Management and Outcomes of Traumatic Liver Injury: A Retrospective Analysis from a Tertiary Care Center Experience
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Data Mining and Processing
- Demographic data;
- Mechanisms of injury: blunt trauma, penetrating, and iatrogenic;
- Type of injury: laceration, contusion/hematoma, and hemoperitoneum;
- Grades of injury on CT using the American Association for the Surgery of Trauma (AAST) liver injury scale;
- Associated extra-abdominal injuries;
- Hemodynamic statuses at presentation;
- Extended Focused Assessment with Sonography in Trauma (E-FAST);
- Interventional radiology procedures: angioembolization; percutaneous transhepatic biliary drainage (PTD);
- Complications;
- Length of ward, hospital, and ICU stay;
- Laboratory values at first admission, including alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels;
- Glasgow coma scale (GCS) score.
2.3. Statistical Analysis
3. Results
Treatment and Outcomes of Patients
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beshay, M.; Mertzlufft, F.; Kottkamp, H.W.; Reymond, M.; Schmid, R.A.; Branscheid, D.; Vordemvenne, T. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: A mono-centre study. World J. Emerg. Surg. 2020, 15, 45. [Google Scholar] [CrossRef] [PubMed]
- Abo-Elhoda, M.F.; Attia, S.M.; Ahmed, M.E.; Abdeldaiem, K.A.E. Solid organs injuries in blunt abdominal trauma patients. Egypt. J. Hosp. Med. 2021, 83, 1477–1483. [Google Scholar] [CrossRef]
- Arumugam, S.; Al-Hassani, A.; El-Menyar, A.; Abdelrahman, H.; Parchani, A.; Peralta, R.; Zarour, A.; Al-Thani, H. Frequency, causes and pattern of abdominal trauma: A 4-year descriptive analysis. J. Emerg. Trauma Shock 2015, 8, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Matthes, G.; Stengel, D.; Seifert, J.; Rademacher, G.; Mutze, S.; Ekkernkamp, A. Blunt liver injuries in polytrauma: Results from a cohort study with the regular use of whole-body helical computed tomography. World J. Surg. 2003, 27, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Badger, S.A.; Barclay, R.; Campbell, P.; Mole, D.J.; Diamond, T. Management of liver trauma. World J. Surg. 2009, 33, 2522–2537. [Google Scholar] [CrossRef] [PubMed]
- La Via, L.; Astuto, M.; Dezio, V.; Muscarà, L.; Palella, S.; Zawadka, M.; Vignon, P.; Sanfilippo, F. Agreement between subcostal and transhepatic longitudinal imaging of the inferior vena cava for the evaluation of fluid responsiveness: A systematic review. J. Crit. Care 2022, 71, 154108. [Google Scholar] [CrossRef]
