Determinants of Continuance Intention to Use Hearing Aids among Older Adults in Tehran (Iran)
Abstract
1. Introduction
2. Theoretical Background and Research Framework
2.1. Expectation-Confirmation Theory (ECT)
2.2. Post-Acceptance Model (PAM)
2.3. Extended Post-Acceptance Model (PAM)
2.4. Confirmation
2.5. Perceived Benefits
2.6. Satisfaction
2.7. Hearing Aid Self-Efficacy
2.8. Extraverted Personality Trait
2.9. Perceived Social Support
2.10. Self-Perceived Hearing Handicap
2.11. Actual Use and Continuance Intention to Use
3. Materials and Methods
3.1. Participants
3.2. Measurement Scales
3.2.1. Continuance Intention and Confirmation Scales
3.2.2. Hearing Aid Self-Efficacy Questionnaire
| Construct | Instruments | Description/Scale | Cronbach’s α |
|---|---|---|---|
| Satisfaction | Persian version of Satisfaction with Amplification in Daily Life (SADL) [65]. | A 15-item questionnaire that evaluates the satisfaction that people feel with their current hearing aids. It quantifies satisfaction using a global score and four subscales: Positive Effect, Service and Cost, Negative Features, and Personal Image. The SADL response scale: 7-point Likert (not at all; a little; somewhat; medium; considerably; greatly; tremendously) | 0.91 |
| Perceived benefit | Persian version of Abbreviated Profile of Hearing Aid Performance (APHAP) [66]. | A 24-item self-assessment inventory that is divided into four subscales that assess communication, including situations in favorable environments (EC scale) and experiences in the presence of noise (BN scale), reverberating rooms (RV scale), and loud sounds (AV scale). The APHAP response scale: A. Always (99%), B. Almost Always (87%), C. Generally, (75%), D. Half the time (50%), E. Occasionally (25%), F. Seldom (12%), G. Never (1%) | 0.92 |
| Actual use | Persian version of the International Outcome Inventory for Hearing Aids (IOI-HA) [67]. | In this study, we defined the actual use of hearing aids based on each participant’s self-report responses to question 1 (average hours of hearing aid use per day) and question 2 (the benefit from hearing aids in the situations where the individual most wanted to hear better) on the IOI-HA. Response scale: 5-point Likert; question 1 (none = 1 … to more than 8 h a day = 5), question 2 (helped not at all = 1 … helped very much = 5) | 0.85 |
| Self-perceived hearing handicap | Persian version of the Hearing Handicap Inventory Screening Version for the Elderly (HHIE-S) [68]. | A 10-item questionnaire that evaluates how an individual perceives the social and emotional effects of hearing impairment. Response scale: 3-point Likert (No = 0; Sometimes = 2; Yes = 4) | 0.85 |
| Perceived social support | The Iranian version of the Multidimensional Scale of Perceived Social Support (MSPSS) [69]. | A 12-item measure of the perceived adequacy of social support from three sources: family, friends, and significant other Response scale: 5-point Likert (strongly disagree = 0, strongly agree = 5) | 0.93 |
| Extraverted personality trait | Persian version of the Ten-Item Personality Inventory (TIPI) [70]. | In this study, we used questions 1 and 6 of the Ten-Item Personality Inventory that evaluates the personality trait of extraversion. Response scale: a 7-point scale ranging from 1 = strongly disagree to 7 = strongly agree | 0.64 |
3.3. Data Analysis
4. Results
4.1. Findings from Multiple Linear Regression
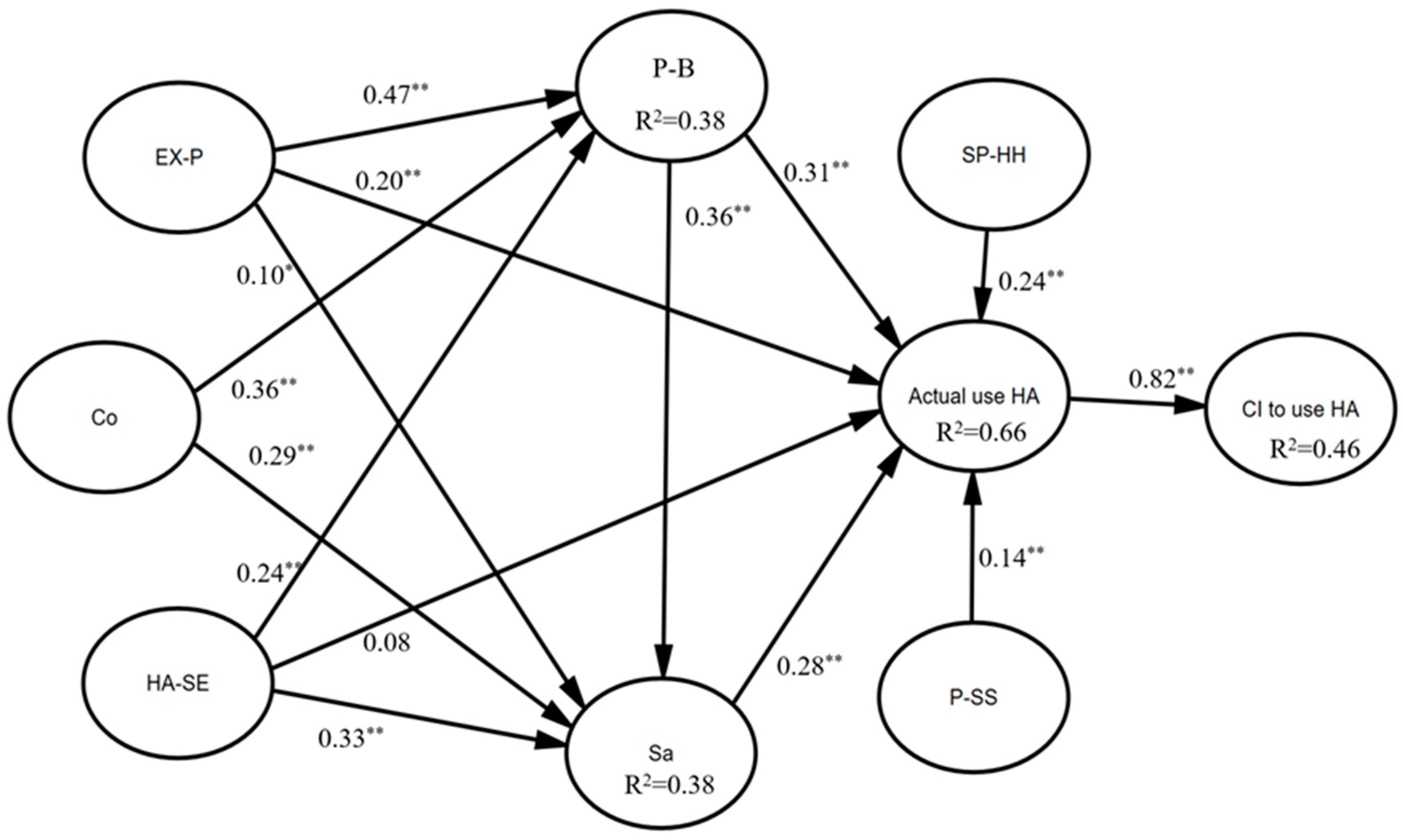
4.2. Results from SEM
5. Discussion
5.1. Demographic and Audiological Characteristics
5.2. Extended PAM-Related Constructs
6. Limitations and Further Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chadha, S.; Kamenov, K.; Cieza, A. The world report on hearing. Bull. World Health Organ. 2021, 99, 242. [Google Scholar] [CrossRef] [PubMed]
