Person-Centred Diabetes Care: Examining Patient Empowerment and Diabetes-Specific Quality of Life in Slovenian Adults with Type 2 Diabetes
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Setting
2.3. Healthcare Context
2.4. Integrated Primary Care Model
2.4.1. Study Population and Patient Recruitment
2.4.2. Inclusion and Exclusion Criteria
2.5. Data Collection
2.5.1. Sociodemographic and Clinical Characteristics
2.5.2. Diabetes Empowerment Scale (DES)
2.5.3. Audit of Diabetes-Dependent Quality of Life (ADDQoL)
2.6. Sample Size Calculation
2.7. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
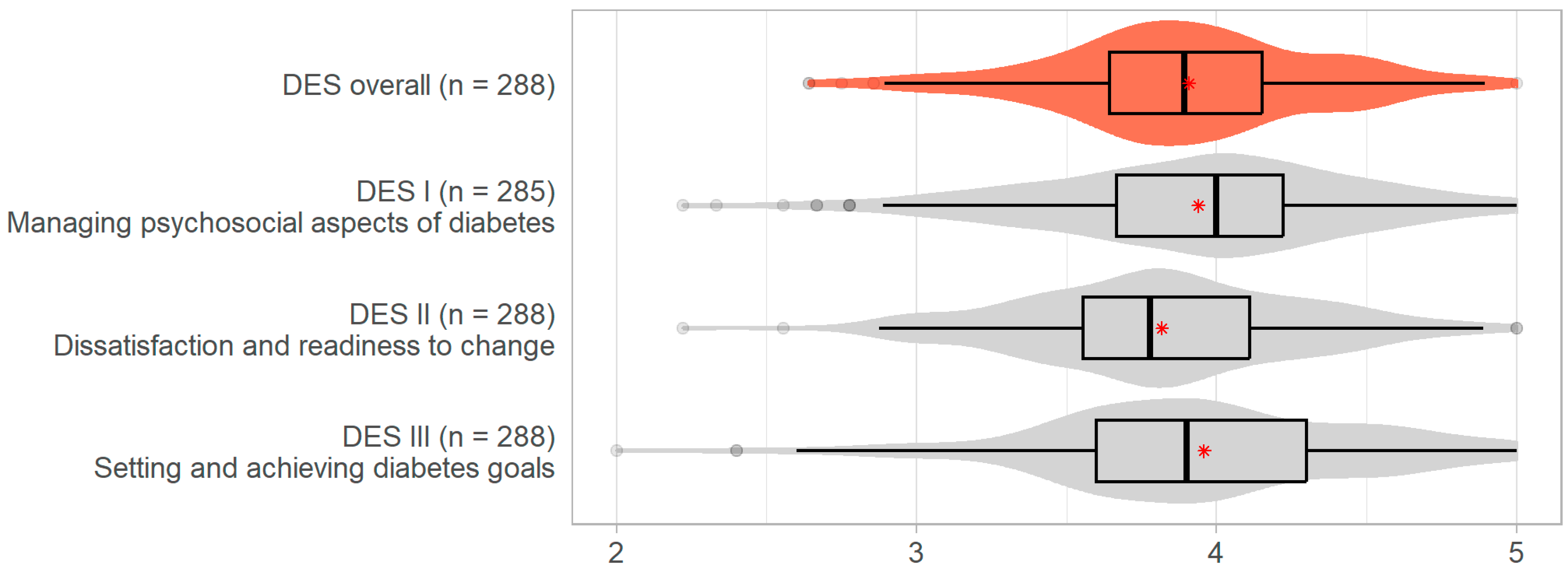
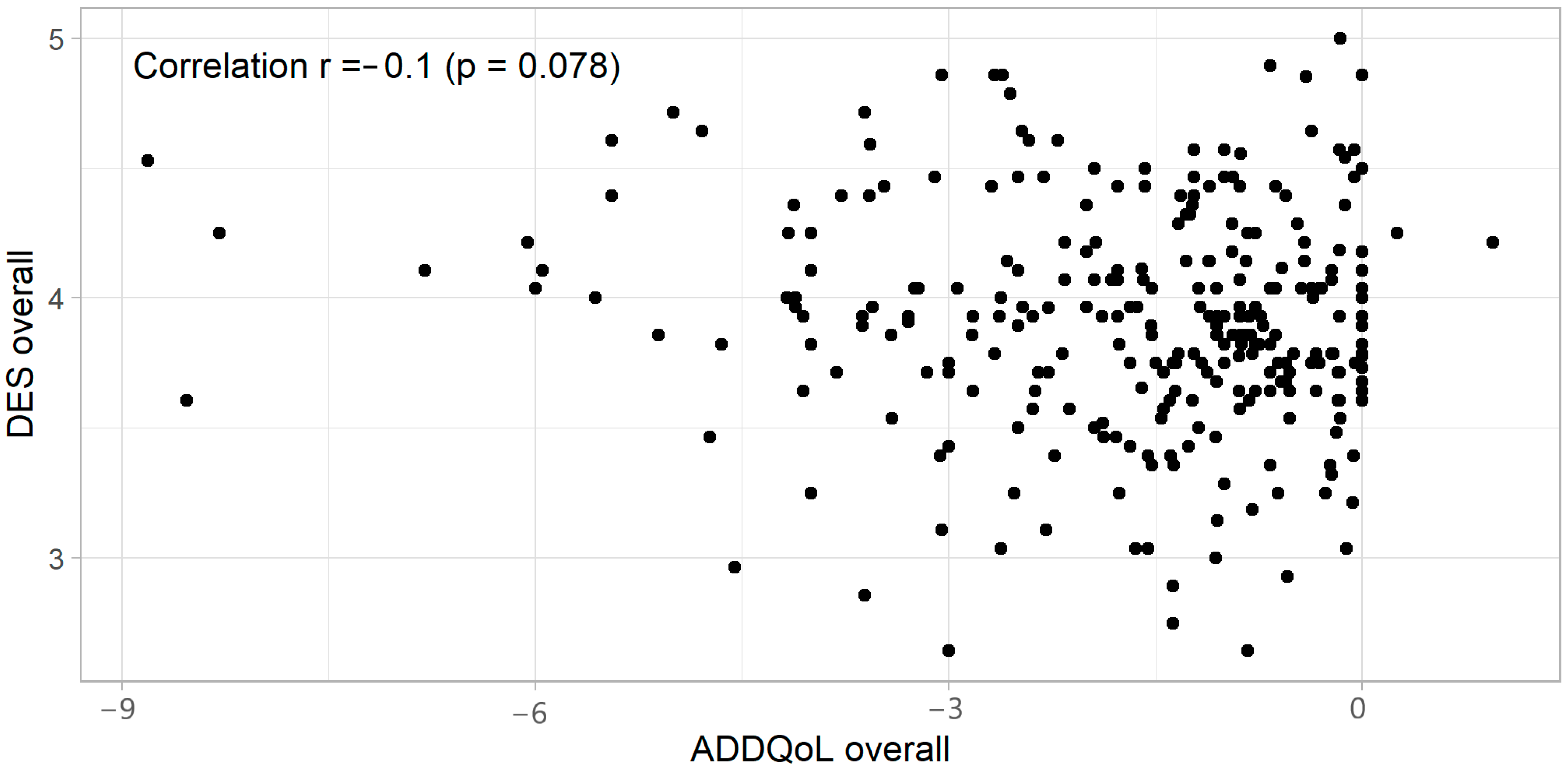
3.2. Assessment of Patient Empowerment
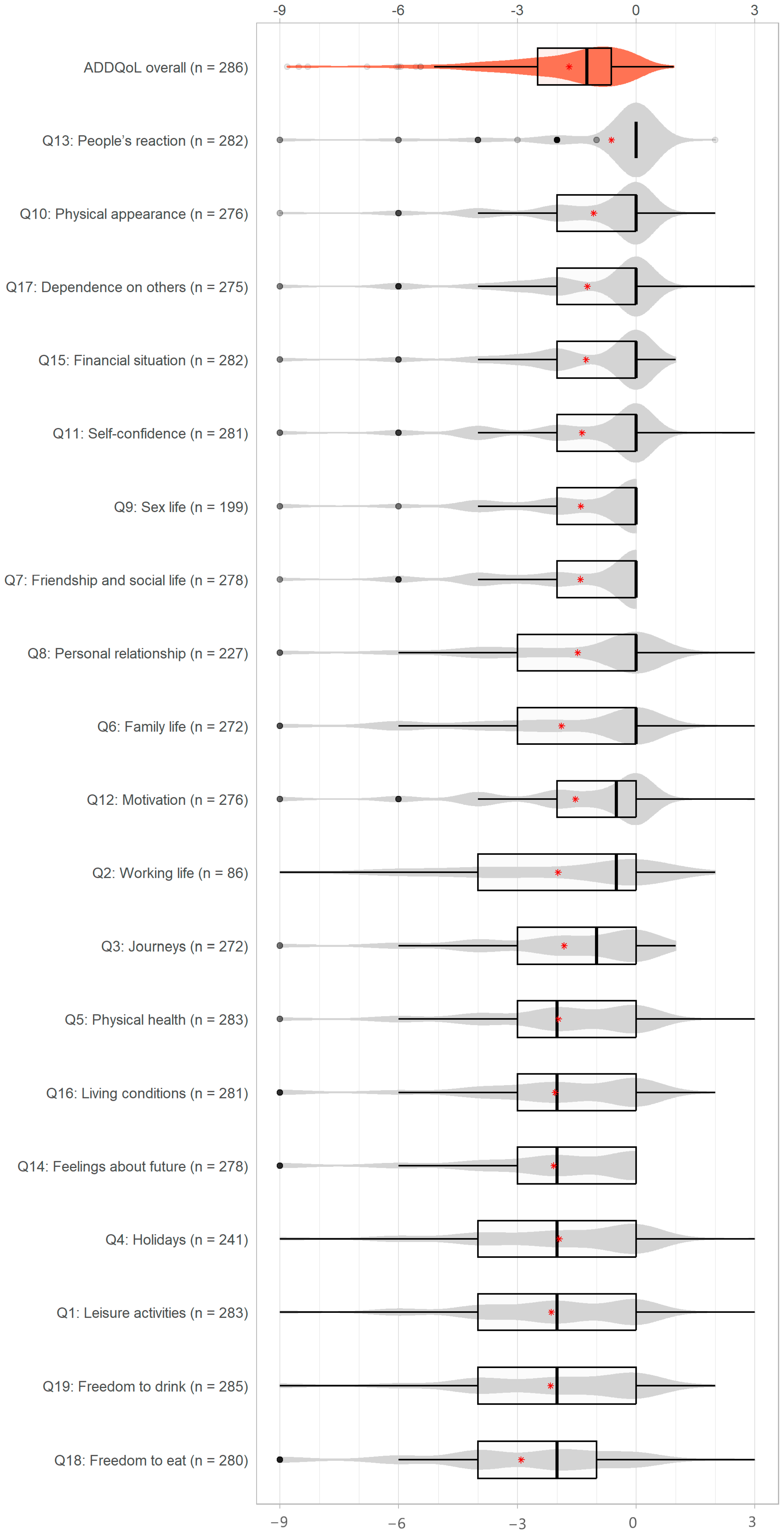
3.3. Assessment of Diabetes-Specific Health-Related Quality of Life
4. Discussion
4.1. Implication for Practice
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119. [Google Scholar] [CrossRef] [PubMed]
- Cannon, A.; Handelsman, Y.; Heile, M.; Shannon, M. Burden of Illness in Type 2 Diabetes Mellitus. J. Manag. Care Spec. Pharm. 2018, 24 (Suppl. 9-a), S5–S13. [Google Scholar] [CrossRef]
- Tang, T.S.; Funnell, M.M.; Brown, M.B.; Kurlander, J.E. Self-management support in “real-world” settings: An empowerment-based intervention. Patient Educ. Couns. 2010, 79, 178–184. [Google Scholar] [CrossRef]
- Simonsen, N.; Koponen, A.M.; Suominen, S. Empowerment among adult patients with type 2 diabetes: Age differentials in relation to person-centred primary care, community resources, social support and other life-contextual circumstances. BMC Public Health 2021, 21, 844. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H.; Austin, B.T.; Davis, C.; Hindmarsh, M.; Schaefer, J.; Bonomi, A. Improving chronic illness care: Translating evidence into action. Health Aff. 2001, 20, 64–78. [Google Scholar] [CrossRef] [PubMed]
