Cross-Sectional and Descriptive Study on the Challenges and Awareness of Hispanic Parents Regarding Their Adolescents’ Mental Health during the COVID-19 Pandemic
Abstract
1. Introduction
- What were the predominant mood states of Hispanic adolescents during the COVID-19 pandemic?
- Has there been a change in these adolescents’ mood states since the pandemic?
- How did Hispanic parents perceive their adolescents’ mood states during the COVID-19 pandemic?
- Have they noticed any changes in their adolescents’ mood since the pandemic?
- Is there a difference in parents’ perceptions of their adolescents’ recent mood states compared with their perceptions during the pandemic?
2. Methods
2.1. Samples and Procedure
2.2. Measures
2.3. Plan of Analysis
3. Results
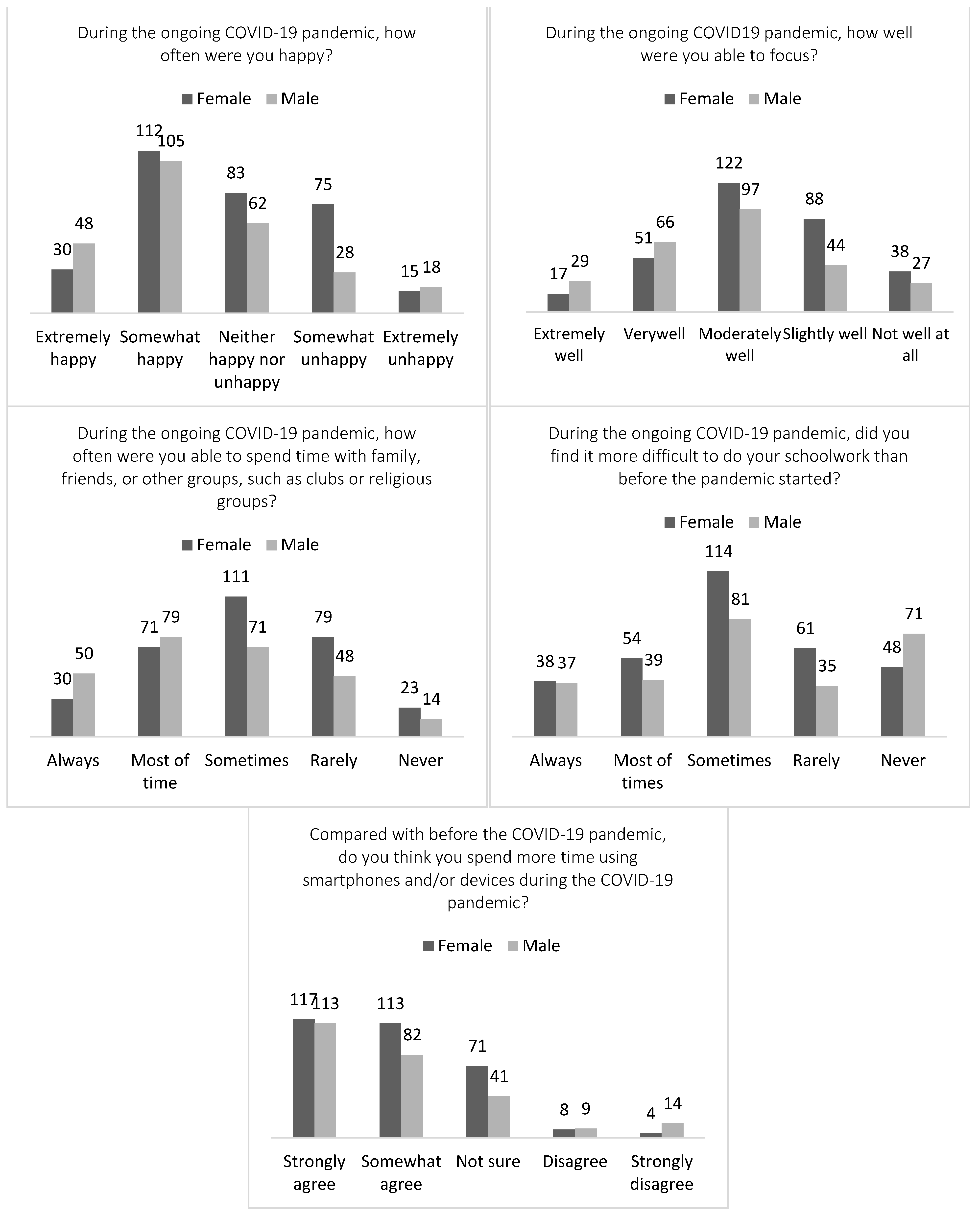
3.1. Adolescents’ Perception about Mood States Related to COVID-19
3.2. Parental Awareness of Adolescents’ Mood States
3.3. Factors Associated with Adolescents’ Mood Change
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. COVID-19 Related Mental Health State Survey (Adolescent Form)
- What grade are you in? _____
- Gender? Female/Male
- Please specify your race. White, Black, Hispanic, Asian, Other______
- During the ongoing COVID-19, how worried were you generally? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19, how happy were you generally? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19, how lonely were you? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19, have you cried often? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19, how well were you able to focus? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19, how easily angered were you? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19 pandemic, did you find it more difficult to do your schoolwork than before the pandemic started? Never; Rarely; Sometimes; Most of time; Always
- Compared to the ongoing COVID-19 pandemic and now, how would you say you feel now? Much worse now; Slightly worse now; About the same; Slightly better now; Much better now
- During the ongoing COVID-19 pandemic, how often were you able to spend time with family, friends, or other groups, such as clubs or religious groups? Never; Rarely; Sometimes; Most of time; Always
- Compared with before the COVID-19 pandemic, do you think you spend more time using smartphones and/or devices during the COVID-19 pandemic? Strongly disagree; Disagree; Not sure; Somewhat agree; strongly agree
- Do you often talk with your parents or caregivers about your feeling when you are sad or angry? Never; Rarely; Sometimes; Most of time; Always
- If you would like to get help about your mental health, do you know where to contact or who to talk with? No; Yes
Appendix B. COVID-19 Related Mental Health State Survey (Parent Form)
- What grades is your child in? _____
- Is your child in special education? Yes/No
- Is your child in the gifted program? Yes/No
- Please specify your race/ethnicity: European American; African American; Latino or Hispanic; Asian; Native American; Native Hawaiian or Pacific Islander; Two or More; Other/Unknown
- What language do you now speak and read the most often at home? English; Spanish; Other_______
