Abstract
The increase in older adults with dementia presents challenges in promoting research to improve the quality of life of this population. The objective of this study was to assess the scientific evidence on the effectiveness of occupational therapy interventions in improving the quality of life of older adults over 65 years old with dementia living in nursing homes. The databases used were PubMed, Web of Science, OTSeeker, clinicaltrials.gov, Dialnet, Scopus, Cochrane, and SciELO between 2013 and 2023. The studies were selected and evaluated according to the Cochrane guidelines. The review was carried out following the PRISMA 2020 Statement. Sixteen articles met the inclusion criteria and were categorized into four groups according to the focus of the intervention: “meaningful activities/occupations”, “physical, cognitive and sensory functioning”, “performance areas”, and “physical and social environment and staff training”. The strength of evidence was moderate, and the risk of bias was low. The findings revealed that occupational therapy interventions based on participation in recreational activities, reminiscence, performance-based activities and the physical and social environment, and specialized staff training, could improve the perceived quality of life of older adults with dementia living in nursing homes.
1. Introduction
Dementia is a major neurocognitive disorder characterized by significant cognitive decline compared to the previous level of performance in one or more cognitive domains (complex attention, executive function, learning and memory, language, perceptual motor function, or social cognition) which interferes with the individual’s autonomy in daily activities [1].
Currently, more than 55 million older adults over 65 years old (8.1% of women and 5.4% of men) have dementia worldwide. This is expected to rise to 78 million by 2030 and 139 million by 2050 [2]. In addition, the prevalence of dementia among older adults living in nursing homes is highly variable, ranging from 16.1% to 85.2%, depending on factors such as the country, the method and timing used to conduct the research, and the degree of aging [3]. Therefore, addressing dementia has become a public health priority and a major socio-health problem, as its scope, size, and socio-economic impact present society with the challenge of promoting study and research to improve the well-being and quality of life (QoL) of this population group [4].
QoL is a multidimensional concept that has evolved throughout history and currently has multiple interpretations. Thus, it is difficult to find a single definition [5].
An integrative definition of the concept of QoL has been proposed by Fernández-Ballesteros [6], in which she proposes two classifications: the first one separates the socio-environmental factors (social support, financial conditions, health and social services, environmental quality, and cultural factors) and the personal factors (social relations, life satisfaction, participation in meaningful activities, health, and functional skills); and the second distinguishes between objective elements (physical environment, availability of social health services, objective health, social networks, and cultural factors) and subjective elements (health, social satisfaction, cultural needs, context evaluation, and functional skills). Taking all these factors into account, the concept of QoL assesses different dimensions of the person’s life, through a comprehensive and complex approach.
Interventions from an occupational therapy (OT) perspective could be offered to older adults with dementia living in nursing homes, where they are provided with temporary or permanent accommodation and appropriate programs to improve their QoL and personal autonomy [7]. These interventions focus on and consider variables such as mental state, physical functioning, characteristics of the residential environment, health promotion, activities of daily living (ADLs), instrumental activities of daily living (IADLs), health management, education, leisure, and social participation [8]. From this perspective, OT interventions represent a vehicle for the promotion and maintenance of autonomy, health, and QoL of older adults with dementia [9].
However, previous literature reviews could not identify the existence of current systematic reviews summarizing the scientific evidence on the effectiveness of OT interventions in this particular population and setting. In the most recent systematic reviews on this topic, the population consisted of either healthy older adults [10] or patients with dementia but not as the primary diagnosis [11,12], or the study setting was not a nursing home [13,14].
Therefore, this study aims to systematically identify, evaluate, and summarize the scientific evidence on OT interventions to improve the QoL of older adults aged 65 and over with dementia living in nursing homes. The research question that guided the review was: What is the quality of the scientific evidence on the effectiveness of OT interventions to improve the QoL of older adults over 65 years old with dementia living in nursing homes?
2. Method
This systematic review was conducted following the Cochrane Collaboration methodology [15] and was reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (PRISMA 2020) [16].
2.1. Search and Screening Strategy
The initial search process was carried out by the authors of this work in collaboration with a medical librarian experienced in conducting systematic reviews.
A formal literature search was conducted (10 July 2023 and 20 July 2023) in the following selected databases: PubMed, Web of Science (WOS), OTSeeker, clinicaltrials.gov, Dialnet, Scopus, Cochrane, and SciELO, using MeSH terms and keywords: “dementia”, “occupational therapy”, “quality of life”, “aged”, and “nursing home”. Studies conducted from 2013 to 2023 in any language and country were included. The latest information has therefore been compiled as comprehensively as possible. We aimed to avoid any bias that might affect the information collected.
The search string used in the databases was:
- −
- PubMed: (((dementia) AND (quality of life)) AND (aged)) AND (occupational therapy) AND (nursing home) → 60 results obtained.
- −
- WOS: ((((ALL=(dementia)) AND ALL=(quality of life)) AND ALL=(aged))) AND ALL=(occupational therapy) → 264 results obtained.
- −
- OTSeeker: [Any Field] like ‘dementia’ AND [Any Field] like ‘quality of life’ AND [Any Field] like ‘occupational therapy’ → 86 results obtained.
- −
- clinicaltrials.gov: (dementia AND occupational therapy) → 51 results obtained.
- −
- Dialnet: (occupational therapy, quality of life, dementia) → 67 results obtained.
