Study to Determine the Prevalence of Menstrual Migraine in Reproductive-Age Women in Saudi Arabia
Abstract
1. Introduction
2. Objectives
3. Methodology
3.1. Methods
3.2. Pure Menstrual Migraine
- Migraine attacks in a reproductive-age woman meeting criteria without aura.
- Migraine headache attacks occur during menstruation or 2 days before menstruation, lasting until the third day of menstruation.
- -
- Attacks occur in at least 2 out of 3 menstrual cycles.
- -
- Do not occur at other times during the menstrual cycle.
3.3. Menstrual-Related Migraine
- -
- Migraine attacks in a reproductive-age woman fulfilling criteria without aura.
- -
- Attacks happen on menstruation days or 2 days before, continuing until the third day of menstruation.
- -
- Occur in at least 2 out of 3 menstrual cycles.
- -
- Can also occur at any time during the menstrual cycle.
3.4. Inclusion and Exclusion Criteria
3.5. Ethical Issues
3.6. Statistical Analysis
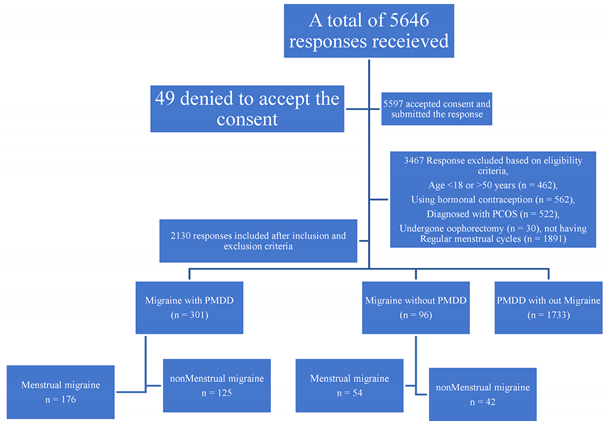
4. Results
5. Discussion
6. Limitations
7. Conclusions and Recommendations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Steiner, T.J.; Stovner, L.J. Global epidemiology of migraine and its implications for public health and health policy. Nat. Rev. Neurol. 2023, 19, 109–117. [Google Scholar] [CrossRef]
- Burch, R. Migraine and tension-type headache: Diagnosis and treatment. Med. Clin. N. Am. 2019, 103, 215–233. [Google Scholar] [CrossRef]
- Pescador Ruschel, M.A.; De Jesus, O. Migraine Headache. [Updated 13 February 2023]. In Stat Pearls; Stat Pearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK560787/ (accessed on 15 September 2023).
- Tonini, M.C. Gender differences in migraine. Neurol. Sci. 2018, 39, 77–78. [Google Scholar] [CrossRef]
- MacGregor, E.A. Progress in the pharmacotherapy of menstrual migraine. Clin. Med. Insights Ther. 2011, 3, 245–273. [Google Scholar] [CrossRef]
- Mayo Clinic. Diagnosis & Treatment. Premenstrual Syndrome (PMS). Last Updated 25 February 2022. Available online: https://www.mayoclinic.org/diseases-conditions/premenstrual-syndrome/symptoms-causes/syc-20376780 (accessed on 5 June 2023).
- Abu Alwafa, R.; Badrasawi, M.; Haj Hamad, R. Prevalence of premenstrual syndrome and its association with psychosocial and lifestyle variables: A cross-sectional study from Palestine. BMC Women’s Health 2021, 21, 233. [Google Scholar] [CrossRef]
- Abbas, K.; Usman, G.; Ahmed, M.; Qazi, R.; Asghar, A.; Shah, A.M.; Rizvi, A.; Abid, K.; Haq, K.U.; Tahir, A.; et al. Physical and Psychological symptoms associated with premenstrual syndrome and their impact on the daily routine of women in a low socioeconomic status locality. Cureus 2020, 12, e10821. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd ed. Cephalalgia 2018, 38, 1–211. [Google Scholar] [CrossRef]
- Ornello, R.; De Matteis, E.; Di Felice, C.; Caponnetto, V.; Pistoia, F.; Sacco, S. Acute and Preventive Management of Migraine during Menstruation and Menopause. J. Clin. Med. 2021, 10, 2263. [Google Scholar] [CrossRef]
- Chalmer, M.A.; Kogelman, L.J.A.; Ullum, H.; Sørensen, E.; Didriksen, M.; Mikkelsen, S.; Dinh, K.M.; Brodersen, T.; Nielsen, K.R.; Bruun, M.T.; et al. Population-Based Characterization of Menstrual Migraine and Proposed Diagnostic Criteria. JAMA Netw. Open 2023, 6, e2313235. [Google Scholar] [CrossRef]
- Amiri, P.; Kazeminasab, S.; Nejadghaderi, S.A.; Mohammadinasab, R.; Pourfathi, H.; Araj-Khodaei, M.; Sullman, M.J.M.; Kolahi, A.-A.; Safiri, S. Migraine: A Review of Its History, Global Epidemiology, Risk Factors, and Comorbidities. Front. Neurol. 2022, 12, 800605. [Google Scholar] [CrossRef]
- Dilbaz, B.; Aksan, A. Premenstrual syndrome, a common but underrated entity: Review of the clinical literature. J. Turk. Ger. Gynecol. Assoc. 2021, 22, 139–148. [Google Scholar] [CrossRef]
- MacGregor, E.A. Migraine headache in perimenopausal and menopausal women. Curr. Pain Headache Rep. 2009, 13, 399–403. [Google Scholar] [CrossRef]
- Macgregor, E.A. Menstrual migraine: Therapeutic approaches. Ther. Adv. Neurol. Disord. 2009, 2, 327–336, Erratum in Ther. Adv. Neurol. Disord. 2010, 3, 197–198. [Google Scholar] [CrossRef]
- Moy, G.; Gupta, V. Menstrual-Related Headache. [Updated 4 October 2022]. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, January 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK557451/ (accessed on 15 September 2023).