- Wagner, E.H. The role of patient care teams in chronic disease management. BMJ 2000, 320, 569–572. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Care in Diabetes—2023 Abridged for Primary Care Providers. Clin. Diabetes 2023, 41, 4–31. [Google Scholar] [CrossRef]
- Funnell, M.M.; Anderson, R.M.; Arnold, M.S.; Barr, P.A.; Donnelly, M.; Johnson, P.D.; Taylor-Moon, D.; White, N.H. Empowerment: An Idea Whose Time Has Come in Diabetes Education. Diabetes Educ. 1991, 17, 37–41. [Google Scholar] [CrossRef]
- Agner, J.; Braun, K.L. Patient empowerment: A critique of individualism and systematic review of patient perspectives. Patient Educ. Couns. 2018, 101, 2054–2064. [Google Scholar] [CrossRef]
- Baldoni, N.R.; Aquino, J.A.; Sanches-Giraud, C.; Oliveira, C.D.L.; de Figueiredo, R.C.; Cardoso, C.S.; Santos, T.R.; Alves, G.C.S.; Fabbro, A.L.D.; Baldoni, A.O. Collective empowerment strategies for patients with Diabetes Mellitus: A systematic review and meta-analysis. Prim. Care Diabetes 2017, 11, 201–211. [Google Scholar] [CrossRef]
- Aquino, J.A.; Baldoni, N.R.; Flôr, C.R.; Sanches, C.; Oliveira, C.D.L.; Alves, G.C.S.; Fabbro, A.L.D.; Baldoni, A.O. Effectiveness of individual strategies for the empowerment of patients with diabetes mellitus: A systematic review with meta-analysis. Prim. Care Diabetes 2018, 12, 97–110. [Google Scholar] [CrossRef]
- Mogueo, A.; Oga-Omenka, C.; Hatem, M.; Kuate Defo, B. Effectiveness of interventions based on patient empowerment in the control of type 2 diabetes in sub-Saharan Africa: A review of randomized controlled trials. Endocrinol. Diabetes Metab. 2021, 4, e00174. [Google Scholar] [CrossRef] [PubMed]