- −
- Scopus: (dementia AND quality AND of AND life AND occupational AND therapy AND nursing AND home) → 194 results obtained.
- −
- Cochrane: (dementia AND quality of life AND occupational therapy AND nursing home) → 223 results obtained.
- −
- SciELO: (dementia AND quality of life AND occupational therapy) → 22 results obtained.
2.2. Inclusion and Exclusion Criteria
The following eligibility criteria were established.
- →
- Inclusion criteria:
- −
- Studies involving OT interventions in nursing homes.
- −
- Studies in older adults over 65 years old of both genders with a formal diagnosis of dementia of any type and stage [1].
- −
- Studies with a level of evidence 1a–1b to 2a–2b.
- −
- Studies that include the MeSH terms in the keyword list.
- →
- Exclusion criteria:
- −
- Studies with a primary focus on intervention other than OT and nursing homes. Older adults living at home or with their family, in the community, in hospitals, and in palliative care facilities.
- −
- Studies that include healthy older adults or older adults with dementia but not as the primary diagnosis.
- −
- Studies that do not contain any of the keywords.
Level 1a (systematic reviews of homogeneous randomized controlled trials [RCTs] with or without meta-analysis), level 1b (properly designed individual RCTs), level 2a (systematic review of cohort studies), and level 2b (individual prospective cohort studies, low-quality RCTs, ecological studies, two-group non-randomized studies) studies were included. Level 3a (systematic review of case-control studies), level 3b (individual retrospective case-control studies, non-randomized one-group pretest-post-test studies, and cohort studies), level 4 (case-series and poor-quality cohort and case-control studies), and level 5 (expert opinion without explicit critical appraisal: protocols, dissertations and theses, and editorials) studies were excluded [17].
2.3. Data Extraction and Analysis
Relevant information was collected from each included study and entered into a data collection form based on Cochrane recommendations [15], using Microsoft Excel®, version 16.16.21 software. Data collection was carried out independently by the researchers C.U. and S.A. Subsequently, the results of each investigator were compared until a consensus was reached. In addition, the entire data collection process was independently supervised by a third researcher (P.M.). Information on the following variables was collected: author/year, level of evidence, study design, risk of bias, participants, inclusion criteria, study setting, intervention and control group, outcome measures, and results. Finally, with the purpose of improving the comprehension, readability, and organization of the information presented on the OT intervention programs analyzed, the researchers C.U. and S.A. consensually grouped the studies according to the main objective or focus of intervention. In addition, a third researcher (P.M.) independently supervised the entire categorization process. Finally, the studies were categorized into four groups: (a) “meaningful activities/occupations”, (b) “physical, cognitive and sensory functioning”, (c) “performance areas”, and (d) “physical and social environment and staff training” (see Table 1, Table 2, Table 3 and Table 4).

Table 1.
Characteristics of studies based on “Meaningful activities/occupations” intervention programs.

Table 2.
Characteristics of studies based on “Physical, cognitive and sensory functioning” intervention programs.

Table 3.
Characteristics of studies based on “Performance areas” intervention programs.

Table 4.
Characteristics of studies based on “Physical and social environment and staff training” intervention programs.
2.4. Risk of Bias
The risk of bias (low, moderate, or high) in each study included in the systematic review was assessed according to the Cochrane risk of bias assessment guidelines [33]. The guidelines for carrying out a Cochrane risk of bias assessment cover five domains of bias: selection bias, performance bias, detection bias, attrition bias, and information bias. Within each domain, the assessment is performed for one or more items, which may cover different aspects of the domain. To determine the overall risk of bias, a risk of bias category must first be assigned for each item. The categories for risk of bias are as follows: low risk of bias (+), unclear risk of bias (?), and high risk of bias (−). The total number of minuses (−) is then summed. Finally, the overall risk of bias in each study is classified as low (L) (0–3 minuses), moderate (M) (4–6 minuses), or high (H) (7–9 minuses). The risk of bias in the systematic reviews included was assessed using the AMSTAR 2 guidelines [34]. The AMSTAR 2 guidelines consist of 12 assessment items, each of which relates to specific aspects of the method used to conduct the systematic review. To determine the overall risk of bias, each item must first be assessed by determining whether the systematic review meets that criterion by assigning a yes (+), no (−), not sure (?), or not applicable (NA). The total number of minuses (−) is then summed. Finally, the overall risk of bias in each study is classified as low (L) (0–3 minuses), moderate (M) (4–6 minuses), or high (H) (7–9 minuses). Two researchers (C.U. and S.A.) independently assessed the risk of bias. The results were then compared collaboratively to reach a consensus. Next, the results were independently reviewed by a third researcher (P.M.). Table 5 and Table 6 show the risk of bias assessment of the included studies.

Table 5.
Risk-of-Bias Table for Systematic Reviews (AMSTAR 2).

Table 6.
Risk-of-Bias Table for Randomized Controlled Trial (RCT) and Non-RCT.
2.5. Overall Strength of Evidence
The strength of the evidence was assessed based on the guidelines developed by the U.S. Preventive Services Task Force [35]. In short, for each topic, the levels of strength of evidence are high strength of evidence, which consists of two or more well-designed RCTs whose conclusions are unlikely to be affected by the results of future studies; moderate strength of evidence, which consists of at least one high-quality RCT or multiple moderate quality studies; and the low strength of evidence, which involves a limited number of incomplete and low-quality studies.