- Cui, Q.; Chen, N.; Wen, C.; Xi, J.; Huang, L. Research trends and hotspot analysis of age-related hearing loss from a bibliographic perspective. Front. Psychol. 2022, 13, 921117. [Google Scholar] [CrossRef] [PubMed]
- Lin, F.R.; Yaffe, K.; Xia, J.; Xue, Q.-L.; Harris, T.B.; Purchase-Helzner, E.; Satterfield, S.; Ayonayon, H.N.; Ferrucci, L.; Simonsick, E.M. Hearing loss and cognitive decline in older adults. JAMA Intern. Med. 2013, 173, 293–299. [Google Scholar] [CrossRef]
- Patel, R.; McKinnon, B.J. Hearing loss in the elderly. Clin. Geriatr. Med. 2018, 34, 163–174. [Google Scholar] [CrossRef] [PubMed]
- Arnold, M.L.; Hyer, K.; Small, B.J.; Chisolm, T.; Saunders, G.H.; McEvoy, C.L.; Lee, D.J.; Dhar, S.; Bainbridge, K.E. Hearing aid prevalence and factors related to use among older adults from the Hispanic community health study/study of Latinos. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Kochkin, S. MarkeTrak VIII: 25-year trends in the hearing health market. Hear. Rev. 2009, 16, 12–31. [Google Scholar]
- McCormack, A.; Fortnum, H. Why do people fitted with hearing aids not wear them? Int. J. Audiol. 2013, 52, 360–368. [Google Scholar] [CrossRef]
- Moon, I.J.; Baek, S.Y.; Cho, Y.-S. Hearing aid use and associated factors in South Korea. Medicine 2015, 94, e1580. [Google Scholar] [CrossRef]
- Hougaard, S.; Ruf, S.; Egger, C. EuroTrak+ JapanTrak 2012: Societal and personal benefits of hearing rehabilitation with hearing aids. Hear. Rev. 2013, 20, 16–26. [Google Scholar]
- Sawyer, C.S.; Armitage, C.J.; Munro, K.J.; Singh, G.; Dawes, P.D. Biopsychosocial Classification of Hearing Health Seeking in Adults Aged Over 50 Years in England. Ear Hear. 2020, 41, 1215–1225. [Google Scholar] [CrossRef]
- Jorbonyan, A.; Momtaz, Y.A.; Foroghan, M.; Mehrkian, S. Factors Affecting the Adoption and Use of Hearing Aids among Older Adults: A Systematic Review. Curr. Psychiatry Res. Rev. Former. 2021, 17, 172–187. [Google Scholar] [CrossRef]
- Vestergaard Knudsen, L.; Öberg, M.; Nielsen, C.; Naylor, G.; Kramer, S.E. Factors influencing help seeking, hearing aid uptake, hearing aid use and satisfaction with hearing aids: A review of the literature. Trends Amplif. 2010, 14, 127–154. [Google Scholar] [CrossRef] [PubMed]
- Ng, J.H.-Y.; Loke, A.Y. Determinants of hearing-aid adoption and use among the elderly: A systematic review. Int. J. Audiol. 2015, 54, 291–300. [Google Scholar] [CrossRef] [PubMed]
- Saunders, G.H.; Chisolm, T.H.; Wallhagen, M.I. Older adults and hearing help-seeking behaviors. Am. J. Audiol. 2012, 21, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Saunders, G.H.; Frederick, M.T.; Silverman, S.C.; Nielsen, C.; Laplante-Lévesque, A. Health behavior theories as predictors of hearing-aid uptake and outcomes. Int. J. Audiol. 2016, 55, S59–S68. [Google Scholar] [CrossRef] [PubMed]
- Saunders, G.H.; Frederick, M.T.; Silverman, S.; Papesh, M. Application of the health belief model: Development of the hearing beliefs questionnaire (HBQ) and its associations with hearing health behaviors. Int. J. Audiol. 2013, 52, 558–567. [Google Scholar] [CrossRef] [PubMed]
- Meister, H.; Grugel, L.; Meis, M. Intention to use hearing aids: A survey based on the theory of planned behavior. Patient Prefer. Adherence 2014, 8, 1265–1275. [Google Scholar] [CrossRef][Green Version]
- Cobelli, N.; Gill, L.; Cassia, F.; Ugolini, M. Factors that influence intent to adopt a hearing aid among older people in Italy. Health Soc. Care Community 2014, 22, 612–622. [Google Scholar] [CrossRef]
- DeSanctis, G.; Poole, M.S. Capturing the complexity in advanced technology use: Adaptive structuration theory. Organ. Sci. 1994, 5, 121–147. [Google Scholar] [CrossRef]