- What is the highest level of education you have completed? Grades 1–6; Grades 7–9; High School Diploma; Associate Degree; Bachelor’s Degree; Master’s Degree; Professional Degree; Doctoral Degree; Other_______________
- Which of the following describes your current employment status since the ongoing COVID-19 outbreak? (Please select all that apply). Working full time (30 or more than hours per week); Working part-time (fewer than 30 h per week); Not working; Retired; Unemployed; Other________
- During the ongoing COVID-19 pandemic, how often was your child worried? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19 pandemic, how often was your child happy? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19 pandemic, how often was your child angry? Never; Rarely; Sometimes; Most of time; Always
- During the ongoing COVID-19 pandemic, has your child cried often? Never; Rarely; Sometimes; Most of time; Always
- Before and during the ongoing COVID-19 pandemic, do you agree that there has been an increase in your child’s sadness, worry, and depression? Strongly disagree; Disagree; Neutral; Agree; Strongly Agree
- During the ongoing COVID-19 pandemic, how lonely was your child? Never; Rarely; Sometimes; Most of time; Always
- Before and during the ongoing COVID-19 pandemic, did you see an increase in your child’s use of a smartphone/device or computer games? Not at all; Not very well; Fairly well; Very well; Always
- During the ongoing COVID-19 pandemic, approximately how many hours a day did your child spend using a smartphone/device or computer games? 0 h; 1–2 h; 3–4 h; 5+ h
- Before and during the ongoing COVID-19 pandemic, did your child tend to avoid activities that they enjoyed in the past? Not at all; Not very well; Fairly well; Very well; Always
- During the ongoing COVID-19 pandemic, how well was your child able to focus? Not at all; Not very well; Fairly well; Very well; Always
- During the ongoing COVID-19 pandemic, do you think your child found it more difficult to do schoolwork than before the pandemic started? Never; Rarely; Sometimes; Most of time; Always
- Compared to the ongoing COVID-19 pandemic and now, how would you say that your child feels now? Much worse now; Slightly worse now; About the same; Slightly better now; Much better now
- During the ongoing COVID-19 pandemic, how often were you able to spend time with your children, family, friends, or other groups, such as clubs or religious groups? Never; Rarely; Sometimes; Most of time; Always
- How stressful were the restrictions for you overall during the ongoing COVID-19 pandemic? Not at all; stressful Slightly; stressful Moderately; stressful Extremely
- How stressful was parenting during the ongoing COVID-19 pandemic? Not at all; stressful Slightly stressful; Moderately stressful; Extremely
- How stressful was the school closure for you during the ongoing COVID-19 pandemic? Not at all stressful; Slightly stressful; Moderately stressful; Extremely