- Kuo, C.; Su, Y.; Lin, C. A systematic review and meta-analysis: Effectiveness of internet empowerment-based self-management interventions on adults with metabolic diseases. J. Adv. Nurs. 2018, 74, 1787–1802. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, P.L.; Morais, C.; Pimenta, R.; Ribeiro, I.; Amorim, I.; Alves, S.M. Empowerment and Knowledge as Determinants for Quality of Life: A Contribution to a Better Type 2 Diabetes Self-Management. Int. J. Environ. Res. Public Health 2023, 20, 4544. [Google Scholar] [CrossRef] [PubMed]
- Arda Sürücü, H.; Büyükkaya Besen, D. Predictors of Empowerment in Individuals with Type 2 Diabetes Mellitus. J. Transcult. Nurs. 2018, 29, 506–513. [Google Scholar] [CrossRef] [PubMed]
- Zhu, T.H.; Mooi, C.S.; Shamsuddin, N.H. Diabetes empowerment scores among type 2 diabetes mellitus patients and its correlated factors: A cross-sectional study in a primary care setting in Malaysia. World J. Diabetes 2019, 10, 403–413. [Google Scholar] [CrossRef] [PubMed]
- D’Souza, M.S.; Karkada, S.N.; Hanrahan, N.P.; Venkatesaperumal, R.; Amirtharaj, A. Do Perceptions of Empowerment Affect Glycemic Control and Self-Care Among Adults with Type 2 Diabetes? Glob. J. Health Sci. 2015, 7, 80. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hendriks, M.; Rademakers, J. Relationships between patient activation, disease-specific knowledge and health outcomes among people with diabetes; a survey study. BMC Health Serv. Res. 2014, 14, 393. [Google Scholar] [CrossRef] [PubMed]
- Duarte-Díaz, A.; González-Pacheco, H.; Rivero-Santana, A.; Ramallo-Fariña, Y.; Perestelo-Pérez, L.; Peñate, W.; Carrion, C.; Serrano-Aguilar, P.; Team, I. Factors associated with patient empowerment in Spanish adults with type 2 diabetes: A cross-sectional analysis. Health Expect. 2022, 25, 2762–2774. [Google Scholar] [CrossRef]
