Young Adult Cancer Survivors: A Scoping Review. Clin. Rehabil. 2023, 37, 1347–1374. [Google Scholar] [CrossRef]
- Latha, R.S. A Scoping Review of Formal Care to Children with Special Needs during the COVID-19 Pandemic. Int. J. Spec. Educ. (IJSE) 2022, 37, 1–14. [Google Scholar] [CrossRef]
- Drummond, M.; Carswell, C.; Husereau, D. Update of the Consolidated Health Economic Evaluation Reporting Standards: CHEERS 2022. Med. Writ. 2022, 31, 60–64. [Google Scholar]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Rasmussen, B.; Maribo, T.; Skovsby Toft, B. The Content and Characteristics of Face-to-Face Interventions to Encourage Patients’ Enrollment in Cardiac Rehabilitation; a Scoping Review. Disabil. Rehabil. 2024, 46, 2734–2746. [Google Scholar] [CrossRef] [PubMed]
- Tingulstad, A.; Maas, E.T.; Rysstad, T.; Øiestad, B.E.; Aanesen, F.; Pripp, A.H.; Van Tulder, M.W.; Grotle, M. Six-Month Cost-Effectiveness of Adding Motivational Interviewing or a Stratified Vocational Advice Intervention to Usual Case Management for Workers with Musculoskeletal Disorders: The MI-NAV Economic Evaluation. J. Occup. Med. Toxicol. 2023, 18, 25. [Google Scholar] [CrossRef] [PubMed]
- Corbacho, B.; Brealey, S.; Keding, A.; Richardson, G.; Torgerson, D.; McDaid, C.; Rangan, A. Cost-Effectiveness of Surgical Treatments Compared with Early Structured Physiotherapy in Secondary Care for Adults with Primary Frozen Shoulder. Bone Jt. Open 2021, 2, 685–695. [Google Scholar] [CrossRef]
- Xin, Y.; Ashburn, A.; Pickering, R.M.; Seymour, K.C.; Hulbert, S.; Fitton, C.; Kunkel, D.; Marian, I.; Roberts, H.C.; Lamb, S.E.; et al. Cost-Effectiveness of the PDSAFE Personalised Physiotherapy Intervention for Fall Prevention in Parkinson’s: An Economic Evaluation alongside a Randomised Controlled Trial. BMC Neurol. 2020, 20, 295. [Google Scholar] [CrossRef]
- Lewkowicz, D.; Wohlbrandt, A.M.; Bottinger, E. Digital Therapeutic Care Apps with Decision-Support Interventions for People With Low Back Pain in Germany: Cost-Effectiveness Analysis. JMIR Mhealth Uhealth 2022, 10, e35042. [Google Scholar] [CrossRef]
- Arora, M.; Harvey, L.A.; Glinsky, J.V.; Chhabra, H.S.; Hossain, M.S.; Arumugam, N.; Bedi, P.K.; Cameron, I.D.; Hayes, A.J. Cost-Effectiveness Analysis of Telephone-Based Support for the Management of Pressure Ulcers in People with Spinal Cord Injury in India and Bangladesh. Spinal Cord 2017, 55, 1071–1078. [Google Scholar] [CrossRef]
- Morgante, N.; Bjørnelv, G.M.W.; Aasdahl, L.; Nguyen, C.; Kunst, N.; Fimland, M.S.; Burger, E.A. Evaluating the Health and Economic Impacts of Return-to-Work Interventions: A Modeling Study. Value Health 2024, 28, 415–423. [Google Scholar] [CrossRef]
- Brusco, N.; Voogt, A.; Nott, M.; Callaway, L.; Mansoubi, M.; Layton, N. Meeting Unmet Needs for Stroke Rehabilitation in Rural Public Health: Explorative Economic Evaluation of Upper Limb Robotics-Based Technologies through a Capabilities Lens. Societies 2022, 12, 143. [Google Scholar] [CrossRef]
- Sutton, B.S.; Ottomanelli, L.; Njoh, E.; Barnett, S.; Goetz, L. Economic Evaluation of a Supported Employment Program for Veterans with Spinal Cord Injury. Disabil. Rehabil. 2020, 42, 1423–1429. [Google Scholar] [CrossRef] [PubMed]