- What were the most challenging things in parenting during the ongoing COVID-19 pandemic? Please select all that apply. Setting regular bedtimes and wakeups; Establishing a daily educational schedule; Taking online classes; Exercise and social contact; Leisure time considerations; Reducing my child’s anxiety of real-life concerns; Other_______________________
References
- Courtney, D.; Watson, P.; Battaglia, M.; Mulsant, B.H.; Szatmari, P. COVID-19 impacts on child and youth anxiety and depression: Challenges and opportunities. Can. J. Psychiatry 2020, 65, 688–691. [Google Scholar] [CrossRef]
- Holmes, E.A.; O’Connor, R.C.; Perry, V.H.; Tracey, I.; Wessely, S.; Arseneault, L.; Ballard, C.; Christensen, H.; Silver, R.C.; Everall, I.; et al. Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. Lancet Psychiatry 2020, 7, 547–560. [Google Scholar] [CrossRef]
- Lee, S.; Juon, H.S.; Martinez, G.; Hsu, C.E.; Robinson, E.S.; Bawa, J.; Ma, G.X. Model minority at risk: Expressed needs of mental health by Asian American young adults. J. Community Health 2009, 34, 144–152. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Gosch, A.; Rajmil, L.; Erhart, M.; Bruil, J.; Power, M.; Duer, W.; Auquier, P.; Cloetta, B.; Czemy, L.; et al. The KIDSCREEN-52 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Value Health 2008, 11, 645–658. [Google Scholar] [CrossRef]
- Fusar-Poli, P. Integrated mental health services for the developmental period (0 to 25 years): A critical review of the evidence. Front. Psychiatry 2019, 10, 355. [Google Scholar] [CrossRef]
- Elharake, J.A.; Akbar, F.; Malik, A.A.; Gilliam, W.; Omer, S.B. Mental health impact of COVID-19 among children and college students: A systematic review. Child Psychiatry Hum. Dev. 2022, 54, 913–925. [Google Scholar] [CrossRef]
- Xiang, Y.; Cipriani, A.; Teng, T.; Del Giovane, C.; Zhang, Y.; Weisz, J.R.; Li, X.; Cuijpers, P.; Liu, X.; Barth, J.; et al. Comparative efficacy and acceptability of psychotherapies for post-traumatic stress disorder in children and adolescents: A systematic review and network meta-analysis. BMJ Ment. Health 2021, 24, 153–160. [Google Scholar] [CrossRef]
- Powell, T.; Wegmann, K.M.; Backode, E. Coping and post-traumatic stress in children and adolescents after an acute onset disaster: A systematic review. Int. J. Environ. Res. Public Health 2021, 18, 4865. [Google Scholar] [CrossRef]
- Selçuk, E.B.; Demir, A.Ç.; Erbay, L.G.; Özcan, Ö.Ö.; Gürer, H.; Dönmez, Y.E. Anxiety, depression and post-traumatic stress disorder symptoms in adolescents during the COVID-19 outbreak and associated factors. Int. J. Clin. Pract. 2021, 75, e14880. [Google Scholar] [CrossRef]
- Stewart, T.M.; Fry, D.; McAra, L.; Hamilton, S.; King, A.; Laurie, M.; McCluskey, G. Rates, perceptions and predictors of depression, anxiety and Post Traumatic Stress Disorder (PTSD)-like symptoms about COVID-19 in adolescents. PLoS ONE 2022, 17, e0266818. [Google Scholar] [CrossRef]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef]
- Shah, K.; Mann, S.; Singh, R.; Bangar, R.; Kulkarni, R. Impact of COVID-19 on the Mental Health of Children and Adolescents. Cureus 2020, 12, e10051. [Google Scholar] [CrossRef]
- Adolescent Mental Health. Available online: http://www.who.int/mental_health/maternal-child/child_adolescent/en/ (accessed on 17 July 2020).
