Spatial Analysis of Health System Factors in Infectious Disease Management: Lessons Learned from the COVID-19 Pandemic in Korea
Abstract
1. Introduction
2. Methods
2.1. Study Design and Data Sources
2.2. Variables
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
3.1. Descriptive Statistics
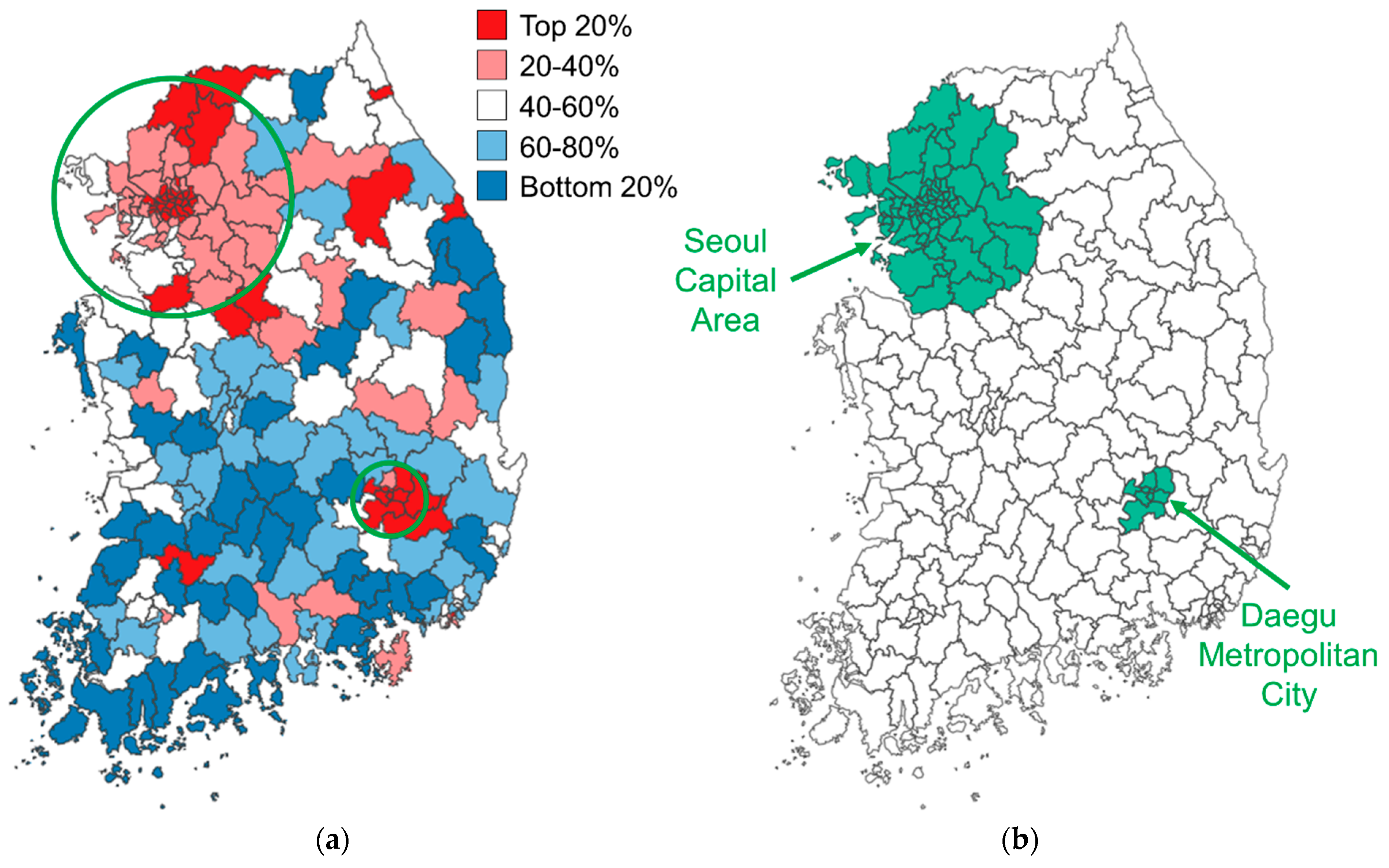
3.2. Geographical Distribution of Confirmed COVID-19 Cases
3.3. Correlation Analysis Results
3.4. Regression Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Nuzzo, J.B.; Meyer, D.; Snyder, M.; Ravi, S.J.; Lapascu, A.; Souleles, J.; Andrada, C.I.; Bishai, D. What makes health systems resilient against infectious disease outbreaks and natural hazards? Results from a scoping review. BMC Public Health 2019, 19, 1310. [Google Scholar] [CrossRef] [PubMed]
- Burrowes, S.A.; Casey, S.M.; Pierre-Joseph, N.; Talbot, S.G.; Hall, T.; Christian-Brathwaite, N.; Del-Carmen, M.; Garofalo, C.; Lundberg, B.; Mehta, P.K.; et al. COVID-19 pandemic impacts on mental health, burnout, and longevity in the workplace among healthcare workers: A mixed methods study. J. Interprofessional Educ. Pract. 2023, 32, 100661. [Google Scholar] [CrossRef] [PubMed]
- Lazenby, M.; Chambers, S.; Chyun, D.; Davidson, P.; Dithole, K.; Norman, I.; Tlou, S. Clinical nursing and midwifery education in the pandemic age. Int. Nurs. Rev. 2020, 67, 323–325. [Google Scholar] [CrossRef] [PubMed]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S.; et al. Health systems resilience in managing the COVID-19 pandemic: Lessons from 28 countries. Nat. Med. 2021, 27, 964–980. [Google Scholar] [CrossRef] [PubMed]
- Meena, P.; Abdellatif, D.; Tiwari, V.; Chatterjee, S.; Luyckx, V.A. Health Systems Preparedness for Infectious Disease Outbreaks: Relevance for Nephrology. Semin. Nephrol. 2023, 43, 151465. [Google Scholar] [CrossRef] [PubMed]