3. Results
The literature search identified 967 studies, of which 48 were subjected to a full-text review. Sixteen studies met the eligibility criteria and were included in the analysis (see Figure 1).
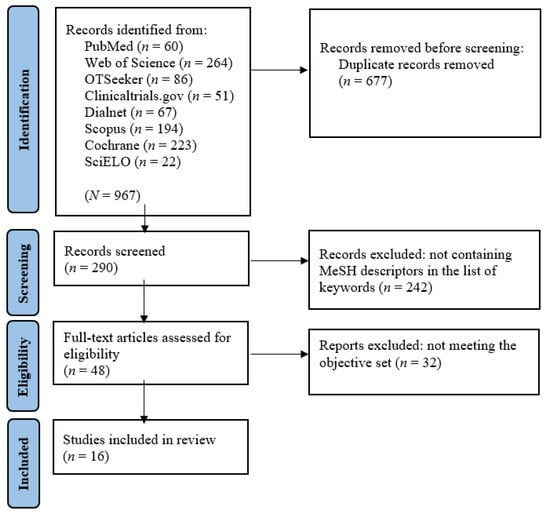
Figure 1.
PRISMA flow diagram. Note. Figure format adapted from Moher et al. [36].
Sixteen studies involved OT interventions to improve the QoL of older adults with dementia living in nursing homes. Three level 1a studies were identified [9,18,30]. Twelve level 1b studies were identified [19,20,21,22,24,25,26,27,28,29,31,32]. A single level 2b study was identified [23]. Fifteen studies showed a low risk of bias, and one study met the criteria for a moderate risk of bias (see Table 1, Table 2, Table 3, Table 4, Table 5 and Table 6).
The sixteen studies were categorized into four groups according to the primary objective or focus of intervention: (a) “meaningful activities/occupations”, (b) “physical, cognitive and sensory functioning”, (c) “performance areas”, and (d) “physical and social environment and staff training”. For group (a) “meaningful activities/occupations”, four studies (25.0%) were identified [18,19,20,21]. For group (b) “physical, cognitive and sensory functioning”, six studies (37.5%) were identified, which were divided into two subgroups: (b1) physical activity [22,23], and (b2) cognitive and sensory functioning [24,25,26,27]. Regarding group (c) “performance areas”, three studies (18.7%) were included [28,29,30]. Regarding group (d) “physical and social environment and staff training”, three studies (18.7%) were identified [9,31,32]. The characteristics of each study and their outcome measures are described in Table 1, Table 2, Table 3 and Table 4.
- (a)
- Meaningful activities/occupations
Meaningful activities/occupations were the primary intervention in four of the included studies [18,19,20,21].
Mansbach et al. [19] (level 1b evidence) conducted an intervention program called “MemPics”, designed to promote meaningful activities and improve QoL for older adults with dementia by engaging them in verbal activities (e.g., fun and stimulating conversations, prompting questions for further conversation) and cognitive stimulation (e.g., reminiscence therapy). The results showed increased engagement in meaningful activities (Engagement in Meaningful Activities Survey [EMAS]) and improved the QoL of the intervention group (assessed with the MemPics Facility Staff Survey).
Livingston et al. [20] (level 1b evidence) developed an intervention program called “MARQUE”, designed to promote agitation management and improve QoL in older adults with dementia through their participation in six sessions (psycho-education on dementia, staff experiences in agitation management, stress reduction techniques, communication, a “Call to Mind” board game to discover participants’ interests, and incorporation of meaningful activities into the daily care of older adults). After the 8-month follow-up, no significant differences were observed between the groups for the level of agitation and QoL (assessed with the Dementia Quality of Life [DEMQOL] and the EuroQol-5D-5L [EQ-5D-5L]).
Sultan Ibrahim et al. [21] (level 1b evidence) conducted a program called “Occupation-based intervention”, consisting of cognitive activities (e.g., image recognition and categorization, memory, sensory recognition) as well as meaningful occupational activities (e.g., personal hygiene, cooking, money management, shopping, leisure, and recreational activities). The results showed a significant improvement in cognitive function (evaluated with the Lowenstein Occupational Therapy Cognitive Assessment-Geriatric [LOTCA-G]), social relations (measured with the Friendship Scale [FS]), and QoL (assessed with the Brief Version of World Health Organization-Quality of Life [WHOQOL-BREF]) of the participants.
The results of the above studies are consistent with those of the systematic review with meta-analysis conducted by Travers et al. [18] (level 1a evidence) to determine the effectiveness of the use of meaningful activities (individualized recreational activities, reminiscence therapy, music therapy, multi-sensory stimulation, staff training to provide individual care, animal-assisted therapy, and social interaction) in addressing behavioral and psychological symptoms (agitation, aggression, depression, wandering, and apathy), and improving the QoL of older adults with dementia. The results revealed beneficial effects as a result of the promotion of individualized recreational activities, reminiscence therapy, and music therapy on the reduction of agitation, depression, and anxiety, as well as an improvement in cognitive functioning and QoL of the residents.
- (b)
- Physical, cognitive, and sensory functioning
This section presents the studies grouped into sub-themes, according to the main findings of each study.
- (b1)
- Physical activity
Physical activity was the primary intervention in two studies [22,23].