- Cherkasova, M.V.; Roy, A.; Molina, B.S.; Scott, G.; Weiss, G.; Barkley, R.A.; Biederman, J.; Uchida, M.; Hinshaw, S.P.; Owens, E.B.; et al. Adult outcome as seen through controlled prospective follow-up studies of children with attention-deficit/hyperactivity disorder followed into adulthood. J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 378–391. [Google Scholar] [CrossRef]
- Kim, J.; Kim, D.G.; Kamphaus, R. Early detection of mental health through universal screening at schools. Ga. Educ. Res. 2022, 19, 62–79. [Google Scholar] [CrossRef]
- Colizzi, M.; Lasalvia, A.; Ruggeri, M. Prevention and early intervention in youth mental health: Is it time for a multidisciplinary and trans-diagnostic model for care? Int. J. Ment. Health Syst. 2020, 14, 23. [Google Scholar] [CrossRef]
- Otto, C.; Reiss, F.; Voss, C.; Wüstner, A.; Meyrose, A.K.; Hölling, H.; Ravens-Sieberer, U. Mental health and well-being from childhood to adulthood: Design, methods and results of the 11-year follow-up of the BELLA study. Eur. Child Adolesc. Psychiatry 2021, 30, 1559–1577. [Google Scholar] [CrossRef]
- Hodes, M.; Vostanis, P. Practitioner review: Mental health problems of refugee children and adolescents and their management. J. Child Psychol. Psychiatry 2019, 60, 716–731. [Google Scholar] [CrossRef]
- Glascoe, F.P. Early detection of developmental and behavioral problems. Pediatr. Rev. 2000, 21, 272–280. [Google Scholar] [CrossRef]
- Adnan, M.; Anwar, K. Online learning amid the COVID-19 pandemic: Students’ perspectives. Online Submiss. 2020, 2, 45–51. [Google Scholar] [CrossRef]
- Chung, E.; Subramaniam, G.; Dass, L.C. Online learning readiness among university students in Malaysia amidst COVID-19. Asian J. Univ. Educ. 2020, 16, 45–58. [Google Scholar] [CrossRef]
- Miller De Rutte, A.M.; Rubenstein, B.P. Acculturative stress and the effects on health and health behaviors in Hispanic immigrants: A systematic review. Hisp. J. Behav. Sci. 2021, 43, 433–455. [Google Scholar] [CrossRef]
- Fadus, M.C.; Ginsburg, K.R.; Sobowale, K.; Halliday-Boykins, C.A.; Bryant, B.E.; Gray, K.M.; Squeglia, L.M. Unconscious bias and the diagnosis of disruptive behavior disorders and ADHD in African American and Hispanic youth. Acad. Psychiatry 2020, 44, 95–102. [Google Scholar] [CrossRef]
- Hough, R.L.; Hazen, A.L.; Soriano, F.I.; Wood, P.; McCabe, K.; Yeh, M. Mental health care for Latinos: Mental health services for Latino adolescents with psychiatric disorders. Psychiatr. Serv. 2002, 53, 1556–1562. [Google Scholar] [CrossRef]
- Lopez-Serrano, J.; Díaz-Bóveda, R.; González-Vallespí, L.; Santamarina-Pérez, P.; Bretones-Rodríguez, A.; Calvo, R.; Lera-Miguel, S. Psychological impact during COVID-19 lockdown in children and adolescents with previous mental health disorders. Span. J. Psychiatry Ment. Health 2023, 16, 32–41. [Google Scholar] [CrossRef]
