A Solution to Reduce the Impact of Patients’ No-Show Behavior on Hospital Operating Costs: Artificial Intelligence-Based Appointment System
Abstract
1. Introduction
2. Materials and Methods
2.1. Design
- The hospital appointment system and the factors affecting the effective operation of the appointment system were identified. Current literature and expert opinions were used to determine these factors.
- The patient characteristics determining the appointment no-show behavior were identified. Data analytics was used to determine these characteristics, and patient-specific behavioral models were created from the data patterns.
- Within the framework of the findings from the first and second stages, the AI-BAS model, based on actual data, was developed and tested in a university hospital and the application performance results were presented.
- The findings were discussed within the framework of the relevant literature.
2.2. Setting
2.3. Data Sources and Structures
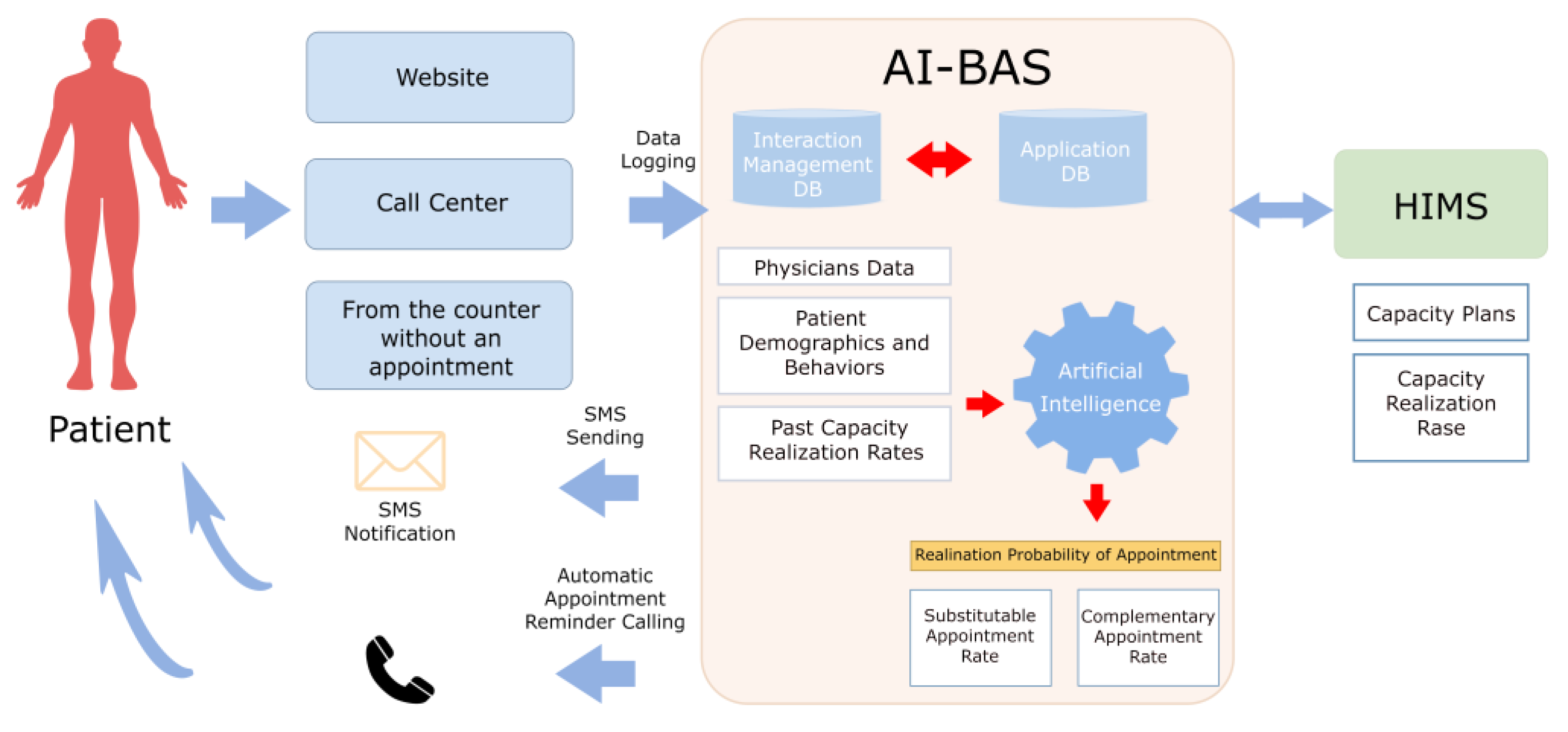
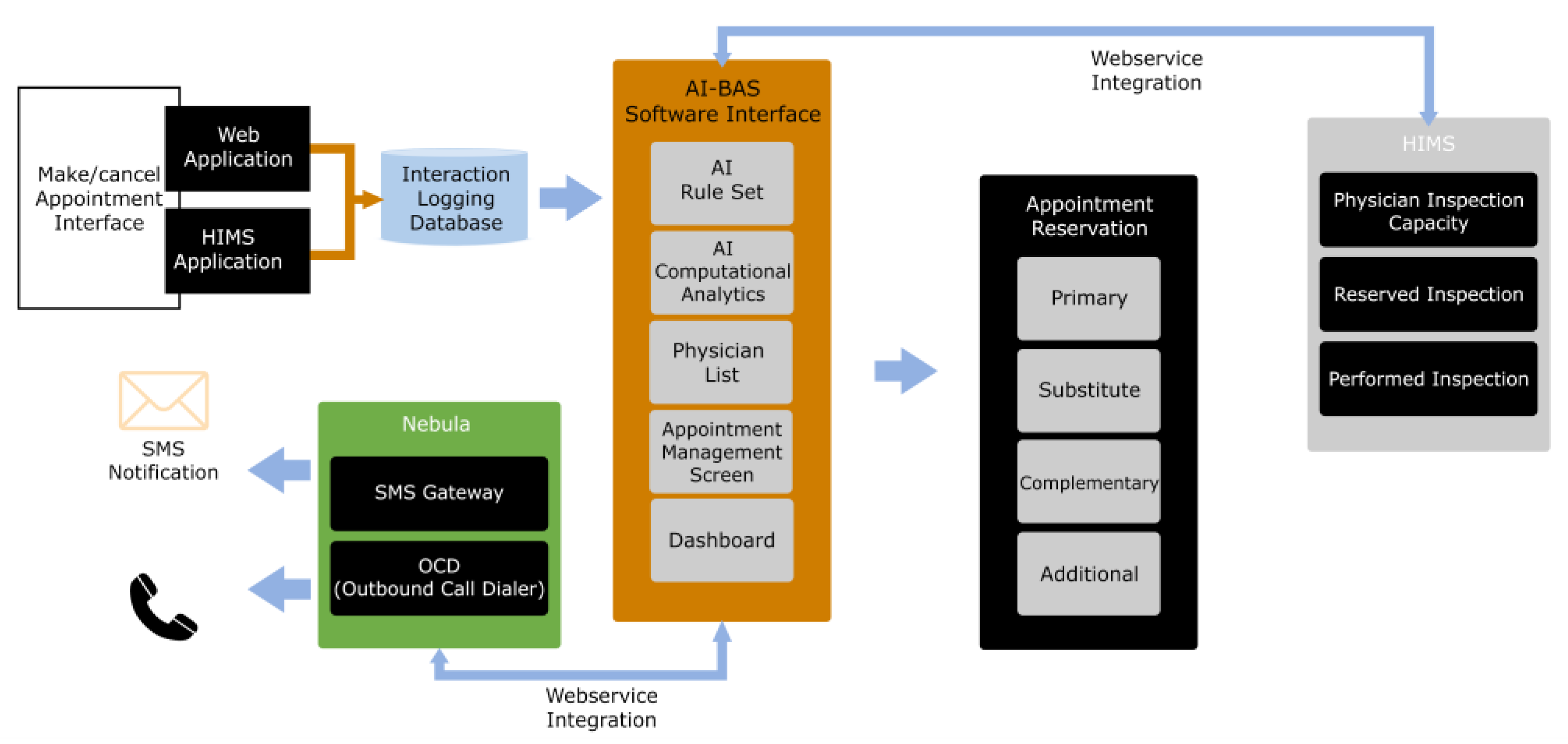
2.4. System Architecture
2.4.1. Data Layer
- Patients’ appointment history: Appointment date, appointment time, physician, branch, and appointment status (completed, canceled, and no-show).
