Surgical Emergencies in Patients with Hemophilia A—What to Expect
Abstract
1. Introduction
2. Results
2.1. Case Report
2.1.1. Case 1
2.1.2. Case 2
2.1.3. Case 3
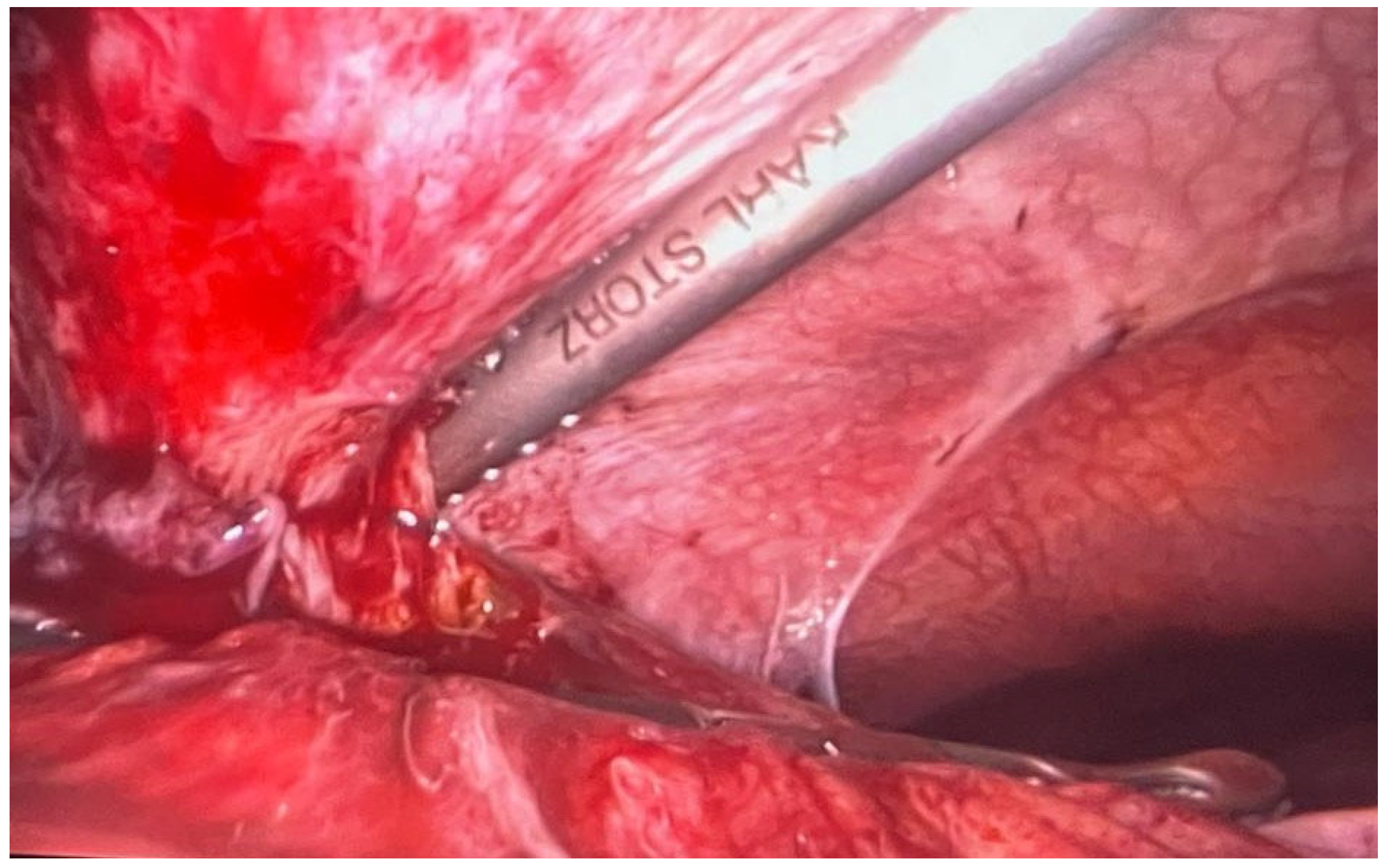
2.1.4. Case 4
2.1.5. Case 5
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Srivastava, A.; Brewer, A.K.; Mauser-Bunschoten, E.P.; Key, N.S.; Kitchen, S.; Llinas, A.; Ludlam, C.A.; Mahlangu, J.N.; Mulder, K.; Poon, M.C.; et al. Guidelines for the management of hemophilia. Haemophilia 2013, 19, e1–e47. [Google Scholar] [CrossRef] [PubMed]
- Blanchette, V.S.; Key, N.S.; Ljung, L.R.; Manco-Johnson, M.J.; van den Berg, H.M.; Srivastava, A. Definitions in hemophilia: Communication from the SSC of the ISTH. J. Thromb. Haemost. 2014, 12, 1935–1939. [Google Scholar] [CrossRef] [PubMed]
- Mazepa, M.A.; Monahan, P.E.; Baker, J.R.; Riske, B.K.; Soucie, J.M. Men with severe hemophilia in the United States: Birth cohort analysis of a large national database. Blood 2016, 127, 3073–3081. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.; Santagostino, E.; Dougall, A.; Kitchen, S.; Sutherland, M.; Pipe, S.W.; Carcao, M.; Mahlangu, J.; Ragni, M.V.; Windyga, J.; et al. WFH guidelines for the management of hemophilia, 3rd edition. Haemophilia 2020, 26 (Suppl. S6), 1–158. [Google Scholar] [CrossRef]
- Krassova, S.; Seremetis, S.; Solimeno, L.P. Major and Minor Surgery in Haemophilia: A Literature Review of Definitions; European Haemophilia Consortium: Belgrade, Serbia, 2015. [Google Scholar]
- Gyanesh, P.; Dhiraaj, S. Anesthetic management of a patient with hemophilia A with spontaneous acute subdural hematoma. J. Anaesthesiol. Clin. Pharmacol. 2013, 29, 117–120. [Google Scholar] [CrossRef]
- World Federation of Hemophilia. Online Registry of Clotting Factor Concentrates. Available online: https://wfh.org/article/wfh-online-registry-of-clotting-factor-concentrates/#:~:text=The%20Online%20CFC%20Registry%20provides,and%20facilitates%20comparisons%20between%20them (accessed on 1 December 2023).
- Giansily-Blaizot, M.; Schved, J.-F. Recombinant human factor VIIa (rFVIIa) in hemophilia: Mode of action and evidence to date. Ther. Adv. Hematol. 2017, 8, 345–352. [Google Scholar] [CrossRef] [PubMed]
- Top, O.; Geisen, U.; Decker, E.L.; Reski, R. Critical Evaluation of Strategies for the Production of Blood Coagulation Factors in Plant-Based Systems. Front. Plant Sci. 2019, 10, 261. [Google Scholar] [CrossRef] [PubMed]