- Calhoun, A.H. Understanding Menstrual Migraine. Headache 2018, 58, 626–630. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A. Menstrual migraine: A distinct disorder needing greater recognition. Lancet Neurol. 2021, 20, 304–315. [Google Scholar] [CrossRef]
- Ramírez, A.L.; Rubio-Beltrán, E.; Villalón, C.M.; Maassen Vandenbrink, A. Gender aspects of CGRP in migraine. Cephalalgia 2017, 39, 435–444. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; Russell, M.B. Symptoms of premenstrual syndrome in female migraineurs with and without menstrual migraine. J. Headache Pain. 2018, 19, 97. [Google Scholar] [CrossRef]
- Wang, S.J.; Fuh, J.L.; Lu, S.R.; Juang, K.D.; Wang, P.H. Migraine prevalence during the menopausal transition. Headache 2003, 43, 470–478. [Google Scholar] [CrossRef]
- Mishra, S.; Elliott, H.; Marwaha, R. Premenstrual Dysphoric Disorder. [Updated 19 February 2023]. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK532307/ (accessed on 15 September 2023).
- Bakhsh, H.; Alghamdi, A.M.; Alyahya, M.A.; Alghamdi, S.J.; Alonazi, A.; Algomaishy, R.; De Vol, E.; Almalki, A. Prevalence of premenstrual syndrome and its impact on life among women in Princess Nourah Bint Abdul Rahman University in Riyadh, Saudi Arabia. Int. J. Med. Dev. Ctries 2020, 4, 1307–1312. [Google Scholar] [CrossRef]
- Balaha, M.; Amr, M.A.; Moghannum, M.; Muhaida, N. The phenomenology of premenstrual syndrome in female medical students: A cross-sectional study. Pan. Afr. Med. J. 2010, 5, 4. [Google Scholar] [CrossRef]
- Marcos, E.; Cáceres, P.; Vela, B.; Cavero, J.M. MIDAS/BD: A Methodological Framework for Web Database Design. In Conceptual Modeling for New Information Systems Technologies; Arisawa, H., Kambayashi, Y., Kumar, V., Mayr, H.C., Hunt, I., Eds.; ER 2001, Lecture Notes in Computer Science; Springer: Berlin/Heidelberg, Germany, 2002; p. 2465. [Google Scholar] [CrossRef]
- Kosinski, M.; Bayliss, M.; Bjorner, J.; Ware, J.E., Jr.; Garber, W.; Batenhorst, A.; Cady, R.; Dahlöf, C.; Dowson, A.; Tepper, S. A six-item short-form survey for measuring headache impact: The HIT-6. Qual. Life Res. 2003, 12, 963–974. [Google Scholar] [CrossRef]
- Vetvik, K.G.; MacGregor, E.A.; Lundqvist, C.; Russell, M.B. Prevalence of menstrual migraine: A population-based study. Cephalalgia 2014, 34, 280–288. [Google Scholar] [CrossRef]
- Tschudin, S.; Bertea, P.C.; Zemp, E. Prevalence and predictors of premenstrual syndrome and premenstrual dysphoric disorder in a population-based sample. Arch. Women’s Ment. Health 2010, 13, 485–494. [Google Scholar] [CrossRef]
- Witteveen, H.; van den Berg, P.; Vermeulen, G. Treatment of menstrual migraine; multidisciplinary or mono-disciplinary approach. J. Headache Pain. 2017, 18, 45. [Google Scholar] [CrossRef]
- Muayqil, T.; Al-Jafen, B.N.; Al-Saaran, Z.; Al-Shammari, M.; Alkthiry, A.; Muhammad, W.S.; Murshid, R.; Alanazy, M.H. Migraine, and headache prevalence and associated comorbidities in a large Saudi sample. Eur. Neurol. 2018, 79, 126–134. [Google Scholar] [CrossRef]