- Patients’ demographic information: Age, gender, and address.
2.4.2. Data Processing Layer
- Data cleaning and pre-processing: Correcting missing or inconsistent data and making it ready for processing.
- Feature engineering: Creating new features from data that will improve the performance of the prediction model.
- Data normalization: Normalizing the data to prevent it from being at different scales.
2.4.3. Data Science
- Appointment Cancellation and No-Show Prediction Model: This model predicts the probability of patients canceling or not showing up for appointments, determines the number of reserve patients accordingly, and opens this pool to reservations.
- Model training: Teaching daily, monthly, and annual data to the instant prediction algorithm.
- Model selection: Extracting the features of canceled and no-show appointments using regression analysis and decision tree methods. Regression analysis is convenient for estimating no-show probabilities by modeling the relationships between dependent and independent variables. Common socio-demographic and clinical characteristics may be shared between patient groups. This increases the relatability among patients who have appointments with the same healthcare provider. For example, patients in the same clinic may exhibit similar no-show behaviors because these patients usually have similar socioeconomic conditions and demographic characteristics. Naturally, this clustered structure should be considered in statistical analysis. Ignoring such dependencies may lead to biased variance estimation and erroneous results. Therefore, it is desirable to consider the semi-parametric regression analysis of clustered panel count data [18]. Decision trees are supervised learning models constructing a series of if-else questions to classify or predict outcomes based on input features. The decision tree model was chosen for its high interpretability and ability to handle complex, nonlinear interactions between variables such as demographics and past appointment behaviors. This method has proven effective in healthcare prediction tasks because it provides clear decision paths that make it easy for healthcare professionals to understand the logic behind each prediction. Also, the decision tree strikes a fundamental balance between accuracy and interoperability. This balance is crucial in environments where actionable insights are needed in real time to manage appointment scheduling efficiently. These two methods are based on the information gain principle, which improves the model’s performance and obtains the best results. Information gain is a metric often used in machine learning algorithms, especially decision trees. It measures how much new information is provided when a dataset is split based on a specific feature. In other words, it is a quantitative indicator of how well a feature can predict the target variable. This calculation starts by measuring the uncertainty (entropy) in the dataset. Entropy indicates how homogeneous the distribution of classes is in the dataset. Then, the dataset is split into subsets according to the selected feature, and the entropy of each subgroup is calculated. Information gain is obtained by subtracting the weighted average entropy of the subsets from the initial total entropy. This difference expresses the success of the selected feature in distinguishing classes in the dataset. For example, if patient age significantly predicts no-show behavior, the decision tree will split on this feature, leading to more homogeneous subgroups with higher prediction accuracy.
2.4.4. Decision-Making Layer
- Determining the number of backup appointments needed for canceled appointments and patients unable to attend: The estimation algorithm’s results determine the number of backup appointments, which are automatically assigned through the website where patients apply for appointments.
- Creating a complementary appointment: The estimation model is instrumental in this step, as it guides the creation of complementary appointments to minimize the possibility of cancellations or no-shows.
- Optimizing appointment planning: Optimizing appointment planning by considering current and complementary appointments. Accordingly, appointment slot quotas in the relevant branches are determined.
2.4.5. Presentation Layer
- User interface: A website appointment management screen has been developed to allow hospitals and patients to use the system and manage appointments. In addition, the system operates entirely in the background and is only accountable to the chief physician and information technology team. The system analyzes the data of three hospital systems (the HIMS, appointment website, and callback reminder search system), and the estimation algorithm works automatically and does not allow manual intervention. Therefore, the system is managed by a single administrator.
