Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer
Abstract
:1. Introduction
2. Participants and Methods
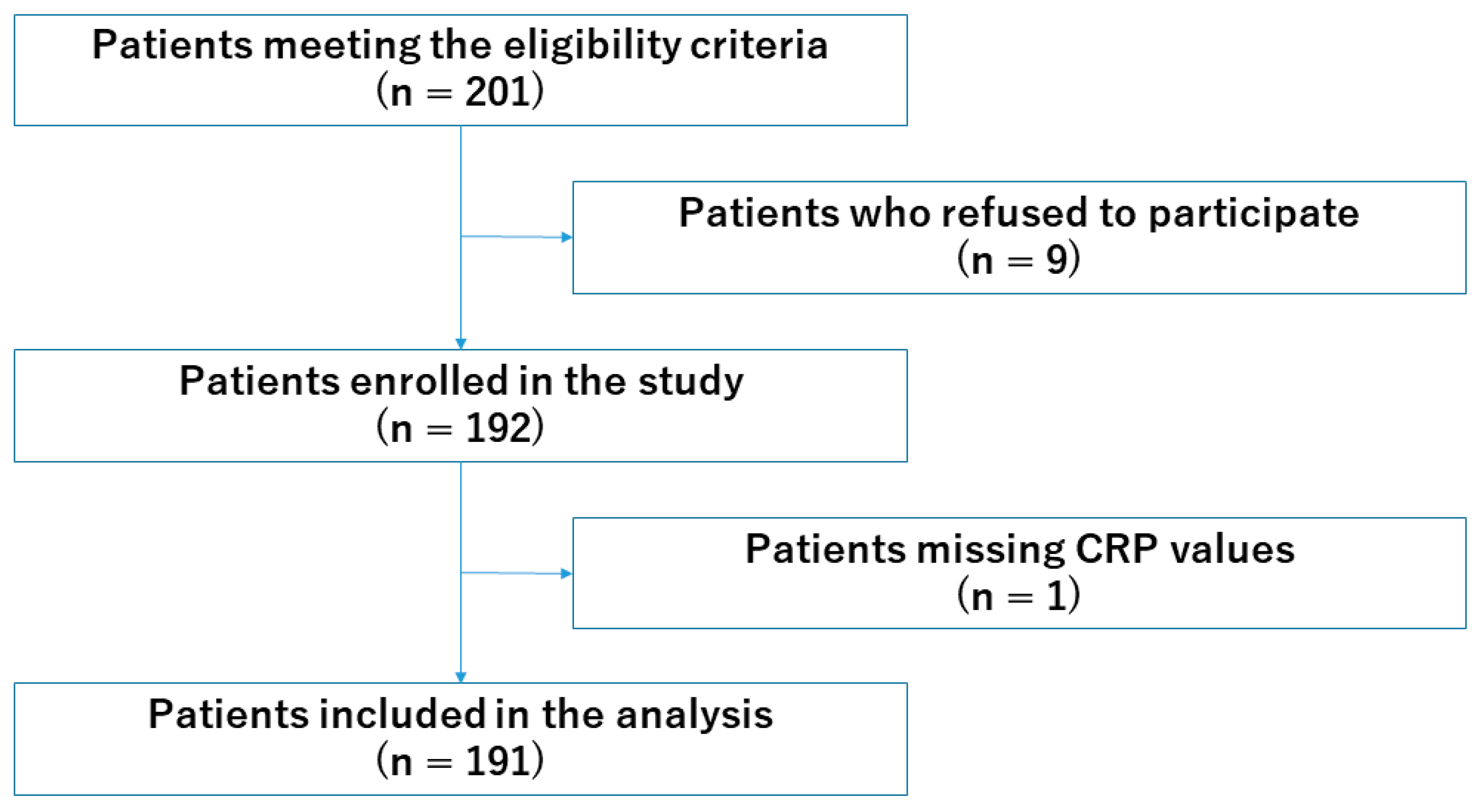
2.1. Sites and Participants
2.2. Ethics Approval and Consent to Participate
2.3. Measurements
2.3.1. Patient Characteristics and Anthropometric Measurements
2.3.2. Dietary Intake
2.3.3. Nutrition Impact Symptoms
2.3.4. Eating-Related Distress
2.3.5. Quality of Life
2.4. Statistical Analysis
2.4.1. Relationships Between Serum C-Reactive Protein Levels, Dietary Intake, Nutrition Impact Symptoms, Eating-Related Distress, and Quality of Life
2.4.2. Association of Serum C-Reactive Protein Levels with Eating-Related Distress
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444. [Google Scholar] [CrossRef] [PubMed]
- Fearon, K.; Strasser, F.; Anker, S.D.; Bosaeus, I.; Bruera, E.; Fainsinger, R.L.; Jatoi, A.; Loprinzi, C.; MacDonald, N.; Mantovani, G.; et al. Definition and classification of cancer cachexia: An international consensus. Lancet Oncol. 2011, 12, 489–495. [Google Scholar] [CrossRef] [PubMed]
- Lippitz, B.E. Cytokine patterns in patients with cancer: A systematic review. Lancet Oncol. 2013, 14, 218–228. [Google Scholar] [CrossRef]
- Candido, J.; Hagemann, T. Cancer-related inflammation. J. Clin. Immunol. 2013, 33, 79–84. [Google Scholar] [CrossRef]
- Diakos, C.I.; Charles, K.A.; McMillan, D.C.; Clarke, S.J. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014, 15, 493–503. [Google Scholar] [CrossRef] [PubMed]
- Baracos, V.E.; Martin, L.; Korc, M.; Guttridge, D.C.; Fearon, K.C. Cancer-associated cachexia. Nat. Rev. Dis. Primers 2018, 4, 17105. [Google Scholar] [CrossRef] [PubMed]
- Ferrer, M.; Anthony, T.G.; Ayres, J.S.; Biffi, G.; Brown, J.C.; Caan, B.J.; Feliciano, E.M.C.; Coll, A.P.; Dunne, R.F.; Goncalves, M.D.; et al. Cachexia: A systemic consequence of progressive, unresolved disease. Cell 2023, 186, 1824–1845. [Google Scholar] [CrossRef] [PubMed]
- Olson, B.; Diba, P.; Korzun, T.; Marks, D.L. Neural Mechanisms of Cancer Cachexia. Cancers 2021, 13, 3990. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Hopkinson, J.; Baracos, V. Psychological symptoms of illness and emotional distress in advanced cancer cachexia. Curr. Opin. Clin. Nutr. Metab. Care 2022, 25, 167–172. [Google Scholar] [CrossRef]