- Bilu, Y.; Flaks-Manov, N.; Bivas-Benita, M.; Akiva, P.; Kalkstein, N.; Yehezkelli, Y.; Mizrahi-Reuveni, M.; Ekka-Zohar, A.; David, S.S.B.; Lerner, U.; et al. Data-driven assessment of adolescents’ mental health during the COVID-19 pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2023, 62, 920–937. [Google Scholar] [CrossRef]
- Leeb, R.T.; Bitsko, R.H.; Radhakrishnan, L.; Martinez, P.; Njai, R.; Holland, K.M. Mental health–related emergency department visits among children aged < 18 years during the COVID-19 pandemic: United States, January 1–October 17, 2020. Morb. Mortal. Wkly. Rep. 2020, 69, 1675–1680. [Google Scholar]
- Kidman, R.; Margolis, R.; Smith-Greenaway, E.; Verdery, A.M. Estimates and projections of COVID-19 and parental death in the US. JAMA Pediatr. 2021, 175, 745–746. [Google Scholar] [CrossRef]
- Mikkelsen, H.T.; Skarstein, S.; Helseth, S.; Småstuen, M.C.; Haraldstad, K.; Rohde, G. Health-related quality of life, health literacy and COVID-19-related worries of 16-to 17-year-old adolescents and parents one year into the pandemic: A cross-sectional study. BMC Public Health 2022, 22, 1321. [Google Scholar] [CrossRef]
- Eriksen, S.; Schipper, E.L.F.; Scoville-Simonds, M.; Vincent, K.; Adam, H.N.; Brooks, N.; Harding, B.; Khatri, D.; Lenaerts, L.; Liverman, D.; et al. Adaptation interventions and their effect on vulnerability in developing countries: Help, hindrance or irrelevance? World Dev. 2021, 141, 105383. [Google Scholar] [CrossRef]
- McKnight-Eily, L.R.; Okoro, C.A.; Strine, T.W.; Verlenden, J.; Hollis, N.D.; Njai, R.; Mitchell, E.W.; Board, A.; Puddy, R.; Thomas, C. Racial and ethnic disparities in the prevalence of stress and worry, mental health conditions, and increased substance use among adults during the COVID-19 pandemic: United States, April and May 2020. Morb. Mortal. Wkly. Rep. 2021, 70, 162–166. [Google Scholar] [CrossRef]
- Baxter, T.; Shenoy, S.; Lee, H.S.; Griffith, T.; Rivas-Baxter, A.; Park, S. Unequal outcomes: The effects of the COVID-19 pandemic on mental health and wellbeing among Hispanic/Latinos with varying degrees of ‘Belonging’. Int. J. Soc. Psychiatry 2023, 69, 853–864. [Google Scholar] [CrossRef]
- Aburto, J.M.; Tilstra, A.M.; Floridi, G.; Dowd, J.B. Significant impacts of the COVID-19 pandemic on race/ethnic differences in US mortality. Proc. Natl. Acad. Sci. USA 2022, 119, e2205813119. [Google Scholar] [CrossRef]
- Garcia, M.A.; Homan, P.A.; García, C.; Brown, T.H. The color of COVID-19: Structural racism and the disproportionate impact of the pandemic on older Black and Latinx adults. J. Gerontol. Ser. B 2021, 76, e75–e80. [Google Scholar] [CrossRef]
- Tai, D.B.G.; Shah, A.; Doubeni, C.A.; Sia, I.G.; Wieland, M.L. The disproportionate impact of COVID-19 on racial and ethnic minorities in the United States. Clin. Infect. Dis. 2021, 72, 703–706. [Google Scholar] [CrossRef]
- Doom, J.R.; Deer, L.K.; Dieujuste, N.; Han, D.; Rivera, K.M.; Scott, S.R. Youth psychosocial resilience during the COVID-19 pandemic. Curr. Opin. Psychol. 2023, 53, 101656. [Google Scholar] [CrossRef]
