A Cross-Sectional Study Exploring the Relationship between Work-Related, Lifestyle Factors and Non-Specific Neck and Shoulder Pain in a Southeast Asian Population
Abstract
1. Introduction
2. Materials and Methods
Questionnaire Design
3. Sample Size Calculation and Statistical Analysis
4. Results
5. Discussion
Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Questions of the Survey in This Study
- What is your age (in years)?
- What is your gender?
- What is your height (in cm)?
- What is your weight (in kg)?
- Do you have any recent (<3 months) injury to the neck or shoulder region?
- Do you have any chronic (>3 months) injury to the neck or shoulder region?
- Do you have any existing auto-immune diseases such as those listed below? (select all that applies)
- Do you have other medical conditions/chronic illnesses? If yes, please state. -Selected Choice
- What is your total duration of computer use in a day (hours)?
- What is your total duration of smartphone use in a day (hours)?
- On average, how many hours do you work or study in a sitting position daily?
- On average, how many hours do you sleep daily?
- How many cigarettes do you smoke daily? (in number of sticks) (Put 0 if you do not smoke)
- Do you consume alcohol?
- How many days do you exercise in a week?
- How long do you exercise per day (hours)?
- Presence of neck or shoulder pain (Yes/No)
- Please rate your level of pain experienced in your neck and shoulder region. (0—no pain at all; 100—extreme and unimaginable pain ever experienced—Pain rating scale
- Do you participate in regular sports activities or exercises?
- How many hours do you participate in sports activities or exercise (include aerobic exercise) in a week?
- Out of the total number of hours you exercise in a week, how many of those hours are aerobic exercises?
- (Aerobic activities are activities that cause a noticeable increase in breathing rate and heart rate. This means that you will be able to carry on a conversation but will not have enough breath to sing. e.g.,: brisk walking/swimming/cycling/jogging/rowing/dancing etc.) If not applicable, put down 0
- Do you have any history of cardiovascular diseases? For example, abnormal blood pressure, heart diseases, stroke etc.
- Do your parents or siblings have any cardiovascular disease mentioned above?
- Are you taking any medications this week? Put down the type of medication (e.g., Painkiller, anti-inflammatory).
References
- Chan, L.L.Y.; Wong, A.Y.L.; Wang, M.H.; Cheung, K.; Samartzis, D. The prevalence of neck pain and associated risk factors among undergraduate students: A large-scale cross-sectional study. Int. J. Ind. Ergon. 2020, 76, 102934. [Google Scholar] [CrossRef]