- Bamalan, B.A.; Khojah, A.B.; Alkhateeb, L.M.; Gasm, I.S.; Alahmari, A.A.; Alafari, S.A.; Sindi, M.A.; Yaghmour, K.A. Prevalence of migraine among the general population, and its effect on the quality of life in Jeddah, Saudi Arabia. Saudi Med. J. 2021, 42, 1103–1108. [Google Scholar] [CrossRef]
- Yamada, K. High prevalence of MM comorbidity in patients with premenstrual dysphoric disorder: Retrospective survey. Cephalalgia 2016, 36, 294–295. [Google Scholar] [CrossRef]
- Pavlović, J.M.; Stewart, W.F.; Bruce, C.A.; Gorman, J.A.; Sun, H.; Buse, D.C.; Lipton, R.B. The burden of migraine related to menses: Results from the AMPP study. J. Headache Pain. 2015, 16, 24. [Google Scholar] [CrossRef]
- Peterlin, B.L.; Rapoport, A.M.; Kurth, T. Migraine and obesity: Epidemiology, mechanisms, and implications. Headache 2010, 50, 631–648. [Google Scholar] [CrossRef]
- Russell, M.B. Genetics of menstrual migraine: The epidemiological evidence. Curr. Pain. Headache Rep. 2010, 14, 385–388. [Google Scholar] [CrossRef]
- Silberstein, S.D. Menstrual migraine. J. Womens Health Gend. Based Med. 1999, 8, 919–931. [Google Scholar] [CrossRef] [PubMed]
- Mattsson, P. Hormonal factors in migraine: A population-based study of women aged 40 to 74 years. Headache 2003, 43, 27–35. [Google Scholar] [CrossRef] [PubMed]
- Mehkri, Y.; Hanna, C.; Sriram, S.; Lucke-Wold, B.; Johnson, R.D.; Busl, K. Calcitonin gene-related peptide and neurologic injury: An emerging target for headache management. Clin. Neurol. Neurosurg. 2022, 220, 107355. [Google Scholar] [CrossRef]
- Sorrentino, Z.A.; Laurent, D.; Hernandez, J.; Davidson, C.; Small, C.; Dodd, W.; Lucke-Wold, B. Headache persisting after aneurysmal subarachnoid hemorrhage: A narrative review of pathophysiology and therapeutic strategies. Headache 2022, 62, 1120–1132. [Google Scholar] [CrossRef]

| Total | Migraine with PMDD | Migraine without PMDD | PMDD without Migraine | |||
|---|---|---|---|---|---|---|
| Characteristics | n = 2130 | n = 301 (14.1) | n = 96 (4.5) | n = 1733 (81.4) | p Value | |
| Prevalence | - | 14.1% | 4.5% | 81.3% | ||
| Age, median (IQR), years | 24 (21–35) | 27 (22–39) | 35 (23–40) | 24 (21–33) | <0.001 * | |
| Weight, median (IQR), kg | 60 (51–70) | 60 (51.5–70) | 62 (52–74) | 59 (51–69) | 0.1 # | |
| Height, median (IQR), m | 1.6 (1.5–1.6) | 1.6 (1.5–1.6) | 1.6 (1.5–1.6) | 1.6 (1.5–1.6) | 0.04 * | |
| BMI, median (IQR), kg/m2 | 23.3 (20.4–27.2) | 24.2 (20.7–27.5) | 24.9 (21.5–29.5) | 23.1 (20.4–27.1) | 0.004 * | |
| BMI, No. (%) | Underweight (<18.5) | 235 (11) | 27 (9) | 8 (8.3) | 200 (11.5) | 0.003 * |
| Normal weight (18.5–24.9) | 1086 (51) | 139 (46.2) | 40 (41.7) | 907 (52.3) | ||
| Overweight (25–29.9) | 472 (22.9) | 89 (29.6) | 25 (26) | 358 (20.7) | ||
| Obese (≥30) | 319 (14.9) | 46 (15) | 23 (24) | 250 (14.4) | ||
| Obesity | Class–I (30–34.9) | 224(10.5) | 23 (51.1) | 17 (73.7) | 184 (73.6) | |
| Class–II (35–39.9) | 61 (2.9) | 14 (31.1) | 4 (17.4) | 43 (17.2) | ||
| Class–III (≥40) | 34 (1.5) | 9 (17.8) | 2 (8.7) | 23 (9.2) | ||
| Saudi Arabia region, No. (%) | Central | 399 (18.7) | 49 (16.3) | 16 (16.7) | 334 (19.3) | 0.001 * |