- Pinto, D.; Garnier, M.; Barbas, J.; Chang, S.H.; Charlifue, S.; Field-Fote, E.; Furbish, C.; Tefertiller, C.; Mummidisetty, C.K.; Taylor, H.; et al. Budget Impact Analysis of Robotic Exoskeleton Use for Locomotor Training Following Spinal Cord Injury in Four SCI Model Systems. J. Neuroeng. Rehabil. 2020, 17, 4. [Google Scholar] [CrossRef] [PubMed]
- Donnelley, C.A.; Von Kaeppler, E.P.; Hetherington, A.; Shirley, C.; Haonga, B.T.; Challa, S.T.; Andrysek, J.; Lutyens, E.M.; Mamseri, L.; Mwakasungula, G.; et al. Cost-Effectiveness Analysis of Prosthesis Provision for Patients with Transfemoral Amputation in Tanzania. Prosthet. Orthot. Int. 2022, 46, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Wagner, T.H.; Lo, A.C.; Peduzzi, P.; Bravata, D.M.; Huang, G.D.; Krebs, H.I.; Ringer, R.J.; Federman, D.G.; Richards, L.G.; Haselkorn, J.K.; et al. An Economic Analysis of Robot-Assisted Therapy for Long-Term Upper-Limb Impairment after Stroke. Stroke 2011, 42, 2630–2632. [Google Scholar] [CrossRef]
- Husereau, D.; Drummond, M.; Petrou, S.; Carswell, C.; Moher, D.; Greenberg, D.; Augustovski, F.; Briggs, A.H.; Mauskopf, J.; Loder, E. Consolidated Health Economic Evaluation Reporting Standards (Cheers) Statement. Int. J. Technol. Assess. Health Care 2013, 29, 117–122. [Google Scholar] [CrossRef]
- Husereau, D.; Drummond, M.; Augustovski, F.; de Bekker-Grob, E.; Briggs, A.H.; Carswell, C.; Caulley, L.; Chaiyakunapruk, N.; Greenberg, D.; Loder, E.; et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Statement: Updated Reporting Guidance for Health Economic Evaluations. Eur. J. Health Econ. 2022, 23, 1309–1317. [Google Scholar] [CrossRef]
- Alheresh, R.; Cahn, P.S. Expanding Global Rehabilitation Services through International Academic-Community Partnerships. Ann. Glob. Health 2020, 86, 71. [Google Scholar] [CrossRef]
- Kayola, G.; Mataa, M.M.; Asukile, M.; Chishimba, L.; Chomba, M.; Mortel, D.; Nutakki, A.; Zimba, S.; Saylor, D. Stroke Rehabilitation in Low- and Middle-Income Countries: Challenges and Opportunities. Am. J. Phys. Med. Rehabil. 2023, 102, S24–S32. [Google Scholar] [CrossRef]
- Zainal, M.N.B.; Wen, P.K.P.; Sien, N.Y.; Kee, K.M.; Chieh, K.J.; Asano, M. Supporting People with Stroke to Return to Work in Singapore: Findings from a Pilot Vocational Rehabilitation Program. Am. J. Occup. Ther. 2020, 74, 7406205040p1–7406205040p9. [Google Scholar] [CrossRef]
- Bonnet, C. Rehabilitating Psychosocial Readaptation Care|Réhabiliter Les Soins de Réadaptation Psychosociale|Rehabilitar Los Cuidados de Readaptación Psicosocial. Inf. Psychiatr. 2024, 100, 29–36. [Google Scholar]
- Miri, F.; Jahanmehr, N.; Goudarzi, R. Cost-Effectiveness Analysis of Rehabilitation Methods for Stroke Survivors. Middle East J. Rehabil. Health Stud. 2024, 11, e141716. [Google Scholar] [CrossRef]
- Magnusson, D.; Sweeney, F.; Landry, M. Provision of Rehabilitation Services for Children with Disabilities Living in Low- and Middle-Income Countries: A Scoping Review. Disabil. Rehabil. 2019, 41, 861–868. [Google Scholar] [CrossRef]
- Cashin, A.G.; Øiestad, B.E.; Aanesen, F.; Storheim, K.; Tingulstad, A.; Rysstad, T.L.; Lee, H.; Mcauley, J.H.; Sowden, G.; Wynne-Jones, G.; et al. Mechanisms of Vocational Interventions for Return to Work from Musculoskeletal Conditions: A Mediation Analysis of the MI-NAV Trial. Occup. Environ. Med. 2023, 80, 246–253. [Google Scholar] [CrossRef] [PubMed]