- Woo, E.H.C.; White, P.; Lai, C.W.K. Musculoskeletal impact of the use of various types of electronic devices on university students in Hong Kong: An evaluation by means of self-reported questionnaire. Man. Ther. 2016, 26, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Hey, H.W.D.; Lim, J.X.Y.; Ong, J.Z.; Luo, N. Epidemiology of Neck Pain and Its Impact on Quality-of-Life—A Population-Based, Cross Sectional Study in Singapore. Spine 2021, 46, 1572–1580. [Google Scholar] [CrossRef] [PubMed]
- Hakala, P.T.; Rimpelä, A.H.; Saarni, L.A.; Salminen, J.J. Frequent computer-related activities increase the risk of neck–shoulder and low back pain in adolescents. Eur. J. Public Health 2006, 16, 536–541. [Google Scholar] [CrossRef]
- Yang, S.-Y.; Chen, M.-D.; Huang, Y.-C.; Lin, C.-Y.; Chang, J.-H. Association Between Smartphone Use and Musculoskeletal Discomfort in Adolescent Students. J. Community Health 2017, 42, 423–430. [Google Scholar] [CrossRef]
- Yue, P.; Liu, F.; Li, L. Neck/shoulder pain and low back pain among school teachers in China, prevalence and risk factors. BMC Public Health 2012, 12, 789. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Randhawa, K.; Yu, H.; Côté, P.; Haldeman, S. The Global Spine Care Initiative: A summary of the global burden of low back and neck pain studies. Eur. Spine J. 2018, 27, 796–801. [Google Scholar] [CrossRef]
- Myrtveit, S.M.; Sivertsen, B.; Skogen, J.C.; Frostholm, L.; Stormark, K.M.; Hysing, M. Adolescent Neck and Shoulder Pain—The Association With Depression, Physical Activity, Screen-Based Activities, and Use of Health Care Services. J. Adolesc. Health 2014, 55, 366–372. [Google Scholar] [CrossRef]
- Russell, R.D.; Knight, J.R.; Mulligan, E.; Khazzam, M.S. Structural Integrity After Rotator Cuff Repair Does Not Correlate with Patient Function and Pain. J. Bone Jt. Surg. 2014, 96, 265–271. [Google Scholar] [CrossRef]
- Slabaugh, M.A.; Nho, S.J.; Grumet, R.C.; Wilson, J.B.; Seroyer, S.T.; Frank, R.M.; Romeo, A.A.; Provencher, M.T.; Verma, N.N. Does the Literature Confirm Superior Clinical Results in Radiographically Healed Rotator Cuffs After Rotator Cuff Repair? Arthrosc. J. Arthrosc. Relat. Surg. 2010, 26, 393–403. [Google Scholar] [CrossRef]
- Tran, G.; Cowling, P.; Smith, T.; Bury, J.; Lucas, A.; Barr, A.; Kingsbury, S.R.; Conaghan, P.G. What Imaging-Detected Pathologies Are Associated With Shoulder Symptoms and Their Persistence? A Systematic Literature Review. Arthritis Care Res. 2018, 70, 1169–1184. [Google Scholar] [CrossRef] [PubMed]
- Hegedus, E.J.; Cook, C.; Lewis, J.; Wright, A.; Park, J.-Y. Combining orthopedic special tests to improve diagnosis of shoulder pathology. Phys. Ther. Sport 2015, 16, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Nordin, M.; Carragee, E.J.; Hogg-Johnson, S.; Weiner, S.S.; Hurwitz, E.L.; Peloso, P.M.; Guzman, J.; van der Velde, G.; Carroll, L.J.; Holm, L.W.; et al. Assessment of Neck Pain and Its Associated Disorders. J. Manip. Physiol. Ther. 2009, 32, S117–S140. [Google Scholar] [CrossRef] [PubMed]