- Yule, M.S.; Brown, L.R.; Skipworth, R.J.E.; Laird, B.J.A. Central neural mechanisms of cancer cachexia. Curr. Opin. Support. Palliat. Care 2024, 18, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Roeland, E.J.; Bohlke, K.; Baracos, V.E.; Bruera, E.; Del Fabbro, E.; Dixon, S.; Fallon, M.; Herrstedt, J.; Lau, H.; Platek, M.; et al. Management of Cancer Cachexia: ASCO Guideline. J. Clin. Oncol. 2020, 38, 2438–2453. [Google Scholar] [CrossRef] [PubMed]
- Arends, J.; Strasser, F.; Gonella, S.; Solheim, T.S.; Madeddu, C.; Ravasco, P.; Buonaccorso, L.; De Van Der Schueren, M.A.E.; Baldwin, C.; Chasen, M.; et al. Cancer cachexia in adult patients: ESMO Clinical Practice Guidelines. ESMO Guidelines Committee. ESMO Open 2021, 6, 100092. [Google Scholar] [CrossRef] [PubMed]
- Muscaritoli, M.; Arends, J.; Bachmann, P.; Baracos, V.; Barthelemy, N.; Bertz, H.; Bozzetti, F.; Hütterer, E.; Isenring, E.; Kaasa, S.; et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. 2021, 40, 2898–2913. [Google Scholar] [CrossRef]
- Crawford, G.B.; Dzierżanowski, T.; Hauser, K.; Larkin, P.; Luque-Blanco, A.I.; Murphy, I.; Puchalski, C.M.; Ripamonti, C.I.; ESMO Guidelines Committee. Care of the adult cancer patient at the end of life: ESMO Clinical Practice Guidelines. ESMO Open 2021, 6, 100225. [Google Scholar] [CrossRef]
- Amano, K.; Hopkinson, J.; Baracos, V.; Mori, N. Holistic multimodal care for patients with cancer cachexia and their family caregivers. Asia Pac. J. Oncol. Nurs. 2023, 10, 100290. [Google Scholar] [CrossRef]
- Laird, B.J.A.; Scott, A.C.; Colvin, L.A.; McKeon, A.L.; Murray, G.D.; Fearon, K.C.H.; Fallon, M.T. Cancer pain and its relationship to systemic inflammation: An exploratory study. Pain 2011, 152, 460–463. [Google Scholar] [CrossRef]
- Laird, B.J.; McMillan, D.C.; Fayers, P.; Fearon, K.; Kaasa, S.; Fallon, M.T.; Klepstad, P. The systemic inflammatory response and its relationship to pain and other symptoms in advanced cancer. Oncologist 2013, 18, 1050–1055. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Maeda, I.; Morita, T.; Miura, T.; Inoue, S.; Ikenaga, M.; Matsumoto, Y.; Baba, M.; Sekine, R.; Yamaguchi, T.; et al. Clinical implications of C-reactive protein as a prognostic marker in advanced cancer patients in palliative care settings. J. Pain Symptom Manag. 2016, 51, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Maeda, I.; Morita, T.; Baba, M.; Miura, T.; Hama, T.; Mori, I.; Nakajima, N.; Nishi, T.; Sakurai, H.; et al. C-reactive protein, symptoms and activity of daily living in patients with advanced cancer receiving palliative care. J. Cachexia Sarcopenia Muscle 2017, 8, 457–465. [Google Scholar] [CrossRef]