- Craciun, O.M.; Del Rosario Torres, M.; Llanes, A.B.; Romay-Barja, M. Tuberculosis Knowledge, Attitudes, and Practice in Middle- and Low-Income Countries: A Systematic Review. J. Trop. Med. 2023, 2023, 1014666. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Bowers, K.; Zhu, D.; Gao, X.; Cheng, T. Spatio-temporal stratified associations between urban human activities and crime patterns: A case study in San Francisco around the COVID-19 stay-at-home mandate. Comput. Urban Sci. 2022, 2, 13. [Google Scholar] [CrossRef] [PubMed]
- Chiesa, V.; Antony, G.; Wismar, M.; Rechel, B. COVID-19 pandemic: Health impact of staying at home, social distancing and ‘lockdown’ measures—A systematic review of systematic reviews. J. Public Health 2021, 43, e462–e481. [Google Scholar] [CrossRef] [PubMed]
- Baker, R.E.; Mahmud, A.S.; Miller, I.F.; Rajeev, M.; Rasambainarivo, F.; Rice, B.L.; Takahashi, S.; Tatem, A.J.; Wagner, C.E.; Wang, L.F.; et al. Infectious disease in an era of global change. Nat. Rev. Microbiol. 2022, 20, 193–205. [Google Scholar] [CrossRef]
- Sarmadi, M.; Marufi, N.; Moghaddam, V.K. Association of COVID-19 global distribution and environmental and demographic factors: An updated three-month study. Environ. Res. 2020, 188, 109748. [Google Scholar] [CrossRef]
- Meyer, D.; Bishai, D.; Ravi, S.J.; Rashid, H.; Mahmood, S.S.; Toner, E.; Nuzzo, J.B. A checklist to improve health system resilience to infectious disease outbreaks and natural hazards. BMJ Glob. Health 2020, 5, e002429. [Google Scholar] [CrossRef]
- KDCA (Korea Disease Control and Prevention Agency). Number of Confirmed COVID-19 Cases by City; KDCA: Cheongju, Republic of Korea, 2024; unpublished raw data.
- KOSIS (Korean Statistical Information Service). 2024. Available online: https://kosis.kr (accessed on 12 June 2024).