- van Kampen, D.A.; van den Berg, T.; van der Woude, H.J.; Castelein, R.M.; Scholtes, V.A.B.; Terwee, C.B.; Willems, W.J. The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J. Orthop. Surg. Res. 2014, 9, 70. [Google Scholar] [CrossRef]
- Namwongsa, S.; Puntumetakul, R.; Neubert, M.S.; Boucaut, R. Factors associated with neck disorders among university student smartphone users. Work 2018, 61, 367–378. [Google Scholar] [CrossRef]
- Kanchanomai, S.; Janwantanakul, P.; Pensri, P.; Jiamjarasrangsi, W. Risk factors for the onset and persistence of neck pain in undergraduate students: 1-year prospective cohort study. BMC Public Health 2011, 11, 566. [Google Scholar] [CrossRef]
- Auvinen, J.P.; Tammelin, T.H.; Taimela, S.P.; Zitting, P.J.; Järvelin, M.-R.; Taanila, A.M.; Karppinen, J.I. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur. Spine J. 2010, 19, 641–649. [Google Scholar] [CrossRef]
- Carter, S.E.; Draijer, R.; Holder, S.M.; Brown, L.; Thijssen, D.H.J.; Hopkins, N.D. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J. Appl. Physiol. 2018, 125, 790–798. [Google Scholar] [CrossRef]
- Dempsey, P.C.; Larsen, R.N.; Dunstan, D.W.; Owen, N.; Kingwell, B.A. Sitting Less and Moving More. Hypertension 2018, 72, 1037–1046. [Google Scholar] [CrossRef]
- Ng, I.Y.H.; Lim, S.S.; Pang, N. Making universal digital access universal: Lessons from COVID-19 in Singapore. Univers. Access Inf. Soc. 2023, 22, 1073–1083. [Google Scholar] [CrossRef]
- Rudolph, J.; Tan, S.; Crawford, J.; Butler-Henderson, K. Perceived quality of online learning during COVID-19 in higher education in Singapore: Perspectives from students, lecturers, and academic leaders. Educ. Res. Policy Pract. 2023, 22, 171–191. [Google Scholar] [CrossRef] [PubMed]
- Watermeyer, R.; Chen, Z.; Ang, B.J. ‘Education without limits’: The digital resettlement of post-secondary education and training in Singapore in the COVID-19 era. J. Educ. Policy 2022, 37, 861–882. [Google Scholar] [CrossRef]
- Rangaswamy, E.; Nawaz, N.; Lu, E. Impact of COVID-19 on Singapore human resource practices. Cogent Bus. Manag. 2024, 11, 2301791. [Google Scholar] [CrossRef]
- Bertozzi, L.; Negrini, S.; Agosto, D.; Costi, S.; Guccione, A.A.; Lucarelli, P.; Villafañe, J.H.; Pillastrini, P. Posture and time spent using a smartphone are not correlated with neck pain and disability in young adults: A cross-sectional study. J. Bodyw. Mov. Ther. 2021, 26, 220–226. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Coombes, B.K.; Sjøgaard, G.; Jun, D.; O’Leary, S.; Johnston, V. Workplace-Based Interventions for Neck Pain in Office Workers: Systematic Review and Meta-Analysis. Phys. Ther. 2018, 98, 40–62. [Google Scholar] [CrossRef]
- Moreira-Silva, I.; Teixeira, P.M.; Santos, R.; Abreu, S.; Moreira, C.; Mota, J. The Effects of Workplace Physical Activity Programs on Musculoskeletal Pain. Workplace Health Saf. 2016, 64, 210–222. [Google Scholar] [CrossRef]
