Impact of the COVID-19 Pandemic on Musculoskeletal Disorder-Related Absenteeism Among Pediatric Healthcare Workers
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.2.1. Inclusion Criteria
2.2.2. Exclusion Criteria
2.3. Data Collection
2.4. Data Analysis
2.5. Ethical Considerations
2.6. Potential Biases and Data Limitations
3. Results
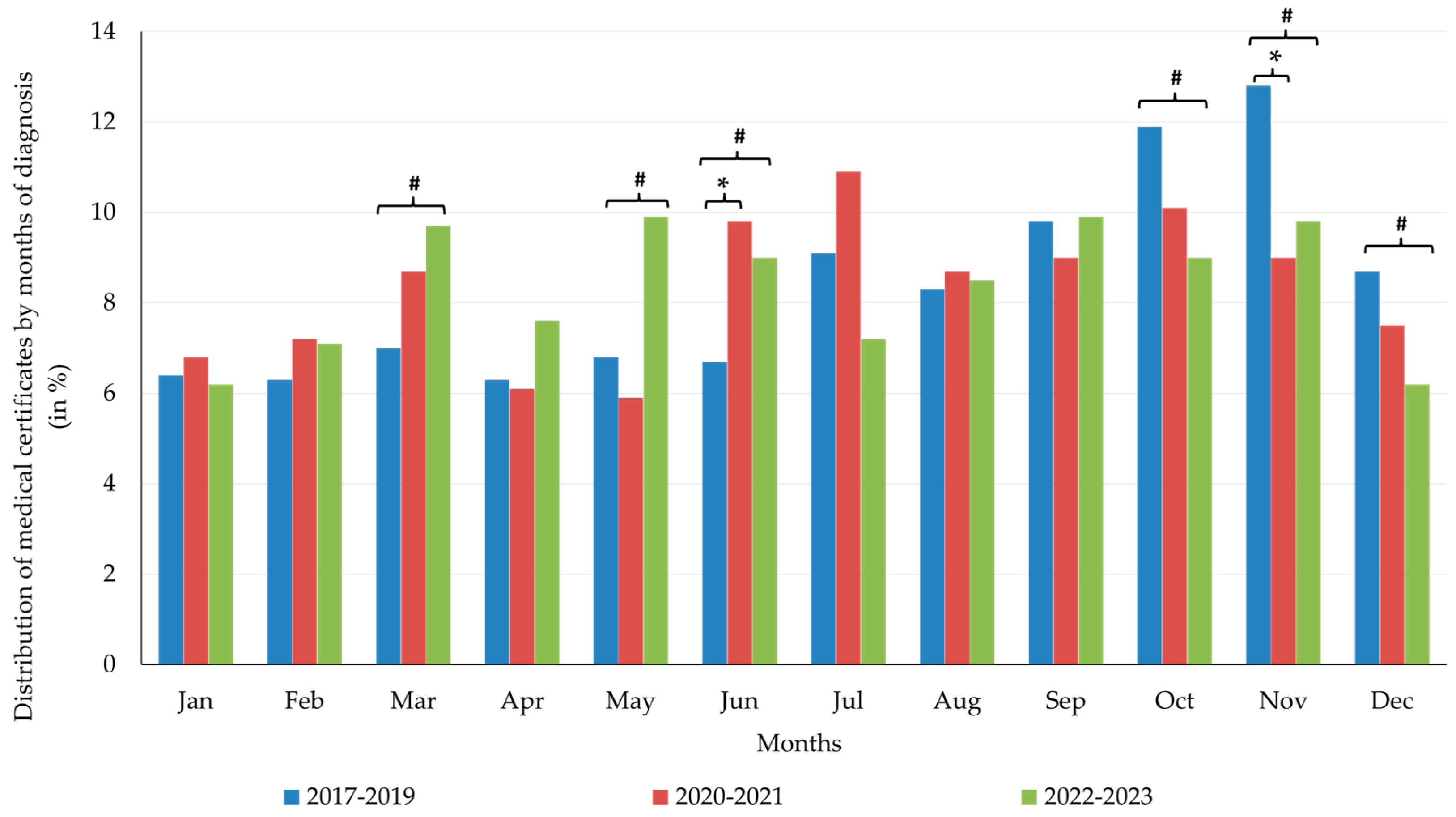
- For the 1019 certificates from the pre-pandemic period (2017–2019), the most frequent months were March (7%), July (9.1%), and November (12.8%) (p = 0.01);
- For the 1009 certificates from the pandemic period (2020–2021), the most frequent months were March (8.7%), July (10.9%), and October (10.1%) (p = 0.073);
- For the 1360 certificates in the post-pandemic period (2022–2023), the most frequent months were March (9.7%), May (9.9%), and September (9.9%) (p = 0.001).
4. Discussion
4.1. Gender-Specific Trends
4.2. Age-Related Vulnerability
4.3. Occupational Differences
4.4. Diagnostic-Specific Patterns
4.5. Temporal and Seasonal Patterns
4.6. Limitations of This Study
4.7. Implications for Policy and Practice
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| % | Percentage |
| ANOVA | Analysis of Variance |
| CI | Confidence Interval |
| COVID-19 | Coronavirus Disease 2019 |
| DaysC | Number of Calendar Days of Sick Leave |
| DaysL | Number of Working Days of Sick Leave |
| F | Female |
| HCWs | Healthcare Workers |
| IBM | International Business Machines |
| ICD-10 | International Statistical Classification of Diseases and Related Health Problems 10th Revision |
| IQR | Interquartile Range |
| JDCS Model | Job Demand–Control–Support Model |
| LR | Likelihood Ratio |
| Month Dg. | The Month of Disease Diagnosis |
| MSDs | Musculoskeletal Disorders |
| N | Number of Observations |
| OR | Odds Ratio |
| Period | The Pre-Pandemic (2017–2019), Pandemic (2020–2021), and Post-Pandemic (2022–2023) Periods |
| p-value | Probability Value (in statistical significance testing) |
| R2 | Coefficient of Determination |
| SD | Standard Deviation |
| SE | Standard Error |
| SPSS | Statistical Package for the Social Sciences |
| Y | Years |
References
- Eliasson, K.; Palm, P.; Nordander, C.; Dahlgren, G.; Lewis, C.; Hellman, T.; Svartengren, M.; Nyman, T. Study Protocol for a Qualitative Research Project Exploring an Occupational Health Surveillance Model for Workers Exposed to Hand-Intensive Work. Int. J. Environ. Res. Public Health 2020, 17, 6400. [Google Scholar] [CrossRef] [PubMed]
- Alruwaili, S.H.; Thirunavukkarasu, A.; Alanazi, R.M.; Alsharari, A.Y.; Alruwaili, D.K.; Alenzi, H.A.; Alruwaili, A.N.; Alruwaili, G.Q. Prevalence, Patterns, and Associated Factors for Musculoskeletal Disorders Among the Healthcare Workers of Northern Saudi Arabia: A Multicenter Cross-Sectional Study. J. Pain Res. 2023, 16, 3735–3746. [Google Scholar] [CrossRef]
- Rossetto, G.; Sala, E.; Albertelli, I.F.; Donatoni, C.; Mazzali, M.; Merlino, V.; Paraggio, E.; De Palma, G.; Lopomo, N.F. Musculoskeletal disorders and diseases in healthcare workers. A scoping review. Work 2024, 79, 1603–1612. [Google Scholar] [CrossRef]
- Teixeira, E.J.S.; Petersen, R.S.; Marziale, M.H.P. Work-related musculoskeletal disorders and work instability of nursing professionals. Rev. Bras. Med. Trab. 2022, 20, 206–214. [Google Scholar] [CrossRef] [PubMed]
- Amaro, J.; Magalhães, J.; Leite, M.; Aguiar, B.; Ponte, P.; Barrocas, J.; Norton, P. Musculoskeletal injuries and absenteeism among healthcare professionals-ICD-10 characterization. PLoS ONE 2018, 13, e0207837. [Google Scholar] [CrossRef] [PubMed]
- Garbin, A.J.Í.; Nascimento, C.C.M.P.; Zacharias, F.C.M.; Garbin, C.A.S.; Moimaz, S.A.S.; Saliba, N.A. Sickness absenteeism of Primary Health Care professionals before and during the COVID-19 pandemic. Rev. Bras. Enferm. 2022, 75, e20220028. [Google Scholar] [CrossRef]
- Waters, T.; Collins, J.; Galinsky, T.; Caruso, C. NIOSH research efforts to prevent musculoskeletal disorders in the healthcare industry. Orthop. Nurs. 2006, 25, 380–389. [Google Scholar] [CrossRef]
- Popa, M.V.; Mîndru, D.E.; Hizanu Dumitrache, M.; Gurzu, I.L.; Anton-Păduraru, D.T.; Ștreangă, V.; Gurzu, B.; Guțu, C.; Elkan, E.M.; Duceac, L.D. Stress Factors for the Paediatric and Adult Palliative Care Multidisciplinary Team and Workplace Wellbeing Solutions. Healthcare 2024, 12, 868. [Google Scholar] [CrossRef]
- Ridremont, D.; Boujut, E. Burnout among French pediatric healthcare workers during the COVID-19 pandemic. Psychol. Health Med. 2023, 28, 1901–1915. [Google Scholar] [CrossRef]
- Martin, S.R.; Heyming, T.; Morphew, T.; Sayrs, L.; Fortier, M.A.; Sanger, T.; Kain, Z.N. Impact of COVID-19 pandemic on pediatric healthcare burnout in acute care: A longitudinal study. Pediatr. Res. 2023, 94, 1771–1778. [Google Scholar] [CrossRef]
- Pozzer, D.; Luzardo, A.R.; Batista, J.D.L.; Barbato, P.R. Sickness absenteeism among health care workers in the municipal public service of Chapecó-SC, in the period 2015–2018. Rev. Bras. Med. Trab. 2024, 22, e2022962. [Google Scholar] [CrossRef]