- Paulsen, Ø.; Laird, B.; Aass, N.; Lea, T.; Fayers, P.; Kaasa, S.; Klepstad, P. The relationship between proinflammatory cytokines and pain, appetite and fatigue in patients with advanced cancer. PLoS ONE 2017, 12, e0177620. [Google Scholar] [CrossRef]
- Kwekkeboom, K.L.; Tostrud, L.; Costanzo, E.; Coe, C.L.; Serlin, R.C.; Ward, S.E.; Zhang, Y. The role of inflammation in the pain, fatigue, and sleep disturbance symptom cluster in advanced cancer. J. Pain Symptom Manag. 2018, 55, 1286–1295. [Google Scholar] [CrossRef] [PubMed]
- Miranda, D.O.; Anatriello, E.; Azevedo, L.R.; Cordeiro, J.F.C.; Peria, F.M.; Flória-Santos, M.; Pereira-da-Silva, G. Elevated serum levels of proinflammatory cytokines potentially correlate with depression and anxiety in colorectal cancer patients in different stages of the antitumor therapy. Cytokine 2018, 104, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Amano, K.; Hatano, Y.; Matsuda, Y.; Maeda, I.; Ishiki, H.; Miura, T.; Imai, K.; Hori, T.; Matsuda, Y.; Funaki, H.; et al. C-reactive protein, delirium, and other psychological symptoms among patients with advanced cancer. JCSM Clin. Rep. 2020, 5, 42–51. [Google Scholar] [CrossRef]
- Amano, K.; Ishiki, H.; Miura, T.; Maeda, I.; Hatano, Y.; Oyamada, S.; Yokomichi, N.; Tagami, K.; Odagiri, T.; Ito, T.; et al. C-reactive protein and its relationship with pain and other symptoms in patients with advanced cancer cachexia: Analysis of a multicenter prospective cohort study. Palliat. Med. Rep. 2021, 2, 122–131. [Google Scholar] [CrossRef] [PubMed]
- Fortes, G.N.; Fortes, M.F.; Fortes, M.N.; Gomes, F.C.; Seelaendar, M.C.L.; de Pinho, A.M.S.; de Jesus, J.D.C.R.; Otoch, J.P. Mood, Anxiety, and Cognitive Alterations in Cancer Patients. J. Surg. Oncol. 2024, 130, 965–973. [Google Scholar] [CrossRef] [PubMed]
- Eba, J.; Nakamura, K. Overview of the ethical guidelines for medical and biological research involving human subjects in Japan. Jpn. J. Clin. Oncol. 2022, 52, 539–544. [Google Scholar] [CrossRef]
- Oken, M.M.; Creech, R.H.; Tormey, D.C.; Horton, J.; Davis, T.E.; McFadden, E.T.; Carbone, P.P. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am. J. Clin. Oncol. 1982, 5, 649–655. [Google Scholar] [CrossRef] [PubMed]