| Eastern | 431 (20.2) | 81 (26.9) | 32 (33.3) | 318 (18.3) | ||
| Northern | 114 (5.4) | 20 (6.6) | 3 (3.1) | 91 (5.3) | ||
| Southern | 704 (33.1) | 84 (27.9) | 29 (30.2) | 591 (34.1) | ||
| Western | 482 (22.6) | 67 (22.3) | 16 (16.7) | 399 (23) | ||
| Marital status, No. (%) | Divorced | 60 (2.8) | 6 (2) | 4 (4.2) | 50 (2.9) | 0.001 * |
| Married | 773 (36.3) | 128 (42.5) | 56 (58.3) | 589 (34) | ||
| Single | 1289 (60.5) | 164 (54.5) | 35 (36.5) | 1090 (62.9) | ||
| Widowed | 8 (0.4) | 3 (1) | 1 (1) | 4 (0.2) | ||
| Education level, No. (%) | Primary | 1 (0) | — | — | 1 (0.1) | 0.2 # |
| Intermediate | 17 (0.8) | 2 (0.7) | 2 (2.1) | 13 (0.8) | ||
| High school | 424 (19.9) | 51 (16.9) | 20 (20.8) | 353 (20.4) | ||
| Diploma | 114 (5.4) | 27 (9) | 6 (6.2) | 81 (4.7) | ||
| Graduate | 1472 (69.1) | 206 (68.4) | 64 (66.7) | 1202 (69.4) | ||
| Postgraduate | 102 (4.8) | 15 (5) | 4 (4.2) | 38 (4.8) | ||
| Pregnancy | No | 2051 (96.3) | 290 (96.3) | 95 (99) | 1666 (96.1) | 0.4 |
| Yes | 79 (3.7) | 11 (3.7) | 1 (1) | 67 (3.9) | ||
| Smoking | No | 2002 (94) | 271 (90) | 92 (95.8) | 1639 (94.6) | 0.01 * |
| Yes | 128 (6) | 30 (10) | 4 (4.2) | 94 (5.4) | ||
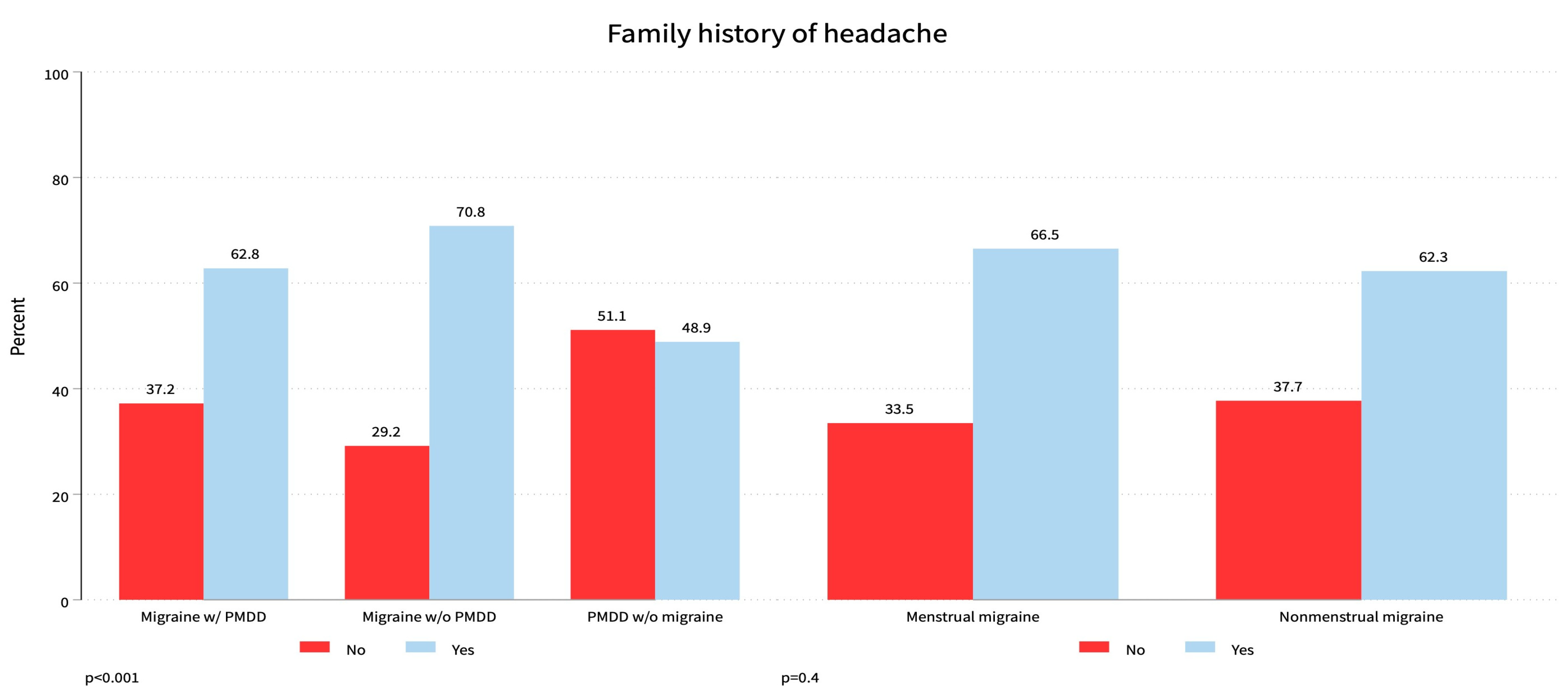
| Family history of headache | No | 1026 (48.2) | 112 (37.2) | 28 (29.2) | 886 (51.1) | 0.001 * |
| Yes | 1104 (51.8) | 189 (62.8) | 68 (70.8) | 847 (48.9) | ||
| Total | Migraine with PMDD | Migraine without PMDD | PMDD without Migraine | |||
|---|---|---|---|---|---|---|
| Characteristics | n = 2130 | n = 301 (14.1) | n = 96 (4.5) | n = 1733 (81.4) | p Value | |
| MM n = 397 | No | 167 (42.1) | 125 (41.5) | 42 (43.8) | NA | 0.7 # |
| Yes | 230 (57.9) | 176 (58.5) | 54 (56.2) | NA | ||
| Time of headache during menstruation n = 397 | Two days before menstruation | 159 (40.0%) | 123 (40.8) | 36 (37.5%) | NA | 0.6 # |
| The first three days of menstruation | 71 (17.8%) | 53 (17.6%) | 18 (18.7%) | NA | ||
| Mid of the menstruation | 167 (42.2%) | 125 (41.6%) | 42 (43.8%) | NA | ||
| Headache attack frequency with menses in the current year, median (IQR) | 5 (2–10) | 5 (2–10) | 5 (0–10) | NA | 1 # | |
| Migraine symptoms | Aggravated by movement | 269 (67.7) | 206 (68.4) | 63 (65.6) | NA | 0.01 * |
| Moderate–severe pain | 277 (69.7) | 221 (73.4) | 56 (58.3) | NA | 0.03 * | |
| Nausea without vomiting | 79 (19.8) | 63 (20.9) | 16 (16.7) | NA | 0.6 # | |
| Photophobia | 44 (11.1) | 35 (11.6) | 9 (9.4) | NA | 0.6 # | |
| Prolonged symptoms (≥72 h) | 397 (100) | 301 (100) | 96 (100) | NA | NA | |
| Pulsatile pain | 270 (68.0) | 228 (75.7) | 62 (64.6) | NA | 0.3 # | |
| Unilateral localization | 318 (80.1) | 241 (80.1) | 77 (80.2) | NA | 1 # | |
| Vomiting | 79 (19.9) | 32 (10.6) | 47 (48.9) | NA | 0.5 # | |
| Aggravating factors | Foods | 44 (11.1) | 35 (11.6) | 9 (9.4) | NA | 0.7 # |
| Menstruation | 260 (65.5) | 210 (69.8) | 50 (52.1) | NA | 0.002 * | |
| Prolonged fasting | 216 (54.4) | 181 (60.1) | 35 (36.5) | NA | 0.001 * | |
| Sleep disturbances | 325 (81.9) | 260 (86.4) | 65 (67.7) | NA | 0.001 * | |