- Sanfilippo, F.; La Via, L.; Dezio, V.; Amelio, P.; Genoese, G.; Franchi, F.; Messina, A.; Robba, C.; Noto, A. Inferior vena cava distensibility from subcostal and trans-hepatic imaging using both M-mode or artificial intelligence: A prospective study on mechanically ventilated patients. Intensive Care Med. Exp. 2023, 11, 40. [Google Scholar] [CrossRef]
- Achatz, G.; Schwabe, K.; Brill, S.; Zischek, C.; Schmidt, R.; Friemert, B.; Beltzer, C. Diagnostic options for blunt abdominal trauma. Eur. J. Trauma Emerg. Surg. 2022, 48, 3575–3589. [Google Scholar] [CrossRef]
- Taourel, P.; Vernhet, H.; Suau, A.; Granier, C.; Lopez, F.M.; Aufort, S. Vascular emergencies in liver trauma. Eur. J. Radiol. 2007, 64, 73–82. [Google Scholar] [CrossRef]
- Sawhney, C.; Kaur, M.; Gupta, B.; Singh, P.M.; Gupta, A.; Kumar, S.; Misra, M.C. Care issues in solid organ injury: Review and experience in a tertiary trauma center. Saudi J. Anaesth. 2014, 8, S29–S35. [Google Scholar] [CrossRef]
- Coccolini, F.; Coimbra, R.; Ordonez, C.; Kluger, Y.; Vega, F.; Moore, E.E.; Biffl, W.; Peitzman, A.; Horer, T.; Abu-Zidan, F.M.; et al. WSES expert panel. Liver trauma: WSES 2020 guidelines. World J. Emerg. Surg. 2020, 15, 24. [Google Scholar] [CrossRef] [PubMed]
- Alghamdi, H.M. Management of liver trauma. Saudi J. Med. Sci. 2017, 5, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.Y.; Li, Q.J.; Gong, J.P. Treatment strategy for hepatic trauma. Chin. J. Traumatol. 2016, 19, 168–171. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.S.; Kumar, G.; Pillai, A.K. Hepatic trauma interventions. Semin. Intervent. Radiol. 2021, 38, 96–10412. [Google Scholar] [CrossRef] [PubMed]
- Kozar, R.A.; Crandall, M.; Shanmuganathan, K.; Zarzaur, B.L.; Coburn, M.; Cribari, C.; Kaups, K.; Schuster, K.; Tominaga, G.T. AAST Patient Assessment Committee Organ injury scaling 2018 update: Spleen, liver, and kidney. J. Trauma Acute Care Surg. 2018, 85, 1119–1122. [Google Scholar] [CrossRef] [PubMed]
- Petrowsky, H.; Raeder, S.; Zuercher, L.; Platz, A.; Simmen, H.P.; Puhan, M.A.; Keel, M.J.; Clavien, P.A. A quarter century experience in liver trauma: A plea for early computed tomography and conservative management for all hemodynamically stable patients. World J. Surg. 2012, 36, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Jang, Y.; Jun, H. Analysis of trauma scoring system for patients with abdominal trauma. Ulus. Travma Acil Cerrahi Derg. 2022, 29, 68–72. [Google Scholar] [CrossRef]
- Hommes, M.; Navsaria, P.H.; Schipper, I.B.; Krige, J.E.; Kahn, D.; Nicol, A.J. Management of blunt liver trauma in 134 severely injured patients. Injury 2015, 46, 837–842. [Google Scholar] [CrossRef]