- Mesman, E.; Vreeker, A.; Hillegers, M. Resilience and mental health in children and adolescents: An update of the recent literature and future directions. Curr. Opin. Psychiatry 2021, 34, 586. [Google Scholar] [CrossRef]
- Lenz, A.S. Evidence for relationships between hope, resilience, and mental health among youth. J. Couns. Dev. 2021, 99, 96–103. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Auquier, P.; Erhart, M.; Gosch, A.; Rajmil, L.; Bruil, J.; Power, M.; Duer, W.; Cloetta, B.; Czemy, L.; et al. The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Qual. Life Res. 2007, 16, 1347–1356. [Google Scholar] [CrossRef]
- Ardelean, V.P.; Andrei, V.L.; Miuţa, C.C.; Boros-Balint, I.; Deak, G.F.; Molnar, A.; Berki, T.; Győri, F.; Geantă, V.A.; Dehelean, C.A.; et al. The KIDSCREEN-27 Quality of Life Measure for Romanian Children Aged 6: Reliability and Validity of the Romanian Version. Healthcare 2022, 10, 1198. [Google Scholar] [CrossRef]
- Birmaher, B.; Brent, D.A.; Chiappetta, L.; Bridge, J.; Monga, S.; Baugher, M. Psychometric properties of the Screen for Child Anxiety Related Emotional Disorders (SCARED): A replication study. J. Am. Acad. Child Adolesc. Psychiatry 1999, 38, 1230–1236. [Google Scholar] [CrossRef]
- Neufeld, S.A.; Dunn, V.J.; Jones, P.B.; Croudace, T.J.; Goodyer, I.M. Reduction in adolescent depression after contact with mental health services: A longitudinal cohort study in the UK. Lancet Psychiatry 2017, 4, 120–127. [Google Scholar] [CrossRef] [PubMed]
- Barkmann, C.; Erhart, M.; Schulte-Markwort, M. The German version of the Centre for Epidemiological Studies Depression Scale for Children: Psychometric evaluation in a population-based survey of 7 to 17 year-old children and adolescents: Results of the BELLA study. Eur. Child Adolesc. Psychiatry 2008, 17, 116–124. [Google Scholar] [CrossRef] [PubMed]
- Jiang, L.; Wang, Y.; Zhang, Y.; Li, R.; Wu, H.; Li, C.; Wu, Y.; Tao, Q. The reliability and validity of the center for epidemiologic studies depression scale (CES-D) for Chinese university students. Front. Psychiatry 2019, 10, 315. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Vélez, R.; Olabarrieta-Landa, L.; Rivera, D.; Izquierdo, M. Factor structure of the 10-item CES-D Scale among patients with persistent COVID-19. J. Med. Virol. 2023, 95, e28236. [Google Scholar] [CrossRef]
- Rahman, A.; Muktadir, M.G. SPSS: An imperative quantitative data analysis tool for social science research. Int. J. Res. Innov. Soc. Sci. 2021, 5, 300–302. [Google Scholar] [CrossRef]
- Kinser, P.; Masho, S. “I just start crying for no reason”: The experience of stress and depression in pregnant, urban, African-American adolescents and their perception of yoga as a management strategy. Women’s Health Issues 2015, 25, 142–148. [Google Scholar] [CrossRef]
- Grazzani, I.; Agliati, A.; Cavioni, V.; Conte, E.; Gandellini, S.; Lupica Spagnolo, M.; Ornaghi, V.; Rossi, F.M.; Cefai, C.; Bartolo, P.; et al. Adolescents’ resilience during COVID-19 pandemic and its mediating role in the association between SEL skills and mental health. Front. Psychol. 2022, 13, 153. [Google Scholar] [CrossRef]