- Khaksar, S.M.S.; Khosla, R.; Singaraju, S.; Slade, B. Carer’s perception on social assistive technology acceptance and adoption: Moderating effects of perceived risks. Behav. Inf. Technol. 2021, 40, 337–360. [Google Scholar] [CrossRef]
- Taherdoost, H. A review of technology acceptance and adoption models and theories. Procedia Manuf. 2018, 22, 960–967. [Google Scholar] [CrossRef]
- Laplante-Lévesque, A.; Hickson, L.; Worrall, L. Stages of change in adults with acquired hearing impairment seeking help for the first time: Application of the transtheoretical model in audiologic rehabilitation. Ear Hear. 2013, 34, 447–457. [Google Scholar] [CrossRef] [PubMed]
- Hickson, L.; Meyer, C.; Lovelock, K.; Lampert, M.; Khan, A. Factors associated with success with hearing aids in older adults. Int. J. Audiol. 2014, 53, S18–S27. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Hickson, L.; Lovelock, K.; Lampert, M.; Khan, A. An investigation of factors that influence help-seeking for hearing impairment in older adults. Int. J. Audiol. 2014, 53, S3–S17. [Google Scholar] [CrossRef] [PubMed]
- Duijvestijn, J.; Anteunis, L.J.; Hoek, C.; Van Den Brink, R.H.; Chenault, M.N.; Manni, J.J. Help-seeking behaviour of hearing-impaired persons aged ≥55 years; effect of complaints, significant others and hearing aid image. Acta Oto-Laryngol. 2003, 123, 846–850. [Google Scholar] [CrossRef] [PubMed]
- Bhattacherjee, A. Understanding information systems continuance: An expectation-confirmation model. MIS Q. 2001, 25, 351–370. [Google Scholar] [CrossRef]
- Bøe, T.; Gulbrandsen, B.; Sørebø, Ø. How to stimulate the continued use of ICT in higher education: Integrating information systems continuance theory and agency theory. Comput. Hum. Behav. 2015, 50, 375–384. [Google Scholar] [CrossRef]
- Lin, C.S.; Wu, S.; Tsai, R.J. Integrating perceived playfulness into expectation-confirmation model for web portal context. Inf. Manag. 2005, 42, 683–693. [Google Scholar] [CrossRef]
- Oliver, R.L. A cognitive model of the antecedents and consequences of satisfaction decisions. J. Mark. Res. 1980, 17, 460–469. [Google Scholar] [CrossRef]
- Lankton, N.; McKnight, D.H. Using Expectation Disconfirmation Theory to Predict Technology Trust and Usage Continuance Intentions; Eli Broad College of Business: East Lansing, MI, USA, 2006. [Google Scholar]
- Schwarz, C. Understanding the Role of Expectation Disconfirmation Theory on IT Outsourcing Success. Ph.D. Thesis, Louisiana State University, Baton Rouge, LA, USA, 2011. [Google Scholar]
- Venkatesh, V.; Goyal, S. Expectation disconfirmation and technology adoption: Polynomial modeling and response surface analysis. MIS Q. 2010, 34, 281–303. [Google Scholar] [CrossRef]
- Liao, C.; Palvia, P.; Chen, J.-L. Information technology adoption behavior life cycle: Toward a Technology Continuance Theory (TCT). Int. J. Inf. Manag. 2009, 29, 309–320. [Google Scholar] [CrossRef]
- Wong, L.L.; Hickson, L.; McPherson, B. Satisfaction with hearing aids: A consumer research perspective. Int. J. Audiol. 2009, 48, 405–427. [Google Scholar] [CrossRef] [PubMed]
- Meyer, C.; Hickson, L.; Khan, A.; Walker, D. What is important for hearing aid satisfaction? Application of the expectancy-disconfirmation model. J. Am. Acad. Audiol. 2014, 25, 644–655. [Google Scholar] [CrossRef] [PubMed]
- Venkatesh, V.; Davis, F.D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 2000, 46, 186–204. [Google Scholar] [CrossRef]
- You, J.-J.; Jong, D.; Wiangin, U. Consumers’ Purchase Intention of Organic Food via Social Media: The Perspectives of Task-Technology Fit and Post-acceptance Model. Front. Psychol. 2020, 11, 579274. [Google Scholar] [CrossRef] [PubMed]
- Thong, J.Y.; Hong, S.-J.; Tam, K.Y. The effects of post-adoption beliefs on the expectation-confirmation model for information technology continuance. Int. J. Hum. Comput. Stud. 2006, 64, 799–810. [Google Scholar] [CrossRef]