- Clark, C.N.; Eby, E.L.; Lensing, C.J.; Fultz, E.; Hart, B.; Lingcaro, L.; Hoffner, R.; Schloot, N.C.; Benneyworth, B.D. Characterizing Diabetes Empowerment and Motivation for Changing Health Behaviors Among People with Type 2 Diabetes: A Cross-Sectional Survey. Diabetes Ther. 2023, 14, 869–882. [Google Scholar] [CrossRef]
- Rossi, M.C.; Lucisano, G.; Funnell, M.; Pintaudi, B.; Bulotta, A.; Gentile, S.; Scardapane, M.; Skovlund, S.E.; Vespasiani, G.; Nicolucci, A. Interplay among patient empowerment and clinical and person-centered outcomes in type 2 diabetes. The BENCH-D study. Patient Educ. Couns. 2015, 98, 1142–1149. [Google Scholar] [CrossRef] [PubMed]
- Fitzgerald, M.; O’Tuathaigh, C.; Moran, J. Investigation of the relationship between patient empowerment and glycaemic control in patients with type 2 diabetes: A cross-sectional analysis. BMJ Open 2015, 5, e008422. [Google Scholar] [CrossRef]
- Lin, Y.H.; Chen, D.A.; Lin, C.; Huang, H. Type D Personality Is Associated with Glycemic Control and Socio-Psychological Factors on Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study. Psychol. Res. Behav. Manag. 2020, 13, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Al-Dwaikat, T.N.; Rababah, J.A.; Al-Hammouri, M.M.; Chlebowy, D.O. Social Support, Self-Efficacy, and Psychological Wellbeing of Adults with Type 2 Diabetes. West. J. Nurs. Res. 2021, 43, 288–297. [Google Scholar] [CrossRef]
- Lin, K.; Park, C.; Li, M.; Wang, X.; Li, X.; Li, W.; Quinn, L. Effects of depression, diabetes distress, diabetes self-efficacy, and diabetes self-management on glycemic control among Chinese population with type 2 diabetes mellitus. Diabetes Res. Clin. Pract. 2017, 131, 179–186. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Shin, S.J.; Wang, R.H.; Lin, K.D.; Lee, Y.L.; Wang, Y.H. Pathways of empowerment perceptions, health literacy, self-efficacy, and self-care behaviors to glycemic control in patients with type 2 diabetes mellitus. Patient Educ. Couns. 2016, 99, 287–294. [Google Scholar] [CrossRef] [PubMed]