Galik et al. [22] (level 1b evidence) conducted a function-focused care intervention program for older adults with dementia (FFC-CI). The intervention included four components: (I) assessment of the physical environment of the nursing home in order to identify architectural barriers when implementing the intervention; (II) training program on FFC-CI for the nursing home staff; (III) development of function-focused care goals (active participation of residents in self-care, household, mobility, physical activity, and dance); and (IV) continuous training and motivation of staff to involve residents in activities that promote their activity and functioning. The results showed significant improvements in the amount and intensity of physical activity (measured with ActiGraph) and physical function (assessed with the Tinetti Scale and Barthel Index [BI]) of older adults, as well as a decrease in the number of falls in the intervention group, resulting in an improvement in their QoL.
Chu et al. [23] (level 2b evidence) carried out a quasi-experimental study consisting of the implementation of a program called “Multifaceted Walking Intervention”, which included low-intensity physical activity (walking session) and an individualized care plan (communication, social interaction, behavior, personality, values, and preferences of the resident). After a four-month intervention, the results showed significant improvements in the functional mobility (Timed Up and Go Test [TUG] and 2-Minute Walk Test [2MWT]), ADLs (Functional Independence Measure [FIM]), and QoL (Alzheimer’s Disease-Related Quality of Life [ADRQOL] Scale) of the participants.
- (b2)
- Cognitive and sensory activities
The primary intervention focused on cognitive and sensory functioning in four studies [24,25,26,27].
Maseda et al. [24] (level 1b evidence) assessed the effect of multisensory stimulation on the behavior, mood, and cognitive and functional levels of residents with dementia. To this end, a “Snoezelen” room with different elements for the stimulation of the senses (e.g., fiber optic cables, water columns, a vibrating waterbed, screen projectors, different music and sounds, aromatherapy, and different textures) and individualized activities (e.g., playing cards, taking questionnaires, and looking at photographs) were used. The results showed significant improvements in the behavior (measured with the Cohen-Mansfield Agitation Inventory [CMAI]), cognitive level (evaluated with the Mini-Mental State Examination [MMSE]), and ADLs (assessed with the BI) of the intervention group.
Raglio et al. [25] (level 1b evidence) conducted a study to explore the effects of an intervention based on music therapy and individualized listening to music on QoL, behavior, and mood in older adults with dementia. Participants were randomly assigned to one of the following three interventions: (I) standard care, which consists of physical (e.g., motor rehabilitation), educational, and occupational activities (e.g., self-care, reading the newspaper, playing cards), with no musical exposure; (II) music therapy and standard care, based on the use of instruments, singing, rhythm, and music production; and (III) individualized listening to music and standard care, focused on listening to personalized music on a one-to-one basis. The findings revealed significant improvements in QoL (measured with the Cornell-Brown Scale for Quality of Life in Dementia [CBS-QoL]), behavior (assessed with the Neuropsychiatric Inventory [NPI]), and mood (measured with the Cornell Scale for Depression in Dementia [CSDD]) for all groups, regardless of the intervention received.
Lök et al. [26] (level 1b evidence) explored the effect of reminiscence therapy on the QoL, cognitive function, and mood of participants. The sessions included recalling memories of childhood experiences, festivals, memorable places visited, favorite foods and music, major historical events, and achievements, using different materials such as photographs, household items, objects from the past, old music, and food. The results indicated a significant improvement in the cognitive function (measured with the MMSE), depressive symptoms (evaluated with the CSDD), and QoL (assessed with the QOL-AD) of older adults with dementia.
Kim [27] (level 1b evidence) explored the effectiveness of a reminiscence-based program on cognitive function, mood, and QoL of residents with dementia. The sessions included physical, musical, artistic, and horticultural activities, and IADLs. Each activity was divided by content according to childhood, adulthood, and late adulthood memories. The results showed a significant improvement in the cognitive function (measured with the Korean-Mini-Mental State Examination [K-MMSE]), depression (assessed with the Short-Form Geriatric Depression Scale-K [SGDS-K]), and QoL (measured with the QOL-AD Scale) of participants.
- (c)
- Performance areas
In three studies, performance-based activities were the primary intervention [28,29,30].
Kumar et al. [28] (level 1b evidence) explored the effects of an OT program to improve the QoL of older adults with dementia, through their participation in ADLs (care of hair, skin, nails and teeth, general cleanliness, dressing), IADLs (bed making, money counting), physical activity (exercises aimed at maintaining strength, mobility, and circulation), cognitive activities (reading aloud, dual-task activity, solving puzzles), recreational activities (watching TV, board games, quizzes, storytelling, singing), relaxation exercises, and pharmacological treatment. The results showed an improvement in the QoL (measured with the WHOQOL-BREF) of the participants.
Murai and Yamaguchi [29] (level 1b evidence) assessed the effects of a cooking program based on the principles of brain-activating rehabilitation on the QoL, executive function, behavior, mood, and ADLs of the participants. The program consisted of cooking 12 homemade Japanese-style dishes (e.g., miso soup with tofu and seaweed, udon noodles), in which different activities, such as knife cutting, boiling, grilling, and seasoning, were carried out. The results showed significant improvements in the executive function (measured with the Yamaguchi Kanji-Symbol Substitution Test [YKSST]) and behavior (assessed with the Dementia Behavior Disturbance [DBD] Scale) of the participants.