- Panchal, U.; Salazar de Pablo, G.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The impact of COVID-19 lockdown on child and adolescent mental health: Systematic review. Eur. Child Adolesc. Psychiatry 2023, 32, 1151–1177. [Google Scholar] [CrossRef]
- Toenders, Y.J.; van der Cruijsen, R.; Runze, J.; van de Groep, S.; Wierenga, L.; Crone, E.A. Mood variability during adolescent development and its relation to sleep and brain development. bioRxiv 2022. [Google Scholar] [CrossRef]
- Tang, S.; Xiang, M.; Cheung, T.; Xiang, Y.T. Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 2021, 279, 353–360. [Google Scholar] [CrossRef]
- Zuckerman, K.E.; Sinche, B.; Mejia, A.; Cobian, M.; Becker, T.; Nicolaidis, C. Latino parents’ perspectives on barriers to autism diagnosis. Acad. Pediatr. 2014, 14, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Todhunter-Reid, A.; Mitsdarffer, M.L.; Muñoz-Laboy, M.; Yoon, A.S.; Xu, L. Barriers and facilitators for mental health service use among racial/ethnic minority adolescents: A systematic review of literature. Front. Public Health 2021, 9, 641605. [Google Scholar] [CrossRef] [PubMed]
- Giano, Z.; Anderson, M.; Shreffler, K.M.; Cox, R.B., Jr.; Merten, M.J.; Gallus, K.L. Immigration-related arrest, parental documentation status, and depressive symptoms among early adolescent Latinos. Cult. Divers. Ethn. Minor. Psychol. 2020, 26, 318. [Google Scholar] [CrossRef] [PubMed]
- Karpman, M.; Gonzalez, D.; Kenney, G.M. Parents Are Struggling to Provide for Their Families during the Pandemic; Urban Institute: Washington, DC, USA, 2020. [Google Scholar]





| Category | Value | % | |
|---|---|---|---|
| Grade | 6 | 162 | 27.7 |
| 7 | 191 | 32.7 | |
| 8 | 230 | 39.4 | |
| Gender | Female | 316 | 54.1 |
| Male | 263 | 45.0 | |
| Race/Ethnicity | Black | 17 | 2.9 |
| Hispanic | 423 | 72.4 | |
| Other/Unknown | 92 | 15.8 | |
| White | 47 | 8.0 | |
| Category | Value | % | |
|---|---|---|---|
| Most-used language at home | English | 10 | 43.5 |
| Spanish | 13 | 56.5 | |
| Child in special education | Yes | 1 | 4.3 |
| No | 22 | 95.7 | |
| Child in gifted program | Yes | 11 | 50.0 |
| No | 11 | 50.0 | |
| Race/Ethnicity | European American | 3 | 2.9 |
| Hispanic | 18 | 72.4 | |
| Other/Unknown | 1 | 15.8 | |
| Education level | ≥high school diploma | 11 | 52.4 |
| <high school diploma | 8 | 38.1 | |
| Unknown | 2 | 9.5 | |
| Employment status | Full time | 13 | 59.1 |
| Part time | 3 | 13.6 | |
| Not working | 5 | 22.7 | |
| Other/Unknown | 1 | 4.5 | |
| Item on Adolescent Survey | Item on Parental Survey | Item |
|---|---|---|
| 4 | 8 | During the ongoing COVID-19 pandemic, how often were you/your child worried? |
| 5 | 9 | During the ongoing COVID-19 pandemic, how often were you/your child happy? |
| 9 | 10 | During the ongoing COVID-19 pandemic, how often were you/your child angry? |
| 6 | 13 | During the ongoing COVID-19 pandemic, how often were you/your child lonely? |