2.4.6. Integration Layer
- Hospital information system integration: We have established direct integration with the HIMS application and website, ensuring seamless compatibility. The web service and the instantaneous movements of the data are monitored by the estimation algorithm.
2.5. Plot Study
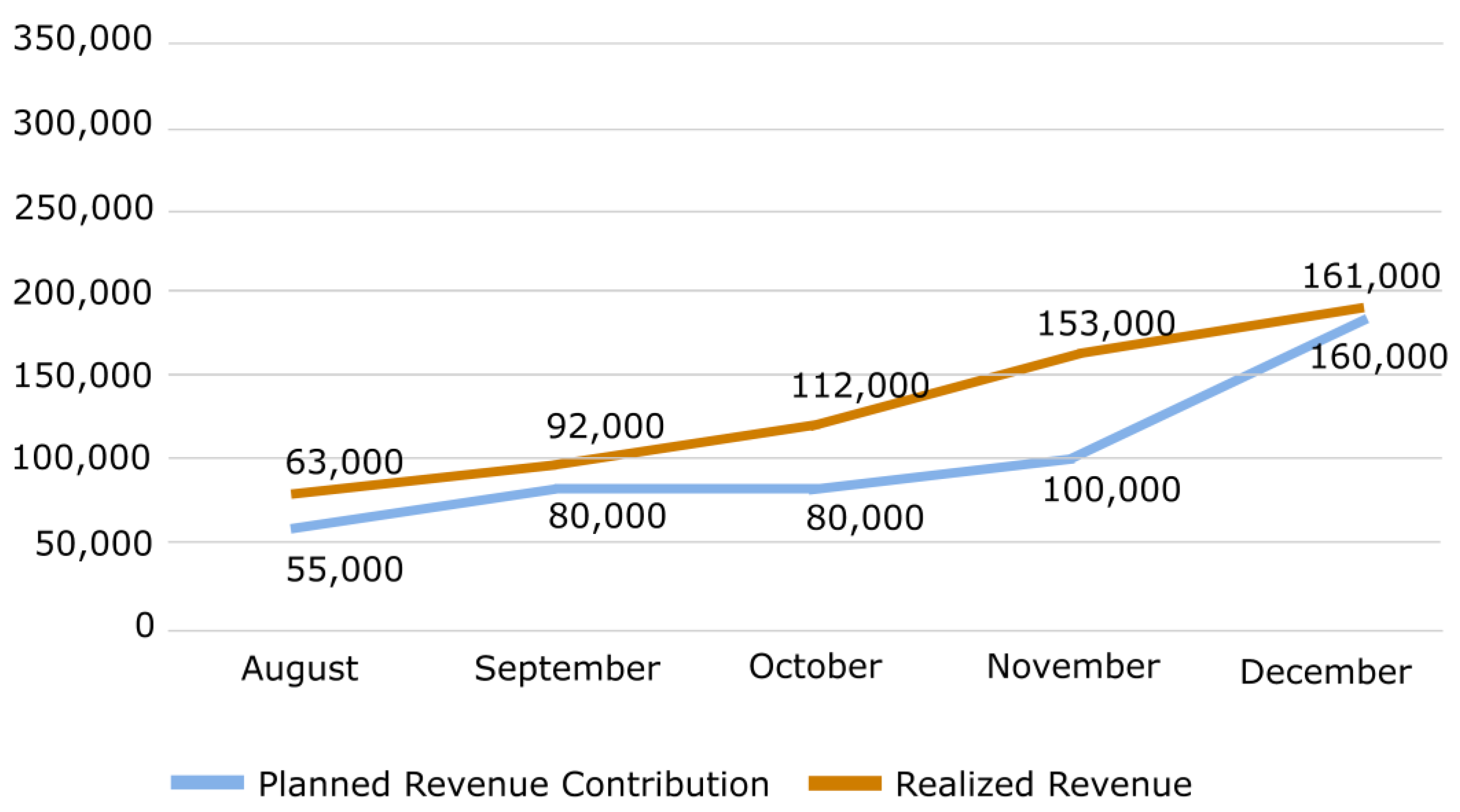
3. Results
4. Discussion
Limitations and Recommendations for Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tang, J.; Yan, C.; Fung, R.Y. Optimal appointment scheduling with no-shows and exponential service time considering overtime work. J. Manag. Anal. 2014, 1, 99–129. [Google Scholar] [CrossRef]
- Leeftink, G.; Martinez, G.; Hans, E.W.; Sir, M.Y.; Pasupathy, K.S. Optimising the booking horizon in healthcare clinics considering no-shows and cancellations. Int. J. Prod. Res. 2022, 60, 3201–3218. [Google Scholar] [CrossRef]
- Bhattacharjee, P.; Ray, P.K. Simulation modelling and analysis of appointment system performance for multiple classes of patients in a hospital: A case study. Oper. Res. Health Care 2016, 8, 71–84. [Google Scholar] [CrossRef]
- Hu, M.; Xu, X.; Li, X.; Che, T. Managing patients’ no-show behaviour to improve the sustainability of hospital appointment systems: Exploring the conscious and unconscious determinants of no-show behaviour. J. Clean. Prod. 2020, 269, 122318. [Google Scholar] [CrossRef]
- Salazar, L.H.A.; Leithardt, V.R.; Parreira, W.D.; da Rocha Fernandes, A.M.; Barbosa, J.L.V.; Correia, S.D. Application of machine learning techniques to predict a patient’s no-show in the healthcare sector. Future Internet 2021, 14, 3. [Google Scholar] [CrossRef]
