Effect of Reformer Spring Resistance Modifications on Core Muscle Activity During Basic Core Muscle Exercises
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Procedure
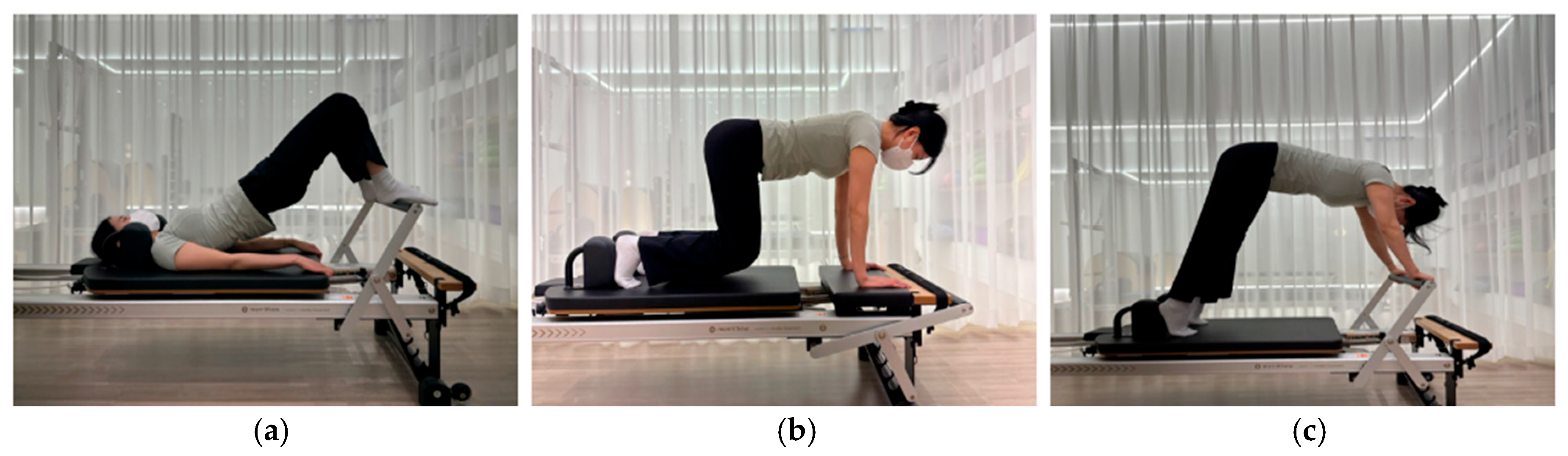
- Hip roll
- 2.
- Knee-off
- 3.
- Elephant
2.3. Electromyography (EMG)
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core Stability Exercise Principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Joyce, A.A.; Kotler, D.H. Core Training in Low Back Disorders: Role of the Pilates Method. Curr. Sports Med. Rep. 2017, 16, 156–161. [Google Scholar] [CrossRef]
- Cabrejas, C.; Solana-Tramunt, M.; Morales, J.; Nieto, A.; Bofill, A.; Carballeira, E.; Pierantozzi, E. The Effects of an Eight-Week Integrated Functional Core and Plyometric Training Program on Young Rhythmic Gymnasts’ Explosive Strength. Int. J. Environ. Res. Public Health 2023, 20, 1041. [Google Scholar] [CrossRef]
- Owen, P.J.; Miller, C.T.; Mundell, N.L.; Verswijveren, S.J.J.M.; Tagliaferri, S.D.; Brisby, H.; Bowe, S.J.; Belavy, D.L. Which Specific Modes of Exercise Training Are Most Effective for Treating Low Back Pain? Network Meta-Analysis. Br. J. Sports Med. 2020, 54, 1279–1287. [Google Scholar] [CrossRef]
- Lee, K. The Relationship of Trunk Muscle Activation and Core Stability: A Biomechanical Analysis of Pilates-Based Stabilization Exercise. Int. J. Environ. Res. Public Health 2021, 18, 12804. [Google Scholar] [CrossRef]
- Donatoni da Silva, L.; Shiel, A.; Sheahan, J.; McIntosh, C. Six Weeks of Pilates Improved Functional Mobility, Postural Balance and Spatiotemporal Parameters of Gait to Decrease the Risk of Falls in Healthy Older Adults. J. Bodyw. Mov. Ther. 2022, 29, 1–9. [Google Scholar] [CrossRef]
- Muscolino, J.E.; Cipriani, S. Pilates and the “Powerhouse”—I. J. Bodyw. Mov. Ther. 2004, 8, 15–24. [Google Scholar] [CrossRef]
- Queiroz, B.C.; Cagliari, M.F.; Amorim, C.F.; Sacco, I.C. Muscle Activation During Four Pilates Core Stability Exercises in Quadruped Position. Arch. Phys. Med. Rehabil. 2010, 91, 86–92. [Google Scholar] [CrossRef]
- Batıbay, S.; Külcü, D.G.; Kaleoğlu, Ö.; Mesci, N. Effect of Pilates Mat Exercise and Home Exercise Programs on Pain, Functional Level, and Core Muscle Thickness in Women with Chronic Low Back Pain. J. Orthop. Sci. 2021, 26, 979–985. [Google Scholar] [CrossRef]
- Cruz-Díaz, D.; Romeu, M.; Velasco-González, C.; Martínez-Amat, A.; Hita-Contreras, F. The Effectiveness of 12 Weeks of Pilates Intervention on Disability, Pain and Kinesiophobia in Patients with Chronic Low Back Pain: A Randomized Controlled Trial. Clin. Rehabil. 2018, 32, 1249–1257. [Google Scholar] [CrossRef]