| Smells | 1 (0.3) | 1 (0.3) | — | NA | 1 # | |
| Sounds | 1 (0.3) | — | 1 (1) | NA | 0.2 # | |
| Stress | 3 (0.8) | 1 (0.3) | 2 (2.1) | NA | 0.1 # | |
| Visual | 2 (0.5) | — | 2 (2.1) | NA | 0.1 # | |
| HIT-6 score, median (IQR) | 66 (62–68) | 66 (63–69) | 65 (61–68) | NA | 0.3 # | |
| Migraine severity | Minimal (<50) | 3 (0.8) | 1 (0.3) | 2 (2.1) | NA | 0.1 # |
| Mild (50–55) | 14 (3.5) | 8 (2.7) | 6 (6.2) | NA | ||
| Moderate (56–59) | 38 (9.6) | 28 (9.3) | 10 (10.4) | NA | ||
| Severe (≥60) | 342 (86.1) | 264 (87.7) | 78 (81.2) | NA | ||
| MIDAS score, median (IQR) | 14 (9–24) | 16 (9–27) | 11.5 (7–20) | NA | 0.02 * | |
| Migraine disability | I–Little or no disability | 55 (13.9) | 35 (11.6) | 20 (20.8) | NA | 0.05 * |
| II–Mild disability | 84 (21.2) | 60 (19.9) | 24 (25) | NA | ||
| III–Moderate disability | 134 (33.8) | 105 (34.9) | 29 (30.2) | NA | ||
| IV–Severe disability | 124 (31.2) | 101 (33.6) | 23 (24) | NA | ||
| Prophylaxis therapy | No | 368 (96.8) | 278 (95.9) | 90 (100) | NA | 0.1 # |
| Yes | 12 (3.2) | 12 (4.1) | — | NA | ||
| Prophylaxis medication | Amitriptyline | 4 (33.3) | 4 (33.3) | — | NA | |
| Propranolol | 2 (16.7) | 2 (16.7) | — | NA | ||
| Topiramate | 4 (33.3) | 4 (33.3) | — | NA | ||
| Valproic acid | 2 (16.7) | 2 (16.7) | — | NA | ||
| PMDD symptoms | Anxiety | 1642 (77.1) | 254 (84.6) | NA | 1363 (78.6) | 0.02 * |
| Apathy and loss of interest | 1117 (52.4) | 188 (62.5) | NA | 918 (53) | 0.003 * | |
| Appetite changes | 1280 (60.1) | 202 (67.1) | NA | 1053 (60.8) | 0.04 * | |
| Confusion | 690 (32.4) | 124 (41.2) | NA | 563 (32.5) | 0.004 * | |
| Depressed mood | 1510 (70.9) | 246 (81.7) | NA | 1246 (71.9) | 0.001 * | |
| Easily irritable | 1710 (80.3) | 257 (85.4) | NA | 1414 (81.6) | 0.1 # | |
| Fatigue | 1773 (83.2) | 273 (90.7) | NA | 1467 (84.7) | 0.01 * | |
| Loss of concentration | 875 (41.1) | 170 (56.5) | NA | 700 (40.4) | 0.001 * | |
| Mood disturbances | 1905 (89.4) | 276 (91.7) | NA | 1577 (91) | 0.7 # | |
| Sleep disturbances | 1152 (54.1) | 188 (62.5) | NA | 948 (54.7) | 0.01 * | |
| Somatic symptoms | 1632 (76.6) | 252 (83.7) | NA | 1333 (76.9) | 0.01 * | |
| BMI: Body-mass index; HIT-6: Headache Impact Test; MIDAS: Migraine Disability Assessment questionnaire; NA: Not applicable; PMDD: Premenstrual dysphoric disorder. | ||||||
| Total | Pure Menstrual Migraine | Non-Menstrual Migraine | ||
|---|---|---|---|---|
| Characteristics | n = 397 | n = 230 (57.9) | n = 167 (42.1) | p Value |
| Age, {IQR} (years) | 28 (22–40) | 33 (24–40) | 24 (21–35) | <0.001 * |
| Weight, (IQR), kg | 60 (52–70) | 62 (54–72) | 58.5 (50–70) | 0.01 * |
| Height, (IQR), m | 1.6 (1.5–1.6) | 1.6 (1.5–1.6) | 1.6 (1.5–1.6) | 0.4 # |
| BMI, (IQR), kg/m2 | 24.3 (21.1–27.6) | 25.2 (21.6–28.7) | 23.2 (20.1–27) | 0.01 * |
| BMI, No. (%) | <0.001 * | |||
| Underweight (<18.5) | 35 (8.8) | 12 (5.9) | 23 (13.9) | |
| Normal weight (18.5–24.9) | 179 (45.2) | 96 (41.7) | 83 (50) | |
| Overweight (25–29.9) | 114 (28.8) | 81 (35.2) | 33 (19.9) | |
| Obese (≥30) | 68 (17.2) | 41 (17.8) | 27 (16.3) | |