- Yidirim, M.A.; Vatansev, H.; Senturk, M.; Kadiyoran, C.; İyisoy, S. Our experience of nonoperative management in patients with liver injury due to multiple blunt trauma. Selcuk Med. J. 2021, 37, 57–63. [Google Scholar]
- Bilgiç, İ.; Gelecek, S.; Akgün, A.E.; Özmen, M.M. Evaluation of liver injury in a tertiary hospital: A retrospective study. Ulus. Travma Acil Cerrahi Derg. 2014, 20, 359–365. [Google Scholar] [CrossRef]
- Gaski, I.A.; Skattum, J.; Brooks, A.; Koyama, T.; Eken, T.; Naess, P.A.; Gaarder, C. Decreased mortality, laparotomy, and embolization rates for liver injuries during a 13-year period in a major Scandinavian trauma center. Trauma Surg. Acute Care Open 2018, 3, e000205. [Google Scholar] [CrossRef] [PubMed]
- Liagkos, G.T.; Spyropoulos, C.; Tsourouflis, G.; Papadopoulos, A.; Ioannides, P.; Vagianos, C. non-operative management of blunt abdominal trauma in highly selective cases: A safe and effective choice. Ulus. Travma Acil Cerrahi Derg. 2018, 24, 104–109. [Google Scholar] [CrossRef] [PubMed]
- Sinha, Y.; Khajanchi, M.U.; Prajapati, R.P.; Dharap, S.; Soni, K.D.; Kumar, V.; Mahindrakar, S.; Roy, N. Management of liver trauma in urban university hospitals in India: An observational multicentre cohort study. World J. Emerg. Surg. 2020, 15, 58. [Google Scholar] [CrossRef] [PubMed]
- Ghnnam, W.M.; Almasry, H.N.; Ghanem, M.A. Non-operative management of blunt liver trauma in a level II trauma hospital in Saudi Arabia. Int. J. Crit. Illn. Inj. Sci. 2013, 3, 118–123. [Google Scholar] [CrossRef] [PubMed]
- Brillantino, A.; Iacobellis, F.; Festa, P.; Mottola, A.; Acampora, C.; Corvino, F.; Del Giudice, S.; Lanza, M.; Armellino, M.; Niola, R.; et al. Non-operative management of blunt liver trauma: Safety, efficacy and complications of a standardized treatment protocol. Bull. Emerg. Trauma 2019, 7, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Parks, R.W.; Chrysos, E.; Diamond, T. Management of liver trauma. Br. J. Surg. 1999, 86, 1121–1135. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Vernick, J.J. Management of liver trauma in adults. J. Emerg. Trauma Shock 2011, 4, 114–119. [Google Scholar] [CrossRef]
- Jyothiprakasan, V.K.; Madhusudhan, C.; Reddy, C.S. Study of blunt trauma abdomen involving liver injuries based on grade of injury, management: A single centre study. Int. Surg. J. 2019, 6, 793–799. [Google Scholar] [CrossRef]
- Nishida, T.; Fujita, N.; Nakao, K. A multivariate analysis of the prognostic factors in severe liver trauma. Surg. Today 1996, 26, 389–394. [Google Scholar] [CrossRef]