- KTDB (Korea Transport Database). Estimated Traffic Volume by Administrative District [Data File]. 2024. Available online: https://www.ktdb.go.kr (accessed on 12 June 2024).
- Cuadros, D.F.; Branscum, A.J.; Mukandavire, Z.; Miller, F.D.; MacKinnon, N. Dynamics of the COVID-19 epidemic in urban and rural areas in the United States. Ann. Epidemiol. 2021, 59, 16–20. [Google Scholar] [CrossRef]
- Yang, S.; Jang, J.; Park, S.; Ahn, S.; Kim, S.; Park, S.; Ryu, B.; Lee, S.; Shin, E.; Kim, N.; et al. Two-year report of COVID-19 outbreak from January 20, 2020 to January 19, 2022 in the Republic of Korea. Public Health Wkly. Rep. 2022, 2022, 414–426. [Google Scholar]
- WHO (World Health Organization). Health Systems Strengthening Glossary. Available online: https://cdn.who.int/media/docs/default-source/documents/health-systems-strengthening-glossary.pdf (accessed on 20 June 2024).
- WHO (World Health Organization). Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies; World Health Organization: Geneva, Switzerland, 2010.
- Liu, L. Study on the spatial decomposition of the infection probability of COVID-19. Sci. Rep. 2023, 13, 13258. [Google Scholar] [CrossRef] [PubMed]
- Franzese, R.J.; Hays, J.C. Spatial Econometric Models of Cross-Sectional Interdependence in Political Science Panel and Time-Series-Cross-Section Data. Political Anal. 2007, 15, 140–164. [Google Scholar] [CrossRef]
- Anselin, L. Spatial Econometrics. In A Companion to Theoretical Econometrics; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2003; pp. 310–330. [Google Scholar] [CrossRef]
- Pace, R.K.; LeSage, J.P. Omitted Variable Biases of OLS and Spatial Lag Models. In Advances in Spatial Science; Springer: Berlin/Heidelberg, Germany, 2009; pp. 17–28. [Google Scholar] [CrossRef]
- Cook, S.J.; An, S.H.; Favero, N. Beyond Policy Diffusion: Spatial Econometric Models of Public Administration. J. Public Adm. Res. Theory 2018, 29, 591–608. [Google Scholar] [CrossRef]
- Anselin, L.; Bera, A.K.; Florax, R.; Yoon, M.J. Simple diagnostic tests for spatial dependence. Reg. Sci. Urban Econ. 1996, 26, 77–104. [Google Scholar] [CrossRef]
- Bera, A.K.; Yoon, M.J. Specification Testing with Locally Misspecified Alternatives. Econom. Theory 1993, 9, 649–658. [Google Scholar] [CrossRef]
- Department of Health and Human Services. Federal Policy for the Protection of Human Subjects. 2017. Available online: https://www.federalregister.gov/d/2017-01058/p-332 (accessed on 28 May 2024).
- Akaike, H. Information theory and an extension of the maximum likelihood principle. In Proceedings of the 2nd International Symposium on Information Theory; Petrov, B.N., Csaki, F., Eds.; Akademiai Kiado: Budapest, Hungary, 1973; pp. 267–281. [Google Scholar]
- LeSage, J.; Pace, R.K. Introduction to Spatial Econometrics; Chapman and Hall: New York, NY, USA; CRC: New York, NY, USA, 2009. [Google Scholar] [CrossRef]
- Schwarz, G. Estimating the Dimension of a Model. Ann. Stat. 1978, 6, 461–464. [Google Scholar] [CrossRef]
- Anselin, L. Under the hood: Issues in the specification and interpretation of spatial regression models. Agric. Econ. 2002, 27, 247–267. [Google Scholar] [CrossRef]
- Adetokunboh, O.O.; Are, E.B. Spatial distribution and determinants of HIV high burden in the Southern African sub-region. PLoS ONE 2024, 19, e0301850. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, M.C.C.; Ferreira, A.F.; Da Silva Filho, J.D.; Da Silveira Lima, M.; Martins-Melo, F.R.; Bezerra, F.S.M.; Sousa, M.S.; Ramos, A.N. Burden of schistosomiasis-related mortality in Brazil: Epidemiological patterns and spatial–temporal distribution, 2003–2018. Trop. Med. Int. Health 2020, 25, 1395–1407. [Google Scholar] [CrossRef] [PubMed]