- Guerdoux-Ninot, E.; Flori, N.; Janiszewski, C.; Vaillé, A.; de Forges, H.; Raynard, B.; Baracos, V.E.; Thezenas, S.; Senesse, P. Assessing dietary intake in accordance with guidelines: Useful correlations with an ingesta-Verbal/Visual Analogue Scale in medical oncology patients. Clin. Nutr. 2019, 38, 1927–1935. [Google Scholar] [CrossRef] [PubMed]
- Wijnhoven, H.A.; van der Velden, L.; Broek, C.; Broekhuizen, M.; Bruynzeel, P.; van Breen, A.; van Oostendorp, N.; de Heer, K. Validation of the Visual/Verbal Analogue Scale of Food Ingesta (Ingesta-VVAS) in Oncology Patients Undergoing Chemotherapy. Nutrients 2022, 14, 3515. [Google Scholar] [CrossRef]
- Amano, K.; Dev, R.; Naito, T.; Del Fabbro, E. International survey on consensus definition on nutrition impact symptoms in patients with cancer. Nutr. Cancer 2024, 1–11. [Google Scholar] [CrossRef]
- Trujillo, E.B.; Kadakia, K.C.; Thomson, C.; Zhang, F.F.; Livinski, A.; Pollard, K.; Mattox, T.; Tucker, A.; Williams, V.; Walsh, D.; et al. Malnutrition risk screening in adult oncology outpatients: An ASPEN systematic review and clinical recommendations. JPEN J. Parenter. Enteral Nutr. 2024, 48, 874–894. [Google Scholar] [CrossRef] [PubMed]
- Aaronson, N.K.; Ahmedzai, S.; Bergman, B.; Bullinger, M.; Cull, A.; Duez, N.J.; Filiberti, A.; Flechtner, H.; Fleishman, S.B.; Haes, J.C.D.; et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. J. Natl. Cancer Inst. 1993, 85, 365–376. [Google Scholar] [CrossRef]
- Amano, K.; Morita, T.; Miura, T.; Mori, N.; Tatara, R.; Kessoku, T.; Matsuda, Y.; Tagami, K.; Otani, H.; Mori, M.; et al. Development and validation of questionnaires for eating-related distress among advanced cancer patients and families. J. Cachexia Sarcopenia Muscle 2023, 14, 310–325. [Google Scholar] [CrossRef] [PubMed]
- Cederholm, T.; Jensen, G.L.; Ballesteros-Pomar, M.D.; Blaauw, R.; Correia, M.I.T.; Cuerda, C.; Evans, D.C.; Fukushima, R.; Gautier, J.B.O.; Gonzalez, M.C.; et al. Guidance for assessment of the inflammation etiologic criterion for the GLIM diagnosis of malnutrition: A modified Delphi approach. Clin. Nutr. 2024, 43, 1025–1032. [Google Scholar] [CrossRef]
- Lasheen, W.; Walsh, D. C-Reactive Protein in Solid Tumors: Clinically Meaningful Change. Biomed. J. Sci. Tech. Res. 2024, 56, 47898–47903. [Google Scholar] [CrossRef]