- Björk Brämberg, E.; Jensen, I.; Kwak, L. Nationwide Implementation of a National Policy for Evidence-Based Rehabilitation with Focus on Facilitating Return to Work: A Survey of Perceived Use, Facilitators, and Barriers. Disabil. Rehabil. 2020, 42, 219–227. [Google Scholar] [CrossRef] [PubMed]
- Couser, G.P.; Hagen, P.T.; Cowl, C.T.; Newcomb, R.D.; Swift, M.D. Part Two: Managing Physicians as Patients and Their Safe Return to Work. Mayo Clin. Proc. 2024, 99, 997–1005. [Google Scholar] [CrossRef]
- Miroshnychenko, A.; Uhlman, K.; Malone, J.; Waltho, D.; Thoma, A. Systematic Review of Reporting Quality of Economic Evaluations in Plastic Surgery Based on the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) Statement. J. Plast. Reconstr. Aesthetic Surg. 2021, 74, 2458–2466. [Google Scholar] [CrossRef]
- Ehteshami-Afshar, S.; Zafari, Z.; Hamidi, N.; FitzGerald, J.M.; Lynd, L.; Sadatsafavi, M. A Systematic Review of Decision-Analytic Models for Evaluating Cost-Effectiveness of Asthma Interventions. Value Health 2019, 22, 1070–1082. [Google Scholar] [CrossRef]

| Author, Year | Country | Type of Disease | Type of Disability | Age | Number of Patients |
|---|---|---|---|---|---|
| Tingulstad, 2023 [16] | Norway | Musculoskeletal disorder | Musculoskeletal disorders | Median 49 years (range 24-66) | 514 |
| Corbacho, 2021 [17] | United Kingdom | Frozen shoulder | Musculoskeletal disorders | Not Reported | 503 |
| Xin, 2020 [18] | United Kingdom | Parkinson’s disease | Neurological disorders | Mean age 71 (SD 7.7) in intervention group, 73 (SD 7.7) in control group | 474 |
| Lewkowicz, 2022 [19] | Germany | Low-back pain | Musculoskeletal disorders; Psychological Disorders | 41 years (mean) | 10,000 |
| Arora, 2017 [20] | India; Bangladesh | Pressure ulcers in spinal cord injury | Neurological disorders | 35 (SD 11) in intervention group, 36 (SD 12) in control group | 115 |
| Morgante, 2024 [21] | Norway | Musculoskeletal and psychological disorders | Musculoskeletal disorders; psychological disorders | 40 years (mean age) | 166 |
| Brusco, 2022 [22] | Australia | Stroke | Neurological | Not Reported | 30 |
| Sutton et al., 2020 [23] | United States | Spinal cord injury | Neurological disorders | 51.0 ± 10.1 years (PrOMOTE group), 49.8 ± 9.8 years (TAU group) | 213 |
| Pinto et al., 2020 [24] | United States | Spinal cord injury (SCI) | Neurological disorders | Mean age 43 years | Not Reported |
| Donnelley et al., 2022 [25] | Tanzania | Transfemoral amputation | Physical disability | Mean 45.9 years (SD 17.6) | 38 |
| Wagner et al., 2011 [26] | United States | Stroke | Neurological disorders | Not Reported | 127 |
| Author, Year | Intervention | Comparator | Program Details | Type of Rehabilitation Intervention |
|---|---|---|---|---|
| Tingulstad, 2023 [16] | Motivational interviewing (MI) and stratified care | Usual case management (UC) | Motivational interviewing sessions and vocational support | Medical (physiotherapy); vocational (stratified vocational advice intervention—SVAI); psychological (motivational interviewing—MI) |