- Solimeno, L.P.; Escobar, M.A.; Krassova, S.; Seremetis, S. Major and Minor Classifications for Surgery in People with Hemophilia: A Literature Review. Clin. Appl. Thromb. 2017, 24, 549–559. [Google Scholar] [CrossRef] [PubMed]
- Zetlaoui, P.J. Ultrasound guided axillary brachial plexus catheter in a patient with severe hemophilia. J. Anesth. Clin. Res. 2013, 4, 1000321. [Google Scholar]
- Gomez, K.; Klamroth, R.; Mahlangu, J.; Mancuso, M.E.; Mingot, M.E.; Ozelo, M.C. Key issues in inhibitor management in patients with haemophilia. Blood Transfus. 2014, 12, s319–s329. [Google Scholar] [CrossRef] [PubMed]
- Poston, J.N.; Kruse-Jarres, R. Perioperative hemostasis for patients with hemophilia. Hematology 2022, 2022, 586–593. [Google Scholar] [CrossRef] [PubMed]
- Parameswaran, R.; Shapiro, A.D.; Gill, J.C.; Kessler, C.M.; HTRS Registry Investigators. Dose effect and efficacy of rFVIIa in the treatment of haemophilia patients with inhibitors: Analysis from the Hemophilia and Thrombosis Research Society Registry. Haemophilia 2005, 11, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Young, G.; Blain, R.; Nakagawa, P.; Nugent, D.J. Individualization of bypassing agent treatment for haemophilic patients with inhibitors utilizing thromboelastography. Haemophilia 2006, 12, 598–604. [Google Scholar] [CrossRef] [PubMed]
- Charoenkwan, K.; Iheozor-Ejiofor, Z.; Rerkasem, K.; Matovinovic, E. Scalpel versus electrosurgery for major abdominal incisions. Cochrane Database Syst. Rev. 2017, 6, CD005987. [Google Scholar] [CrossRef]
- Samuel, R.M.; Kshirsagar, A.Y. Comparative study between scalpel versus electrocautery incisions in abdominal surgeries. Int. J. Health Sci. 2022, 6, 3107–3116. [Google Scholar] [CrossRef]
- Mandrioli, M.; Inaba, K.; Piccinini, A.; Biscardi, A.; Sartelli, M.; Agresta, F.; Catena, F.; Cirocchi, R.; Jovine, E.; Tugnoli, G.; et al. Advances in laparoscopy for acute care surgery and trauma. World J. Gastroenterol. 2016, 22, 668–680. [Google Scholar] [CrossRef] [PubMed]
- Zabihi, F.; Rahimi, S.; Moghaddam, K.R. Successful laparoscopic cholecystectomy in a severe type A hemophiliac patient: A case report and review of the literature. Clin. Case Rep. 2022, 10, e6254. [Google Scholar] [CrossRef] [PubMed]

| Clinical Examination and Treatment | ||||
|---|---|---|---|---|
| Symptoms | Diagnostic | Surgical Intervention | Hemostatic Treatment | Evolution |
| Edema and pain in the calf and right leg, chills, and fever | A superinfected hematoma | Puncture and evacuation | Complex anti-inhibitors of factor VIII activity (FEIBA) | Favorable |