- da Costa, B.R.; Vieira, E.R. Risk factors for work-related musculoskeletal disorders: A systematic review of recent longitudinal studies. Am. J. Ind. Med. 2010, 53, 285–323. [Google Scholar] [CrossRef] [PubMed]
- Koehoorn, M.; Demers, P.A.; Hertzman, C.; Village, J.; Kennedy, S.M. Work organization and musculoskeletal injuries among a cohort of health care workers. Scand. J. Work Environ. Health 2006, 32, 285–293. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.L.; Clausen, T.; Burr, H.; Holtermann, A. Threshold of musculoskeletal pain intensity for increased risk of long-term sickness absence among female healthcare workers in eldercare. PLoS ONE 2012, 7, e41287. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.; Clausen, T.; Mortensen, O.; Burr, H.; Holtermann, A. A prospective cohort study on musculoskeletal risk factors for long-term sickness absence among healthcare workers in eldercare. Int. Arch. Occup. Environ. Health 2011, 85, 615–622. [Google Scholar] [CrossRef]
- Magnavita, N.; Elovainio, M.; De Nardis, I.; Heponiemi, T.; Garbarino, S.; Magnavita, G.; Bergamaschi, A. Influence of environmental discomfort on musculoskeletal disorders. G. Ital. Med. Lav. Ergon. 2011, 33, 222–225. [Google Scholar]
- Zerbo Šporin, D.; Kozinc, Ž.; Prijon, T.; Metličar, T.; Šarabon, N. The impact of the COVID-19 pandemic on musculoskeletal disorders-related sick leave among healthcare workers: A retrospective analysis of Slovenian national data. Front. Public Health 2025, 12, 1478204. [Google Scholar] [CrossRef]
- Luger, T.; Maher, C.G.; Rieger, M.A.; Steinhilber, B. Work-break schedules for preventing musculoskeletal symptoms and disorders in healthy workers. Cochrane Database Syst. Rev. 2019, 7, CD012886. [Google Scholar] [CrossRef]
- Bos, E.H.; Krol, B.; Van Der Star, A.; Groothoff, J.W. The effects of occupational interventions on reduction of musculoskeletal symptoms in the nursing profession. Ergonomics 2006, 49, 706–723. [Google Scholar] [CrossRef]
- van Amelsvoort, L.G.; Spigt, M.G.; Swaen, G.M.; Kant, I. Leisure time physical activity and sickness absenteeism; a prospective study. Occup. Med. 2006, 56, 210–212. [Google Scholar] [CrossRef]
- Janc, M.; Jozwiak, Z.; Jankowska, A.; Makowiec-Dabrowska, T.; Kujawa, J.; Polanska, K. Ergonomics of E-Learning Workstations and the Prevalence of Musculoskeletal Disorders-Study among University Students. Int. J. Environ. Res. Public Health 2023, 20, 3309. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Kwon, M.J.; Choi, H.G.; Lee, S.J.; Hwang, S.; Lee, J.; Lee, S.H.; Lee, J.W. Changes in the mean incidence and variance of orthopedic diseases before and during the COVID-19 pandemic in Korea: A retrospective study. BMC Musculoskelet. Disord. 2023, 24, 540. [Google Scholar] [CrossRef] [PubMed]
- Gebrye, T.; Niyi-Odumosu, F.; Lawoe, J.; Mbada, C.; Fatoye, F. The impact of COVID-19 related lockdown restrictions on musculoskeletal health: A systematic review. Rheumatol. Int. 2023, 43, 2011–2019. [Google Scholar] [CrossRef] [PubMed]
- Fatoye, F.; Fatoye, C.; Lawoe, J.; Mbada, C.; Gebrye, T. Does COVID-19 Related Lockdown Restrictions Impact People with Musculoskeletal Disorders? A Systematic Review. Musculoskelet. Care 2024, 22, e1920. [Google Scholar] [CrossRef]
- Parsirad, M.; Oomen-Lochtefeld, S.; Suerig, B.; Wang, C. Has the COVID 19 Pandemic Impacted the Management of Chronic Musculoskeletal Pain? Curr. Rheumatol. Rep. 2023, 25, 128–143. [Google Scholar] [CrossRef]
- Aydin, A.; Atiç, R. Negative effects of the COVID-19 pandemic on the musculoskeletal system and depression in healthcare professionals. J. Back Musculoskelet. Rehabil. 2023, 36, 1273–1283. [Google Scholar] [CrossRef]
- Efe Is, E.; Sahillioglu, A.; Demirel, S.; Kuran, B.; Mustafa Ozdemir, H. Effect of COVID-19 Pandemic on Physical Activity Habits, Musculoskeletal Pain, and Mood of Healthcare Workers. Sisli Etfal Hastan. Tip Bul. 2021, 55, 462–468. [Google Scholar] [CrossRef]
- Pires, R.E.; Reis, I.G.N.; Waldolato, G.S.; Pires, D.D.; Bidolegui, F.; Giordano, V. What Do We Need to Know About Musculoskeletal Manifestations of COVID-19?: A Systematic Review. JBJS Rev. 2022, 10, e22.00013. [Google Scholar] [CrossRef]
- Snodgrass, S.J.; Weerasekara, I.; Edwards, S.; Heneghan, N.R.; Puentedura, E.J.; James, C. Relationships Between the Physical Work Environment, Postures and Musculoskeletal Pain During COVID-19: A Survey of Frequent Computer Users. J. Occup. Environ. Med. 2022, 64, e782–e791. [Google Scholar] [CrossRef]
- Sinha, P.R.; Mallick, N.; Sahu, R.L. Orthopedic Manifestations and Post-COVID-19 Infection. J. Pharm. Bioallied Sci. 2023, 15, S665–S668. [Google Scholar] [CrossRef]
- Crăciun, M.D.; Nițescu, G.V.; Golumbeanu, M.; Tănase, A.A.; Pițigoi, D.; Săndulescu, O.; Crăciun, P.; Enciu, B.G.; Bălănescu, R.N.; Ulici, A. mRNA COVID-19 Vaccine Reactogenicity among Healthcare Workers: Results from an Active Survey in a Pediatric Hospital from Bucharest, January-February 2021. Vaccines 2022, 10, 836. [Google Scholar] [CrossRef] [PubMed]