- Hsiao, C.-H. The effects of post-adoption beliefs on the expectation–confirmation model in an electronics retail setting. Total Qual. Manag. Bus. Excell. 2018, 29, 866–880. [Google Scholar] [CrossRef]
- Cho, J.; Lee, H.E. Post-adoption beliefs and continuance intention of smart device use among people with physical disabilities. Disabil. Health J. 2020, 13, 100878. [Google Scholar] [CrossRef]
- Cho, J. The impact of post-adoption beliefs on the continued use of health apps. Int. J. Med. Inform. 2016, 87, 75–83. [Google Scholar] [CrossRef]
- Gao, S.; Zhang, X.; Peng, S. Understanding the adoption of smart wearable devices to assist healthcare in China. In Proceedings of the Conference on e-Business, e-Services and e-Society, Swansea, UK, 13–15 September 2016; pp. 280–291. [Google Scholar]
- Oliver, R.L. Satisfaction: A Behavioral Perspective on the Consumer; Routledge: New York, NY, USA, 2014. [Google Scholar]
- Cox, R.M.; Alexander, G.C. Expectations about hearing aids and their relationship to fitting outcome. J. Am. Acad. Audiol. 2000, 11, 368–382. [Google Scholar] [CrossRef]
- Saunders, G.H.; Lewis, M.S.; Forsline, A. Expectations, prefitting counseling, and hearing aid outcome. J. Am. Acad. Audiol. 2009, 20, 320–334. [Google Scholar] [CrossRef] [PubMed]
- Ferguson, M.A.; Woolley, A.; Munro, K.J. The impact of self-efficacy, expectations, and readiness on hearing aid outcomes. Int. J. Audiol. 2016, 55, S34–S41. [Google Scholar] [CrossRef] [PubMed]
- Davis, F.D. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989, 13, 319–340. [Google Scholar] [CrossRef]
- Davis, F.D.; Bagozzi, R.P.; Warshaw, P.R. User acceptance of computer technology: A comparison of two theoretical models. Manag. Sci. 1989, 35, 982–1003. [Google Scholar] [CrossRef]
- Kim, J.; Park, H.-A. Development of a health information technology acceptance model using consumers’ health behavior intention. J. Med. Internet Res. 2012, 14, e133. [Google Scholar] [CrossRef] [PubMed]
- Kochkin, S. On the Issue of Value: Hearing Aid Benefit. Price Satisf. Brand Repurchase Rates Hear. Rev. 2003, 7, 6–34. [Google Scholar]
- Purdy, S.C.; Jerram, C.K. Investigation of the profile of hearing aid performance in experienced hearing aid users. Ear Hear. 1998, 19, 473–480. [Google Scholar] [CrossRef]
- Aazh, H.; Prasher, D.; Nanchahal, K.; Moore, B.C. Hearing-aid use and its determinants in the UK National Health Service: A cross-sectional study at the Royal Surrey County Hospital. Int. J. Audiol. 2015, 54, 152–161. [Google Scholar] [CrossRef]
- Singh, G.; Lau, S.-T.; Pichora-Fuller, M.K. Social support predicts hearing aid satisfaction. Ear Hear. 2015, 36, 664–676. [Google Scholar] [CrossRef]
- Korkmaz, M.H.; Bayır, Ö.; Er, S.; Işık, E.; Saylam, G.; Tatar, E.Ç.; Özdek, A. Satisfaction and compliance of adult patients using hearing aid and evaluation of factors affecting them. Eur. Arch. Oto-Rhino-Laryngol. 2016, 273, 3723–3732. [Google Scholar] [CrossRef]
- Meyer, C.; Hickson, L.; Fletcher, A. Identifying the barriers and facilitators to optimal hearing aid self-efficacy. Int. J. Audiol. 2014, 53, S28–S37. [Google Scholar] [CrossRef] [PubMed]
- Barry, E.K.; McCarthy, P. The relationship between personality type and perceived hearing aid benefit. Hear. J. 2001, 54, 41–44. [Google Scholar] [CrossRef]
- Cox, R.M.; Alexander, G.C.; Gray, G.A. Who wants a hearing aid? Personality profiles of hearing aid seekers. Ear Hear. 2005, 26, 12–26. [Google Scholar] [CrossRef]