- Chua, S.L.; Chow, W.L. Development of predictive scoring model for risk stratification of no-show at a public hospital specialist outpatient clinic. Proc. Singap. Healthc. 2019, 28, 96–104. [Google Scholar] [CrossRef]
- Lenzi, H.; Ben, Â.J.; Stein, A.T. Development and validation of a patient no-show predictive model at a primary care setting in Southern Brazil. PLoS ONE 2019, 14, e0214869. [Google Scholar] [CrossRef]
- da Silva, R.B.Z.; Fogliatto, F.S.; Garcia, T.S.; Faccin, C.S.; Zavala, A.A.Z. Modelling the no-show of patients to exam appointments of computed tomography. Int. J. Health Plan. Manag. 2022, 37, 2889–2904. [Google Scholar] [CrossRef]
- Dantas, L.F.; Fleck, J.L.; Oliveira, F.L.C.; Hamacher, S. No-shows in appointment scheduling—A systematic literature review. Health Policy 2018, 122, 412–421. [Google Scholar] [CrossRef]
- Huang, Y.; Zuniga, P. Effective cancellation policy to reduce the negative impact of patient no-show. J. Oper. Res. Soc. 2014, 65, 605–615. [Google Scholar] [CrossRef]
- Ellis, D.A.; Jenkins, R. Weekday affects attendance rate for medical appointments: Large-scale data analysis and implications. PLoS ONE 2012, 7, e51365. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.; Millard, A.; McCartney, G.; McCullough, S. ‘Who Is Least Likely to Attend? An Analysis of Outpatient Appointment “Did Not Attend” (DNA) Data in Scotland.’, NHS Health Scotland. March, 2015. pp. 1–37. Available online: http://www.healthscotland.scot/publications/who-is-least-likely-to-attend-an-analysis-of-outpatient-appointment-did-not-attend-dna-data-in-scotland (accessed on 16 February 2024).