- Palacios-Ceña, D.; Albaladejo-Vicente, R.; Hernández-Barrera, V.; Lima-Florencio, L.; Fernández-de-las-Peñas, C.; Jimenez-Garcia, R.; López-de-Andrés, A.; de Miguel-Diez, J.; Perez-Farinos, N. Female Gender Is Associated with a Higher Prevalence of Chronic Neck Pain, Chronic Low Back Pain, and Migraine: Results of the Spanish National Health Survey, 2017. Pain Med. 2021, 22, 382–395. [Google Scholar] [CrossRef]
- Mann, C.J. Observational research methods—Cohort studies, cross sectional studies, and case–control studies. Afr. J. Emerg. Med. 2012, 2, 38–46. [Google Scholar] [CrossRef]
- Peterson, G.; Pihlström, N. Factors associated with neck and shoulder pain: A cross-sectional study among 16,000 adults in five county councils in Sweden. BMC Musculoskelet. Disord. 2021, 22, 872. [Google Scholar] [CrossRef]
- Caruana, E.J.; Roman, M.; Hernández-Sánchez, J.; Solli, P. Longitudinal studies. J. Thorac. Dis. 2015, 7, E537–E540. [Google Scholar] [CrossRef]
- Sihawong, R.; Janwantanakul, P.; Jiamjarasrangsi, W. Effects of an exercise programme on preventing neck pain among office workers: A 12-month cluster-randomised controlled trial. Occup. Environ. Med. 2014, 71, 63–70. [Google Scholar] [CrossRef] [PubMed]
- Fanavoll, R.; Nilsen, T.I.; Holtermann, A.; Mork, P.J. Psychosocial work stress, leisure time physical exercise and the risk of chronic pain in the neck/shoulders: Longitudinal data from the Norwegian HUNT Study. Int. J. Occup. Med. Environ. Health 2016, 29, 585–595. [Google Scholar] [CrossRef] [PubMed]
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, L.H.; Bigal, M.E.; Katz, M.; Derby, C.; Lipton, R.B. Chronic Pain and Obesity in Elderly People: Results from the Einstein Aging Study. J. Am. Geriatr. Soc. 2009, 57, 115–119. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.; Zdziarski, L.; Wasser, J. Chronic pain management in the obese patient: A focused review of key challenges and potential exercise solutions. J. Pain Res. 2015, 63, 63–77. [Google Scholar] [CrossRef]
- Farrell, S.F.; de Zoete, R.M.J.; Cabot, P.J.; Sterling, M. Systemic inflammatory markers in neck pain: A systematic review with meta-analysis. Eur. J. Pain 2020, 24, 1666–1686. [Google Scholar] [CrossRef]
- Blake, P.; Burstein, R. Emerging evidence of occipital nerve compression in unremitting head and neck pain. J. Headache Pain 2019, 20, 76. [Google Scholar] [CrossRef]
- Peng, B.; DePalma, M.J. Cervical disc degeneration and neck pain. J. Pain Res. 2018, 11, 2853–2857. [Google Scholar] [CrossRef]
- Childress, M.A.; Stuek, S.J. Neck Pain: Initial Evaluation and Management. Am. Fam. Physician 2020, 102, 150–156. [Google Scholar]
- Lin, C.-C.; Hua, S.-H.; Lin, C.-L.; Cheng, C.-H.; Liao, J.-C.; Lin, C.-F. Impact of Prolonged Tablet Computer Usage with Head Forward and Neck Flexion Posture on Pain Intensity, Cervical Joint Position Sense and Balance Control in Mechanical Neck Pain Subjects. J. Med. Biol. Eng. 2020, 40, 372–382. [Google Scholar] [CrossRef]