- Dwarakanath, V.M.; Manjula, P. Influence of Personality and Attitude towards Loss of Hearing on Hearing Aid Outcome in Older Adults with Hearing Loss. Indian J. Otolaryngol. Head Neck Surg. 2022, 74, 387–394. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Launer, S. Social context and hearing aid adoption. Trends Hear. 2016, 20, 2331216516673833. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Classification of Impairments, Disabilities, and Handicaps: A Manual of Classification Relating to the Consequences of Disease, Published in Accordance with Resolution WHA29. 35 of the Twenty-Ninth World Health Assembly, May 1976; World Health Organization: Geneva, Switzerland, 1980. [Google Scholar]
- Angara, P.; Tsang, D.C.; Hoffer, M.E.; Snapp, H.A. Self-Perceived Hearing Status Creates an Unrealized Barrier to Hearing Healthcare Utilization. Laryngoscope 2021, 131, E289–E295. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Sugaya, A.; Nagayasu, R.; Nakagawa, A.; Nishizaki, K. Subjective hearing-related quality-of-life is a major factor in the decision to continue using hearing aids among older persons. Acta Oto-Laryngol. 2016, 136, 919–922. [Google Scholar] [CrossRef]
- Sadeghi, R.; Zanjari, N. The inequality of development in the 22 districts of Tehran metropolis. Soc. Welf. Q. 2017, 17, 149–184. [Google Scholar]
- West, R.L.; Smith, S.L. Development of a hearing aid self-efficacy questionnaire. Int. J. Audiol. 2007, 46, 759–771. [Google Scholar] [CrossRef]
- FarajiKhiavi, F.; Bayat, A.; Dashti, R.; Sameni, S.J. Hearing aid-related satisfaction based on type and degree of hearing loss in elderly. Bimon. Audiol. Tehran Univ. Med. Sci. 2015, 23, 114–122. [Google Scholar]
- Madani, R. Standard Translation APHAB Questionnaire and Evaluation of Benefit in People with Mild to Severe Hearing Loss; Iran University of Medical Sceinces: Tehran, Iran, 2008. (In Persian) [Google Scholar]
- Moossavi, A.; Jalilzade, A.P.; Lotfian, E.; Bakhshi, E. Translating and Assessing the Validity and Reliability of Persian Version of the International Outcome Inventory for Hearing Aids (IOI-HA). J. Rehabil. Sci. Res. 2018, 5, 36–40. [Google Scholar]
- Heidari, F.; Ghahraman, M.A.; Tavanai, E.; Jalaie, S.; Abdollahi, F.Z. Self-assessed hearing handicap in the elderly: A pilot study on Iranian population. Audit. Vestib. Res. 2021, 30, 33–41. [Google Scholar] [CrossRef]
- Bagherian-Sararoudi, R.; Hajian, A.; Ehsan, H.B.; Sarafraz, M.R.; Zimet, G.D. Psychometric properties of the Persian version of the multidimensional scale of perceived social support in Iran. Int. J. Prev. Med. 2013, 4, 1277–1281. [Google Scholar] [PubMed]
- Azkhosh, M.; Sahaf, R.; Rostami, M.; Ahmadi, A. Reliability and Validity of the 10-Item Personality Inventory among Older Iranians. Psychol. Russ. 2019, 12, 28. [Google Scholar] [CrossRef]
- Hartley, D.; Rochtchina, E.; Newall, P.; Golding, M.; Mitchell, P. Use of hearing aids and assistive listening devices in an older Australian population. J. Am. Acad. Audiol. 2010, 21, 642–653. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, L.; Novak, M. Factors influencing hearing aid adoption. Semin. Hear. 2020, 41, 6–20. [Google Scholar] [CrossRef] [PubMed]
- Bulğurcu, S.; Uçak, I.; Yönem, A.; Erkul, E.; Çekin, E. Hearing Aid Problems in Elderly Populations. Ear Nose Throat J. 2020, 99, 323–326. [Google Scholar] [CrossRef]
- Klyn, N.A.M.; Shaikh, Z.M.; Dhar, S. Health literacy and self-reported hearing aid use in the Health and Retirement Study. Ear Hear. 2020, 41, 386–394. [Google Scholar] [CrossRef]
- Ji-Su, K. Prevalence and factors associated with hearing loss and hearing aid use in korean elders. Iran. J. Public Health 2015, 44, 308–317. [Google Scholar]
- Helvik, A.-S.; Krokstad, S.; Tambs, K. How sociodemographic and hearing related factors were associated with use of hearing aid in a population-based study: The HUNT Study. BMC Ear Nose Throat Disord. 2016, 16, 8. [Google Scholar] [CrossRef][Green Version]
- Perez, E.; Edmonds, B.A. A systematic review of studies measuring and reporting hearing aid usage in older adults since 1999: A descriptive summary of measurement tools. PLoS ONE 2012, 7, e31831. [Google Scholar] [CrossRef] [PubMed]
