Destigmatizing Palliative Care among Young Adults—A Theoretical Intervention Mapping Approach
Abstract
1. Introduction
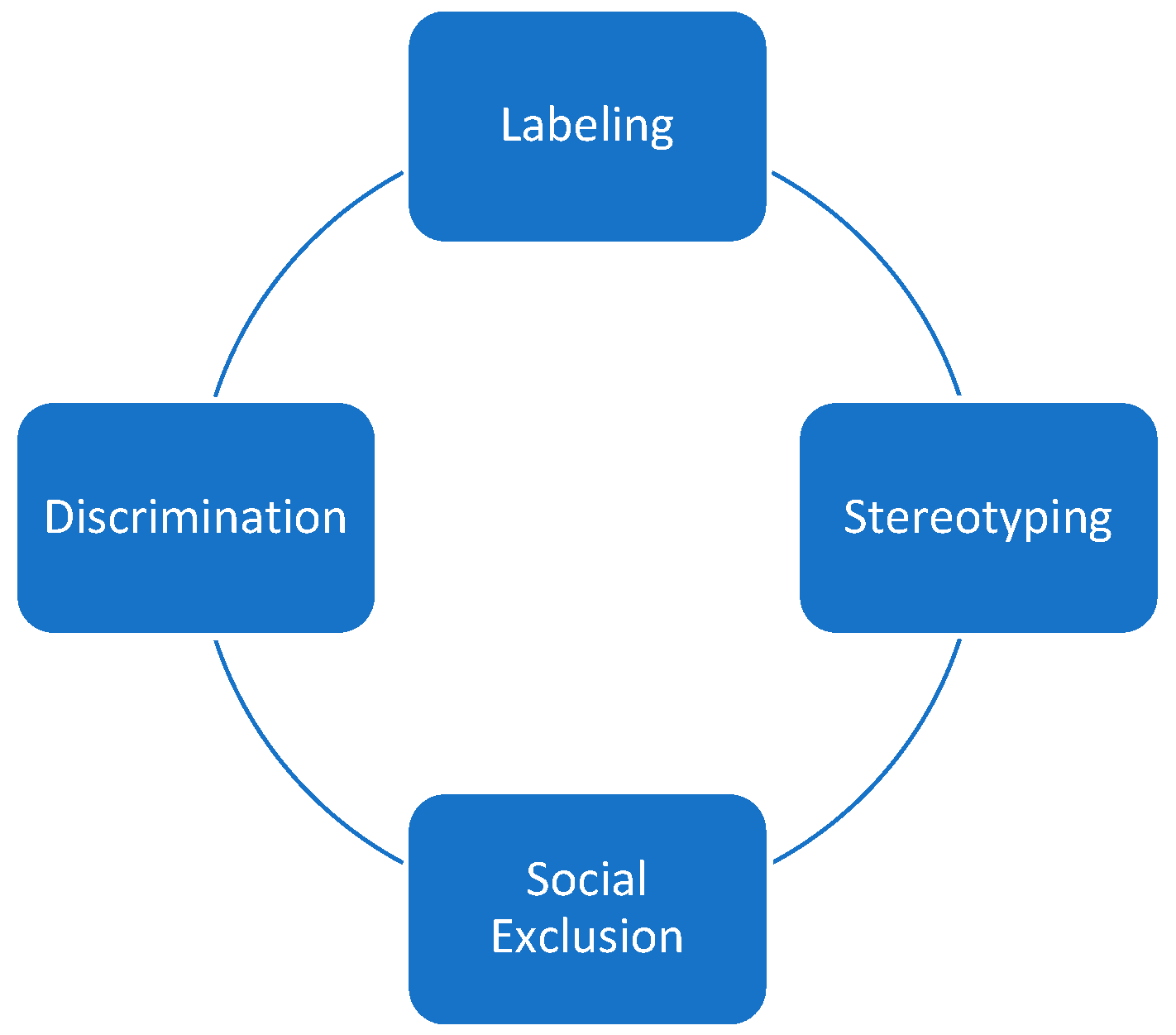
1.1. Stigmatization and Palliative Care
1.2. Reduction of Stigmas
1.3. Intervention Planning
1.4. Intervention Mapping
1.5. International Campaigns
1.6. Aim
2. Material and Methods
- Logic Model of the Problem: Needs Assessment
- Logical Model of Change: Defining Intervention Goals and Determinants of Behavioral Change
- Design of the Intervention through the Targeted Selection of Theory- and Evidence-Based Methods for behavioral Change
- Program Organization and Design, including Pretesting
- Implementation
- Evaluation Planning.