- Brandt, M.; Sundstrup, E.; Jakobsen, M.D.; Jay, K.; Colado, J.C.; Wang, Y.; Zebis, M.K.; Andersen, L.L. Association between Neck/Shoulder Pain and Trapezius Muscle Tenderness in Office Workers. Pain Res. Treat. 2014, 2014, 352735. [Google Scholar] [CrossRef] [PubMed]
- Bárány, I.; Vu, V. Central limit theorems for Gaussian polytopes. Ann. Probab. 2007, 35, 1593–1621. [Google Scholar] [CrossRef]
- Buse, J.H.M.; Fong, C.; Tripathi, S. The Interplay of Social Behaviour and Demographics in Cyber Scam Susceptibility: A Singapore Study. Open J. Bus. Manag. 2024, 12, 2949–2964. [Google Scholar] [CrossRef]
| NSNSP Group | Comparison Group | Independent t-Test/Chi-Square Test | |
|---|---|---|---|
| Age | n = 212 31.49 ± 10.57 | n = 90 31.34 ± 13.67 | p = 0.93 |
| Gender (Male/Female) *# | Male: 45 (21.2%) Female: 163 (76.9%) Non-binary/Prefer not to say: 4 (1.9%) | Male: 34 (37.8%) Female: 55 (61.1%) Non-binary/Prefer not to say: 1 (1.1%) | * p = 0.02 |
| BMI (kg/m2) | n = 212 22.66 ± 4.05 | n = 90 22.55 ± 3.83 | p = 0.82 |
| Computer use (h/day) | n = 203 6.0 ± 3.54 | n = 88 5.8 ± 3.65 | p = 0.67 |
| Smartphone use (h/day) * | n = 205 5.37 ± 3.50 | n = 89 4.46 ± 3.36 | * p = 0.04 |
| Sitting position (h/day) | n = 204 6.96 ± 3.37 | n = 89 6.34 ± 3.44 | p = 0.15 |
| Sleep (h/day) | n = 208 6.49 ± 1.33 | n = 88 6.47 ± 1.66 | p = 0.88 |
| Exercise frequency (days/week) * | n = 211 2.10 ± 1.74 | n = 89 2.93 ± 2.21 | * p < 0.01 |
| Daily exercise duration (h/day) | n = 205 0.97 ± 0.78 | n = 87 1.08 ± 0.81 | p = 0.442 |
| Weekly exercise duration (h/week) * | n = 205 2.69 ± 3.05 | n = 87 4.11 ± 4.15 | * p < 0.01 |
| Aerobic exercise (h/week) | n = 127 2.16 ± 1.96 | n = 64 2.64 ± 2.93 | p = 0.24 |
| Drinking | n = 212 Non-drinker = 87 (41%) Social drinker = 114 (53.8%) Drink weekly = 9 (4.2%) Drink daily = 2 (0.9%) | n = 90 Non-drinker = 44 (48.9%) Social drinker = 42 (46.7%) Drink weekly = 3 (3.3%) Drink daily = 1 (1.1%) | p = 0.65 |
| History of cardiovascular disease | Yes = 23 (10.8%) No = 173 (88.2%) | Yes = 14 (15.6%) No = 75 (84.4%) | p = 0.35 |
| Family history of cardiovascular disease | Yes = 76 (35.8%) No = 120 (64.2%) | Yes = 29 (32.2%) No = 60 (67.8%) | p = 0.32 |
| Dependent Variable | Factor | Partial Eta Squared | F-Value | p-Value |
|---|---|---|---|---|
| Computer use (h/day) | Age | 0.00 | 0.04 | 0.85 |
| Gender | 0.00 | 0.35 | 0.56 | |
| Presence of NSNSP | 0.00 | 0.27 | 0.60 | |
| Smartphone use (h/day) | * Age | 0.02 | 5.08 | 0.03 * |
| Gender | 0.01 | 2.20 | 0.14 | |
| Presence of NSNSP | 0.01 | 3.40 | 0.07 | |
| Sitting position (h/day) | Age | 0.01 | 2.65 | 0.10 |
| Gender | 0.00 | 0.06 | 0.80 | |
| Presence of NSNSP | 0.01 | 1.98 | 0.16 | |
| Sleep (h/day) | Age | 0.00 | 0.24 | 0.62 |
| Gender | 0.00 | 0.94 | 0.33 | |
| Presence of NSNSP | 0.00 | 0.09 | 0.77 | |