- Silva-Junior, J.S.; Martinez, M.C.; Sekiya, F.S.; de Miranda, C.B.; Fischer, F.M. Return to work after sick leave due to musculoskeletal disorder or injury: A longitudinal study conducted in Brazil. BMC Public Health 2023, 23, 1881. [Google Scholar] [CrossRef] [PubMed]
- Zahrawi, H.; Asaad, S.H.A.; Al Houri, A.N.; Kadri, S.A.; Kahal, F.; Torbey, A.; Al Houri, H.N.; Odeh, A.; Alshallah, N.; Dugha, G.; et al. The prevalence of work-related musculoskeletal disorder among health care workers in Damascus, Syria. A cross-sectional study. Health Sci. Rep. 2024, 7, e1860. [Google Scholar] [CrossRef] [PubMed]
- Jacquier-Bret, J.; Gorce, P. Prevalence of Body Area Work-Related Musculoskeletal Disorders among Healthcare Professionals: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 841. [Google Scholar] [CrossRef]
- Maltezou, H.C.; Ledda, C.; Sipsas, N.V. Absenteeism of Healthcare Personnel in the COVID-19 Era: A Systematic Review of the Literature and Implications for the Post-Pandemic Seasons. Healthcare 2023, 11, 2950. [Google Scholar] [CrossRef]
- Oranye, N.O.; Wallis, B.; Roer, K.; Archer-Heese, G.; Aguilar, Z. Do Personal Factors or Types of Physical Tasks Predict Workplace Injury? Workplace Health Saf. 2016, 64, 141–151. [Google Scholar] [CrossRef]
- Barbosa, R.E.; Assunção, A.Á.; de Araújo, T.M. Musculoskeletal pain among healthcare workers: An exploratory study on gender differences. Am. J. Ind. Med. 2013, 56, 1201–1212. [Google Scholar] [CrossRef]
- Robinson, L.J.; Engelson, B.J.; Hayes, S.N. Who is caring for healthcare workers’ families amid COVID-19? Acad. Med. J. Assoc. Am. Med. Coll. 2021, 96, 1254–1258. [Google Scholar] [CrossRef]
- Tobin-Tyler, E.; Adashi, E.Y. The ACGME’s New Paid Family and Medical Leave Policy: Just the Beginning. J. Am. Board Fam. Med. 2023, 36, 190–192. [Google Scholar] [CrossRef]
- Landry, L.G. Characterization of women’s occupational musculoskeletal exposures. AAOHN J. Off. J. Am. Assoc. Occup. Health Nurses 2007, 55, 351–359. [Google Scholar] [CrossRef]
- Vallejo, M.S.; Blümel, J.E.; Chedraui, P.; Tserotas, K.; Salinas, C.; Rodrigues, M.A.; Rodríguez, D.A.; Rey, C.; Ojeda, E.; Ñañez, M.; et al. Association of muscle disorders in late postmenopausal women according to the type of experienced menopause. Menopause 2024, 31, 641–646. [Google Scholar] [CrossRef] [PubMed]
- Newman, M.; Donahue, H.J.; Neigh, G.N. Connecting the dots: Sex, depression, and musculoskeletal health. J. Clin. Investig. 2024, 134, e180072. [Google Scholar] [CrossRef]
- Wei, W.; Qi, X.; Cheng, B.; Zhang, N.; Zhao, Y.; Qin, X.; He, D.; Chu, X.; Shi, S.; Cai, Q.; et al. Prospective study of associations between accelerated biological aging and twenty musculoskeletal disorders. Commun. Med. 2024, 4, 266. [Google Scholar] [CrossRef]
- Mihcin, S. Spinal curvature for the assessment of spinal stability. Int. J. Biomed. Eng. Technol. 2016, 20, 226–242. [Google Scholar] [CrossRef]
- Manning, C.; Ali, D.; Nagrecha, S. The influence of Gender/Sex on Work-Related Musculoskeletal Disorders: A Systematic Review and Meta-Analysis. In Human Factors in Design, Engineering, and Computing; Ahram, T., Karwowski, W., Eds.; AHFE International: Louisville, Ky, USA, 2024; Volume 159. [Google Scholar] [CrossRef]
- Punnett, L.; Gillespie, R.M.; Herbert, R. Work-Related Musculoskeletal Disorders: Is there a Gender Differential, and if so, What Does it Mean? In Women and Health, 2nd ed.; Goldman, M.B., Troisi, R., Rexrode, K.M., Eds.; Academic Press: Cambridge, MA, USA, 2013; pp. 613–624. [Google Scholar] [CrossRef]
- Silverstein, B.; Fan, Z.J.; Smith, C.K.; Bao, S.; Howard, N.; Spielholz, P.; Bonauto, D.; Viikari-Juntura, E. Gender adjustment or stratification in discerning upper extremity musculoskeletal disorder risk? Scand. J. Work Environ. Health 2009, 35, 113–126. [Google Scholar] [CrossRef] [PubMed]
- Campbell, E.; Popescu, G.H. Psychological distress, moral trauma, and burnout syndrome among COVID-19 frontline medical personnel. Psychosociological Issues Hum. Resour. Manag. 2021, 9, 63–76. [Google Scholar] [CrossRef]
- Korošec, D.; Vrbnjak, D.; Štiglic, G. Prevalence of mental disorders and high rates of absenteeism from work among healthcare professionals in Slovenia: A retrospective study. BMJ Open 2023, 13, e075718. [Google Scholar] [CrossRef]
- Duceac (Covrig), M.; Eva, L.; Dabija, M.G.; Stoica, G.; Druguș, D.; Duceac, L.-D.; Voinescu, D.-C. Does oral health affect your bone loss? The link between periodontitis disease and osteoporosis—An epidemiological approach to lumbar disc herniation in a neurosurgery hospital in the northeastern region of Romania. Rom. J. Oral Rehabil. 2023, 15, 44–53. [Google Scholar]
- Patrascu, A.; Savin, L.; Lupescu, O.; Mihailescu, D.; Mihai, D.N.; Neculaes, M.; Grigorescu, V.; Greierosu, C.; Botez, P. Multifocal osteonecrosis glucocorticoid induced. Rev. Chimie 2017, 68, 200–202. [Google Scholar] [CrossRef]