The results of the above studies are consistent with those of the systematic review with a meta-analysis conducted by Möhler et al. [30] (level 1a evidence) to assess the effects of personally tailored activities (IADLs, such as household chores and meal preparation; artistic activities, such as painting and singing; work-related activities, such as gardening; and recreational activities, such as games) on the improvement of the psycho-social outcomes and QoL of older adults with dementia. This study concluded that offering personally tailored activities to people with dementia in long-term care could slightly improve challenging behavior.
- (d)
- Physical and social environment and staff training
Activities based on the physical environment, social environment, and staff training were the primary interventions in three studies [9,31,32].
Wenborn et al. [31] (level 1b evidence) developed an OT program that included an assessment of the physical environment of the nursing home, with recommendations on how to adapt and improve it to enable residents to be active. In addition, a training program for nursing home staff, consisting of group discussions, didactic teaching, and practical exercises was designed. This training program aimed, on the one hand, to improve the knowledge, attitudes, and skills of the staff to provide personally meaningful activities, and, on the other hand, to identify the interests and abilities of the residents to carry them out, in order to redesign and subsequently conduct new meaningful activities (self-care, domestic activities, music therapy, sensory stimulation, and physical exercise activities) adapted to each participant. At the quarterly follow-up, staff-rated QoL (measured with the Quality of Life in Alzheimer’s Disease—Patient and Caregiver Report [QOL-AD] Scale) was slightly lower in the intervention group.
Froggatt et al. [32] (level 1b evidence) conducted an intervention program called “Namaste Care”, focused on improving the physical environment, comfort, and sensory engagement of residents with dementia, in which personalized and structured care (creative activities, multisensory stimulation, social participation, and a training program for nursing home staff) was provided in a specific space (cozy and homely, with natural light, relaxing music, and aromatherapy). After a six-month intervention, the results revealed a significant improvement in the comfort (assessed with the Comfort Assessment in Dying-End of Life Care in Dementia [CAD-EOLD] Scale) of the participants.
The results of the above studies are consistent with those of the systematic review with meta-analysis conducted by Ojagbemi and Owolabi [9] (level 1a evidence), which aimed to explore the effects of OT interventions (compensatory and environmental modification activities; training for nursing home staff; relaxation exercises; sensorimotor activities, e.g., video viewing; recreational activities, e.g., playing musical instruments; cognitive activities, e.g., word games; and IADLs, e.g., caring for farm animals) on the QoL of older adults with dementia. This study concluded that OT interventions resulted in small improvements in the overall QoL of this population.
4. Discussion
This systematic review aimed to assess the scientific evidence on the effectiveness of OT interventions on improving the QoL of older adults over 65 years old with dementia living in nursing homes.
First, the intervention programs focused on meaningful activities and occupations and structured according to individual changes in activities based on the preferences and wishes of each participant, the type and stage of dementia, and the functional ability of the older adult with dementia to perform them [18,19,20], or specific programs of activities and occupations [21], show therapeutic effects on the behavioral and psychological symptoms of dementia, which in turn positively influence the perception of the QoL.
Individualized recreational activities/occupations such as music or painting show a high strength of evidence for the improvement of agitation, depression, anxiety, and mood. Also, reminiscence activities have positive effects on the cognitive functioning and QoL of residents [18].
Verbal and communication-enhancing activities [19] and meaningful occupational activities [21] show a moderate strength of evidence for the improvement of social relationships, cognitive function, and QoL. However, no improvement in agitation in older adults with dementia is observed with psycho-education and stress reduction activities [20].
Overall, these results are consistent with those of Testad et al. [37], which support the value of personalized enjoyable activities, with and without social interaction, for the treatment of dementia symptoms such as depression, anxiety, and challenging behavior. These interventions require the design of tailored activities to meet the individual characteristics of each participant. Therefore, OT professionals play a key role in selecting activities that are adapted to the needs, interests, and degree of impairment of people with dementia in nursing homes [38].
However, the findings show that the level of activity in nursing homes for people with dementia remains low [31]. Therefore, it is essential to offer meaningful activities and to increase the level of activity, for which professionals need knowledge, skills, and tools [39].
In summary, the design and delivery of individualized activities and occupations seem to be beneficial for older adults with dementia, as they facilitate the improvement of behavioral symptoms, anxiety and depression, cognitive functioning, social relationships, and QoL [21].
Second, intervention programs focusing on physical [22,23], cognitive, and sensory activities [24,25,26,27] have therapeutic effects on the physical function, mood, cognitive level, and QoL of residents.
Person-centered physical activity programs that provide physical activities tailored to each individual show moderate strength of evidence in improving the physical function, functional mobility, reduction of falls, ADLs, and QoL in older adults with dementia. In addition, they increase treatment adherence [22,23].
It should also be noted that multisensory stimulation activities complemented with individualized cognitive activities [24], and those based on reminiscence or recall [26,27], show moderate strength of evidence in improving the cognitive function, behavior, mood (depressive symptoms), and QoL of residents. However, music therapy and individualized listening to music show no significant effects on the behavioral and psychological symptoms of dementia [25].
These findings are supported by previous research which identified improvements in mental state and physical functioning associated with increased personal autonomy in older adults with dementia living in nursing homes [40,41].
In short, the design of physical, cognitive, and sensory activity programs seems to be effective in promoting the improved physical, cognitive, and emotional functioning and QoL of older adults with dementia living in nursing homes [22,27].