| Exercise frequency (days/week) | * Age | 0.02 | 6.11 | 0.01 * |
| * Gender | 0.04 | 13.3 | <0.01 * | |
| * Presence of NSNSP | 0.03 | 8.55 | <0.01 * | |
| Daily exercise duration (h/day) | * Age | 0.02 | 6.19 | 0.01 * |
| * Gender | 0.03 | 7.46 | 0.01 * | |
| Presence of NSNSP | 0.00 | 0.48 | 0.49 | |
| Weekly exercise duration (h/week) | * Age | 0.06 | 17.64 | <0.01 * |
| * Gender | 0.02 | 6.97 | 0.02 * | |
| Presence of NSNSP | 0.00 | 6.97 | 0.57 | |
| Aerobic exercise (h/week) | Age | 0.00 | 0.59 | 0.45 |
| Gender | 0.01 | 1.28 | 0.26 | |
| Presence of NSNSP | 0.01 | 1.48 | 0.23 | |
| Drinking | Age | 0.00 | 0.06 | 0.81 |
| * Gender | 0.02 | 4.50 | 0.04 | |
| Presence of NSNSP | 0.00 | 0.31 | 0.58 | |
| History of cardiovascular disease | Age | 0.00 | 0.4 | 0.53 |
| * Gender | 0.02 | 5.66 | 0.02 * | |
| Presence of NSNSP | 0.00 | 0.27 | 0.61 | |
| Family history of cardiovascular disease | * Age | 0.02 | 6.43 | 0.01 * |
| Gender | 0.00 | 0.06 | 0.8 | |
| Presence of NSNSP | 0.00 | 1.06 | 0.30 |
| Variable | Correlation (r) | p-Value |
|---|---|---|
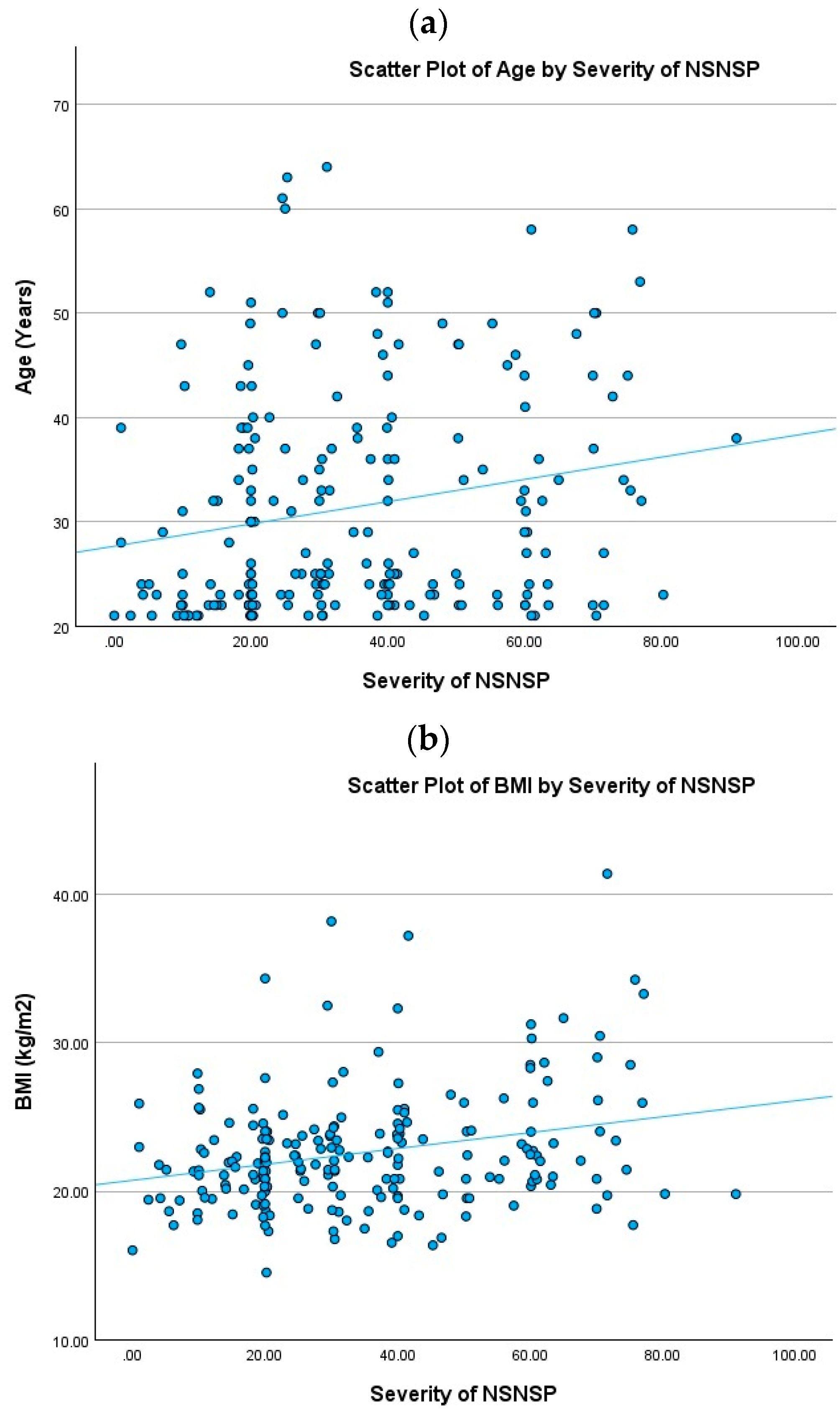
| Age ** | 0.201 | <0.01 |
| BMI ** | 0.266 | <0.01 |
| Computer use (h/day) | −0.002 | >0.05 |
| Smartphone use (h/day) | −0.017 | >0.05 |
| Sitting position (h/day) | 0.000 | >0.05 |
| Sleep (h/day) | −0.126 | >0.05 |
| Exercise (days/week) | 0.090 | >0.05 |
| Exercise (h/day) | 0.098 | >0.05 |
| Exercise (h/week) | 0.081 | >0.05 |
| Aerobic (h/week) | 0.133 | >0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lo, C.N.; Teo, V.Y.E.; Manaff, N.F.A.B.A.; Seow, T.C.-Y.; Harve, K.S.; Leung, B.P.L. A Cross-Sectional Study Exploring the Relationship between Work-Related, Lifestyle Factors and Non-Specific Neck and Shoulder Pain in a Southeast Asian Population. Healthcare 2024, 12, 1861. https://doi.org/10.3390/healthcare12181861
Lo CN, Teo VYE, Manaff NFABA, Seow TC-Y, Harve KS, Leung BPL. A Cross-Sectional Study Exploring the Relationship between Work-Related, Lifestyle Factors and Non-Specific Neck and Shoulder Pain in a Southeast Asian Population. Healthcare. 2024; 12(18):1861. https://doi.org/10.3390/healthcare12181861
Chicago/Turabian StyleLo, Chi Ngai, Victoria Yu En Teo, Nur Farah Ain Binte Abdul Manaff, Tessa Chu-Yu Seow, Karthik Subramhanya Harve, and Bernard Pui Lam Leung. 2024. "A Cross-Sectional Study Exploring the Relationship between Work-Related, Lifestyle Factors and Non-Specific Neck and Shoulder Pain in a Southeast Asian Population" Healthcare 12, no. 18: 1861. https://doi.org/10.3390/healthcare12181861
APA StyleLo, C. N., Teo, V. Y. E., Manaff, N. F. A. B. A., Seow, T. C.-Y., Harve, K. S., & Leung, B. P. L. (2024). A Cross-Sectional Study Exploring the Relationship between Work-Related, Lifestyle Factors and Non-Specific Neck and Shoulder Pain in a Southeast Asian Population. Healthcare, 12(18), 1861. https://doi.org/10.3390/healthcare12181861