- Patti, A.; Thornton, J.S.; Giustino, V.; Drid, P.; Paoli, A.; Schulz, J.M.; Palma, A.; Bianco, A. Effectiveness of Pilates Exercise on Low Back Pain: A Systematic Review with Meta-Analysis. Disabil. Rehabil. 2024, 46, 3535–3548. [Google Scholar] [CrossRef] [PubMed]
- Rangabprai, Y.; Mitranun, W.; Mitarnun, W. Effect of 60-Min Single Bout of Resistance Exercise, Reformer Pilates, on Vascular Function Parameters in Older Adults: A Randomized Crossover Study. Gerontology 2024, 70, 764–775. [Google Scholar] [CrossRef]
- Gou, Y.; Lei, H.; Zeng, Y.; Tao, J.; Kong, W.; Wu, J. The Effect of Pilates Exercise Training for Scoliosis on Improving Spinal Deformity and Quality of Life: Meta-Analysis of Randomized Controlled Trials. Medicine 2021, 100, E27254. [Google Scholar] [CrossRef]
- Lee, K. Motion Analysis of Core Stabilization Exercise in Women: Kinematics and Electromyographic Analysis. Sports 2023, 11, 66. [Google Scholar] [CrossRef]
- Anderson, B.D.; Spector, A. Introduction to Pilates-Based Rehabilitation. Orthop. Phys. Ther. Clin. N. Am. 2020, 9, 395–410. [Google Scholar]
- Johnson, E.G.; Larsen, A.; Ozawa, H.; Wilson, C.A.; Kennedy, K.L. The Effects of Pilates-Based Exercise on Dynamic Balance in Healthy Adults. J. Bodyw. Mov. Ther. 2007, 11, 238–242. [Google Scholar] [CrossRef]
- Evans, B. Anatomy of a Reformer: What to Look for in This Classic Piece of Pilates Equipment. IDEA Health Fit. Source 2003, 21, 28–32. [Google Scholar]
- Endleman, I.; Critchley, D.J. Transversus Abdominis and Obliquus Internus Activity During Pilates Exercises: Measurement With Ultrasound Scanning. Arch. Phys. Med. Rehabil. 2008, 89, 2205–2212. [Google Scholar] [CrossRef]
- Anderson, K.; Behm, D.G. The Impact of Instability Resistance Training on Balance and Stability. Sports Med. 2005, 35, 43–53. [Google Scholar] [CrossRef]
- Panhan, A.C.; Gonçalves, M.; Eltz, G.D.; Villalba, M.M.; Cardozo, A.C.; Bérzin, F. Electromyographic Evaluation of Trunk Core Muscles during Pilates Exercise on Different Supporting Bases. J. Bodyw. Mov. Ther. 2019, 23, 855–859. [Google Scholar] [CrossRef]
- Nouillot, P.; Bouisset, S.; Do, M.C. Do Fast Voluntary Movements Necessitate Anticipatory Postural Adjustments Even If Equilibrium Is Unstable? Neurosci. Lett. 1992, 147, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Latey, P. The Pilates Method: History and Philosophy. J. Bodyw. Mov. Ther. 2001, 5, 275–282. [Google Scholar] [CrossRef]