3. Results
3.1. Intervention Mapping
- Theoretical knowledge dissemination in secondary schools, vocational schools, and universities;
- Interactions with affected individuals and palliative care teams;
- Public awareness campaigns in public spaces;
- Public awareness campaigns on social media;
- An accompanying website with a discussion forum.
- Their concrete elaboration follows the Intervention Mapping approach.
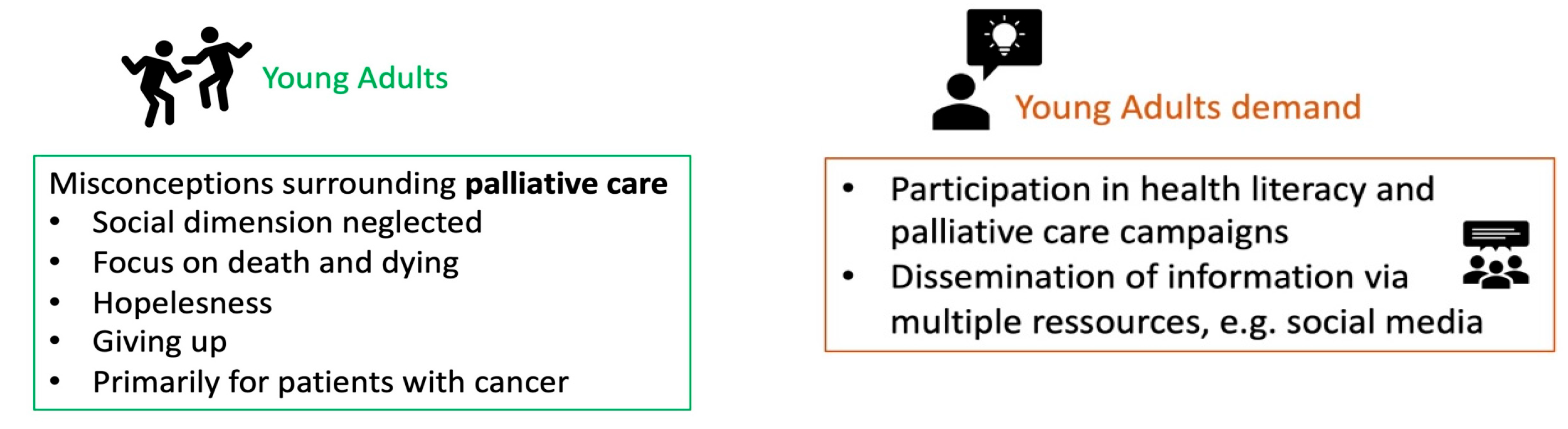
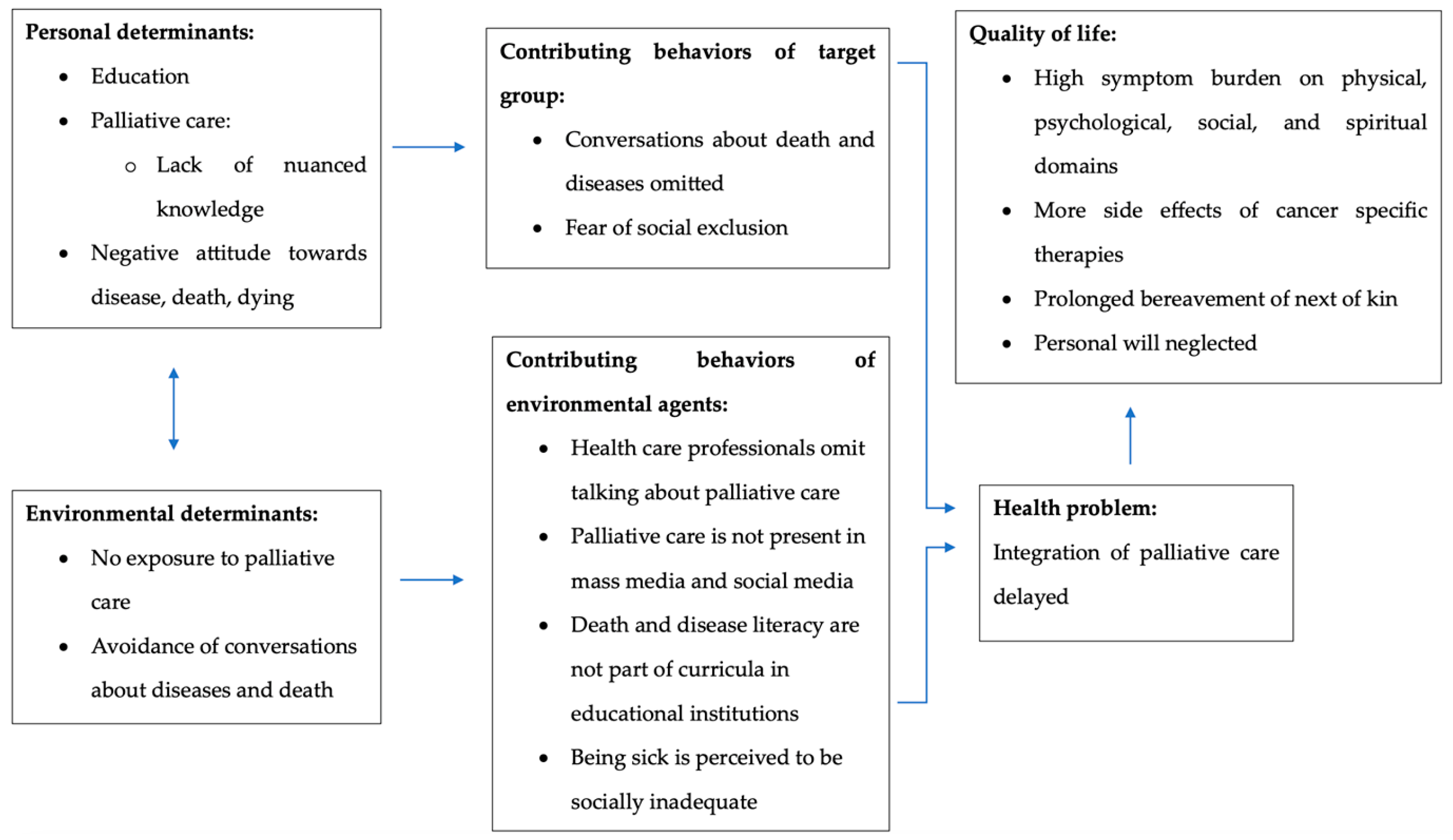
3.1.1. Step 1: Needs Assessment and Logic Model of the Problem
- -
- Regarding knowledge of palliative care, the following were found:
- Young adults often have heard of palliative care;
- Young adults, however, have little detailed knowledge of palliative care;
- Young adults assume that palliative care is only relevant in the last six months of a person’s life.
- -
- This affects the perception and attitude towards palliative care:
- Palliative care is seen as indicated only for certain illnesses;
- Palliative care is closely associated with death and dying, which can trigger fears;
- Death and dying are associated with hopelessness, and thus palliative care is also linked with giving up and hopelessness.
- -
- Increase in detailed knowledge of palliative care: palliative care is available for patients of any age at any stage of illness and follows a holistic approach.
- -
- Change of the perception of palliative care: palliative care is life-affirming, improves quality of life, and conveys hope.
3.1.2. Step 2: Logic Model of Change
- -
- Young adults:
- … discuss acquired knowledge of palliative care with each other;
- … talk about death, dying, and dealing with diseases to each other.