- Eržen, I.; Zaletel, J.; Nadrag, P. Sladkorna Bolezen-ključni Podatki za Leto 2021 [Internet]. Nacionalni Inštitut za Javno Zdravje, Trubarjeva 2, 1000 Ljubljana. Available online: https://nijz.si/ (accessed on 20 January 2024).
- Klemenc-Ketis, Z.; Stojnić, N.; Zavrnik, Č.; Gorenjec, N.R.; Danhieux, K.; Lukančič, M.M.; Susič, A.P. Implementation of Integrated Primary Care for Patients with Diabetes and Hypertension: A Case from Slovenia. Int. J. Integr. Care 2021, 21, 15. [Google Scholar] [CrossRef] [PubMed]
- Stojnić, N.; Klemenc-Ketiš, Z.; Mori Lukančič, M.; Zavrnik, Č.; Poplas Susič, A. Perceptions of the primary health care team about the implementation of integrated care of patients with type 2 diabetes and hypertension in Slovenia: Qualitative study. BMC Health Serv. Res. 2023, 23, 362. [Google Scholar] [CrossRef] [PubMed]
- Zavrnik, Č.; STOJNIĆ, N.; Lukančič, M.M.; Mihevc, M.; Potočnik, T.V.; Klemenc-Ketiš, Z.; Susič, A.P. Facilitators and Barriers to Scaling-Up Integrated Care for Arterial Hypertension and Type 2 Diabetes in Slovenia: Qualitative Study. Zdr. Varst. 2024, 63, 38–45. [Google Scholar] [CrossRef]
- Turk, E.; Prevolnik Rupel, V.; Tapajner, A.; Leyshon, S.; Isola, A. An Audit of Diabetes-Dependent Quality of Life (ADDQOL) in Older Patients with Diabetes Mellitus Type 2 in Slovenia. Value Health Reg. Issues 2013, 2, 248–253. [Google Scholar] [CrossRef][Green Version]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef] [PubMed]
- Statistical Office of the Republic of Slovenia. Gross Domestic Product by Region in Slovenia. 2022. Available online: https://www.stat.si/StatWeb/en/News/Index/11537 (accessed on 28 January 2024).