| Obesity, No. (%) | 0.047 * | |||
| Class–I (30–34.9) | 40 (58.8) | 24 (58.5) | 16 (59.3) | |
| Class–II (35–39.9) | 18 (26.5) | 14 (34.1) | 4 (14.8) | |
| Class–III (≥40) | 10 (14.7) | 3 (7.3) | 7 (25.9) | |
| Saudi Arabia region, No. (%) | 0.1 # | |||
| Central | 65 (16.4) | 35 (15.2) | 30 (18) | |
| Eastern | 113 (28.5) | 76 (33) | 37 (22.2) | |
| Northern | 23 (5.8) | 16 (7) | 7 (4.2) | |
| Southern | 113 (28.5) | 56 (24.3) | 57 (34.1) | |
| Western | 83 (20.9) | 47 (20.4) | 36 (21.6) | |
| Marital status, No. (%) | 0.002 * | |||
| Single | 199 (50.1) | 98 (42.6) | 101 (60.5) | |
| Married | 184 (46.3) | 124 (53.9) | 60 (35.9) | |
| Divorced | 10 (2.5) | 5 (2.2) | 5 (3) | |
| Widowed | 4 (1) | 3 (1.3) | 1 (0.6) | |
| Education level, No. (%) | 0.3 # | |||
| Primary | — | — | — | |
| Intermediate | 4 (1) | 3 (1.3) | 1 (0.6) | |
| High school | 71 (17.9) | 38 (16.5) | 33 (19.8) | |
| Diploma | 33 (8.3) | 19 (8.3) | 14 (8.4) | |
| Graduate | 270 (68) | 155 (67.4) | 115 (68.9) | |
| Postgraduate | 19 (4.8) | 15 (6.5) | 4 (2.4) | |
| Pregnant, No. (%) | 0.6 # | |||
| No | 385 (97) | 224 (97.4) | 161 (96.4) | |
| Yes | 12 (3) | 6 (2.6) | 6 (3.6) | |
| Smoking, No. (%) | 1 # | |||
| No | 363 (91.4) | 210 (91.3) | 153 (91.6) | |
| Yes | 34 (8.6) | 20 (8.7) | 14 (8.4) | |
| Family history of headache, No. (%) | 0.4 # | |||
| No | 140 (35.3) | 77 (33.5) | 63 (37.7) | |
| Yes | 257 (64.7) | 153 (66.5) | 104 (62.3) | |
| Time of headache during menses, No (%) | <0.001 * | |||
| Three days before menses | 155 (58.7) | 147 (63.9) | 8 (23.5) | |
| The first two days of menses | 70 (26.5) | 64 (27.8) | 6 (17.6) | |
| Middle of menses | 19 (7.2) | 18 (7.8) | 1 (2.9) | |
| After menses | 20 (7.6) | 1 (0.4) | 19 (55.9) | |
| Headache attacks frequently with menses in the current year, median (IQR) | 5 (2–10) | 8 (5–12) | 5 (0–5) | <0.001 * |
| Migraine symptoms. No (%) | ||||
| Aggravated by movement | 277 (69.8) | 158 (68.7) | 119 (71.3) | 0.7 # |
| Moderate–severe pain | 290 (73) | 167 (72.6) | 123 (73.7) | 0.9 # |
| Nausea without vomiting | 269 (67.8) | 160 (69.6) | 109 (65.3) | 0.4 # |
| Photophobia | 342 (86.1) | 200 (87) | 142 (85) | 0.7 # |
| Prolonged symptoms (≥72 h) | 397 (100) | 230 (100) | 167 (100) | NA |
| Pulsatile pain | 301 (75.8) | 184 (80) | 117 (70.1) | 0.02 * |
| Unilateral localization | 318 (80.1) | 187 (81.3) | 131 (78.4) | 0.5 # |
| Vomiting | 79 (19.9) | 45 (19.6) | 34 (20.4) | 0.9 # |
| Aggravating factors, No. (%) | ||||
| Foods | 44 (11.1) | 26 (11.3) | 18 (10.8) | 1 # |
| Menstruation | 260 (65.5) | 215 (93.5) | 45 (26.9) | <0.001 * |
| Prolonged fasting | 216 (54.4) | 128 (55.7) | 88 (52.7) | 0.6 # |
| Sleep disturbances | 325 (81.9) | 189 (82.2) | 136 (81.4) | 0.9 # |
| Smells | 1 (0.3) | — | 1 (0.6) | 0.4 |
| Sounds | 1 (0.3) | — | 1 (0.6) | 0.4 # |
| Stress | 3 (0.8) | — | 3 (1.8) | 0.1 # |
| Visual | 2 (0.5) | — | 2 (1.2) | 0.2 # |
| HIT-6 score, median (IQR) | 66 (62–68) | 66 (63–69) | 65 (61–68) | 0.2 # |
| Migraine severity, No (%) | 0.02 * | |||
| Minimal (<50) | 3 (0.8) | — | 3 (1.8) | |