| Corbacho, 2021 [17] | Manipulation under anesthesia (MUA), arthroscopic surgery | Standardized physiotherapy programs | Standardized physiotherapy programs, intra-articular injections | Medical: Early structured physiotherapy (ESP) with steroid injection; Vocational: not reported; Psychological: not reported |
| Xin, 2020 [18] | PDSAFE intervention | Usual care | Personalized physiotherapy program targeting balance and mobility | Medical: Personalized physiotherapy program |
| Lewkowicz, 2022 [19] | Digital therapeutic care app | Treatment as usual | Digital therapeutic care app with video-based guidance and feedback | Medical (digital therapeutic care app with video-based exercises and educational material); Psychological (decision-support interventions) |
| Arora, 2017 [20] | Telephone-based support | Usual care | Weekly telephone support reinforcing self-help strategies | Medical (education on wound care, diet, equipment use); Psychological (stress management); Vocational (self-help strategies) |
| Morgante, 2024 [21] | O-ACT (outpatient acceptance and commitment therapy) | Usual care | O-ACT: 6-week program with weekly sessions, homework assignments, and follow-up | O-ACT: Outpatient acceptance and commitment therapy (psychological); I-MORE: Inpatient multimodal occupational rehabilitation (medical, psychological, vocational) |
| Brusco, 2022 [22] | Robotics-based therapy (RBT) | Standardized outpatient therapy | Robotics-based therapy with standardized protocols for rehabilitation | Medical (robotics-based therapy for upper-limb rehabilitation); Conventional therapy (physiotherapy and occupational therapy) |
| Sutton et al., 2020 [23] | Supported employment program based on individual placement | Usual care | Individual placement and support model focusing on job placement and support | Vocational (individual placement and support employment program) |
| Pinto et al., 2020 [24] | Robotic exoskeleton over-ground training | Standard rehabilitation | Robotic exoskeleton training for locomotor rehabilitation | Robotic exoskeleton training (RT-exo), body-weight-supported treadmill training (BWSTT), over-ground training (OGT), stationary robotic systems (treadmill-based robotic gait orthoses) |
| Donnelley et al., 2022 [25] | Prosthesis provision | No prosthesis | Provision of modular endoskeletal transfemoral prosthesis with follow-up care | Medical: Prosthesis provision and gait training |
| Wagner et al., 2011 [26] | Robot-assisted therapy | Intensive comparison therapy | Robot-assisted therapy and intensive comparison to standard rehabilitation methods | Medical: Robot-assisted therapy; Intensive comparison therapy; Usual care |
| Author, Year | Economic Outcomes | Time Horizon | Threshold | ICER |
|---|---|---|---|---|
| Tingulstad, 2023 [16] | Cost-Effectiveness Analysis (CEA) | 6 months | NOK 275,000 (EUR 27,500/USD 35,628) per QALY | ICER for MI: EUR 1,756,221 per QALY; ICER for SVAI: EUR 1,553,061 per QALY |
| Corbacho, 2021 [17] | Cost Utility Analysis (CUA) | 1 year | GBP 20,000/QALY | GBP 6984 per additional QALY for MUA compared to ESP |
| Xin, 2020 [18] | Cost Utility Analysis (CUA) | 6 months; 12 months in sensitivity analysis | GBP 30,000/QALY | GBP 120,659 per QALY |
| Lewkowicz, 2022 [19] | Cost-Effectiveness Analysis (CEA) | 3 years | EUR 10,000/QALY and EUR 20,000/QALY | EUR 5486 per QALY |