- Alexe, O.; Gainaru, C.; Serafinceanu, C.; Plesea-Condratovici, A.; Danciulescu-Miulescu, R.; Plesea-Condratovici, C. Patient-Reported Outcomes (PROs) in Romanian Type 2 Diabetic Patients: Results from a Multicentre National Registry. In Interdisciplinary Approaches in Diabetic Chronic Kidney Disease; Niculescu Publishing House: Bucharest, Romania, 2015; pp. 76–88. [Google Scholar]
- Alzahrani, M.S.; Hakeem, A.A.L.; Talmesany, T.A. Knowledge of the primary healthcare physicians in the Al-Baha region about COVID-19 personal protective measures. J. Fam. Med. Prim. Care 2022, 11, 4536–4544. [Google Scholar] [CrossRef]
- Muthelo, L.; Sinyegwe, N.F.; Phukubye, T.A.; Mbombi, M.O.; Ntho, T.A.; Mothiba, T.M. Prevalence of Work-Related Musculoskeletal Disorders and Its Effects amongst Nurses in the Selected Intellectual Disability Unit of the Limpopo Province. Healthcare 2023, 11, 777. [Google Scholar] [CrossRef] [PubMed]
- Sakr, C.J.; Fakih, L.M.; Musharrafieh, U.M.; Khairallah, G.M.; Makki, M.H.; Doudakian, R.M.; Tamim, H.; Redlich, C.A.; Slade, M.D.; Rahme, D.V. Absenteeism Among Healthcare Workers: Job Grade and Other Factors That Matter in Sickness Absence. Int. J. Environ. Res. Public Health 2025, 22, 127. [Google Scholar] [CrossRef]
- Palladino, R.; Mercogliano, M.; Fiorilla, C.; Frangiosa, A.; Iodice, S.; Sanduzzi Zamparelli, S.; Montella, E.; Triassi, M.; Sanduzzi Zamparelli, A. Association between COVID-19 and Sick Leave for Healthcare Workers in a Large Academic Hospital in Southern Italy: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 9670. [Google Scholar] [CrossRef] [PubMed]
- Schug, C.; Geiser, F.; Hiebel, N.; Beschoner, P.; Jerg-Bretzke, L.; Albus, C.; Weidner, K.; Morawa, E.; Erim, Y. Sick Leave and Intention to Quit the Job among Nursing Staff in German Hospitals during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 1947. [Google Scholar] [CrossRef] [PubMed]
- Arca, M.; Dönmezdil, S.; Durmaz, E.D. The effect of the COVID-19 pandemic on anxiety, depression, and musculoskeletal system complaints in healthcare workers. Work 2021, 69, 47–54. [Google Scholar] [CrossRef]
- Piel, S.; Presotto, M.A.; Jörres, R.A.; Karrasch, S.; Gesierich, W.; Bullwinkel, J.; Rabe, K.F.; Hayden, M.C.; Kaestner, F.; Harzheim, D.; et al. Cause and risk factors for absenteeism among medical staff in German specialized lung clinics during the COVID pandemic. Respir. Int. Rev. Thorac. Dis. 2023, 102, 924–933. [Google Scholar] [CrossRef]
- Nestor, S.; O’ Tuathaigh, C.; O’ Brien, T. Assessing the impact of COVID-19 on healthcare staff at a combined elderly care and specialist palliative care facility: A cross-sectional study. Palliat. Med. 2021, 35, 1492–1501. [Google Scholar] [CrossRef]
- Schrader, H.; Ruck, J.; Borgulya, G.; Parisi, S.; Ehlers-Mondorf, J.; Kaduszkiewicz, H.; Joos, S.; Grau, A.; Linde, K.; Gágyor, I. Stress experiences of healthcare assistants in family practice at the onset of the COVID-19 pandemic: A mixed methods study. Front. Public Health 2023, 11, 1238144. [Google Scholar] [CrossRef]
- Putekova, S.; Martinkova, J.; Urickova, A.; Kober, L.; Reichertova, S.; Plancikova, D.; Majdan, M. The impact of the COVID-19 pandemic on the health and working conditions of nurses and its implications for policies: A cross-sectional study in Slovakia. BMC Nurs. 2023, 22, 185. [Google Scholar] [CrossRef]
- Popa, M.V.; Bogdan Goroftei, E.R.; Guțu, C.; Duceac (Covrig), M.; Marcu, C.; Popescu, M.R.; Druguș, D.; Duceac, L.-D. Observational study of post-COVID-19 syndrome in health care workers infected with SARS-CoV-2 virus: General and oral cavity complications. Rom. J. Oral Rehabil. 2023, 15, 198–207. [Google Scholar]
- Barros, C.; Baylina, P. Disclosin. Strain: How Psychosocial Risk Factors Influence Work-Related Musculoskeletal Disorders in Healthcare Workers Preceding and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2024, 21, 564. [Google Scholar] [CrossRef] [PubMed]
- Restrepo-Martínez, M.; Escobar, M.; Marín, L.A.; Restrepo, D. Prevalence and clinical characteristics of depression and symptoms of anxiety in staff at a health institution in Medellin during the COVID-19 pandemic. Rev. Colomb. Psiquiatria 2023, 52, 51–57. [Google Scholar] [CrossRef]
- Giorgi, G.; Lecca, L.I.; Alessio, F.; Finstad, G.L.; Bondanini, G.; Lulli, L.G.; Arcangeli, G.; Mucci, N. COVID-19-Related Mental Health Effects in the Workplace: A Narrative Review. Int. J. Environ. Res. Public Health 2020, 17, 7857. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, D.; Esin, M.N. Predisposing factors for musculoskeletal symptoms in intensive care unit nurses. Int. Nurs. Rev. 2015, 62, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Sierpińska, L.E.; Ptasińska, E. Evaluation of work conditions of nurses employed in a shift system in hospital wards during the COVID-19 pandemic. Work 2023, 75, 401–412. [Google Scholar] [CrossRef]
- Macaluso, F.; Macaluso, M.; Daraiseh, N.M. The psychosocial work environment, musculoskeletal disorders and their functional consequences among pediatric healthcare providers. Ann. Epidemiol. 2021, 58, 76–82. [Google Scholar] [CrossRef]