- Gao, J.M.; Du, D.Y.; Zhao, X.J.; Liu, G.L.; Yang, J.; Zhao, S.H.; Lin, X. Liver trauma: Experience in 348 cases. World J. Surg. 2003, 27, 703–708. [Google Scholar] [CrossRef]
- Afifi, I.; Abayazeed, S.; El-Menyar, A.; Abdelrahman, H.; Peralta, R.; Al-Thani, H. Blunt liver trauma: A descriptive analysis from a level I trauma center. BMC Surg. 2018, 18, 42. [Google Scholar] [CrossRef] [PubMed]
- Roh, H.S.; Park, Y.C.; Jo, Y.G.; Kim, J.C. The incidence and impact of abdominal surgery on delirium in abdominal trauma patients. J. Acute Care Surg. 2020, 10, 42–46. [Google Scholar] [CrossRef]
- Bala, M.; Gazalla, S.A.; Faroja, M.; Bloom, A.I.; Zamir, G.; Rivkind, A.I.; Almogy, G. Complications of high grade liver injuries: Management and outcome with focus on bile leaks. Scand. J. Trauma Resusc. Emerg. Med. 2012, 20, 20. [Google Scholar] [CrossRef] [PubMed]
- Fabian, T.C.; Croce, M.A.; Stanford, G.G.; Payne, L.W.; Mangiante, E.C.; Voeller, G.R.; Kudsk, K.A. Factors affecting morbidity following hepatic trauma. A prospective analysis of 482 injuries. Ann. Surg. 1991, 213, 540. [Google Scholar] [CrossRef]
- Sikhondze, W.L.; Madiba, T.E.; Naidoo, N.M.; Muckart, D.J. Predictors of outcome in patients requiring surgery for liver trauma. Injury 2007, 38, 65–70. [Google Scholar] [CrossRef]
- Cascella, M.; Racca, E.; Nappi, A.; Coluccia, S.; Maione, S.; Luongo, L.; Guida, F.; Avallone, A.; Cuomo, A. Bayesian Network Analysis for Prediction of Unplanned Hospital Readmissions of Cancer Patients with Breakthrough Cancer Pain and Complex Care Needs. Healthcare 2022, 10, 1853. [Google Scholar] [CrossRef]
| Study Variables | n (%) |
|---|---|
| Age in years (mean ± SD) | 29.3 ± 15.5 |
| Gender | |
| Male | 35 (77.8%) |
| Female | 10 (22.2%) |
| Mechanism of injury | |
| Blunt trauma | 39 (86.7%) |
| Penetrating | 4 (8.9%) |
| Iatrogenic | 2 (4.4%) |
| Type of injury † | |
| Laceration | 44 (97.8%) |
| Contusion/hematoma | 23 (51.1%) |
| Hemoperitoneum | 13 (28.9%) |
| Grade | |
| Grade 1 | 5 (11.1%) |
| Grade 2 | 13 (28.9%) |
| Grade 3 | 17 (37.8%) |
| Grade 4 | 9 (20%) |
| Grade 5 | 1 (2.2%) |
| Study Variables | n (%) |
|---|---|
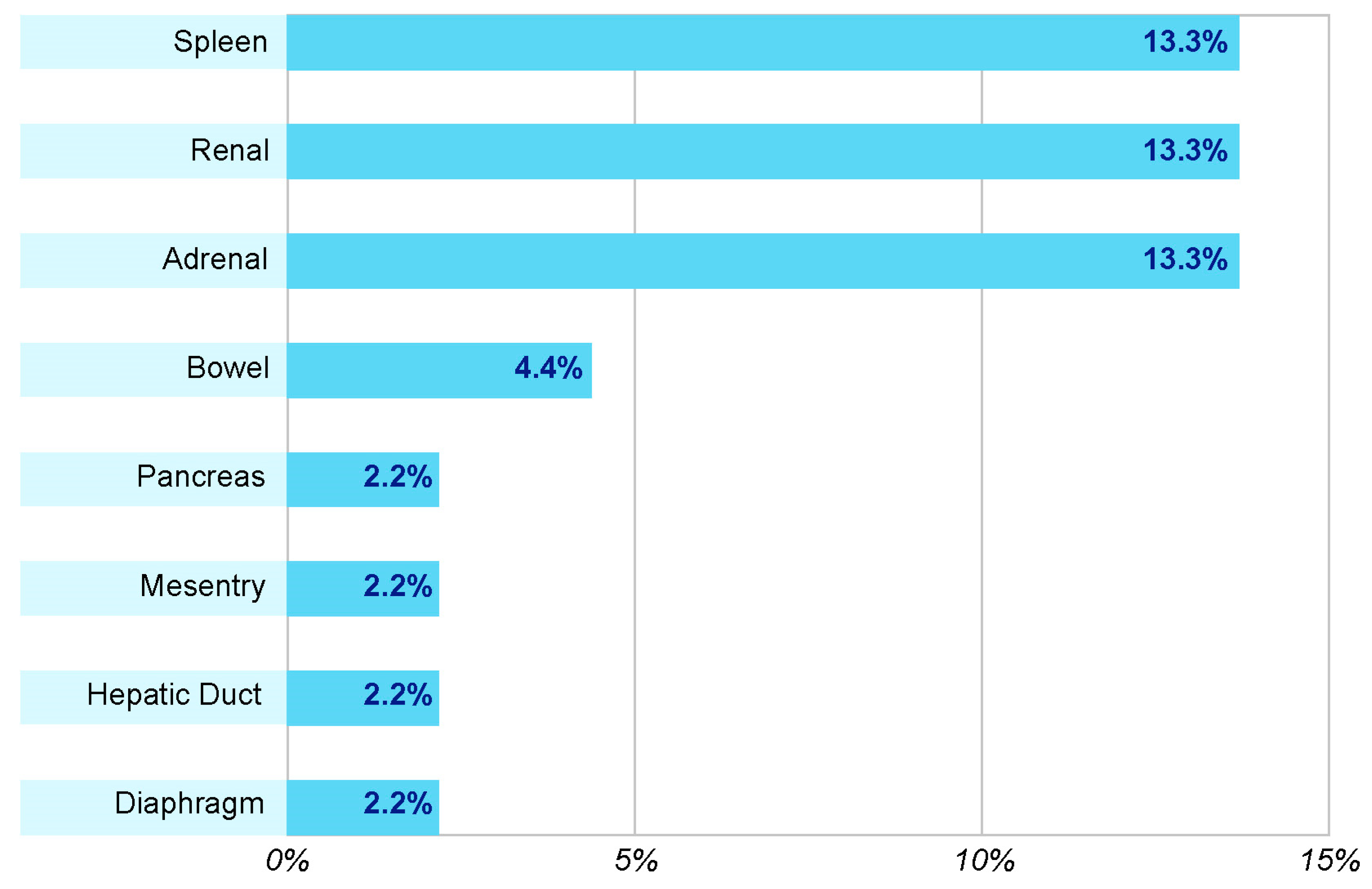
| Associated extra-abdominal injuries † | |
| Thoracic injury | 35 (77.8%) |
| Orthopedic injury | 23 (51.1%) |
| Head injury | 22 (48.9%) |
| Abdominal injury | 18 (40%) |
| Vascular injury | 6 (13.3%) |
| Ophthalmic injury | 5 (11.1%) |
| Variables | n (%) |
|---|---|
| Treatment performed | |
| Conservative | 37 (82.2%) |
| Laparotomy | 6 (13.3%) |
| Conservative to laparotomy | 2 (4.4%) |