- Poplas Susic, A.; Svab, I.; Klemenc Ketis, Z. Upgrading the model of care in family medicine: A Slovenian example. Public Health Panor. 2018, 4, 550–555. [Google Scholar]
- Albreht, T.; Polin, K.; Brinovec, R.P.; Kuhar, M.; Poldrugovac, M.; Rehberger, P.O.; Rupel, V.P.; Vracko, P. Slovenia: Health System Review. Health Syst. Transit. 2021, 23, 1–183. [Google Scholar] [PubMed]
- Sebastian, M.J.; Khan, S.K.; Pappachan, J.M.; Jeeyavudeen, M.S. Diabetes and cognitive function: An evidence-based current perspective. World J. Diabetes 2023, 14, 92–109. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.M.; Funnell, M.M.; Fitzgerald, J.T.; Marrero, D.G. The Diabetes Empowerment Scale: A measure of psychosocial self-efficacy. Diabetes Care 2000, 23, 739–743. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Turk, E.; Rupel, V.P.; Tapajner, A.; Isola, A. Reliability and Validity of the Audit on Diabetes-Dependent Quality of Life (ADDQoL) and EQ-5D in Elderly Slovenian Diabetes Mellitus Type 2 Patients. Health 2014, 6, 699–711. [Google Scholar] [CrossRef][Green Version]
- Anthoine, E.; Moret, L.; Regnault, A.; Sébille, V.; Hardouin, J.B. Sample size used to validate a scale: A review of publications on newly-developed patient reported outcomes measures. Health Qual. Life Outcomes 2014, 12, 176. [Google Scholar] [CrossRef]
- Boateng, G.O.; Neilands, T.B.; Frongillo, E.A.; Melgar-Quiñonez, H.R.; Young, S.L. Best Practices for Developing and Validating Scales for Health, Social, and Behavioral Research: A Primer. Front. Public Health 2018, 6, 149. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2023; Available online: https://www.R-project.org/ (accessed on 10 January 2024).
- Tol, A.; Sharifirad, G.R.; Pourreza, A.G.; Rahimi, A.; Shojaeezadeh, D.; Mohajeritehrani, M.R.; Alhani, F. Development of a valid and reliable diabetes empowerment scale: An Iranian version. Iran. Red. Crescent Med. J. 2012, 14, 305–308. [Google Scholar]
- Khowaja, M.A.; Rozi, S.; Sawani, S.; Ahmed, A. Factors associated with Diabetes Empowerment among patients with type 2 diabetes, at OPD setting, Karachi, Pakistan. Sci. Rep. 2023, 13, 7165. [Google Scholar] [CrossRef] [PubMed]
- Sigurdardottir, A.K.; Jonsdottir, H. Empowerment in diabetes care: Towards measuring empowerment. Scand. J. Caring Sci. 2008, 22, 284–291. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Integrated, person-centred primary health care produces results: Case study from Slovenia. In Copenhagen: WHO Regional Office for Europe; WHO: Geneva, Switzerland, 2020. [Google Scholar]
- Prevolnik Rupel, V.; Divjak, M.; Turk, E. Changes in the level of knowledge of diabetes among elderly with diabetes in Slovenia in the period 2011–2020. Prim. Care Diabetes 2021, 15, 879–883. [Google Scholar] [CrossRef]
- Mihevc, M.; Zavrnik, Č.; Lukančič, M.M.; Virtič, T.; Rupel, V.P.; Šter, M.P.; Ketiš, Z.K.; Susič, A.P. Telemonitoring of elderly with hypertension and type 2 diabetes at the primary care level: Protocol for a multicentric randomized controlled pilot study. Zdr. Varst. 2022, 61, 216–223. [Google Scholar] [CrossRef]