- Amano, K.; Baracos, V.E.; Mori, N.; Okamura, S.; Yamada, T.; Miura, T.; Tatara, R.; Kessoku, T.; Matsuda, Y.; Tagami, K.; et al. Associations of nutrition impact symptoms with dietary intake and eating-related distress in patients with advanced cancer. Clin. Nutr. ESPEN 2024, 60, 313–319. [Google Scholar] [CrossRef] [PubMed]
| CRP < 5 | CRP ≥ 5 | p Value | |
|---|---|---|---|
| (n = 117) | (n = 75) | ||
| Age in years | 68.0 (56.0, 76.0) | 66.0 (51.0, 74.0) | 0.102 |
| Sex | 0.365 | ||
| Female | 64 (54.7%) | 36 (48.0%) | |
| Male | 53 (45.3%) | 39 (52.0%) | |
| Primary cancer site, n (%) | 0.117 | ||
| Upper and lower gastrointestinal tracts | 12 (10.3%) | 12 (16.0%) | |
| Liver, biliary system, and pancreas | 20 (17.1%) | 13 (17.3%) | |
| Lung | 27 (23.1%) | 13 (17.3%) | |
| Breast | 9 (7.7%) | 3 (4.0%) | |
| Gynecological | 8 (6.8%) | 15 (20.0%) | |
| Urological | 9 (7.7%) | 5 (6.7%) | |
| Head and neck | 6 (5.1%) | 4 (5.3%) | |
| Hematologic malignancy | 11 (9.4%) | 2 (2.7%) | |
| Others | 15 (12.8%) | 8 (10.7%) | |
| Treatment status | 0.072 | ||
| Pre-chemotherapy | 17 (14.5%) | 7 (9.3%) | |
| Chemotherapy | 86 (73.5%) | 50 (66.7%) | |
| Never treated/previous treatment | 14 (12.0%) | 18 (24.0%) | |
| ECOG PS, n (%) | 0.045 | ||
| 0 | 2 (1.7%) | 0 (0.0%) | |
| 1 | 28 (23.9%) | 9 (12.0%) | |
| 2 | 44 (37.6%) | 23 (30.7%) | |
| 3 | 37 (31.6%) | 38 (50.7%) | |
| 4 | 6 (5.1%) | 5 (6.7%) | |
| Body mass index (kg/m2) | 21.3 (18.9, 24.2) | 20.2 (18.7, 23.4) | 0.464 |
| Weight loss rate over 6 months (%) | 5.8 (0.3, 9.9) | 7.2 (3.1, 13.8) | 0.043 |
| Cachexia/refractory cachexia, yes | 71 (60.7%) | 52 (69.3%) | 0.237 |
| Pleural effusion, ascites, or edema affecting weight, yes | 17 (14.5%) | 25 (33.3%) | 0.003 |
| Albumin (g/dL) | 3.5 (3.1, 3.8) | 2.8 (2.4, 3.2) | <0.001 |
| CRP (mg/dL) | 0.7 (0.2, 2.1) | 9.2 (7.0, 12.7) | <0.001 |
| CRP < 5 | CRP ≥ 5 | p-Value | |
|---|---|---|---|
| Dietary intake | |||
| Dietary intake score | 5.0 (3.0, 7.0) | 4.0 (2.0, 5.0) | 0.002 |
| Number of patients with a dietary intake score of 7 or less | 93 (79.5%) | 70 (93.3%) | 0.009 |
| Symptoms that interfere with patients’ ability to ingest or digest nutrients | |||
| Oral pain | 0.0 (0.0, 1.0) | 0.0 (0.0, 1.0) | 0.751 |
| Appetite loss | 5.0 (1.0, 7.0) | 5.0 (3.0, 7.0) | 0.304 |
| Early satiety | 5.0 (2.0, 7.5) | 5.0 (2.0, 8.0) | 0.956 |
| Nausea | 1.0 (0.0, 3.0) | 1.0 (0.0, 3.0) | 0.661 |
| Vomiting | 0.0 (0.0, 1.0) | 0.0 (0.0, 2.0) | 0.012 |
| Constipation | 3.0 (0.0, 6.0) | 5.0 (0.0, 7.0) | 0.458 |