Third, intervention programs based on performance areas such as ADLs, IADLs, health management activities, work-related activities, and recreational and leisure activities [28,29,30] show therapeutic effects on the physical functioning, and behavioral and psychological symptoms of dementia and the QoL of the residents.
Personally tailored activities programs based on the performance of IADLs, work-related activities, and recreational and leisure activities show a high strength of evidence for the improvement of challenging behavior (restlessness, agitation, and aggression) of older adults with dementia [30].
In addition, programs for the improvement of ADLs performance and health management [28], as well as cooking activities in a group format [29], indicate moderate strength of evidence in improving the physical performance, behavior, executive function, and QoL of the residents.
These results are in line with those of Korczak et al. [42], which support the value of performance area-based activities, taking into account the individual’s functional ability to perform the activity and the degree of dementia, for the improvement of the behavior, functional independence, and QoL.
In short, the design and delivery of performance area-based activities seem to be beneficial for older adults with dementia, as they facilitate the improvement of the behavioral symptoms, physical function, functional independence, and QoL [28].
Finally, intervention programs aimed at modifying the physical and social environment and staff training [9,31,32] positively affect the comfort of the residents and thus their QoL.
The specialized training of staff and environmental modification programs show a high strength of evidence for the overall improvement of the QoL in older adults with dementia by improving functional independence and increasing the individual’s control over their immediate environment [9].
Moreover, the findings indicate with moderate strength of evidence [31,32] that such programs can significantly improve resident comfort.
In short, strategies aimed at improving the QoL in people over 65 years old with dementia should follow a two-fold approach. On the one hand, personalized programs that include ADLs, IADLs, recreational and leisure activities, and reminiscence activities, all of which with a strong social component, are required. On the other hand, adapting the residential environment is essential, with particular attention to the specialized training of the nursing home staff [9,32,43].
4.1. Implications for Practice, Policy, and Future Research
- −
- The ability to choose meaningful activities and occupations in which the level of challenge is tailored to the type and stage of dementia and the functional capacity of the older adult with dementia to perform them are key elements in the design of intervention programs for the improvement of the QoL.
- −
- It is essential to increase the level of activity of the residents. Therefore, modifications to residential environments are necessary, including a wider range and variety of activities, organizational changes that favor greater choice for older adults, and the provision of specialized training for healthcare professionals working in nursing homes.
- −
- OT professionals could encourage older adults with dementia to participate in physical, cognitive, sensory, social, and performance area-based activities tailored to their needs, interests, and degree of impairment in order to enhance their well-being and QoL.
- −
- Interventions focused on ADLs, IADLs, reminiscence activities, and recreational and leisure activities from a person-centered approach could improve the physical and cognitive functioning, behavioral and psychological symptoms of dementia, and QoL of residents.
- −
- Future research should focus on such interventions, as well as on the formulation of new policies that consider such an approach.
4.2. Limitations
First, this review was limited by the heterogeneity of studies focused on improving the QoL of older adults with dementia living in nursing homes, in terms of the type, frequency, and duration of OT interventions; QoL measurements; and outcomes. Therefore, the impact of OT interventions on the QoL of this population cannot be fully ascertained. Second, articles indexed in other literature databases were excluded, which might have left out a significant number of related studies. Finally, only articles published in serialized journals were included, so unpublished articles or searches in the gray literature were not taken into account, which may be a valuable source for materials dealing with the specific review question.
5. Conclusions
OT intervention programs based on participation in recreational and free-time activities, reminiscence activities, performance-based activities and the physical and social environment, and specialized staff training, on a frequent and regular basis, and which take into account the interests and abilities of the residents could improve physical and cognitive functioning, behavioral and psychological symptoms of dementia, and the perceived QoL of older adults with dementia living in nursing homes. Therefore, we consider that the current findings can be used as a basis for the design of future intervention programs for the improvement of the QoL of older adults with dementia, as well as to inform care practices and service provision in nursing homes. However, due to the aforementioned limitations of this systematic review, the results should be viewed with caution, and improved studies are required. For future research, it would be necessary to unify the intervention programs in terms of frequency, duration, methodology, and the instruments used to measure QoL.
Author Contributions
Writing—Original Draft: C.U.-P., S.A.-V. and P.M.-M.; Writing—Review and Editing: C.U.-P., S.A.-V. and P.M.-M.; Conceptualization: C.U.-P. and P.M.-M.; Methodology: C.U.-P., S.A.-V. and P.M.-M.; Formal Analysis: C.U.-P., S.A.-V. and P.M.-M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- American Psychiatric Association. DSM-5 Task Force. In Diagnostic and Statistical Manual of Mental Disorders: DSM-5TM, 5th ed.; American Psychiatric Publishing, Inc.: Arlington, VA, USA, 2013. [Google Scholar] [CrossRef]
- World Health Organization. Dementia; WHO: Geneva, Switzerland, 2023; Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 11 July 2023).
- Kao, Y.H.; Hsu, C.C.; Yang, Y.H. A Nationwide Survey of Dementia Prevalence in Long-Term Care Facilities in Taiwan. J. Clin. Med. 2022, 11, 1554. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Action Plan on the Public Health Response to Dementia 2017–2025; WHO: Geneva, Switzerland, 2017; Available online: https://apps.who.int/iris/bitstream/handle/10665/259615/9789241513487-eng.pdf?sequence=1 (accessed on 12 July 2023).