- Tahden, M.A.; Gieseler, A.; Meis, M.; Wagener, K.C.; Colonius, H. What Keeps Older Adults With Hearing Impairment From Adopting Hearing Aids? Trends Hear. 2018, 22, 2331216518809737. [Google Scholar] [CrossRef] [PubMed]
- Bertoli, S.; Staehelin, K.; Zemp, E.; Schindler, C.; Bodmer, D.; Probst, R. Survey on hearing aid use and satisfaction in Switzerland and their determinants. Int. J. Audiol. 2009, 48, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Bertoli, S.; Bodmer, D.; Probst, R. Survey on hearing aid outcome in Switzerland: Associations with type of fitting (bilateral/unilateral), level of hearing aid signal processing, and hearing loss. Int. J. Audiol. 2010, 49, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Yueh, B.; Souza, P.E.; McDowell, J.A.; Collins, M.P.; Loovis, C.F.; Hedrick, S.C.; Ramsey, S.D.; Deyo, R.A. Randomized trial of amplification strategies. Arch. Otolaryngol. Head Neck Surg. 2001, 127, 1197–1204. [Google Scholar] [CrossRef] [PubMed]
- Solheim, J.; Gay, C.; Hickson, L. Older adults’ experiences and issues with hearing aids in the first six months after hearing aid fitting. Int. J. Audiol. 2018, 57, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Cox, R.M.; Alexander, G.C.; Gray, G.A. Personality, hearing problems, and amplification characteristics: Contributions to self-report hearing aid outcomes. Ear Hear. 2007, 28, 141–162. [Google Scholar] [CrossRef]
- Gatehouse, S. Components and determinants of hearing aid benefit. Ear Hear. 1994, 15, 30–49. [Google Scholar] [CrossRef]
- Fuentes-López, E.; Fuente, A.; Valdivia, G.; Luna-Monsalve, M. Does educational level predict hearing aid self-efficacy in experienced older adult hearing aid users from Latin America? Validation process of the Spanish version of the MARS-HA questionnaire. PLoS ONE 2019, 14, e0226085. [Google Scholar] [CrossRef]
- Kelly-Campbell, R.J.; McMillan, A. The relationship between hearing aid self-efficacy and hearing aid satisfaction. Am. J. Audiol. 2015, 24, 529–535. [Google Scholar] [CrossRef]
- Johnson, C.E.; Jilla, A.M.; Danhauer, J.L.; Sullivan, J.C.; Sanchez, K.R. Benefits from, satisfaction with, and self-efficacy for advanced digital hearing aids in users with mild sensorineural hearing loss. Semin. Hear. 2018, 39, 158–171. [Google Scholar]
- Mizutari, K.; Michikawa, T.; Saito, H.; Okamoto, Y.; Enomoto, C.; Takebayashi, T.; Ogawa, K.; Nishiwaki, Y. Age-related hearing loss and the factors determining continued usage of hearing aids among elderly community-dwelling residents. PLoS ONE 2013, 8, e73622. [Google Scholar] [CrossRef]
- Hallberg, L.R.-M.; Hallberg, U.; Kramer, S.E. Self-reported hearing difficulties, communication strategies and psychological general well-being (quality of life) in patients with acquired hearing impairment. Disabil. Rehabil. 2008, 30, 203–212. [Google Scholar] [CrossRef] [PubMed]
- Kamil, R.J.; Genther, D.J.; Lin, F.R. Factors associated with the accuracy of subjective assessments of hearing impairment. Ear Hear. 2015, 36, 164–167. [Google Scholar] [CrossRef] [PubMed]
- Amirkhan, J.H.; Risinger, R.T.; Swickert, R.J. Extraversion: A “hidden” personality factor in coping? J. Personal. 1995, 63, 189–212. [Google Scholar] [CrossRef] [PubMed]
- Vollrath, M.; Torgersen, S. Personality types and coping. Personal. Individ. Differ. 2000, 29, 367–378. [Google Scholar] [CrossRef]
- Alexander, G.C.; Gray, G. Personality and the subjective assessment of hearing aids. J. Am. Acad. Audiol. 1999, 10, 1–13. [Google Scholar]
- Berens, E.-M.; Ganahl, K.; Vogt, D.; Schaeffer, D. Health literacy among elderly immigrants in Germany. Findings from a cross-sectional survey. Eur. J. Public Health 2018, 28, 191–192. [Google Scholar] [CrossRef]