| Diarrhea | 0.0 (0.0, 3.0) | 0.0 (0.0, 5.0) | 0.363 |
| Abnormal taste | 0.0 (0.0, 3.0) | 1.0 (0.0, 7.0) | 0.219 |
| Abnormal smell | 0.0 (0.0, 2.0) | 0.0 (0.0, 1.0) | 0.534 |
| Dry mouth | 2.0 (0.0, 4.0) | 2.0 (0.0, 6.0) | 0.108 |
| Dental problems | 0.0 (0.0, 2.5) | 0.0 (0.0, 2.0) | 0.489 |
| Difficulty swallowing | 0.0 (0.0, 2.0) | 0.0 (0.0, 2.0) | 0.625 |
| Food bolus obstruction | 0.0 (0.0, 3.0) | 0.0 (0.0, 3.0) | 0.533 |
| Symptoms that compromise patients’ desire to eat and take nutrients | |||
| Fatigue | 3.0 (2.0, 6.0) | 4.0 (2.0, 5.0) | 0.709 |
| Drowsiness | 3.0 (1.0, 6.0) | 5.0 (2.0, 6.0) | 0.041 |
| Anxiety | 2.5 (1.0, 5.0) | 3.0 (0.0, 5.0) | 0.823 |
| Feeling sad | 3.0 (1.0, 5.0) | 3.0 (1.0, 5.0) | 0.982 |
| Symptoms that indirectly compromise patients’ food and nutrient intake | |||
| Pain other than oral pain | 3.5 (0.0, 7.0) | 3.0 (0.0, 7.0) | 0.738 |
| Shortness of breath | 2.0 (0.0, 5.0) | 1.0 (0.0, 3.0) | 0.494 |
| Number of nutrition impact symptoms with a score of 4 or more | 6.0 (2.0, 8.0) | 6.0 (4.0, 9.0) | 0.212 |
| CRP < 5 | CRP ≥ 5 | p-Value | |
|---|---|---|---|
| Functional scales | |||
| Physical functioning | 53.3 (33.3, 73.3) | 46.7 (26.7, 73.3) | 0.122 |
| Role functioning | 33.3 (0.0, 66.7) | 33.3 (0.0, 66.7) | 0.604 |
| Emotional functioning | 66.7 (50.0, 83.3) | 66.7 (50.0, 83.3) | 0.221 |
| Cognitive functioning | 66.7 (33.3, 83.3) | 66.7 (50.0, 66.7) | 0.957 |
| Social functioning | 50.0 (33.3, 83.3) | 50.0 (33.3, 83.3) | 0.728 |
| Symptom scales | |||
| Fatigue | 66.7 (44.4, 88.9) | 77.8 (55.6, 88.9) | 0.067 |
| Nausea and vomiting | 16.7 (0.0, 33.3) | 16.7 (0.0, 50.0) | 0.419 |
| Pain | 66.7 (33.3, 100.0) | 83.3 (50.0, 100.0) | 0.222 |
| Dyspnea | 33.3 (33.3, 66.7) | 33.3 (0.0, 100.0) | 0.869 |
| Sleep disturbance | 66.7 (33.3, 100.0) | 66.7 (33.3, 100.0) | 0.612 |
| Appetite loss | 66.7 (33.3, 100.0) | 66.7 (33.3, 100.0) | 0.008 |
| Constipation | 33.3 (0.0, 66.7) | 33.3 (33.3, 66.7) | 0.158 |
| Diarrhea | 0.0 (0.0, 33.3) | 33.3 (0.0, 66.7) | 0.181 |
| Global health status | 33.3 (16.7, 50.0) | 16.7 (16.7, 41.7) | 0.096 |
| Financial difficulties | 33.3 (0.0, 66.7) | 33.3 (0.0, 66.7) | 0.560 |
| CRP < 5 | CRP ≥ 5 | p-Value | |
|---|---|---|---|
| Factor 1: Reduced dietary intake | |||
| It is distressing that I cannot eat even though I want to eat more. | 5.0 (3.0, 6.0) | 5.0 (3.0, 6.0) | 0.308 |