| Mild (50–55) | 14 (3.5) | 5 (2.2) | 9 (5.4) | |
| Moderate (56–59) | 38 (9.6) | 18 (7.8) | 20 (12) | |
| Severe (≥60) | 342 (86.1) | 207 (90) | 135 (80.8) | |
| MIDAS score, median (IQR) | 14 (9–24) | 15 (9–27) | 13 (6–23) | 0.3 # |
| Migraine disability, No. (%) | <0.001 * | |||
| I–Little or no disability | 55 (13.9) | 17 (7.4) | 38 (22.8) | |
| II–Mild disability | 84 (21.2) | 58 (25.2) | 26 (15.6) | |
| III–Moderate disability | 134 (33.8) | 78 (33.9) | 56 (33.5) | |
| IV–Severe disability | 124 (31.2) | 77 (33.5) | 47 (28.1) | |
| Prophylaxis therapy, No. (%) | 0.8 # | |||
| No | 368 (96.8) | 214 (96.4) | 154 (97.5) | |
| Yes | 12 (3.2) | 8 (3.6) | 4 (2.5) | |
| Prophylaxis medications, No. (%) | 0.05 * | |||
| Amitriptyline | 4 (33.3) | 2 (25) | 2 (50) | |
| Propranolol | 2 (16.7) | 2 (25) | — | |
| Topiramate | 4 (33.3) | 4 (50) | — | |
| Valproic acid | 2 (16.7) | — | 2 (50) | |
| BMI: Body-mass index; HIT-6: Headache Impact Test-6 questionnaire; MIDAS: Migraine Disability Assessment questionnaire. | ||||
| Total | Migraine with PMDD | Migraine without PMDD | ||
|---|---|---|---|---|
| Questions, No. (%) | n = 397 | n = 301 (75.8) | n = 96 (24.2) | p Value |
| 1. When you have headaches, how often is the pain severe? | 0.1 # | |||
| Never | — | — | — | |
| Rarely | 11 (2.8) | 6 (2) | 5 (5.2) | |
| Sometimes | 98 (24.7) | 80 (26.6) | 18 (18.8) | |
| Very often | 199 (50.1) | 146 (48.5) | 53 (55.2) | |
| Always | 89 (22.4) | 69 (22.9) | 20 (20.8) | |
| 2. How often do headaches limit your ability to do usual daily activities including household work, work, school, or social activities? | 0.08 # | |||
| Never | 2 (0.5) | 2 (0.7) | — | |
| Rarely | 30 (7.6) | 17 (5.6) | 13 (13.5) | |
| Sometimes | 137 (34.5) | 111 (36.9) | 26 (27.1) | |
| Very often | 165 (41.6) | 124 (41.2) | 41 (42.7) | |
| Always | 63 (15.9) | 47 (15.6) | 16 (16.7) | |
| 3. When you have a headache, how often do you wish you could lie down? | 0.4 # | |||
| Never | 2 (0.5) | 2 (0.7) | — | |
| Rarely | 4 (1) | 2 (0.7) | 2 (2.1) | |
| Sometimes | 44 (11.1) | 30 (10) | 14 (14.6) | |
| Very often | 131 (33) | 102 (33.9) | 29 (30.2) | |
| Always | 216 (54.4) | 165 (54.8) | 51 (53.1) | |
| 4. In the past 4 weeks, how often have you felt too tired to do work or daily activities because of your headaches? | 0.3 # | |||
| Never | 6 (1.5) | 3 (1) | 3 (3.1) | |
| Rarely | 36 (9.1) | 26 (8.6) | 10 (10.4) | |
| Sometimes | 186 (46.9) | 137 (45.5) | 49 (51) | |
| Very often | 131 (33) | 103 (34.2) | 28 (29.2) | |
| Always | 38 (9.6) | 32 (10.6) | 6 (6.2) | |
| 5. In the past 4 weeks, how often have you felt fed up or irritated because of your headaches? | 0.3 # | |||
| Never | 5 (1.3) | 2 (0.7) | 3 (3.1) | |
| Rarely | 38 (9.6) | 26 (8.6) | 12 (12.5) | |
| Sometimes | 161 (40.6) | 115 (38.2) | 46 (47.9) | |
| Very often | 134 (33.8) | 109 (36.2) | 25 (26) | |
| Always | 59 (14.9) | 49 (16.3) | 10 (10.4) | |
| 6. In the past 4 weeks, how often did headaches limit your ability to concentrate on work or daily activities? | 0.1 # | |||