- Ibrahim, N.I.; Mohanadas, D. Prevalence of musculoskeletal disorders among staffs in specialized healthcare centre. Work 2012, 41, 2452–2460. [Google Scholar] [CrossRef]
- Almhdawi, K.A.; Alrabbaie, H.; Arabiat, A.; Almahdawi, S.; Alhammouri, A.T.; Nadar, M.S.; Al-Tamimi, F.; Obeidat, D.; Alazrai, A.; Jaber, H. Quality of life and its health and occupational determinants among hospital-based nurses during the COVID-19 pandemic. Work 2023, 74, 1321–1329. [Google Scholar] [CrossRef]
- Krishnan, K.S.; Raju, G.; Shawkataly, O. Prevalence of Work-Related Musculoskeletal Disorders: Psychological and Physical Risk Factors. Int. J. Environ. Res. Public Health 2021, 18, 9361. [Google Scholar] [CrossRef]
- Popa, M.V.; Luchian, N.; Gurzu, B.; Gurzu, I.L.; Duceac, L.D. Neurological complications in infection with the SARS-CoV-2 virus: Parkinson’s disease and the impact on professional reintegration—Case study. Rom. J. Occup. Med. 2022, 73, 35–39. [Google Scholar] [CrossRef]
- de Wilton, A.; Kilich, E.; Chaudhry, Z.; Bell, L.C.; Gahir, J.; Cadman, J.; Lever, R.A.; Logan, S.A.; UCLH COVID-19 Response Team. Delayed healthcare seeking and prolonged illness in healthcare workers during the COVID-19 pandemic: A single-centre observational study. BMJ Open 2020, 10, e040216. [Google Scholar] [CrossRef]
- Edge, R.; van der Plaat, D.A.; Parsons, V.; Coggon, D.; van Tongeren, M.; Muiry, R.; Madan, I.; Cullinan, P. Changing patterns of sickness absence among healthcare workers in England during the COVID-19 pandemic. J. Public Health 2022, 44, e42–e50. [Google Scholar] [CrossRef] [PubMed]
- Kirk, A.H.P.; Chong, S.L.; Kam, K.Q.; Huang, W.; Ang, L.S.L.; Lee, J.H.; Sultana, R.; Hon, K.L.; Wong, J.J.M. Psychosocial impact of the COVID-19 pandemic on paediatric healthcare workers. Ann. Acad. Med. Singap. 2021, 50, 203–211. [Google Scholar] [CrossRef]
- Koutsouri, A.K.; Gkentzi, D.; Paraskevas, T.; Michailides, C.; Papantoniou, K.; Kavvousanos, M.; Kantanis, A.; Assimakopoulos, S.; Marangos, M.; Lagadinou, M. Burnout Among Healthcare Workers During Covid-19 Pandemic: Results from Seven Hospitals in Western Greece. Mater. Socio Medica 2023, 35, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Karasek, R.A. Job demands, job decision latitude, and mental strain: Implications for job redesign. Adm. Sci. Q. 1979, 24, 285–308. [Google Scholar] [CrossRef]
- Johnson, J.V.; Hall, E.M. Job strain, workplace social support, and cardiovascular disease: A cross-sectional study. Am. J. Public Health 1988, 78, 1336–1342. [Google Scholar] [CrossRef]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef]
- Fayzi, R.; Karimi, A.; Fereidouni, A.; Salavatian, A.; Imani, B.; Tavakkol, R. Prevalence and clinical characteristics of low back pain among operating room personnel: A cross-sectional study in South of Iran. Front. Surg. 2022, 9, 841339. [Google Scholar] [CrossRef]
- Duceac (Covrig), M.; Gutu, C.; Eva, L.; Dabija, M.G.; Calin, G.; Duceac, L.D.; Ciupilan, C.; Voinescu, D.C. Retrospective study of lumbar disc herniation in a hospital in north-eastern Romania. Balneo PRM Res. J. 2024, 15, 666. [Google Scholar] [CrossRef]
- Kim, J.Y.; Shin, J.S.; Lim, M.S.; Choi, H.G.; Kim, S.K.; Kang, H.T.; Koh, S.B.; Oh, S.S. Relationship between simultaneous exposure to ergonomic risk factors and work-related lower back pain: A cross-sectional study based on the fourth Korean working conditions survey. Ann. Occup. Environ. Med. 2018, 30, 58. [Google Scholar] [CrossRef]
- Kakaraparthi, V.N.; Vishwanathan, K. Increased prevalence of work-related musculoskeletal disorders among physiotherapists during the COVID-19 pandemic: A Commentary. Work 2022, 72, 1191–1193. [Google Scholar] [CrossRef] [PubMed]
- Bouziri, H.; Descatha, A.; Roquelaure, Y.; Dab, W.; Jean, K. Can we distinguish the roles of demographic and temporal changes in the incidence and prevalence of musculoskeletal disorders? A systematic review. Scand. J. Work Environ. Health 2022, 48, 253–263. [Google Scholar] [CrossRef] [PubMed]
- Ateş, R.; Yakut, H. Investigation of musculoskeletal disorders, physical activity level, sleep quality, and fatigue in health professionals with and without a history of COVID-19. Work 2023, 74, 1277–1287. [Google Scholar] [CrossRef] [PubMed]
- Glette, M.K.; Bates, D.W.; Dykes, P.C.; Wiig, S.; Kringeland, T. A resilience perspective on healthcare personnels’ experiences of managing the COVID-19 pandemic: A qualitative study in Norwegian nursing homes and come care services. BMC Health Serv. Res. 2023, 23, 1177. [Google Scholar] [CrossRef]
- Bütün, A.; Yeşil, Y. Cross-Sectional Study of Emergency Care Services During the COVID-19 Pandemic: A Multicenter Study of Healthcare Staff Perspectives. Cureus 2024, 16, e61475. [Google Scholar] [CrossRef]
- Mostafa, R.; El-Atawi, K. Strategies to Measure and Improve Emergency Department Performance: A Review. Cureus 2024, 16, e52879. [Google Scholar] [CrossRef]
- David, E.; DePierro, J.M.; Marin, D.B.; Sharma, V.; Charney, D.S.; Katz, C.L. COVID-19 Pandemic Support Programs for Healthcare Workers and Implications for Occupational Mental Health: A Narrative Review. Psychiatr. Q. 2022, 93, 227–247. [Google Scholar] [CrossRef]