| It is distressing that I cannot enjoy eating. | 5.0 (3.0, 6.0) | 6.0 (4.0, 7.0) | 0.048 |
| It is distressing that I get full quickly and cannot eat enough. | 4.0 (3.0, 6.0) | 5.0 (3.0, 6.0) | 0.245 |
| Factor 2: Reasons why I cannot eat | |||
| I do not understand the reason why I cannot eat. | 3.0 (1.0, 5.0) | 3.0 (2.0, 5.0) | 0.126 |
| I do not understand the reason why I do not have an appetite. | 3.0 (1.0, 4.0) | 3.0 (2.0, 5.0) | 0.100 |
| I do not understand the reason why I cannot eat enough. | 3.0 (1.0, 5.0) | 3.0 (2.0, 5.0) | 0.121 |
| Factor 3: Becoming weaker | |||
| I am concerned that I will become weaker if I cannot eat. | 5.0 (3.0, 6.0) | 6.0 (5.0, 7.0) | 0.022 |
| I am concerned that I will lose muscle strength if I cannot eat. | 5.0 (4.0, 6.0) | 6.0 (5.0, 7.0) | 0.090 |
| I am concerned that I will lose weight if I cannot eat. | 5.0 (3.0, 6.0) | 5.5 (4.0, 6.5) | 0.117 |
| Factor 4: Insufficient information | |||
| I have insufficient information about which nutrients I should prioritized. | 4.0 (3.0, 6.0) | 5.0 (3.0, 5.5) | 0.321 |
| I have insufficient information about which nutrients I should avoid. | 4.0 (3.0, 5.0) | 5.0 (3.0, 5.0) | 0.731 |
| I have insufficient information about which nutritional supplements I should take. | 4.0 (3.0, 5.0) | 5.0 (3.0, 5.0) | 0.460 |
| Factor 5: Arguments with my family | |||
| I have arguments with my family about food. | 2.0 (1.0, 3.0) | 2.0 (1.0, 4.5) | 0.014 |
| I am troubled that my family seems to try to force me to eat. | 1.0 (1.0, 3.0) | 2.0 (1.0, 4.0) | 0.017 |
| I get frustrated with my family over food. | 1.0 (1.0, 3.0) | 1.5 (1.0, 4.0) | 0.274 |
| Factor 6: Change in appearance | |||
| It’s hard for me that my appearance had changed a lot from before as I became thin. | 3.0 (1.0, 5.0) | 4.0 (2.0, 5.0) | 0.157 |
| It’s hard for me to be seen by others as so skinny. | 3.0 (1.0, 5.0) | 3.0 (2.0, 5.0) | 0.635 |
| It’s hard to see myself as so skinny. | 3.0 (1.0, 5.0) | 4.0 (2.0, 5.0) | 0.149 |
| Factor 7: Time with my family | |||
| I spend less time talking with my family because I do not eat with them. | 3.0 (2.0, 5.0) | 4.0 (1.0, 5.0) | 0.557 |
| I spend less time enjoying with my family during meals. | 4.0 (2.0, 5.0) | 4.5 (1.0, 6.0) | 0.372 |
| I spend less time in daily life with my family because I cannot eat. | 3.0 (1.0, 4.0) | 4.0 (1.0, 5.0) | 0.281 |
| Total score of the long version | 76.0 (58.0, 92.0) | 83.0 (66.0, 99.0) | 0.040 |