| Paraclinical examination | ||||
| Parameter | Value | Parameter | Value | |
| Leukocytes | 12,370/µL | Fibrinogen | 567 mg/dL | |
| Neutrophils | 95,000/µL | INR | 1.02 | |
| Hemoglobin | 12.6 g/dL | PT | 12.3 s | |
| Hematocrit | 38.9% | aPTT | 39.1 s | |
| RBC | 4.33 × 106/µL | aPTT (%) | 1.45 | |
| MCV | 89.8 fL | Prothrombin activity | 97% | |
| MCH | 29.1 pg | FDPs | ++ | |
| MCHC | 32.4 g/dL | Inhibitors | - | |
| Thrombocyte | 228,000/µL | |||
| Clinical Examination and Treatment | ||||
|---|---|---|---|---|
| Symptoms | Diagnostic | Surgical Intervention | Hemostatic Treatment | Evolution |
| Bleeding from tumoral formation at the level of the second toe of the right foot | Toe II gangrene on the level of the right foot | Amputation of the second toe of the right foot with resection of the second metatarsal. | Coagulation factor VIII | Favorable |
| Paraclinical examination | ||||
| Parameter | Value | Parameter | Value | |
| Leukocytes | 8790/µL | Fibrinogen | 387 mg/dL | |
| Neutrophils | 82,400/µL | INR | 1.04 | |
| Hemoglobin | 12.9 g/dL | PT | 12.3 s | |
| Hematocrit | 40.1% | aPTT | 48.8 s | |
| RBC | 5.23 × 106/µL | aPTT (%) | 1.81 | |
| MCV | 76.7 fL | Prothrombin activity | 104% | |
| MCH | 24.7 pg | FDPs | - | |
| MCHC | 32.2 g/dL | Inhibitors | - | |
| Thrombocyte | 294,000/µL | |||
| Clinical Examination and Treatment | ||||
|---|---|---|---|---|
| Symptoms | Diagnostic | Surgical Intervention | Hemostatic Treatment | Evolution |
| Affected general condition and diffuse abdominal pain | Giant ruptured retroperitoneal with hemoperitoneum | Exploratory laparotomy with peritoneal lavage | Coagulation factor VIII and von Willebrand Factor | Favorable |
| Paraclinical examination | ||||
| Parameter | Value | Parameter | Value | |
| Leukocytes | 25,060/µL | Fibrinogen | 472 mg/dL | |
| Neutrophils | 19,000/µL | INR | 1.77 | |
| Hemoglobin | 8.6 g/dL | PT | 19.5 s | |
| Hematocrit | 25.7% | aPTT | 109.1 s | |
| RBC | 3.43 × 106/µL | aPTT (%) | 4.04 | |
| MCV | 74.9 fL | Prothrombin activity | 49% | |
| MCH | 25.1 pg | Inhibitors | + | |
| MCHC | 33.5 g/dL | |||
| Thrombocyte | 631,000/µL | |||
| Clinical Examination and Treatment | ||||
|---|---|---|---|---|
| Symptoms | Diagnostic | Surgical Intervention | Hemostatic Treatment | Evolution |
| Upper abdominal pain | Acute cholecystitis | Classic cholecystectomy | Eptacog alfa | Favorable |
| Paraclinical examination | ||||