- Cohen, C.; Pignata, S.; Bezak, E.; Tie, M.; Childs, J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: A systematic review. BMJ Open 2023, 13, e071203. [Google Scholar] [CrossRef]
- De Vries, N.; Lavreysen, O.; Boone, A.; Bouman, J.; Szemik, S.; Baranski, K.; Godderis, L.; De Winter, P. Retaining Healthcare Workers: A Systematic Review of Strategies for Sustaining Power in the Workplace. Healthcare 2023, 11, 1887. [Google Scholar] [CrossRef]
- Byrne, J.P.; Humphries, N.; McMurray, R.; Scotter, C. COVID-19 and healthcare worker mental well-being: Comparative case studies on interventions in six countries. Health Policy 2023, 135, 104863. [Google Scholar] [CrossRef]
- Pop, T.L.; Burlea, M.; Falup-Pecurariu, O.; Borzan, C.; Gabor-Harosa, F.; Herdea, V.; Pop, C.F.; Rajka, D.; Ognean, M.L.; Căinap, S.S. Overview of the pediatric healthcare system in Romania. Turk Pediatri Ars. 2020, 55, 69–84. [Google Scholar] [CrossRef] [PubMed]
- Kantor, C.; Corlade-Andrei, M.; Nedelea, P.; Ursu, R.; Bulgaru, D.; Cimpoesu, D. Assessing the resilience of healthcare professionals in a Romanian emergency unit during the COVID-19 pandemic. Rev. Med. Chir. 2023, 127, 19–31. [Google Scholar] [CrossRef]
- Tanner, A.R.; Dorey, R.B.; Brendish, N.J.; Clark, T.W. Influenza vaccination: Protecting the most vulnerable. Eur. Respir. Rev. Off. J. Eur. Respir. Soc. 2021, 30, 200258. [Google Scholar] [CrossRef]
- Mansoor, S.N.; Al Arabia, D.H.; Rathore, F.A. Ergonomics and musculoskeletal disorders among health care professionals: Prevention is better than cure. JPMA J. Pak. Med. Assoc. 2022, 72, 1243–1245. [Google Scholar] [CrossRef]
- Bernardes, J.M.; Monteiro-Pereira, P.E.; Gómez-Salgado, J.; Ruiz-Frutos, C.; Dias, A. Healthcare workers’ knowledge for safe handling and moving of the patient. Int. J. Occup. Saf. Ergon. 2022, 28, 2105–2111. [Google Scholar] [CrossRef]
- Søvold, L.E.; Naslund, J.A.; Kousoulis, A.A.; Saxena, S.; Qoronfleh, M.W.; Grobler, C.; Münter, L. Prioritizing the Mental Health and Well-Being of Healthcare Workers: An Urgent Global Public Health Priority. Front. Public Health 2021, 9, 679397. [Google Scholar] [CrossRef]
- Pollock, A.; Campbell, P.; Cheyne, J.; Cowie, J.; Davis, B.; McCallum, J.; McGill, K.; Elders, A.; Hagen, S.; McClurg, D.; et al. Interventions to support the resilience and mental health of frontline health and social care professionals during and after a disease outbreak, epidemic or pandemic: A mixed methods systematic review. Cochrane Database Syst. Rev. 2020, 11, CD013779. [Google Scholar] [CrossRef] [PubMed]
- Estephan, L.; Pu, C.; Bermudez, S.; Waits, A. Burnout, mental health, physical symptoms, and coping behaviors in healthcare workers in Belize amidst COVID-19 pandemic: A nationwide cross-sectional study. Int. J. Soc. Psychiatry 2023, 69, 1033–1042. [Google Scholar] [CrossRef]
- Duceac, L.D.; Eva, L.; Dabija, M.; Ciuhodaru, T.; Guțu, C.; Romila, L.; Nazarie, S. Prevention and limitation of Coronavirus SARS-CoV-2 cases in hospitals and dental medicine offices. Int. J. Med. Dent. 2020, 24, 149–156. [Google Scholar]
- Kłak, A.; Raciborski, F.; Samel-Kowalik, P. Social implications of rheumatic diseases. Reumatologia 2016, 54, 73–78. [Google Scholar] [CrossRef]
- Buck, R.; Wynne-Jones, G.; Varnava, A.; Main, C.J.; Phillips, C.J. Working with Musculoskeletal Pain. Rev. Pain 2009, 3, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Brito, M.P.; Chen, Z.; Wise, J.; Mortimore, S. Quantifying the impact of environment factors on the risk of medical responders’ stress-related absenteeism. Risk Anal. Off. Publ. Soc. Risk Anal. 2022, 42, 1834–1851. [Google Scholar] [CrossRef] [PubMed]
- Abzhandadze, T.; Westerlind, E.; Persson, H. Impact of pre-pandemic sick leave diagnoses on the length of COVID-19-related sick leave: A nationwide registry-based study. BMC Public Health 2023, 23, 195. [Google Scholar] [CrossRef] [PubMed]
- Neculăeș, M.; Hernandez-Lucas, P.; Lucaci, P. Implications of Stabilometric Assessment in Determining Functional Deficits in Patients with Severe Knee Osteoarthritis: Observational Study. J. Clin. Med. 2024, 13, 3181. [Google Scholar] [CrossRef]


| Arthropathies | Dorsopathies | Other MSD Diseases | Trauma/Fracture | Total | Chi Square Test | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Cases | % | No. of Cases | % | No. of Cases | % | No. of Cases | % | No. of Cases | % | p | |
| 217 | 6.40 | 2116 | 62.46 | 147 | 4.34 | 908 | 26.80 | 3388 | 100 | ||
| Period | |||||||||||
| 2017–2019 | 64 | 29.5 | 597 | 28.2 | 40 | 27.2 | 318 | 35.0 | 1019 | 30.1 | |
| 2020–2021 | 68 | 31.3 | 693 | 32.8 | 41 | 27.9 | 207 | 22.8 | 1009 | 29.8 | 0.001 |
| 2023–2023 | 85 | 39.2 | 826 | 39.0 | 66 | 44.9 | 383 | 42.2 | 1360 | 40.1 | |
| Gender | |||||||||||
| Male | 17 | 7.9 | 269 | 12.8 | 10 | 6.8 | 150 | 16.6 | 446 | 13.2 | |
| Female | 199 | 92.1 | 1833 | 87.2 | 137 | 93.2 | 754 | 83.4 | 2923 | 86.8 | 0.001 |