- -
- Environmental actors:
- Educational institutions facilitate education on palliative care;
- Educational institutions distribute information on palliative care;
- Communities place posters in public spaces;
- Information on palliative care is openly accessible via the internet.
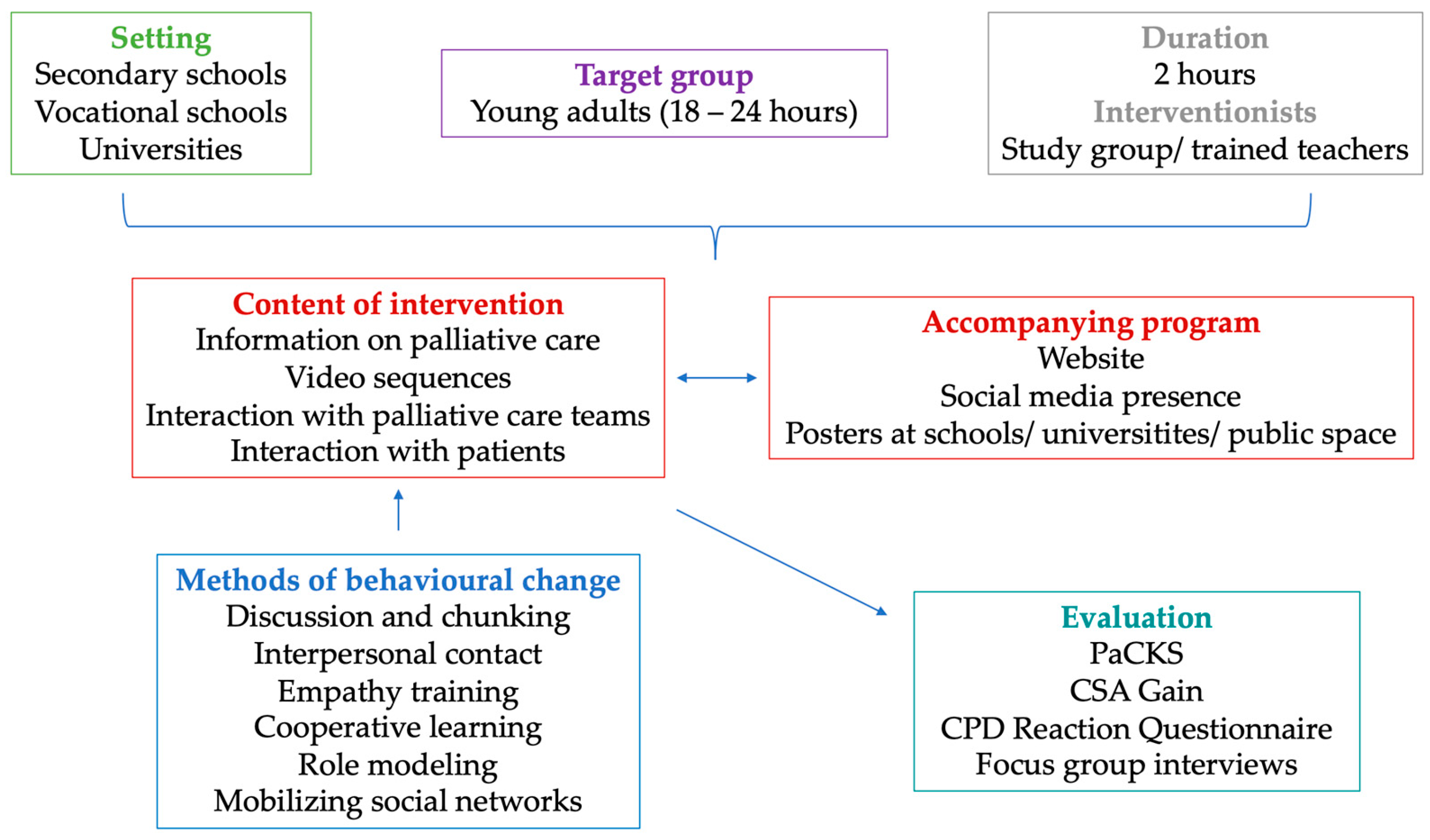
3.1.3. Step 3: Components and Behavior Change Methods
- -
- Intervention components:
- Knowledge dissemination about palliative care in educational institutions;
- Interaction with palliative care patients and staff;
- Informational brochures.