| Never | 8 (2) | 3 (1) | 8 (4.8) | |
| Rarely | 27 (6.8) | 19 (6.3) | 11 (6.6) | |
| Sometimes | 163 (41.1) | 122 (40.5) | 79 (47.3) | |
| Very often | 153 (38.5) | 120 (39.9) | 50 (29.9) | |
| Always | 46 (11.6) | 37 (12.3) | 19 (11.4) | |
| Total | MM | NMM | ||
|---|---|---|---|---|
| Questions, Median (IQR) | n = 397 | n = 230 (57.9) | n = 167 (42.1) | p Value |
| On how many days in the last 3 months did you miss work or school because of your headaches? | 0 (0–3) | 0 (0–3) | 0 (0–2) | |
| How many days in the last 3 months was your productivity at work or school reduced by half or more because of your headaches? (Do not include days you counted in question 1 where you missed work or school.) | 3 (1–5) | 3 (1–6) | 0 (0–5) | 0.1 # |
| On how many days in the last 3 months did you not do household work (such as housework, home repairs, and maintenance, shopping, caring for children and relatives) because of headaches? | 4 (2–6) | 4 (2–7) | 3 (1–5) | 0.1 # |
| How many days in the last 3 months was your productivity in household work reduced by half or more because of headaches? (Do not include days you counted in question 3 where you did not do household work.) | 4 (2–6) | 4 (2–6) | 3 (1–5) | 0.1 # |
| On how many days in the last 3 months did you miss family, social, or leisure activities because of your headaches? | 3 (1–5) | 3 (1–5) | 2 (0–4) | 0.01 * |
| MM: Menstrual migraine; NMM: Non-menstrual migraine. | ||||
| a—Mood’s test with exact calculation | ||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Qahtani, Z.; Narapureddy, B.R.; Reddy, L.K.V.; Asiri, H.Y.M.; Alsulami, A.A.H.; Hassan, N.K.A.; Shawkhan, R.A.; Hamood, N.A.; Almahdi, H.A.M.; Al Qasim, Y.Y.; et al. Study to Determine the Prevalence of Menstrual Migraine in Reproductive-Age Women in Saudi Arabia. Healthcare 2024, 12, 317. https://doi.org/10.3390/healthcare12030317
Al-Qahtani Z, Narapureddy BR, Reddy LKV, Asiri HYM, Alsulami AAH, Hassan NKA, Shawkhan RA, Hamood NA, Almahdi HAM, Al Qasim YY, et al. Study to Determine the Prevalence of Menstrual Migraine in Reproductive-Age Women in Saudi Arabia. Healthcare. 2024; 12(3):317. https://doi.org/10.3390/healthcare12030317
Chicago/Turabian StyleAl-Qahtani, Zainah, Bayapa Reddy Narapureddy, Lingala Kalyan Viswanath Reddy, Hassan Yahya M. Asiri, Ahmed Abdullah H. Alsulami, Nawaf Khalid Ahmed Hassan, Rammas Abdullah Shawkhan, Nouf Abdulraheem Hamood, Hussein Ahmed M. Almahdi, Yousef Yahya Al Qasim, and et al. 2024. "Study to Determine the Prevalence of Menstrual Migraine in Reproductive-Age Women in Saudi Arabia" Healthcare 12, no. 3: 317. https://doi.org/10.3390/healthcare12030317
APA StyleAl-Qahtani, Z., Narapureddy, B. R., Reddy, L. K. V., Asiri, H. Y. M., Alsulami, A. A. H., Hassan, N. K. A., Shawkhan, R. A., Hamood, N. A., Almahdi, H. A. M., Al Qasim, Y. Y., Al Majbar, Y. A. M., Swadi, A. A. A., Asiri, A. H. H., & Almaker, B. A. A. (2024). Study to Determine the Prevalence of Menstrual Migraine in Reproductive-Age Women in Saudi Arabia. Healthcare, 12(3), 317. https://doi.org/10.3390/healthcare12030317