| Age | |||||||||||
| <46 years | 40 | 18.4 | 783 | 37.3 | 56 | 38.1 | 379 | 41.9 | 1258 | 37.3 | |
| ≥46 years | 176 | 81.5 | 1319 | 62.7 | 91 | 61.9 | 525 | 58.1 | 2111 | 62.7 | 0.001 |
| Occupation | |||||||||||
| Physician | 19 | 8.8 | 279 | 13.2 | 13 | 8.8 | 118 | 13.0 | 429 | 12.7 | |
| Nurse | 114 | 52.5 | 985 | 46.6 | 80 | 54.4 | 403 | 44.4 | 1582 | 46.7 | 0.025 |
| Porter, carer | 63 | 29.0 | 537 | 25.4 | 40 | 27.2 | 270 | 29.7 | 910 | 26.9 | |
| Registrar | 8 | 3.7 | 118 | 5.6 | 6 | 4.1 | 52 | 5.7 | 184 | 5.4 | |
| Auxiliary staff | 1 | 0.5 | 39 | 1.8 | 3 | 2.0 | 15 | 1.7 | 58 | 1.7 | |
| Administrative staff | 10 | 4.6 | 112 | 5.3 | 3 | 2.0 | 34 | 3.7 | 159 | 4.7 | |
| Other HCWs with higher ed. qualification | - | - | 20 | 1.0 | 2 | 1.4 | 11 | 1.2 | 33 | 1.0 | |
| N | 3388 | |
| Mean | 8.25 | |
| Median | 6 | |
| Standard Deviation | 5.86 | |
| Variance | 34.32 | |
| Skewness Test | 1.335 | |
| Skewness Standard Error | 0.042 | |
| Minimum | 1 | |
| Maximum | 31 | |
| Percentiles | 25th | 4 |
| 50th | 6 | |
| 75th | 12 | |
| N | 3388 | |
| Mean | 6.14 | |
| Median | 5 | |
| Standard Deviation | 4.03 | |
| Variance | 16.22 | |
| Skewness Test | 1.160 | |
| Skewness Standard Error | 0.042 | |
| Minimum | 0 | |
| Maximum | 23 | |
| Percentile | 25th | 3 |
| 50th | 5 | |
| 75th | 9 | |
| Clinical Characteristics | Arthropathies (n = 217) | Dorsopathies (n = 2116) | Other MSDs (n = 147) | Trauma/Fracture (n = 908) | Total Lot (n = 3388) | Chi-Square Test p |
|---|---|---|---|---|---|---|
| Calendar days | ||||||
| Mean ± SD | 10.14 ± 6.24 | 7.38 ± 4.86 | 8.25 ± 5.09 | 9.83 ± 7.38 | 8.25 ± 5.86 | 0.001 |
| Min–Max | 1–31 | 1–31 | 1–23 | 1–31 | 1–31 | |
| Working days | ||||||
| Mean ± SD | 7.53 ± 4.41 | 5.69 ± 3.43 | 6.16 ± 3.61 | 6.87 ± 5.00 | 6.14 ± 4.03 | 0.001 |
| Min–Max | 0–21 | 0–22 | 0–17 | 0–23 | 0–23 |
| Characteristics of the Analyzed Group of HCWs | Mean Value (± Standard Deviation) of Calendar Days of Sick Leave In | Analysis of Variance (ANOVA) Comparing the Pre-Pandemic, Pandemic, and Post-Pandemic Periods | ||
|---|---|---|---|---|
| Gender | Pre-pandemic period | Pandemic period | Post-pandemic period | p-value (ANOVA) |
| Male | 9.56 ± 7.19 | 7.41 ± 5.87 | 6.96 ± 5.31 | 0.001 |
| Female | 8.92 ± 6.15 | 8.27 ± 5.62 | 7.87 ± 5.66 | 0.001 |
| Age | Pre-pandemic period | Pandemic period | Post-pandemic period | p-value (ANOVA) |
| <46 y | 8.56 ± 6.50 | 7.97 ± 5.91 | 7.62 ± 5.64 | 0.069 |
| ≥46 y | 9.42 ± 6.14 | 8.27 ± 5.41 | 7.83 ± 5.62 | 0.001 |
| Diseases | Pre-pandemic period | Pandemic period | Post-pandemic period | p-value (ANOVA) |
| Arthropathies | 10.84 ± 6.79 | 10.26 ± 6.02 | 9.62 ± 6.00 | 0.432 |
| Dorsopathies | 7.95 ± 4.95 | 7.35 ± 4.64 | 6.86 ± 4.93 | 0.001 |
| Other MSDs | 8.35 ± 5.01 | 7.66 ± 4.76 | 8.56 ± 5.37 | 0.668 |
| Trauma/fracture | 10.72 ± 8.01 | 9.62 ± 7.74 | 9.21 ± 6.54 | 0.023 |
| Occupation | Pre-pandemic period | Pandemic period | Post-pandemic period | p-value (ANOVA) |
| Physician | 8.55 ± 7.05 | 6.15 ± 5.99 | 5.20 ± 4.10 | 0.001 |
| Medical assistant | 8.81 ± 6.32 | 8.46 ± 5.51 | 8.35 ± 5.97 | 0.456 |
| Carer, porter | 10.20 ± 6.68 | 8.96 ± 5.85 | 7.84 ± 5.53 | 0.001 |
| Medical registrar | 7.63 ± 4.95 | 7.94 ± 4.62 | 8.36 ± 5.02 | 0.615 |
| Auxiliary staff | 6.71 ± 4.15 | 7.82 ± 3.34 | 8.09 ± 5.14 | 0.549 |
| Administrative staff | 8.76 ± 4.94 | 6.28 ± 3.89 | 8.73 ± 4.64 | 0.009 |
| Other staff with higher education | 5.11 ± 3.25 | 5.82 ± 4.31 | 5.09 ± 3.51 | 0.401 |
| Logistic Regression Models Tailored Model | Independent Variables | OR (95% CI) | p-Value |
|---|---|---|---|
| Arthropathy Gender (F) | |||
| Time frame | Pre-pandemic (1) | 8.000 (4.274–6.656) | 0.001 |
| Pandemic (2) | 21.667 (6.810–68.936) | 0.001 | |
| Month of diagnosis | January | 5.765 (0.618–53.669) | 0.124 |
| March | 7.132 (1.993–25.514) | 0.003 | |
| April | 2.308 (0.561–9.490) | 0.246 | |
| May | 14.804 (1.935–113.25) | 0.009 | |
| June | 2.498 (0.939–6.643) | 0.067 | |
| July | 10.381 (2.296–46.934) | 0.002 | |
| November | 11.541 (1.408–94.624) | 0.023 | |
| Age | ≥46 years | 1.857 (1.039–3.526) | 0.003 |
| Number of calendar days of sick leave | 1.043 (0.931–1.168) | 0.246 | |
| Number of working days lost due to sick leave | 1.043 (0.965–1.128) | 0.284 | |
| Logistic Regression Models Tailored Model | Independent Variables | OR (95% CI) | p-Value |
|---|---|---|---|
| Dorsopathy Gender (F) | |||
| Time frame | Pre-pandemic (1) | 5.333 (3.646–6.656) | 0.001 |
| Pandemic (2) | 7.378 (5.858–9.292) | 0.001 | |
| Month of diagnosis | January | 4.572 (2.873–7.277) | 0.001 |
| February | 13.539 (6.832–26.831) | 0.001 | |
| March | 8.129 (4.876–13.554) | 0.001 | |
| April | 7.210 (4.170–12.465) | 0.001 | |
| May | 4.290 (2.838–6.485) | 0.001 | |
| June | 3.847 (2.526–5.941) | 0.001 | |
| July | 9.271 (5.272–16.306) | 0.001 | |
| August | 3.559 (2.412–5.250) | 0.001 | |
| September | 5.857 (3.805–9.017) | 0.001 | |
| October | 6.779 (4.329–10.615) | 0.001 | |
| November | 7.416 (4.329–10.615) | 0.001 | |