- -
- Public awareness campaign:
- Website;
- Social media presence;
- Posters in public spaces.
3.1.4. Step 4: Program Organization and Design
3.1.5. Step 5: Implementation
3.1.6. Step 6: Evaluation Plan
4. Discussion
5. Limitations
6. Conclusions and Outlook
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Friedman, S.R.; Williams, L.D.; Guarino, H.; Mateu-Gelabert, P.; Krawczyk, N.; Hamilton, L.; Walters, S.M.; Ezell, J.M.; Khan, M.; Di Iorio, J.; et al. The stigma system: How sociopolitical domination, scapegoating, and stigma shape public health. J. Community Psychol. 2022, 50, 385–408. [Google Scholar] [CrossRef] [PubMed]
- Hatzenbuehler, M.L.; Phelan, J.C.; Link, B.G. Stigma as a Fundamental Cause of Population Health Inequalities. Public Health 2013, 103, 813–821. [Google Scholar] [CrossRef] [PubMed]
- De Col, C.; Seewald, G.; Meise, U. Individuelle Bewältigung von Stigmatisierung und Diskriminierung. In Psychiatrische Rehabilitation; Springer: Berlin/Heidelberg, Germany, 2004; pp. 861–874. [Google Scholar]
- De Zwaan, M.; Herpertz, S.; Zipfel, S. Adipositas und Stigmatisierung. In Psychosoziale Aspekte der Adipositas-Chirurgie; Springer: Berlin/Heidelberg, Germany, 2018; pp. 67–81. [Google Scholar]
- Harwood, A.; Carter, D.; Eliott, J. A public health framework for reducing stigma: The example of weight stigma. J. Bioeth. Inq. 2022, 19, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Angermeyer, M.C. Stigmatisierung psychisch kranker in der gesellschaft. Psychiatr. Prax. 2004, 31 (Suppl. S2), 246–250. [Google Scholar] [CrossRef]
- Shen, M.J.; Wellman, J.D. Evidence of palliative care stigma: The role of negative stereotypes in preventing willingness to use palliative care. Palliat. Support. Care 2019, 17, 374–380. [Google Scholar] [CrossRef]
- Shalev, A.; Phongtankuel, V.; Kozlov, E.; Shen, M.J.; Adelman, R.D.; Reid, M.C. Awareness and Misperceptions of Hospice and Palliative Care: A Population-Based Survey Study. Am. J. Hosp. Palliat. Med. 2018, 35, 431–439. [Google Scholar] [CrossRef]
- Heckel, M.; Peters, J.; Schweighart, S.; Habermann, M.; Ostgathe, C. Knowledge and Public Perception of Palliative Care in Germany. J. Palliat. Med. 2024, 27, 986–992. [Google Scholar] [CrossRef]
- Fliedner, M.C.; Zambrano, S.C.; Eychmueller, S. Public perception of palliative care: A survey of the general population. Palliat. Care Soc. Pract. 2021, 15, 26323524211017544. [Google Scholar] [CrossRef]
- Roy, U.B.; Elkins, I.; Petrillo, L.; Jacobson, M.; Feldman, J. Perception of Palliative Care and Prognostic Awareness of Lung Cancer Treatment in an Oncogene-Driven Lung Cancer Community. J. Thorac. Oncol. 2021, 16, S395–S396. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J.C. Conceptualizing Stigma. Annu. Rev. Sociol. 2001, 27, 363–385. [Google Scholar] [CrossRef]
- Andersen, M.M.; Varga, S.; Folker, A.P. On the definition of stigma. J. Eval. Clin. Pract. 2022, 28, 847–853. [Google Scholar] [CrossRef] [PubMed]
- Wittwer, H.; Schäfer, D.; Frewer, A. Handbuch Sterben und Tod. In Handbuch Sterben und Tod: Geschichte—Theorie—Ethik, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar] [CrossRef]
- Müller-Busch, H.C. Definitionen und Ziele in der Palliativmedizin. Internist 2011, 52, 7–14. [Google Scholar] [CrossRef] [PubMed]
- Lyons, B.; Dolezal, L. Shame, stigma and medicine. Med. Humanit. 2017, 43, 208–210. [Google Scholar] [CrossRef] [PubMed]
- Alcalde, J.; Zimmermann, C. Stigma about palliative care: Origins and solutions. Ecancermedicalscience 2022, 16, 1377. [Google Scholar] [CrossRef]
- Ryan, S.; Wong, J.; Chow, R.; Zimmermann, C. Evolving Definitions of Palliative Care: Upstream Migration or Confusion? Curr. Treat. Options Oncol. 2020, 21, 20. [Google Scholar] [CrossRef]
- World Health Organization. Palliative Care. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care (accessed on 22 September 2023).