- Virtič, T.; Mihevc, M.; Zavrnik, Č.; Mori Lukančič, M.; Poplas Susič, A.; Klemenc-Ketiš, Z. Peer Support as Part of Scaling-Up Integrated Care in Patients with Type 2 Diabetes and Arterial Hypertension at the Primary Healthcare Level: A Study Protocol. Zdr. Varst. 2023, 62, 93–100. [Google Scholar] [CrossRef]
- Ostini, R.; Dower, J.; Donald, M. The Audit of Diabetes-Dependent Quality of Life 19 (ADDQoL): Feasibility, reliability and validity in a population-based sample of Australian adults. Qual. Life Res. 2012, 21, 1471–1477. [Google Scholar] [CrossRef]
- Arditi, C.; Zanchi, A.; Peytremann-Bridevaux, I. Health status and quality of life in patients with diabetes in Switzerland. Prim. Care Diabetes 2019, 13, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Abbatecola, A.M.; Spazzafumo, L.; Fabbietti, P.; Testa, R.; Rabini, R.A.; Bonfigli, A.R.; Corsonello, A.; Lattanzio, F.; Paolisso, G. Diabetes-related quality of life is enhanced by glycaemic improvement in older people. Diabet. Med. 2015, 32, 243–249. [Google Scholar] [CrossRef]
- Mihevc, M.; Virtič Potočnik, T.; Zavrnik, Č.; Šter, M.P.; Klemenc-Ketiš, Z.; Poplas Susič, A. Beyond diagnosis: Investigating factors influencing health-related quality of life in older people with type 2 diabetes in Slovenia. Prim. Care Diabetes 2024, 18, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Volčanšek, Š.; Lunder, M.; Janež, A. Health-Related Quality of Life Assessment in Older Patients with Type 1 and Type 2 Diabetes. Healthcare 2023, 11, 2154. [Google Scholar] [CrossRef]
- Gómez-Velasco, D.V.; Almeda-Valdes, P.; Martagón, A.J.; Galán-Ramírez, G.A.; Aguilar-Salinas, C.A. Empowerment of patients with type 2 diabetes: Current perspectives. Diabetes Metab. Syndr. Obes. 2019, 12, 1311–1321. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | n (%)/Mean (SD) | [Range] |
|---|---|---|
| Age (years), n = 287 | 67.2 (9.2) | [30, 91] |
| Gender, n = 288 | ||
| Male | 131 (45.5) | |
| Female | 157 (54.5) | |
| Region of residence, n = 287 | ||
| Urban setting | 80 (27.9) | |
| Rural setting | 207 (72.1) | |
| Education, n = 280 | ||
| Primary school | 40 (14.3) | |
| Secondary/vocational school | 168 (60.0) | |
| Higher vocational college | 55 (19.6) | |
| University education | 12 (4.3) | |
| Master’s/doctoral degree | 5 (1.8) | |
| Marital status, n = 284 | ||
| Married | 193 (68.0) | |
| Single | 18 (6.3) | |
| Divorced | 15 (5.3) | |
| Widowed | 58 (20.4) | |
| Employment status, n = 288 | ||
| Employed | 52 (18.1) | |
| Unemployed | 8 (2.8) | |
| Retired | 228 (79.2) | |
| Comorbidity of T2D and AH, n = 287 | 147 (51.2) | |
| Time since diagnosis of T2D (years), n = 278, median [IQR] | 8.0 [4.0–15.0] | [1, 34] |
| Treatment method for T2D | ||
| Antihyperglycemics, n = 288 | 190 (66.0) | |
| Insulin treatment, n = 286 | 72 (25.2) | |
| Height (cm), n = 282 | 169.7 (9.4) | [141, 193] |
| Weight (kg), n = 282 | 83.4 (15.5) | [52, 135] |
| BMI (kg/m2), n = 282 | 28.9 (4.5) | [20.8, 45.1] |
| Underweight (BMI < 18.5) | 0 (0) | |
| Normal weight (18.5 < BMI < 24.9) | 51 (18.1) | |