| Arora, 2017 [20] | Cost-Effectiveness Analysis (CEA) | 12 weeks | Less than three times GDP per capita | INR 2306 (USD 130) per cm2 reduction; INR 44,915 (USD 2523) per QALY gained |
| Morgante, 2024 [21] | Cost-Effectiveness Analysis (CEA) | 25 years | USD 50,000 per QALY | USD 356,447 per QALY gained (healthcare perspective); I-MORE dominated O-ACT (societal perspective) |
| Brusco, 2022 [22] | Cost-Effectiveness Analysis (CEA) | 6 months (6 program cycles) | Not Reported | Not Reported |
| Sutton et al., 2020 [23] | Cost-Effectiveness Analysis (CEA) | 2 years | USD 50,000/QALY; USD 100,000/QALY | Not Reported |
| Pinto et al., 2020 [24] | Budget Impact Analysis (BIA) | 1 year | Not Reported | Not Reported |
| Donnelley et al., 2022 [25] | Cost-Effectiveness Analysis (CEA) | 1 year (study duration); Lifetime (modeled) | USD 1080 (conservative); USD 3140 (PPP-adjusted) | USD 242/QALY (payer, no replacement); USD 390/QALY (payer, with replacement); Dominated (societal perspective) |
| Wagner et al., 2011 [26] | Cost-Effectiveness Analysis (CEA) | 36 weeks | Not reported | Wide confidence region (-USD 450,255 to USD 393,356); uncertainty remains about cost-effectiveness |
| Author, Year | RTW Implication |
|---|---|
| Tingulstad, 2023 [16] | Reduction in sickness absence days: 5.1 days (UC + MI) and 7.9 days (UC + SVAI) over six months |
| Corbacho, 2021 [17] | Median lost workdays: 14 days (ESP), 56.5 days (MUA), 71.5 days (ACR) |
| Xin, 2020 [18] | Not Reported |
| Lewkowicz, 2022 [19] | 8 workdays lost per cycle |
| Arora, 2017 [20] | 8 workdays lost per cycle |
| Morgante, 2024 [21] | Workdays lost: O-ACT (GB: 21 days, DB: 24 days); I-MORE (GB: 20 days, DB: 18 days); I-MORE presents a faster RTW than O-ACT |
| Brusco, 2022 [22] | Not reported |
| Sutton et al., 2020 [23] | Not reported |
| Pinto et al., 2020 [24] | Cost savings from RT-exo adoption ranged from USD 1114 to USD 4784 annually across facilities |
| Donnelley et al., 2022 [25] | Return to work increased from 10% to 30% after 1 year; 20% increase attributed to prosthesis provision |
| Wagner et al., 2011 [26] | Not Reported |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurnianto, A.A.; Kovács, S.; Ágnes, N.; Kumar, P. Economic Evaluations of Rehabilitation Interventions: A Scoping Review with Implications for Return to Work Programs. Healthcare 2025, 13, 1152. https://doi.org/10.3390/healthcare13101152
Kurnianto AA, Kovács S, Ágnes N, Kumar P. Economic Evaluations of Rehabilitation Interventions: A Scoping Review with Implications for Return to Work Programs. Healthcare. 2025; 13(10):1152. https://doi.org/10.3390/healthcare13101152
Chicago/Turabian StyleKurnianto, Arie Arizandi, Sándor Kovács, Nagy Ágnes, and Prabhat Kumar. 2025. "Economic Evaluations of Rehabilitation Interventions: A Scoping Review with Implications for Return to Work Programs" Healthcare 13, no. 10: 1152. https://doi.org/10.3390/healthcare13101152
APA StyleKurnianto, A. A., Kovács, S., Ágnes, N., & Kumar, P. (2025). Economic Evaluations of Rehabilitation Interventions: A Scoping Review with Implications for Return to Work Programs. Healthcare, 13(10), 1152. https://doi.org/10.3390/healthcare13101152