- Moser, S.; Luxenberger, W.; Freidl, W. The influence of social support and coping on quality of life among elderly with age-related hearing loss. Am. J. Audiol. 2017, 26, 170–179. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Pichora-Fuller, M.K. The benefits of social support for listeners with impaired hearing. Hear. J. 2016, 69, 34–36. [Google Scholar] [CrossRef]
- Saunders, G.H.; Jutai, J.W. Hearing specific and generic measures of the psychosocial impact of hearing aids. J. Am. Acad. Audiol. 2004, 15, 238–248. [Google Scholar] [CrossRef]
- Hamidi Pouyandeh, M.; Hoseinabadi, R. Factors Influencing the Hearing Aids Use and Satisfaction: A Review Study. J. Mod. Rehabil. 2019, 13, 137–146. [Google Scholar] [CrossRef]
- Laperuta, E.B.; Fiorini, A.C. Satisfaction of elderly individuals with hearing aids in the first six months of use. J. Soc. Bras. Fonoaudiol. 2012, 24, 316–321. [Google Scholar] [CrossRef][Green Version]
- Kaplan-Neeman, R.; Muchnik, C.; Hildesheimer, M.; Henkin, Y. Hearing aid satisfaction and use in the advanced digital era. Laryngoscope 2012, 122, 2029–2036. [Google Scholar] [CrossRef]
- Laplante-Lévesque, A.; Knudsen, L.V.; Preminger, J.E.; Jones, L.; Nielsen, C.; Öberg, M.; Lunner, T.; Hickson, L.; Naylor, G.; Kramer, S.E. Hearing help-seeking and rehabilitation: Perspectives of adults with hearing impairment. Int. J. Audiol. 2012, 51, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Aurélio, F.S.; Silva, S.P.d.; Rodrigues, L.B.; Kuniyoshi, I.C.; Botelho, M.S. Satisfaction of patients fit with a hearing aid in a high complexity clinic. Braz. J. Otorhinolaryngol. 2012, 78, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.M.; Lee, D. Healthcare wearable devices: An analysis of key factors for continuous use intention. Serv. Bus. 2020, 14, 503–531. [Google Scholar] [CrossRef]
- Davidson, A.; Marrone, N.; Wong, B.; Musiek, F. Predicting Hearing Aid Satisfaction in Adults: A Systematic Review of Speech-in-noise Tests and Other Behavioral Measures. Ear Hear. 2021, 42, 1485–1498. [Google Scholar] [CrossRef]
| Variable | n (%) | Variable | n (%) |
|---|---|---|---|
| Age (mean) | 71.38 (8.05) | Hearing aid usage | |
| 60–74 years | 194 (64.7%) | 6–12 months | 90 (30%) |
| 74–85 years | 81 (27%) | 12–18 months | 75 (25%) |
| +85 years | 25 (8.3%) | ˃18 months | 135 (45%) |
| Gender | Hearing aid fitting | ||
| Female | 152 (50.7%) | Monaural | 98 (32.7%) |
| Male | 148 (49.3%) | Binaural | 202 (67.3%) |
| Education status | Degree of hearing impairment (BEA) | ||
| Illiterate | 45 (15%) | ˂26 dB HL | 12 (4%) |
| Primary | 66 (22%) | 26–40 dB HL | 60 (20%) |
| Secondary | 65 (21.7%) | 41–55 dB HL | 97 (32.3%) |
| Diploma | 77 (25.7%) | 56–70 dB HL | 104 (34.7%) |
| Higher education | 47 (15.6%) | ≥71 dB HL | 27 (9%) |
| Marital status | Hearing aid style | ||
| Married | 211 (70.3%) | ||
| Widow/single | 71 (23.7%) | Behind the ear (BTE) | 203 (67.7%) |
| Divorced | 18 (6%) | In the ear (ITE) | 97 (32.3%) |
| Employment status | Hearing aid type | ||
| Employed | 57 (19%) | ||
| Retired | 99 (33%) | Digital | 243 (81%) |
| Unemployed | 59 (19.7%) | Programmable | 37 (12.3%) |
| Housewife | 85 (28.3%) | Analog | 20 (6.7%) |
| Variable | Actual Use | df | CI to Use HA | ||
|---|---|---|---|---|---|
| Mean Square | Value | Mean Square | Value | ||
| Age | r = −0.16 *** | r = 0.07 * | |||
| Gender | t = 1.36 * | t = 1.53 * | |||
| Education status | 51.28 | F = 12.29 *** | 4 | 16.89 | F = 2.002 * |
| Marital status | 18.67 | F = 2.96 * | 2 | 13.87 | F = 1.63 * |
| Employment status | 20.08 | F = 4.32 *** | 3 | 7.13 | F = 0.83 |
| Degree of hearing impairment (BEA) | 1.70 | F = 0.35 | 4 | 1.13 | F = 0.13 |
| Hearing aid fitting | t = 0.24 | t = 1.22 | |||
| Style of hearing aid | t = −1.16 | t = −0.08 | |||