| Total score of the short version | 25.0 (20.0, 31.0) | 28.0 (23.0, 33.0) | 0.029 |
| The QERD-P Long Version | The QERD-P Short Version | |||
|---|---|---|---|---|
| Odds Ratio (95% CI) | p-Value | Odds Ratio (95% CI) | p-Value | |
| CRP levels | ||||
| <5 mg/dL | Reference | Reference | ||
| ≥5 mg/dL | 2.13 (1.10, 4.11) | 0.024 | 2.06 (1.05, 4.05) | 0.035 |
| Age in years | 0.99 (0.97, 1.02) | 0.640 | 0.99 (0.97, 1.02) | 0.490 |
| Sex | ||||
| Female | Reference | Reference | ||
| Male | 1.49 (0.78, 2.84) | 0.230 | 1.72 (0.89, 3.33) | 0.105 |
| Primary cancer site | ||||
| Lung | Reference | Reference | ||
| Gastrointestinal | 1.56 (0.63, 3.85) | 0.334 | 1.77 (0.70, 4.47) | 0.225 |
| Others | 0.77 (0.33, 1.83) | 0.559 | 0.94 (0.39, 2.23) | 0.883 |
| Treatment status | ||||
| Non-chemotherapy | Reference | Reference | ||
| Chemotherapy | 1.01 (0.50, 2.03) | 0.974 | 1.17 (0.58, 2.37) | 0.667 |
| ECOG PS | ||||
| 0, 1 | Reference | Reference | ||
| 2 | 0.62 (0.25, 1.51) | 0.294 | 0.84 (0.34, 2.07) | 0.706 |
| 3, 4 | 0.73 (0.30, 1.76) | 0.484 | 1.20 (0.49, 2.95) | 0.683 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amano, K.; Koshimoto, S.; Okamura, S.; Sakaguchi, T.; Arakawa, S.; Matsuda, Y.; Tokoro, A.; Takeuchi, T.; Satomi, E.; Wada, T.; et al. Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer. Healthcare 2024, 12, 2533. https://doi.org/10.3390/healthcare12242533
Amano K, Koshimoto S, Okamura S, Sakaguchi T, Arakawa S, Matsuda Y, Tokoro A, Takeuchi T, Satomi E, Wada T, et al. Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer. Healthcare. 2024; 12(24):2533. https://doi.org/10.3390/healthcare12242533
Chicago/Turabian StyleAmano, Koji, Saori Koshimoto, Satomi Okamura, Tatsuma Sakaguchi, Sayaka Arakawa, Yoshinobu Matsuda, Akihiro Tokoro, Takashi Takeuchi, Eriko Satomi, Tamiki Wada, and et al. 2024. "Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer" Healthcare 12, no. 24: 2533. https://doi.org/10.3390/healthcare12242533
APA StyleAmano, K., Koshimoto, S., Okamura, S., Sakaguchi, T., Arakawa, S., Matsuda, Y., Tokoro, A., Takeuchi, T., Satomi, E., Wada, T., Wada, M., Yamada, T., & Mori, N. (2024). Association of Systemic Inflammation with Dietary Intake, Nutrition Impact Symptoms, and Eating-Related Distress Among Patients with Advanced Cancer. Healthcare, 12(24), 2533. https://doi.org/10.3390/healthcare12242533