- Parker, R. Stigma, prejudice and discrimination in global public health. Cad. Saúde Pública 2012, 28, 164–169. [Google Scholar] [CrossRef]
- Weiss, M.G.; Ramakrishna, J.; Somma, D. Health-related stigma: Rethinking concepts and interventions. Psychol. Health Med. 2006, 11, 277–287. [Google Scholar] [CrossRef]
- Scambler, G. Health-related stigma. Sociol. Health Illn. 2009, 31, 441–455. [Google Scholar] [CrossRef]
- Link, B.G.; Phelan, J.C. Stigma and its public health implications. Lancet 2006, 367, 528–529. [Google Scholar] [CrossRef]
- Noh, H.; Lee, L.H.; Won, C. Educational intervention to improve palliative care knowledge among informal caregivers of cognitively impaired older adults. Palliat. Support. Care 2021, 19, 515–523. [Google Scholar] [CrossRef]
- Baik, D.; Cho, H.; Creber, R.M.M. Examining Interventions Designed to Support Shared Decision Making and Subsequent Patient Outcomes in Palliative Care: A Systematic Review of the Literature. Am. J. Hosp. Palliat. Med. 2019, 36, 76–88. [Google Scholar] [CrossRef] [PubMed]
- Perry, L.M.; Sartor, O.; Malhotra, S.; Alonzi, S.; Kim, S.; Voss, H.M.; Rogers, J.L.; Robinson, W.; Harris, K.; Shank, J.; et al. Increasing Readiness for Early Integrated Palliative Oncology Care: Development and Initial Evaluation of the EMPOWER 2 Intervention. J. Pain Symptom Manag. 2021, 62, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Millum, J.; Campbell, M.; Luna, F.; Malekzadeh, A.; Karim, Q.A. Ethical challenges in global health-related stigma research. BMC Med. 2019, 17, 84. [Google Scholar] [CrossRef] [PubMed]
- Stutterheim, S.E.; Ratcliffe, S.E. Understanding and addressing stigma through qualitative research: Four reasons why we need qualitative studies. Stigma Health 2021, 6, 8–19. [Google Scholar] [CrossRef]
- Hartung, S.; Rosenbrock, R. Bundeszentrale für gesundheitliche Aufklärung (BZgA) (Hrsg.). Leitbegriffe der Gesundheitsförderung und Prävention; Köln, Germany, 2022. [Google Scholar] [CrossRef]
- Green, L.W.; Kreuter, M.W. Health program planning. In An Educational and Ecological Approach, 4th ed.; McGraw-Hill: Boston, MA, USA, 2005. [Google Scholar]
- Bartholomew Eldredge, L.K.; Markham, C.M.; Ruiter, R.A.C.; Fernández, M.E.; Kok, G.; Parcel, G.S. Planning health promotion programs. In An Intervention Mapping Approach, 4th ed.; Jossey-Bass: San Francisco, CA, USA, 2016. [Google Scholar]
- Stutterheim, S.E.; van der Kooij, Y.L.; Crutzen, R.; Ruiter, R.A.C.; Bos, A.E.R.; Kok, G. Intervention Mapping as a Guide to Developing, Implementing, and Evaluating Stigma Reduction Interventions. Stigma Health 2023. [Google Scholar] [CrossRef]
- Kemp, C.G.; Jarrett, B.A.; Kwon, C.-S.; Song, L.; Jetté, N.; Sapag, J.C.; Bass, J.; Murray, L.; Rao, D.; Baral, S. Implementation science and stigma reduction interventions in low- and middle-income countries: A systematic review. BMC Med. 2019, 17, 6. [Google Scholar] [CrossRef]
- Aulino, F.; Foley, K. The Project on Death in America. J. R. Soc. Med. 2001, 94, 492–495. [Google Scholar] [CrossRef]
- Seymour, J. The Impact of Public Health Awareness Campaigns on the Awareness and Quality of Palliative Care. J. Palliat. Med. 2018, 21, S30–S36. [Google Scholar] [CrossRef]
- Dying Matters Awareness Week. Available online: https://www.nptcvs.wales/2022/04/ (accessed on 22 September 2023).