| 7 | 11 | During the ongoing COVID-19 pandemic, have you/your child cried often? |
| 8 | 17 | During the ongoing COVID-19 pandemic, how well were you/your child able to focus? |
| 11 | 19 | Compared to the ongoing COVID-19 pandemic and now, how would you/your child the general feeling now? |
| 13 | 15 | Compared with before the COVID-19 pandemic, do you think you/your child spend(s) more time using smartphones and/or devices during the COVID-19 pandemic? |
| Predictor | B | SE | β | CI 95% Lower | CI 95% Upper | t | df | p | VIF |
|---|---|---|---|---|---|---|---|---|---|
| Worried | −0.050 | 0.047 | −0.049 | −0.143 | 0.042 | n − 1.073 | 10 | 0.284 | 1.263 |
| Happy | 0.069 | 0.040 | 0.075 | −0.010 | 0.147 | 1.720 | 10 | 0.086 | 1.169 |
| Angry | 0.009 | 0.048 | 0.009 | −0.086 | 0.103 | 0.180 | 10 | 0.857 | 1.415 |
| lonely | 0.004 | 0.028 | 0.006 | −0.052 | 0.059 | 0.125 | 10 | 0.900 | 1.462 |
| cried | −0.085 | 0.045 | −0.098 | −0.174 | 0.003 | −1.889 | 10 | 0.059 | 1.640 |
| focus | 0.111 | 0.042 | 0.119 | 0.028 | 0.193 | 2.635 | 10 | 0.009 ** | 1.248 |
| device | 0.079 | 0.040 | 0.087 | 0.000 | 0.158 | 1.960 | 10 | 0.051 | 1.069 |
| talk | 0.117 | 0.042 | 0.117 | 0.035 | 0.198 | 2.798 | 10 | 0.005 ** | 1.108 |
| Family time | 0.108 | 0.036 | 0.128 | 0.037 | 0.178 | 3.009 | 10 | 0.003 ** | 1.208 |
| Gender | 0.022 | 0.090 | 0.011 | −0.153 | 0.198 | 0.251 | 10 | 0.802 | 1.210 |
| 0.106 | |||||||||
| F | 6.542 | ||||||||
| Durbin-Watson | 1.996 | ||||||||
| Predictor | B | SE | Wald | df | p | Exp (B) |
|---|---|---|---|---|---|---|
| Worried | −0.04 | 0.16 | 0.06 | 1 | 0.800 | 0.96 |
| Angry | −0.09 | 0.16 | 0.33 | 1 | 0.560 | 0.91 |
| Cried | −0.42 | 0.14 | 9.61 | 1 | 0.001 *** | 0.66 |
| Lonely | −0.07 | 0.1 | 0.56 | 1 | 0.450 | 0.93 |
| Happy | 0.31 | 0.14 | 5.17 | 1 | 0.020 ** | 1.36 |
| 2 Log likelihood | 75.171 | |||||
| Cox & Snell R Square | 0.750 | |||||
| Nagelkerke R Square | 0.103 | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.; Scott, R. Cross-Sectional and Descriptive Study on the Challenges and Awareness of Hispanic Parents Regarding Their Adolescents’ Mental Health during the COVID-19 Pandemic. Healthcare 2024, 12, 279. https://doi.org/10.3390/healthcare12020279
Kim J, Scott R. Cross-Sectional and Descriptive Study on the Challenges and Awareness of Hispanic Parents Regarding Their Adolescents’ Mental Health during the COVID-19 Pandemic. Healthcare. 2024; 12(2):279. https://doi.org/10.3390/healthcare12020279
Chicago/Turabian StyleKim, Jihye, and Robyn Scott. 2024. "Cross-Sectional and Descriptive Study on the Challenges and Awareness of Hispanic Parents Regarding Their Adolescents’ Mental Health during the COVID-19 Pandemic" Healthcare 12, no. 2: 279. https://doi.org/10.3390/healthcare12020279
APA StyleKim, J., & Scott, R. (2024). Cross-Sectional and Descriptive Study on the Challenges and Awareness of Hispanic Parents Regarding Their Adolescents’ Mental Health during the COVID-19 Pandemic. Healthcare, 12(2), 279. https://doi.org/10.3390/healthcare12020279