| Parameter | Value | Parameter | Value | |
| Leukocytes | 14,030/µL | Fibrinogen | 598 mg/dL | |
| Neutrophils | 10,480/µL | CRP | 9.53 mg/dL | |
| Hemoglobin | 15.1 g/dL | INR | 14.90 | |
| Hematocrit | 44.6% | PT | 12.3 s | |
| RBC | 5.27 × 106/µL | aPTT | 96.6 s | |
| MCV | 84.6 fL | aPTT (%) | 3.58 | |
| MCH | 28.7 pg | Prothrombin activity | 68% | |
| MCHC | 33.9 g/dL | Inhibitors | + | |
| Thrombocyte | 474,000/µL | |||
| Clinical Examination and Treatment | ||||
|---|---|---|---|---|
| Symptoms | Diagnostic | Surgical Intervention | Hemostatic Treatment | Evolution |
| Affected general condition and diffuse abdominal pain | Ischemic pancolitis | Total colectomy with partial resection of the rectum | Eptacog alfa | Favorable |
| Paraclinical examination | ||||
| Parameter | Value | Parameter | Value | |
| Leukocytes | 13,020/µL | Fibrinogen | 695 mg/dL | |
| Neutrophils | 89,000/µL | CRP | 39.98 | |
| Hemoglobin | 15.7 g/dL | INR | 1.47 | |
| Hematocrit | 44.2% | PT | 16.2 s | |
| RBC | 5.34 × 106/µL | aPTT | 38.3 s | |
| MCV | 82.8 fL | aPTT (%) | 1.45 | |
| MCH | 29.4 pg | Prothrombin activity | 64% | |
| MCHC | 35.5 g/dL | |||
| Thrombocyte | 204,000/µL | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanevski, A.; Ciuntu, B.M.; Badulescu, O.V.; Buescu, D.O.; Zuzu, M.M.; Lutenco, V.; Mihailov, R.; Cirdeiu, C.; Vintila, D.; Lozneanu, L.G.; et al. Surgical Emergencies in Patients with Hemophilia A—What to Expect. Healthcare 2024, 12, 610. https://doi.org/10.3390/healthcare12060610
Tanevski A, Ciuntu BM, Badulescu OV, Buescu DO, Zuzu MM, Lutenco V, Mihailov R, Cirdeiu C, Vintila D, Lozneanu LG, et al. Surgical Emergencies in Patients with Hemophilia A—What to Expect. Healthcare. 2024; 12(6):610. https://doi.org/10.3390/healthcare12060610
Chicago/Turabian StyleTanevski, Adelina, Bogdan Mihnea Ciuntu, Oana Viola Badulescu, David Ovidiu Buescu, Mihai Marius Zuzu, Valerii Lutenco, Raul Mihailov, Ciprian Cirdeiu, Dan Vintila, Lili Gabriela Lozneanu, and et al. 2024. "Surgical Emergencies in Patients with Hemophilia A—What to Expect" Healthcare 12, no. 6: 610. https://doi.org/10.3390/healthcare12060610
APA StyleTanevski, A., Ciuntu, B. M., Badulescu, O. V., Buescu, D. O., Zuzu, M. M., Lutenco, V., Mihailov, R., Cirdeiu, C., Vintila, D., Lozneanu, L. G., Andronic, D., & Georgescu, S. O. (2024). Surgical Emergencies in Patients with Hemophilia A—What to Expect. Healthcare, 12(6), 610. https://doi.org/10.3390/healthcare12060610