| Interventional radiology procedures | |
| Angioembolization | 2 (4.4%) |
| PTD | 1 (2.2%) |
| Hemodynamic stability | |
| Unstable | 14 (31.1%) |
| Stable | 31 (68.9%) |
| E-FAST | |
| Not performed | 3 (6.7%) |
| Positive | 16 (35.6%) |
| Negative | 26 (57.8%) |
| Complications | 12 (26.7%) |
| Specific complication | |
| Delirium | 6 (13.3%) |
| Sepsis | 6 (13.3%) |
| Acute renal failure | 2 (4.4%) |
| Pneumonia | 2 (4.4%) |
| Seizure | 2 (4.4%) |
| Cardiac arrest | 1 (2.2%) |
| Splenic infarction | 1 (2.2%) |
| Meningitis | 1 (2.2%) |
| Acute respiratory distress syndrome | 1 (2.2%) |
| Disseminated intravascular coagulation | 1 (2.2%) |
| Presence of biliary leak | 4 (8.9%) |
| Mortality | 1 (2.2%) |
| Mean ± SD | |
| PRBCs | 5.91 ± 4.48 |
| FFP | 6.36 ± 3.67 |
| Platelet | 5.89 ± 3.79 |
| Median (min–max) | |
| ALT | 229 units/L (21–1277) |
| AST | 198.5 units/L (19–1000) |
| Re-bleed rate | 1 (1–5) |
| GCS score | 15 (3–15) |
| Length of hospital stay (days) | 11 (1–316) |
| ICU stay (days) | 4 (1–54) |
| Ward stay (days) | 7 (1–262) |
| Factor | Type of Treatment | |
|---|---|---|
| Conservative n (%) (n = 37) | Laparotomy/ Conservative to Laparotomy n (%) (n = 8) | |
| Age in years (mean ± SD) | 27.6 ± 14.4 | 37.2 ± 18.6 |
| Gender | ||
| Male | 29 (78.4%) | 6 (75%) |
| Female | 8 (21.6%) | 2 (25%) |
| Mechanism of injury | ||
| Blunt trauma | 35 (94.6%) | 4 (50%) |
| Non-blunt trauma | 2 (5.4%) | 4 (50%) |
| Type of injury † | ||
| Laceration | 36 (97.3%) | 8 (100%) |
| Contusion/hematoma | 21 (56.8%) | 2 (25%) |
| Hemoperitoneum | 9 (5.4%) | 4 (50%) |
| Grade | ||
| Grade 1 | 4 (10.8%) | 1 (12.5%) |
| Grade 2 | 10 (27%) | 3 (37.5%) |
| Grade 3 | 15 (40.5%) | 2 (25%) |
| Grade 4 | 7 (18.9%) | 2 (25%) |
| Grade 5 | 1 (2.7%) | 0 |
| Complications | 7 (18.9%) | 5 (62.5%) |
| Positive E-FAST * | 10 (28.6%) | 6 (85.7%) |
| Hemodynamic stability | ||
| Unstable | 10 (27%) | 4 (50%) |
| Stable | 27 (73%) | 4 (50%) |
| Mean ± SD | Mean ± SD | |
| PRBCs | 5.59 ± 4.24 | 6.83 ± 5.42 |
| FFP | 6.57 ± 3.05 | 6.00 ± 5.09 |
| Platelet | 5.33 ± 4.08 | 7.00 ± 3.61 |
| Median (min–max) | Median (min–max) | |
| ALT | 241 (21–1277) | 207.5 (63–935) |
| AST | 198.5 (19–1000) | 232.5 (39–950) |
| Re-bleed rate | 1 (1–2) | 2 (1–5) |
| GCS score | 11.5 (5–15) | 15 (5–15) |
| Length of hospital stay (days) | 22 (8–92) | 30 (15–316) |
| ICU stay (days) | 11 (2–20) | 16 (4–54) |
| Ward stays (days) | 13.5 (4–76) | 14 (4–262) |
| Factor | Hemodynamic Stability | |
|---|---|---|
| Unstable n (%) (n = 14) | Stable n (%) (n = 31) | |
| Age in years (mean ± SD) | 28.9 ± 14.0 | 29.5 ± 16.3 |