- Danneels, L.A.; Vanderstraeten, G.G.; Cambier, D.C.; Witvrouw, E.E.; Stevens, V.K.; De Cuyper, H.J. A Functional Subdivision of Hip, Abdominal, and Back Muscles during Asymmetric Lifting. Spine 2001, 26, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Stevens, V.K.; Bouche, K.G.; Mahieu, N.N.; Coorevits, P.L.; Vanderstraeten, G.G.; Danneels, L.A. Trunk Muscle Activity in Healthy Subjects during Bridging Stabilization Exercises. BMC Musculoskelet. Disord. 2006, 7, 75. [Google Scholar] [CrossRef]
- Richardson, C. EMG Study of Erector Spinae and Multifidus in Two Isometric Back Extension Exercises. Aust. J. Physiother. 1994, 40, 115–121. [Google Scholar] [CrossRef]
- Hall, M.; Stevermer, C.A.; Gillette, J.C. Muscle Activity Amplitudes and Co-Contraction during Stair Ambulation Following Anterior Cruciate Ligament Reconstruction. J. Electromyogr. Kinesiol. 2015, 25, 298–304. [Google Scholar] [CrossRef]
- Merrithew™. Spring Resistance Chart. Available online: https://www.merrithew.com/docs/default-source/distributors---customer-service/spring-resistance-chart (accessed on 4 December 2024).
- Tsartsapakis, I.; Gerou, M.; Zafeiroudi, A.; Kellis, E. Transversus Abdominis Ultrasound Thickness during Popular Trunk–Pilates Exercises in Young and Middle-Aged Women. J. Funct. Morphol. Kinesiol. 2023, 8, 110. [Google Scholar] [CrossRef]
- Geweniger, V.; Bohlander, A. Therapeutic Pilates: Applications. In Pilates—A Teachers’ Manual; Springer: Berlin/Heidelberg, Germany, 2014; pp. 211–264. [Google Scholar] [CrossRef]
- Kong, Y.S.; Park, S.; Kweon, M.G.; Park, J.W. Change in Trunk Muscle Activities with Prone Bridge Exercise in Patients with chronic Low Back Pain. J. Phys. Ther. Sci. 2016, 28, 264. [Google Scholar] [CrossRef][Green Version]
- Czaprowski, D.; Afeltowicz, A.; Gebicka, A.; Pawłowska, P.; Kedra, A.; Barrios, C.; Hadała, M. Abdominal Muscle EMG-Activity during Bridge Exercises on Stable and Unstable Surfaces. Phys. Ther. Sport 2014, 15, 162–168. [Google Scholar] [CrossRef]
- Agostini, V.; Ghislieri, M.; Rosati, S.; Balestra, G.; Knaflitz, M. Surface Electromyography Applied to Gait Analysis: How to Improve Its Impact in Clinics? Front. Neurol. 2020, 11, 994. [Google Scholar] [CrossRef]
- Hermens, H.J.; Freriks, B.; Merletti, R.; Stegeman, D.; Blok, J.; Rau, G.; Disselhorst-Klug, C.; Hägg, G. European Recommendations for Surface ElectroMyoGraphy Results of the SENIAM Project. Roessingh Res. Dev. 1999, 8, 13–54. [Google Scholar]
- Burden, A.; Bartlett, R. Normalisation of EMG Amplitude: An Evaluation and Comparison of Old and New Methods. Med. Eng. Phys. 1999, 21, 247–257. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Routledge: London, UK, 2013. [Google Scholar] [CrossRef]