- Boggatz, T. Quality of life in old age—A concept analysis. Int. J. Older People Nurs. 2016, 11, 55–69. [Google Scholar] [CrossRef]
- Fernández-Ballesteros, R. Quality of Life in old life. Some problematic issues. Appl. Res. Qual. Life 2011, 11, 21–40. [Google Scholar] [CrossRef]
- Imserso. Los Centros Residenciales. 16 December 2022. Available online: https://imserso.es/centros/centros-personas-mayores/centros-residenciales (accessed on 12 July 2023).
- American Occupational Therapy Association. Occupational therapy practice framework: Domain and process (4th ed.). Am. J. Occup. Ther. 2020, 74 (Suppl. S2), 7412410010. [CrossRef] [PubMed]
- Ojagbemi, A.; Owolabi, M. Do occupational therapy interventions improve quality of life in persons with dementia? A meta-analysis with implications for future directions. Psychogeriatr. Off. J. Jpn. Psychogeriatr. Soc. 2017, 17, 133–141. [Google Scholar] [CrossRef] [PubMed]
- Portillo, C.U.; Calvo Arenillas, J.I.; Miralles, P.M. Occupational Therapy Interventions for the Improvement of the Quality of Life of Healthy Older Adults Living in Nursing Homes: A Systematic Review. Am. J. Health Promot. 2023, 37, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Tokolahi, E.; Hocking, C.; Kersten, P.; Vandal, A.C. Quality and Reporting of Cluster Randomized Controlled Trials Evaluating Occupational Therapy Interventions: A Systematic Review. OTJR Occup. Particip. Health 2016, 36, 14–24. [Google Scholar] [CrossRef] [PubMed]
- Kirsh, B.; Martin, L.; Hultqvist, J.; Eklund, M. Occupational Therapy Interventions in Mental Health: A literature review in search of evidence. Occup. Ther. Ment. Health 2019, 35, 109–156. [Google Scholar] [CrossRef]
- Bennett, S.; Laver, K.; Voigt-Radloff, S.; Letts, L.; Clemson, L.; Graff, M.; Wiseman, J.; Gitlin, L. Occupational therapy for people with dementia and their family carers provided at home: A systematic review and meta-analysis. BMJ Open 2019, 9, e026308. [Google Scholar] [CrossRef] [PubMed]
- Birken, M.; Wenborn, J.; Connell, C. Randomised controlled trials of occupational therapy interventions for adults with a mental health condition or dementia: A systematic review of study methods and outcome measurement. Br. J. Occup. Ther. 2022, 85, 761–778. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; Wiley: Hoboken, NJ, USA, 2019. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Oxford Centre for Evidence-Based Medicine. Oxford Centre for Evidence-Based Medicine: Levels of Evidence (March 2009); Oxford Centre for Evidence-Based Medicine: Oxford, UK, 2009; Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/oxford-centre-for-evidence-based-medicine-levels-of-evidence-march-2009 (accessed on 13 July 2023).
- Travers, C.; Brooks, D.; Hines, S.; O’Reilly, M.; McMaster, M.; He, W.; MacAndrew, M.; Fielding, E.; Karlsson, L.; Beattie, E. Effectiveness of meaningful occupation interventions for people living with dementia in residential aged care: A systematic review: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2016, 14, 163–225. [Google Scholar] [CrossRef] [PubMed]
- Mansbach, W.E.; Mace, R.A.; Clark, K.M.; Firth, I.M. Meaningful Activity for Long-Term Care Residents with Dementia: A Comparison of Activities and Raters. Gerontologist 2017, 57, 461–468. [Google Scholar] [CrossRef] [PubMed]
- Livingston, G.; Barber, J.; Marston, L.; Stringer, A.; Panca, M.; Hunter, R.; Cooper, C.; Laybourne, A.; La Frenais, F.; Reeves, S.; et al. Clinical and cost-effectiveness of the Managing Agitation and Raising Quality of Life (MARQUE) intervention for agitation in people with dementia in care homes: A single-blind, cluster-randomised controlled trial. Lancet Psychiatry 2019, 6, 293–304. [Google Scholar] [CrossRef] [PubMed]
- Sultan Ibrahim, S.A.; Dahlan, A.; Che Daud, A.Z. Effects of Occupation-Based Intervention for Older People with Mild Dementia in the Institution. Environ. Behav. Proc. J. 2021, 6, 119–125. [Google Scholar] [CrossRef]
- Galik, E.; Resnick, B.; Hammersla, M.; Brightwater, J. Optimizing function and physical activity among nursing home residents with dementia: Testing the impact of function-focused care. Gerontologist 2014, 54, 930–943. [Google Scholar] [CrossRef] [PubMed]
- Chu, C.H.; Puts, M.; Brooks, D.; Parry, M.; McGilton, K.S. A Feasibility Study of a Multifaceted Walking Intervention to Maintain the Functional Mobility, Activities of Daily Living, and Quality of Life of Nursing Home Residents with Dementia. Rehabil. Nurs. Off. J. Assoc. Rehabil. Nurses 2020, 45, 204–217. [Google Scholar] [CrossRef] [PubMed]
- Maseda, A.; Sánchez, A.; Marante, M.P.; González-Abraldes, I.; Buján, A.; Millán-Calenti, J.C. Effects of Multisensory Stimulation on a Sample of Institutionalized Elderly People with Dementia Diagnosis: A Controlled Longitudinal Trial. Am. J. Alzheimer’s Dis. Other Dement. 2014, 29, 463–473. [Google Scholar] [CrossRef] [PubMed]