| Gender | ||
| Male | 12 (85.7%) | 23 (74.2%) |
| Female | 2 (14.3%) | 8 (25.8%) |
| Mechanism of injury | ||
| Blunt trauma | 12 (85.7%) | 27 (87.1%) |
| Non-blunt trauma | 2 (14.3%) | 4 (12.9%) |
| Type of injury † | ||
| Laceration | 14 (100%) | 30 (96.8%) |
| Contusion/hematoma | 5 (35.7%) | 18 (58.1%) |
| Hemoperitoneum | 5 (35.7%) | 8 (25.8%) |
| Grade | ||
| Grade 1 | 1 (7.1%) | 4 (12.9%) |
| Grade 2 | 4 (28.6%) | 9 (29%) |
| Grade 3 | 7 (50%) | 10 (32.3%) |
| Grade 4 | 2 (14.3%) | 7 (22.6%) |
| Grade 5 | 0 | 1 (3.2%) |
| Complications | 8 (57.1%) | 4 (12.9%) |
| Positive E-FAST * | 5 (38.5%) | 11 (37.9%) |
| Mean ± SD | Mean ± SD | |
| PRBCs | 8.36 ± 4.5 | 3.67 ± 3.2 |
| FFP | 7.29 ± 4.31 | 4.75 ± 1.5 |
| Platelet | 7 ± 4 | 3.67 ± 2.52 |
| Median (min–max) | Median (min–max) | |
| ALT | 165.5 (34–935) | 259 (21–1277) |
| AST | 155.5 (27–950) | 230.5 (19–1000) |
| Re-bleed rate | 1 (1–5) | 1 (1–3) |
| GCS score | 10 (5–15) | 15 (5–15) |
| Length of hospital stay (days) | 29 (8–316) | 19 (10–30) |
| ICU stay (days) | 16 (2–54) | 9 (4–16) |
| Ward stays (days) | 19 (4–262) | 9 (4–18) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alanezi, T.; Altoijry, A.; Alanazi, A.; Aljofan, Z.; Altuwaijri, T.; Iqbal, K.; AlSheikh, S.; Molla, N.; Altuwaijri, M.; Aloraini, A.; et al. Management and Outcomes of Traumatic Liver Injury: A Retrospective Analysis from a Tertiary Care Center Experience. Healthcare 2024, 12, 131. https://doi.org/10.3390/healthcare12020131
Alanezi T, Altoijry A, Alanazi A, Aljofan Z, Altuwaijri T, Iqbal K, AlSheikh S, Molla N, Altuwaijri M, Aloraini A, et al. Management and Outcomes of Traumatic Liver Injury: A Retrospective Analysis from a Tertiary Care Center Experience. Healthcare. 2024; 12(2):131. https://doi.org/10.3390/healthcare12020131
Chicago/Turabian StyleAlanezi, Tariq, Abdulmajeed Altoijry, Aued Alanazi, Ziyad Aljofan, Talal Altuwaijri, Kaisor Iqbal, Sultan AlSheikh, Nouran Molla, Mansour Altuwaijri, Abdullah Aloraini, and et al. 2024. "Management and Outcomes of Traumatic Liver Injury: A Retrospective Analysis from a Tertiary Care Center Experience" Healthcare 12, no. 2: 131. https://doi.org/10.3390/healthcare12020131
APA StyleAlanezi, T., Altoijry, A., Alanazi, A., Aljofan, Z., Altuwaijri, T., Iqbal, K., AlSheikh, S., Molla, N., Altuwaijri, M., Aloraini, A., Altuwaijri, F., & Aldossary, M. Y. (2024). Management and Outcomes of Traumatic Liver Injury: A Retrospective Analysis from a Tertiary Care Center Experience. Healthcare, 12(2), 131. https://doi.org/10.3390/healthcare12020131