- Tomczak, M.; Tomczak, E. The Need to Report Effect Size Estimates Revisited. An Overview of Some Recommended Measures of Effect Size. Trends Sport Sci. 2014, 1, 19–25. [Google Scholar]
- Andersson, E.A.; Ma, Z.; Thorstensson, A. Relative EMG Levels in Training Exercises for Abdominal and Hip Flexor Muscles. Scand J. Rehabil. Med. 1998, 30, 175–183. [Google Scholar] [CrossRef]
- Vezina, M.J.; Hubley-Kozey, C.L. Muscle Activation in Therapeutic Exercises to Improve Trunk Stability. Arch. Phys. Med. Rehabil. 2000, 81, 1370–1379. [Google Scholar] [CrossRef]
- Souza, G.M.; Baker, L.L.; Powers, C.M. Electromyographic Activity of Selected Trunk Muscles during Dynamic Spine Stabilization Exercises. Arch. Phys. Med. Rehabil. 2001, 82, 1551–1557. [Google Scholar] [CrossRef]
- de Oliveira, N.T.B.; Freitas, S.M.S.F.; Fuhro, F.F.; da Luz, M.A.; Amorim, C.F.; Cabral, C.M.N. Muscle Activation During Pilates Exercises in Participants with Chronic Nonspecific Low Back Pain: A Cross-Sectional Case-Control Study. Arch. Phys. Med. Rehabil. 2017, 98, 88–95. [Google Scholar] [CrossRef]
- Marshall, P.; Murphy, B. The Validity and Reliability of Surface EMG to Assess the Neuromuscular Response of the Abdominal Muscles to Rapid Limb Movement. J. Electromyogr. Kinesiol. 2003, 13, 477–489. [Google Scholar] [CrossRef]
- Vera-Garcia, F.J.; Grenier, S.G.; McGill, S.M. Abdominal Muscle Response During Curl-Ups on Both Stable and Labile Surfaces. Phys. Ther. 2000, 80, 564–569. [Google Scholar] [CrossRef]
- Lehman, G.J.; Hoda, W.; Oliver, S. Trunk Muscle Activity during Bridging Exercises on and off a Swissball. Chiropr. Osteopat. 2005, 13, 14. [Google Scholar] [CrossRef]
- Dondelinger, R. Electromyography—An Overview. Biomed. Instrum. Technol. 2010, 44, 128–131. [Google Scholar] [CrossRef] [PubMed]


| Muscle | Attachment Sites |
|---|---|
| Rectus abdominis | 2 cm lateral and 2 cm superior to the umbilicus |
| Internal obliques | 2 cm medial and inferior to the anterior superior iliac spine |
| Erector spinae | 2 cm lateral to the spinous process of L1 |
| Multifidus | 3 cm lateral to the midpoint between the spinous processes of L1 and L5 |
| Rectus femoris | Midway between the ASIS and the superior aspect of the knee |
| Biceps femoris | Midway between the ischium and the lateral epicondyle of the fibula |
| Fixed | Moderate | Low | Main Effect | ||
|---|---|---|---|---|---|
| % MVIC | % MVIC | % MVIC | p-Value | Effect Size (η2) | |