- Raglio, A.; Bellandi, D.; Baiardi, P.; Gianotti, M.; Ubezio, M.C.; Zanacchi, E.; Granieri, E.; Imbriani, M.; Stramba-Badiale, M. Effect of Active Music Therapy and Individualized Listening to Music on Dementia: A Multicenter Randomized Controlled Trial. J. Am. Geriatr. Soc. 2015, 63, 1534–1539. [Google Scholar] [CrossRef]
- Lök, N.; Bademli, K.; Selçuk-Tosun, A. The effect of reminiscence therapy on cognitive functions, depression, and quality of life in Alzheimer patients: Randomized controlled trial. Int. J. Geriatr. Psychiatry 2019, 34, 47–53. [Google Scholar] [CrossRef]
- Kim, D. The Effects of a Recollection-Based Occupational Therapy Program of Alzheimer’s Disease: A Randomized Controlled Trial. Occup. Ther. Int. 2020, 2020, 6305727. [Google Scholar] [CrossRef]
- Kumar, P.; Tiwari, S.C.; Goel, A.; Sreenivas, V.; Kumar, N.; Tripathi, R.K.; Gupta, V.; Dey, A.B. Novel occupational therapy interventions may improve quality of life in older adults with dementia. Int. Arch. Med. 2014, 7, 26. [Google Scholar] [CrossRef]
- Murai, T.; Yamaguchi, H. Effects of a Cooking Program Based on Brain-activating Rehabilitation for Elderly Residents with Dementia in a Roken Facility: A Randomized Controlled Trial. Prog. Rehabil. Med. 2017, 2, 20170004. [Google Scholar] [CrossRef][Green Version]
- Möhler, R.; Renom, A.; Renom, H.; Meyer, G. Personally tailored activities for improving psychosocial outcomes for people with dementia in long-term care. Cochrane Database Syst. Rev. 2018, 2, CD009812. [Google Scholar] [CrossRef]
- Wenborn, J.; Challis, D.; Head, J.; Miranda-Castillo, C.; Popham, C.; Thakur, R.; Illes, J.; Orrell, M. Providing activity for people with dementia in care homes: A cluster randomised controlled trial. Int. J. Geriatr. Psychiatry 2013, 28, 1296–1304. [Google Scholar] [CrossRef]
- Froggatt, K.; Best, A.; Bunn, F.; Burnside, G.; Coast, J.; Dunleavy, L.; Goodman, C.; Hardwick, B.; Jackson, C.; Kinley, J.; et al. A group intervention to improve quality of life for people with advanced dementia living in care homes: The Namaste feasibility cluster RCT. Health Technol. Assess. 2020, 24, 1–140. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Sterne, J.; Savović, J.; Page, M.; Hróbjartsson, A.; Boutron, I.; Reeves, B.; Eldridge, S. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst. Rev. 2016, 10 (Suppl. S1), 29–31. [Google Scholar] [CrossRef]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- U.S. Preventive Services Task Force. U.S. Preventive Services Task Force Ratings; U.S. Preventive Services Task Force: Rockville, MD, USA, 2018; Available online: https://www.uspreventiveservicestaskforce.org/uspstf/us-preventive-services-task-force-ratings (accessed on 14 July 2023).
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Testad, I.; Corbett, A.; Aarsland, D.; Lexow, K.O.; Fossey, J.; Woods, B.; Ballard, C. The value of personalized psychosocial interventions to address behavioral and psychological symptoms in people with dementia living in care home settings: A systematic review. Int. Psychogeriatr. 2014, 26, 1083–1098. [Google Scholar] [CrossRef]
- Schuhmacher, T.P.; Andresen, M.; Fallahpour, M. Clinical reasoning of occupational therapists in selecting activities together with older adults with dementia to postpone further development of cognitive decline. Scand. J. Occup. Ther. 2023, 30, 98–108. [Google Scholar] [CrossRef]
- Smit, D.; de Lange, J.; Willemse, B.; Pot, A.M. Predictors of activity involvement in dementia care homes: A cross-sectional study. BMC Geriatr. 2017, 17, 175. [Google Scholar] [CrossRef]
- Littbrand, H.; Stenvall, M.; Rosendahl, E. Applicability and effects of physical exercise on physical and cognitive functions and activities of daily living among people with dementia: A systematic review. Am. J. Phys. Med. Rehabil. 2011, 90, 495–518. [Google Scholar] [CrossRef]
- Telenius, E.W.; Engedal, K.; Bergland, A. Physical performance and quality of life of nursing-home residents with mild and moderate dementia. Int. J. Environ. Res. Public Health 2013, 10, 6672–6686. [Google Scholar] [CrossRef]
- Korczak, D.; Habermann, C.; Braz, S. The effectiveness of occupational therapy for persons with moderate and severe dementia. GMS Health Technol. Assess. 2013, 9, Doc09. [Google Scholar] [CrossRef]
- Borau, P.; López, A.; Blasco, M.; Pardo Sanz, M.P. La ocupación como medio terapéutico, una mirada a través de la historia. Rev. Sanit. De Investig. 2022, 3, 1–5. Available online: https://revistasanitariadeinvestigacion.com/la-ocupacion-como-medio-terapeutico-una-mirada-a-traves-de-la-historia/ (accessed on 14 July 2023).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).