- Hospiz Macht Schule. Available online: https://www.hospizmachtschule.de (accessed on 24 July 2024).
- Deutsche Gesellschaft für Palliativmedizin das ist Palliativ. Available online: https://www.dasistpalliativ.de/blog (accessed on 22 September 2023).
- Mallon, A.; Hasson, F.; Casson, K.; Slater, P.; McIlfatrick, S. Young adults understanding and readiness to engage with palliative care: Extending the reach of palliative care through a public health approach: A qualitative study. BMC Palliat. Care 2021, 20, 120. [Google Scholar] [CrossRef]
- Abel, T.; Hofmann, K.; Ackermann, S.; Bucher, S.; Sakarya, S. Health literacy among young adults: A short survey tool for public health and health promotion research. Health Promot. Int. 2015, 30, 725–735. [Google Scholar] [CrossRef]
- Batzler, Y.-N.; Schallenburger, M.; Schwartz, J.; Marazia, C.; Neukirchen, M. The General Public and Young Adults’ Knowledge and Perception of Palliative Care: A Systematic Review. Healthcare 2024, 12, 957. [Google Scholar] [CrossRef] [PubMed]
- Witzke, S. Jugendliche und junge Erwachsene—Eine Begriffsdefinition. In Carsharing und die Gesellschaft von Morgen; Springer Fachmedien Wiesbaden: Wiesbaden, Germany, 2016; pp. 17–18. [Google Scholar]
- Sawyer, J.M.; Higgs, P.; Porter, J.D.H.; Sampson, E.L. New public health approaches to palliative care, a brave new horizon or an impractical ideal? An Integrative literature review with thematic synthesis. Palliat. Care Soc. Pract. 2021, 15, 263235242110329. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, E. Development and Validation of the Palliative Care Knowledge Scale (PaCKS). Ph.D. Thesis, Washington University in St. Louis, St. Louis, MO, USA, 2016; p. 862. Available online: https://openscholarship.wustl.edu/art_sci_etds/862 (accessed on 31 December 2016).