| Overweight (25 < BMI < 29.9) | 142 (50.4) | |
| Obese (BMI > 30) | 89 (31.6) | |
| HbA1c (%), n = 224 | 7.3 (1.1) | [5.4, 13] |
| Variable | n Complete | n Considered | Mean (SD) | Median [IQR] | Range |
|---|---|---|---|---|---|
| DES | 268 | 288 | 3.9 (0.4) | 3.9 [3.6, 4.2] | [2.6, 5] |
| DES I | 280 | 285 | 3.9 (0.5) | 4.0 [3.7, 4.2] | [2.2, 5] |
| DES II | 275 | 288 | 3.8 (0.5) | 3.8 [3.6, 4.1] | [2.2, 5] |
| DES III | 282 | 288 | 4.0 (0.5) | 3.9 [3.6, 4.3] | [2, 5] |
| ADDQoL | 241 | 286 | −1.7 (1.6) | −1.2 [−2.5, −0.6] | [−8.8, 0.9] |
| GQoL | 286 | 286 | 1.2 (0.9) | 1 [1, 2] | [−3, 3] |
| DDQoL | 286 | 286 | −1.2 (0.9) | −1 [−2, −1] | [−3, 1] |
| Variable | Regression Coefficient (95% CI) | p |
|---|---|---|
| Female gender | 0.06 [−0.06, 0.19] | 0.321 |
| Age (years) | 0.00 [−0.01, 0.01] | 0.986 |
| Rural setting | 0.15 [0.01, 0.29] | 0.034 |
| Higher education | 0.16 [0.02, 0.30] | 0.028 |
| Marital status | 0.182 | |
| Single vs. married | 0.03 [−0.22, 0.27] | 0.825 |
| Divorced vs. married | −0.32 [−0.60, −0.03] | 0.031 |
| Widowed vs. married | −0.04 [−0.21, 0.13] | 0.622 |
| Employment status | 0.432 | |
| Unemployed vs. employed | −0.27 [−0.68, 0.14] | 0.198 |
| Retired vs. employed | −0.05 [−0.26, 0.16] | 0.621 |
| Time since diagnosis of T2D (years) | 0.01 [−0.00, 0.02] | 0.099 |
| Treatment with antihyperglycemics | −0.10 [−0.23, 0.03] | 0.140 |
| Treatment with insulin | −0.05 [−0.22, 0.12] | 0.535 |
| Comorbidity of T2D and AH | −0.16 [−0.29, −0.03] | 0.016 |
| HbA1c (%) | 0.00 [−0.06, 0.06] | 0.992 |
| BMI | 0.607 | |
| Overweight vs. normal | −0.09 [−0.27, 0.09] | 0.319 |
| Obese vs. normal | −0.06 [−0.25, 0.12] | 0.502 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Virtič Potočnik, T.; Ružić Gorenjec, N.; Mihevc, M.; Zavrnik, Č.; Mori Lukančič, M.; Poplas Susič, A.; Klemenc-Ketiš, Z. Person-Centred Diabetes Care: Examining Patient Empowerment and Diabetes-Specific Quality of Life in Slovenian Adults with Type 2 Diabetes. Healthcare 2024, 12, 899. https://doi.org/10.3390/healthcare12090899
Virtič Potočnik T, Ružić Gorenjec N, Mihevc M, Zavrnik Č, Mori Lukančič M, Poplas Susič A, Klemenc-Ketiš Z. Person-Centred Diabetes Care: Examining Patient Empowerment and Diabetes-Specific Quality of Life in Slovenian Adults with Type 2 Diabetes. Healthcare. 2024; 12(9):899. https://doi.org/10.3390/healthcare12090899
Chicago/Turabian StyleVirtič Potočnik, Tina, Nina Ružić Gorenjec, Matic Mihevc, Črt Zavrnik, Majda Mori Lukančič, Antonija Poplas Susič, and Zalika Klemenc-Ketiš. 2024. "Person-Centred Diabetes Care: Examining Patient Empowerment and Diabetes-Specific Quality of Life in Slovenian Adults with Type 2 Diabetes" Healthcare 12, no. 9: 899. https://doi.org/10.3390/healthcare12090899
APA StyleVirtič Potočnik, T., Ružić Gorenjec, N., Mihevc, M., Zavrnik, Č., Mori Lukančič, M., Poplas Susič, A., & Klemenc-Ketiš, Z. (2024). Person-Centred Diabetes Care: Examining Patient Empowerment and Diabetes-Specific Quality of Life in Slovenian Adults with Type 2 Diabetes. Healthcare, 12(9), 899. https://doi.org/10.3390/healthcare12090899