- Kheirkhah, P.; Feng, Q.; Travis, L.M.; Tavakoli-Tabasi, S.; Sharafkhaneh, A. Prevalence, predictors and economic consequences of no-shows. BMC Health Serv. Res. 2016, 16, 13. [Google Scholar] [CrossRef] [PubMed]
- Klassen, K.J.; Yoogalingam, R. Strategies for appointment policy design with patient unpunctuality. Decis. Sci. 2014, 45, 881–911. [Google Scholar] [CrossRef]
- Elkhider, H.; Sharma, R.; Sheng, S.; Thostenson, J.; Kapoor, N.; Veerapaneni, P.; Siddamreddy, S.; Ibrahim, F.; Yadala, S.; Onteddu, S.; et al. Predictors of no-show in neurology clinics. Healthcare 2022, 10, 599. [Google Scholar] [CrossRef]
- Xu, X.; Hu, M.; Li, X. Coping with no-show behaviour in appointment services: A multistage perspective. J. Serv. Theory Pract. 2022, 32, 452–474. [Google Scholar] [CrossRef]
- Huang, Y.L.; Hanauer, D.A. Time dependent patient no-show predictive modelling development. Int. J. Health Care Qual. Assur. 2016, 29, 475–488. [Google Scholar] [CrossRef]
- Wang, W.; Cui, Z.; Chen, R.; Wang, Y.; Zhao, X. Regression analysis of clustered panel count data with additive mean models. Stat. Pap. 2024, 65, 2915–2936. [Google Scholar] [CrossRef]
- Xiao, F.; Lai, K.K.; Lau, C.K.; Ram, B. Robust Overbooking for no-shows and cancellations in healthcare. Mathematics 2024, 12, 2563. [Google Scholar] [CrossRef]
- Hekler, E.; Tiro, J.A.; Hunter, C.M.; Nebeker, C. Precision health: The role of the social and behavioral sciences in advancing the vision. Ann. Behav. Med. 2020, 54, 805–826. [Google Scholar] [CrossRef]
- Khun, M.; Johnson, K. Applied Predictive Modeling; Springer: New York, NY, USA, 2013. [Google Scholar] [CrossRef]
- Zhu, H.; Chen, Y.; Leung, E.; Liu, X. Outpatient appointment scheduling with unpunctual patients. Int. J. Prod. Res. 2018, 56, 1982–2002. [Google Scholar] [CrossRef]
- Ferro, D.B.; Brailsford, S.; Bravo, C.; Smith, H. Improving healthcare access management by predicting patient no-show behaviour. Decis. Support Syst. 2020, 138, 113398. [Google Scholar] [CrossRef]
- Davies, M.L.; Goffman, R.M.; May, J.H.; Monte, R.J.; Rodriguez, K.L.; Tjader, Y.C.; Vargas, D.L. Large-scale no-show patterns and distributions for clinic operational research. Healthcare 2016, 4, 15. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Wan, Y.; Tu, H.; Shang, F.; Liu, D.; Tan, Z.; Sun, C.; Ye, Q.; Xu, Y. A web-based appointment system to reduce waiting for outpatients: A retrospective study. BMC Health Serv. Res. 2011, 11, 318. [Google Scholar] [CrossRef]
- Jerbi, B.; Kamoun, H. Multiobjective study to implement outpatient appointment system at Hedi Chaker Hospital. Simul. Model. Pract. Theory 2011, 19, 1363–1370. [Google Scholar] [CrossRef]
- Woicik, K.; Van der Lem, R.; Sijtsema, J.J.; Bogaerts, S. Treatment no-show in forensic outpatients with ADHD. Crim. Behav. Ment. Health 2017, 27, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Denton, B. Appointment scheduling in health care: Challenges and opportunities. IIE Trans. 2008, 40, 800–819. [Google Scholar] [CrossRef]
- Atalan, A.; Dönmez, C.Ç. Dynamic price application to prevent financial losses to hospitals based on machine learning algorithms. Healthcare 2024, 12, 1272. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, P.; Ray, P.K. Patient flow modelling and performance analysis of healthcare delivery processes in hospitals: A review and reflections. Comput. Ind. Eng. 2014, 78, 299–312. [Google Scholar] [CrossRef]