- Kozlov, E.; Carpenter, B.D.; Rodebaugh, T.L. Development and validation of the Palliative Care Knowledge Scale (PaCKS). Palliat. Support. Care 2017, 15, 524–534. [Google Scholar] [CrossRef] [PubMed]
- Kozlov, E.; McDarby, M.; Reid, M.C.; Carpenter, B.D. Knowledge of Palliative Care Among Community-Dwelling Adults. Am. J. Hosp. Palliat. Med. 2018, 35, 647–651. [Google Scholar] [CrossRef] [PubMed]
- Raupach, T.; Münscher, C.; Beißbarth, T.; Burckhardt, G.; Pukrop, T. Towards outcome-based programme evaluation: Using student comparative self-assessments to determine teaching effectiveness. Med. Teach. 2011, 33, e446–e453. [Google Scholar] [CrossRef]
- Légaré, F.; Borduas, F.; Freitas, A.; Jacques, A.; Godin, G.; Luconi, F.; Grimshaw, J.; CPD-KT Team. Developing a theory-based instrument to assess the impact of continuing professional development activities on clinical practice: A study protocol. Implement. Sci. 2011, 6, 17. [Google Scholar] [CrossRef]
- Ayivi-Vinz, G.; Bakwa Kanyinga, F.; Bergeron, L.; Décary, S.; Adisso, É.L.; Zomahoun, H.T.V.; Daniel, S.J.; Tremblay, M.; Plourde, K.V.; Guay-Bélanger, S.; et al. Use of the CPD-REACTION Questionnaire to Evaluate Continuing Professional Development Activities for Health Professionals: Systematic Review. JMIR Med. Educ. 2022, 8, e36948. [Google Scholar] [CrossRef]
- McIlfatrick, S.; Roulston, N.K.; Hasson, A.; Mclaughlin, F.; Rutherford, G. Exploring public awareness and perceptions of palliative care: A qualitative study. Palliat. Med. 2013, 28, 273–280. [Google Scholar] [CrossRef]
- Bichu, P.B.; Abyraj, K.; Shaliet, R.S. Awareness and Self Reported Utilization Pattern of Community Palliative Care Units in a Rural Area in Central Kerala. Contemp. Social. Sci. 2020, 29, 17–26. [Google Scholar]
- Taubert, M.; Watts, G.; Boland, J.; Radbruch, L. Palliative social media. BMJ Support. Palliat. Care 2014, 4, 13–18. [Google Scholar] [CrossRef]
| Performance Objective | Knowledge | Attitude | Values |
|---|---|---|---|
| Young adults talk about palliative medicine | Young adults recall core elements of palliative medicine in conversation. | Young adults express positive feelings regarding palliative care for improving quality of life. | Young adults recognize that palliative medicine is life-affirming. |
| Young adults talk about death and dying | Young adults know that there are symptom control options in the dying phase and fears are unfounded. | Young adults recognize that an open approach to death and dying leads to better end-of-life care. | Young adults recognize that death and dying are integral parts of life. |
| Performance Objective | Knowledge | Attitude | Norms |
|---|---|---|---|
| Educational institutions enable training on palliative medicine | Detailed knowledge of palliative medicine is not known in the target population. | Palliative medicine is a relief for affected families. Young adults can focus on education. | Palliative medicine is a relevant medical discipline with equal importance as other disciplines. |
| Communities place posters in accessible locations | Communities are aware that knowledge about palliative medicine is only rudimentary in the general population. | Communities recognize that palliative medicine, like death and dying, is an integral part of the community. | Communities realize that palliative medicine should be sought earlier. |
| Interventionists distribute information on palliative care via the internet | Interventionists know about the specific needs of the target population. | Interventionists realize that the attitude of the target group must be altered. | Education on death, dying, and coping with diseases is as easily accessible as other content. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Batzler, Y.-N.; Schallenburger, M.; Schwartz, J.; Marazia, C.; Neukirchen, M. Destigmatizing Palliative Care among Young Adults—A Theoretical Intervention Mapping Approach. Healthcare 2024, 12, 1863. https://doi.org/10.3390/healthcare12181863
Batzler Y-N, Schallenburger M, Schwartz J, Marazia C, Neukirchen M. Destigmatizing Palliative Care among Young Adults—A Theoretical Intervention Mapping Approach. Healthcare. 2024; 12(18):1863. https://doi.org/10.3390/healthcare12181863
Chicago/Turabian StyleBatzler, Yann-Nicolas, Manuela Schallenburger, Jacqueline Schwartz, Chantal Marazia, and Martin Neukirchen. 2024. "Destigmatizing Palliative Care among Young Adults—A Theoretical Intervention Mapping Approach" Healthcare 12, no. 18: 1863. https://doi.org/10.3390/healthcare12181863
APA StyleBatzler, Y.-N., Schallenburger, M., Schwartz, J., Marazia, C., & Neukirchen, M. (2024). Destigmatizing Palliative Care among Young Adults—A Theoretical Intervention Mapping Approach. Healthcare, 12(18), 1863. https://doi.org/10.3390/healthcare12181863