| Age | ≥46 years | 1.302 (1.000–1.903) | 0.006 |
| Number of calendar days of sick leave | 1.170 (1.122–1.219) | 0.001 | |
| Number of working days lost due to sick leave | 0.917 (0.827–1.016) | 0.098 | |
| Logistic Regression Models Tailored Model | Independent Variables | OR (95% CI) | p-Value |
|---|---|---|---|
| Other musculoskeletal disorders Gender (F) | |||
| Period | Pre-pandemic (1) | 7.873 (5.358–69.893) | 0.001 |
| Month of diagnosis | January | 6.289 (1.765–51.697) | 0.087 |
| March | 8.124 (1.010–65.317) | 0.049 | |
| September | 8.836 (1.116–69.976) | 0.039 | |
| October | 3.473 (0.717–16.830) | 0.122 | |
| November | 2.089 (0.390–11.185) | 0.390 | |
| Age | ≥46 years | 1.058 (0.899–1.090) | 0.058 |
| Number of calendar days of sick leave | 1.410 (0.034–5.470) | 0.619 | |
| Number of working days lost due to sick leave | 0.784 (0.208–2.138) | 0.635 | |
| Logistic Regression Models Tailored Model | Independent Variables | OR (95% CI) | p-Value |
|---|---|---|---|
| Trauma/injuries/fractures Gender (F) | |||
| Period | Pre-pandemic (1) | 4.925 (3.665–6.616) | 0.001 |
| Pandemic (2) | 2.764 (2.030–3.762) | 0.001 | |
| Month of diagnosis | January | 5.356 (2.882–8.448) | 0.001 |
| March | 6.257 (3.000–13.051) | 0.001 | |
| April | 5.276 (2.612–10.655) | 0.001 | |
| May | 4.506 (2.343–8.664) | 0.001 | |
| June | 3.367 (2.013–5.631) | 0.001 | |
| July | 5.282 (2.931–9.520) | 0.001 | |
| August | 4.802 (2.594–8.891) | 0.001 | |
| September | 2.685 (1.622–4.445) | 0.001 | |
| October | 2.810 (1.708–4.622) | 0.001 | |
| November | 6.252 (3.423–11.418) | 0.001 | |
| Age | ≥46 years | 1.052 (0.653–1.740) | 0.049 |
| Number of calendar days of sick leave | 1.520 (1.018–1.987) | 0.003 | |
| Number of working days lost due to sick leave | 1.049 (0.915–1.204) | 0.491 | |
| Diagnosis | Adjusted R2 | Std. Error | Regression Equation | p-Value |
|---|---|---|---|---|
| Arthropathy | 0.964 | 1.176 | Y = 1.21 − 0.45 (Period) − 0.01 (MonthDg) − 0.03 (Age) + 1.39 (DaysC) | 0.001 |
| Dorsopathy | 0.939 | 1.2 | Y = −0.177 − 0.086 (Period) − 0.009 (MonthDg) − 0.001 (Age) + 1.374 (DaysC) | 0.001 |
| Other MSDs | 0.95 | 1.135 | Y = 0.694 + 0.022 (Period) − 0.046 (MonthDg) − 0.014 (Age) + 1.371 (DaysC) | 0.001 |
| Trauma/Fracture | 0.971 | 1.265 | Y = −0.678 − 0.043 (Period) + 0.007 (MonthDg) + 0.012 (Age) + 1.452 (DaysC) | 0.001 |
| Model | Component | Real-World Application in This Study |
|---|---|---|
| Job Demand–Control–Support (JDCS) Model [78,79] | Job Demands | Pediatric nurses face frequent lifting of patients, prolonged standing, emotionally intense care, and increased workload during the pandemic. |
| Job Control | Limited autonomy over shift schedules, task allocation, and pacing of work. | |
| Social Support | Reduced peer and managerial support during COVID-19 increased isolation and stress. | |
| Implication | High demands, low control, and low support collectively raise occupational stress and risk of MSD-related absenteeism. | |
| Biopsychosocial Model [80] | Biological Factors | Age-related vulnerability (>46 years), repetitive musculoskeletal strain, and diagnosis-specific risks such as dorsopathies. |
| Psychological Factors | Increased emotional burden, anxiety, and burnout, especially during the pandemic and in high-responsibility care roles. | |
| Social Factors | Gender-based role expectations, work–home imbalance, and institutional ergonomics (e.g., poor lifting support). | |
| Implication | Absenteeism reflects the cumulative effect of interacting physical, psychological, and social stressors. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popa, M.V.; Gurzu, I.L.; Handra, C.M.; Gurzu, B.; Pleșea Condratovici, A.; Duceac, M.; Elkan, E.M.; Mîndru, D.E.; Dabija, V.A.; Duceac, L.D. Impact of the COVID-19 Pandemic on Musculoskeletal Disorder-Related Absenteeism Among Pediatric Healthcare Workers. Healthcare 2025, 13, 1116. https://doi.org/10.3390/healthcare13101116
Popa MV, Gurzu IL, Handra CM, Gurzu B, Pleșea Condratovici A, Duceac M, Elkan EM, Mîndru DE, Dabija VA, Duceac LD. Impact of the COVID-19 Pandemic on Musculoskeletal Disorder-Related Absenteeism Among Pediatric Healthcare Workers. Healthcare. 2025; 13(10):1116. https://doi.org/10.3390/healthcare13101116
Chicago/Turabian StylePopa, Maria Valentina, Irina Luciana Gurzu, Claudia Mariana Handra, Bogdan Gurzu, Alina Pleșea Condratovici, Mădălina Duceac (Covrig), Eva Maria Elkan, Dana Elena Mîndru, Vlad Andrei Dabija, and Letiția Doina Duceac. 2025. "Impact of the COVID-19 Pandemic on Musculoskeletal Disorder-Related Absenteeism Among Pediatric Healthcare Workers" Healthcare 13, no. 10: 1116. https://doi.org/10.3390/healthcare13101116
APA StylePopa, M. V., Gurzu, I. L., Handra, C. M., Gurzu, B., Pleșea Condratovici, A., Duceac, M., Elkan, E. M., Mîndru, D. E., Dabija, V. A., & Duceac, L. D. (2025). Impact of the COVID-19 Pandemic on Musculoskeletal Disorder-Related Absenteeism Among Pediatric Healthcare Workers. Healthcare, 13(10), 1116. https://doi.org/10.3390/healthcare13101116