- Yang, P.C.; Chu, F.Y.; Liu, H.Y.; Shih, M.J.; Chen, T.J.; Chou, L.F.; Hwang, S.J. Features of online hospital appointment systems in Taiwan: A nationwide survey. Int. J. Environ. Res. Public Health 2019, 16, 171. [Google Scholar] [CrossRef]
- Küçük, A.; Demirci, M.; Kerman, G.; Özsoy, V.S. Evaluating of hospital appointment systems in Turkey: Challenges and opportunities. Health Policy Technol. 2021, 10, 69–74. [Google Scholar] [CrossRef]
- Toker, K.; Pinar, R.İ. The mediating role effect of internal integration between long term relationship with suppliers and customers and business performance in Turkey ici 500 enterprises. Braz. J. Oper. Prod. Manag. 2019, 16, 592–604. [Google Scholar] [CrossRef]
- Safdar, K.A.; Emrouznejad, A.; Dey, P.K. An optimized queue management system to improve patient flow in the absence of appointment system. Int. J. Health Care Qual. Assur. 2020, 33, 477–494. [Google Scholar] [CrossRef] [PubMed]

| Months | June (Before AI-BAS) | July (Pilot) | August | September | October | November | December | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parameters | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| The number of Web Appoint. | 92,527 | 100 | 62,110 | 100 | 77,389 | 100 | 78,696 | 100 | 75,324 | 100 | 81,966 | 100 | 80,481 | 100 |
| Realized Web Appoint. | 52,846 | 57.1 | 36,008 | 58.0 | 44,307 | 57.3 | 45,789 | 58.2 | 43,513 | 57.8 | 46,748 | 57.0 | 45,170 | 56.1 |
| Web Cancel Appoint. | 29,227 | 31.6 | 18,605 | 30.0 | 23,341 | 30.2 | 23,043 | 29.3 | 22,544 | 29.9 | 26,321 | 32.1 | 25,797 | 32.1 |
| Web No-Show | 10,454 | 11.3 | 7497 | 12.1 | 9741 | 12.6 | 9864 | 12.5 | 9267 | 12.3 | 8897 | 10.9 | 9514 | 11.8 |
| Realized AI-BAS | 859 | 1.3 | 2934 | 3.7 | 4683 | 6.0 | 4556 | 6.1 | 5430 | 6.59 | 5800 | 7.3 | ||
| Realized Web + AI-BAS | 36,867 | 59.2 | 47,241 | 61 | 50,472 | 64.2 | 48,069 | 63.8 | 52,178 | 63.6 | 50,970 | 63.4 | ||
| The ratio of AI-BAS-Realization to Web Realization | 2.2 | 6.5 | 10.4 | 10.5 | 11.6 | 12.9 | ||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Toker, K.; Ataş, K.; Mayadağlı, A.; Görmezoğlu, Z.; Tuncay, I.; Kazancıoğlu, R. A Solution to Reduce the Impact of Patients’ No-Show Behavior on Hospital Operating Costs: Artificial Intelligence-Based Appointment System. Healthcare 2024, 12, 2161. https://doi.org/10.3390/healthcare12212161
Toker K, Ataş K, Mayadağlı A, Görmezoğlu Z, Tuncay I, Kazancıoğlu R. A Solution to Reduce the Impact of Patients’ No-Show Behavior on Hospital Operating Costs: Artificial Intelligence-Based Appointment System. Healthcare. 2024; 12(21):2161. https://doi.org/10.3390/healthcare12212161
Chicago/Turabian StyleToker, Kerem, Kadir Ataş, Alpaslan Mayadağlı, Zeynep Görmezoğlu, Ibrahim Tuncay, and Rümeyza Kazancıoğlu. 2024. "A Solution to Reduce the Impact of Patients’ No-Show Behavior on Hospital Operating Costs: Artificial Intelligence-Based Appointment System" Healthcare 12, no. 21: 2161. https://doi.org/10.3390/healthcare12212161
APA StyleToker, K., Ataş, K., Mayadağlı, A., Görmezoğlu, Z., Tuncay, I., & Kazancıoğlu, R. (2024). A Solution to Reduce the Impact of Patients’ No-Show Behavior on Hospital Operating Costs: Artificial Intelligence-Based Appointment System. Healthcare, 12(21), 2161. https://doi.org/10.3390/healthcare12212161