| RA | 5.4 (3.3) | 6.3 (3.5) a | 6.9 (2.8) a | p = 0.002 | 0.039 |
| IO | 19.1 (13.2) | 19.6 (16.5) | 18.3 (12.7) | p = 0.64 | 0.002 |
| ES | 6.9 (3.0) | 8.5 (3.5) a | 10.6 (4.5) a,b | p < 0.001 * | 0.790 * |
| MU | 8.9 (7.6) | 11.1 (9.5) a | 13.7 (11.1) a,b | p < 0.001 * | 0.651 * |
| RF | 2.5 (0.9) | 2.9 (0.9) a | 3.4 (1.1) a,b | p < 0.001 | 0.139 |
| BF | 6.9 (3.3) | 11.6 (4.9) a | 16.4 (6.7) a,b | p < 0.001 | 0.371 |
| Fixed | Moderate | Low | Main Effect | ||
|---|---|---|---|---|---|
| % MVIC | % MVIC | % MVIC | p-Value | Effect Size (η2) | |
| RA | 11.2 (5.6) | 13.9 (5.6) a | 18.1 (7.0) a,b | p < 0.001 | 0.188 |
| IO | 17.9 (8.0) | 17.7 (7.7) | 21.0 (9.4) a | p = 0.004 | 0.032 |
| ES | 2.7 (1.1) | 3.0 (1.2) | 3.3 (1.3) a | p = 0.005 | 0.033 |
| MU | 5.8 (8.4) | 6.5 (8.8) a | 7.2 (9.6) a,b | p < 0.001 * | 0.481 * |
| RF | 14.1 (6.7) | 15.0 (6.5) | 16.2 (9.8) | p = 0.183 | 0.012 |
| BF | 2.2 (1.2) | 2.4 (1.5) | 2.4 (1.4) | p = 0.092 * | 0.133 * |
| Fixed | Moderate | Low | Main Effect | ||
|---|---|---|---|---|---|
| % MVIC | % MVIC | % MVIC | p-Value | Main Effect (η2) | |
| RA | 7.5 (4.8) | 14.4 (7.7) a | 24.6 (13.3) a,b | p < 0.001 | 0.377 |
| IO | 16.2 (9.0) | 23.1 (11.2) a | 26.9 (11.6) a | p < 0.001 | 0.154 |
| ES | 3.3 (1.6) | 3.1 (1.6) | 3.5 (1.3) b | p = 0.024 * | 0.207 * |
| MU | 5.6 (5.2) | 5.7 (7.2) | 6.8 (7.7) b | p = 0.006 * | 0.281 * |
| RF | 8.0 (5.4) | 12.3 (6.2) a | 16.0 (8.0) a,b | p < 0.001 | 0.206 |
| BF | 2.9 (1.9) | 2.9 (1.9) | 3.3 (1.9) | p = 0.412 | 0.010 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.-J.; Sung, J.-H.; Ryu, J.-K.; Jung, H.-C.; Wang, J. Effect of Reformer Spring Resistance Modifications on Core Muscle Activity During Basic Core Muscle Exercises. Healthcare 2024, 12, 2447. https://doi.org/10.3390/healthcare12232447
Kim H-J, Sung J-H, Ryu J-K, Jung H-C, Wang J. Effect of Reformer Spring Resistance Modifications on Core Muscle Activity During Basic Core Muscle Exercises. Healthcare. 2024; 12(23):2447. https://doi.org/10.3390/healthcare12232447
Chicago/Turabian StyleKim, Hee-Jeong, Jung-Ha Sung, Jae-Kyun Ryu, Hyun-Chul Jung, and Junsig Wang. 2024. "Effect of Reformer Spring Resistance Modifications on Core Muscle Activity During Basic Core Muscle Exercises" Healthcare 12, no. 23: 2447. https://doi.org/10.3390/healthcare12232447
APA StyleKim, H.-J., Sung, J.-H., Ryu, J.-K., Jung, H.-C., & Wang, J. (2024). Effect of Reformer Spring Resistance Modifications on Core Muscle Activity During Basic Core Muscle Exercises. Healthcare, 12(23), 2447. https://doi.org/10.3390/healthcare12232447