| Types of hearing aids | 32.72 | F = 7.09 *** | 2 | 56.41 | F = 6.87 *** |
| Hearing aid use | 0.52 | F = 0.1 | 2 | 13.04 | F = 1.53 |
| Variable | Mean (SD) | Possible Range | CI to Use HA | Actual Use HA | Sa | P-B |
|---|---|---|---|---|---|---|
| 1. CI to use HA | 10.14 (2.91) | 3–15 | 1 | |||
| 2. Actual use HA | 6.12 (2.19) | 2–10 | 0.67 ** | 1 | ||
| 5. SP hearing handicap | 17.31 (9.13) | 0–40 | 0.34 ** | 0.41 ** | ||
| 6. HA self-efficacy | 64.58 (16.10) | 0–100 | 0.30 ** | 0.47 ** | ||
| 7. P social support | 45.59 (9.36) | 12–60 | 0.40 ** | 0.41 ** | ||
| 3. Satisfaction | 65.41 (14.78) | 15–105 | 0.50 ** | 0.62 ** | 1 | |
| 4. Perceived benefit | 71.87 (14.40) | 1–99 | 0.49 ** | 0.65 ** | 0.56 ** | 1 |
| 8. Extraversion Pt | 7.83 (2.71) | 2–14 | 0.37 ** | 0.48 ** | 0.39 ** | 0.50 ** |
| 9. Confirmation | 11.67 (2.33) | 3–15 | 0.59 ** | 0.60 ** | 0.46 ** | 0.47 ** |
| Model | F | Sig | R2 | R2adj | SE | Durbin–Watson |
|---|---|---|---|---|---|---|
| CI to use HA | 22.91 | 0.001 | 0.60 | 0.57 | 1.91 | 1.93 |
| Actual use HA | 63.43 | 0.001 | 0.69 | 0.67 | 1.25 | 2.10 |
| Indicators | Cut Point | Results | Conclusion |
|---|---|---|---|
| CMIN/DF | ≤4 | 2.52 | good fit |
| RMSEA | ≤0.08 | 0.07 | good fit |
| GFI | ≥0.90 | 0.87 | Not fit |
| CFI | ≥0.90 | 0.92 | good fit |
| TLI | ≥0.90 | 0.90 | good fit |
| IFI | ≥0.90 | 0.92 | good fit |
| RFI | ≥0.60 | 0.84 | good fit |
| PNFI | ≥0.60 | 0.72 | good fit |
| PCFI | ≥0.60 | 0.76 | good fit |
| AGFI | ≥0.90 | 0.82 | Not fit |
| Path | Total | Direct | Indirect | SE | CR | Sig | Support |
|---|---|---|---|---|---|---|---|
| Confirmation → Perceived Benefit | 0.35 | 0.35 | 0 | 7.35 | 5.34 | 0.001 | yes |
| Confirmation → Satisfaction | 0.41 | 0.29 | 0.12 | 0.22 | 4.23 | 0.002 | yes |
| Perceived Benefit → Satisfaction | 0.35 | 0.35 | 0 | 0.003 | 4.02 | 0.001 | yes |
| Perceived Benefit → Actual Use | 0.40 | 0.30 | 0.10 | 0.004 | 3.96 | 0.001 | yes |
| Perceived Benefit → Actual Use | 0.28 | 0.28 | 0 | 0.03 | 3.54 | 0.001 | yes |
| HA Self-efficacy → Perceived Benefit | 0.24 | 0.24 | 0 | 0.02 | 4.31 | 0.001 | yes |
| HA Self-efficacy → Satisfaction | 0.41 | 0.32 | 0.09 | 0.001 | 4.61 | 0.001 | yes |
| HA Self-efficacy → Actual Use | 0.26 | 0.08 | 0.19 | 0.001 | 1.67 | 0.09 | no |
| Extraversion Pt → Actual Use | 0.41 | 0.20 | 0.21 | 0.06 | 2.69 | 0.007 | yes |
| Extraversion Pt → Perceived Benefit | 0.46 | 0.46 | 0 | 5.51 | 5.96 | 0.001 | yes |
| Extraversion Pt → Satisfaction | 0.26 | 0.10 | 0.16 | 0.16 | 2.24 | 0.04 | yes |
| P Social Support → Actual Use | 0.14 | 0.14 | 0 | 0.01 | 3.19 | 0.001 | yes |
| SP Hearing Handicap → Actual Use | 0.24 | 0.24 | 0 | 0.01 | 4.97 | 0.001 | yes |
| Actual Use → Continuance Intention | 0.81 | 0.81 | 0 | 0.05 | 10.94 | 0.001 | yes |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jorbonyan, A.; Abolfathi Momtaz, Y.; Foroughan, M.; Mehrkian, S. Determinants of Continuance Intention to Use Hearing Aids among Older Adults in Tehran (Iran). Healthcare 2024, 12, 487. https://doi.org/10.3390/healthcare12040487
Jorbonyan A, Abolfathi Momtaz Y, Foroughan M, Mehrkian S. Determinants of Continuance Intention to Use Hearing Aids among Older Adults in Tehran (Iran). Healthcare. 2024; 12(4):487. https://doi.org/10.3390/healthcare12040487
Chicago/Turabian StyleJorbonyan, Abdolhakim, Yadollah Abolfathi Momtaz, Mahshid Foroughan, and Saeideh Mehrkian. 2024. "Determinants of Continuance Intention to Use Hearing Aids among Older Adults in Tehran (Iran)" Healthcare 12, no. 4: 487. https://doi.org/10.3390/healthcare12040487
APA StyleJorbonyan, A., Abolfathi Momtaz, Y., Foroughan, M., & Mehrkian, S. (2024). Determinants of Continuance Intention to Use Hearing Aids among Older Adults in Tehran (Iran). Healthcare, 12(4), 487. https://doi.org/10.3390/healthcare12040487