- Tang, X.; Xie, X.; Rao, Z.; Zheng, Z.; Hu, C.; Li, S.; Hu, Z. Spatial Analysis and Comparison of the Economic Burden of Common Diseases: An Investigation of 5.7 Million Rural Elderly Inpatients in Southeast China, 2010–2016. Front. Public Health 2021, 9, 774342. [Google Scholar] [CrossRef] [PubMed]
- Andrés-Rosales, R.; Quintana-Romero, L.; De Jesús-Almonte, L.; De La Cruz Del Río-Rama, M. Spatial spillovers of economic growth and public spending in Mexico: Evidence from a SpVAR model, 1999–2019. Econ. Anal. Policy 2021, 71, 660–673. [Google Scholar] [CrossRef]
- Chih, Y.; Kishan, R.P.; Ojede, A. Be good to thy neighbours: A spatial analysis of foreign direct investment and economic growth in sub-Saharan Africa. World Econ. 2021, 45, 657–701. [Google Scholar] [CrossRef]
- Ren, Y.; Ren, X.; Hu, J. Driving factors of China’s city-level carbon emissions from the perspective of spatial spillover effect. Carbon Manag. 2019, 10, 551–566. [Google Scholar] [CrossRef]
- Wells, K.; O’Hara, R.B.; Morand, S.; Lessard, J.P.; Ribas, A. The importance of parasite geography and spillover effects for global patterns of host–parasite associations in two invasive species. Divers. Distrib. 2014, 21, 477–486. [Google Scholar] [CrossRef]
- Mitchell, J.L. Does Policy Diffusion Need Space? Spatializing the Dynamics of Policy Diffusion. Policy Stud. J. 2017, 46, 424–451. [Google Scholar] [CrossRef]
- Song, Z.; Wang, C.; Bergmann, L. China’s prefectural digital divide: Spatial analysis and multivariate determinants of ICT diffusion. Int. J. Inf. Manag. 2020, 52, 102072. [Google Scholar] [CrossRef]
- Campedelli, G.M.; Favarin, S.; Aziani, A.; Piquero, A.R. Disentangling community-level changes in crime trends during the COVID-19 pandemic in Chicago. Crime Sci. 2020, 9, 21. [Google Scholar] [CrossRef]
- Yang, M.; Chen, Z.; Zhou, M.; Liang, X.; Bai, Z. The Impact of COVID-19 on Crime: A Spatial Temporal Analysis in Chicago. ISPRS Int. J. Geo-Inf. 2021, 10, 152. [Google Scholar] [CrossRef]
- Wang, J.; Yang, X.; Kumari, S. Investigating the Spatial Spillover Effect of Transportation Infrastructure on Green Total Factor Productivity. Energies 2023, 16, 2733. [Google Scholar] [CrossRef]
- Yu, N.; De Jong, M.; Storm, S.; Mi, J. Spatial spillover effects of transport infrastructure: Evidence from Chinese regions. J. Transp. Geogr. 2013, 28, 56–66. [Google Scholar] [CrossRef]
- Kim, D. Exploratory study on the spatial relationship between emerging infectious diseases and urban characteristics: Cases from Korea. Sustain. Cities Soc. 2021, 66, 102672. [Google Scholar] [CrossRef]
- Hamidi, S.; Ewing, R.; Sabouri, S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: Early evidence from 1,165 metropolitan counties in the United States. Health Place 2020, 64, 102378. [Google Scholar] [CrossRef] [PubMed]
- Ehlert, A. The socio-economic determinants of COVID-19: A spatial analysis of German county level data. Socio-Econ. Plan. Sci. 2021, 78, 101083. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Villamizar, L.A.; Belalcázar-Ceron, L.C.; Fernández-Niño, J.A.; Marín-Pineda, D.M.; Rojas-Sánchez, O.A.; Acuña-Merchán, L.A.; Ramírez-García, N.; Mangones-Matos, S.C.; Vargas-González, J.M.; Herrera-Torres, J.; et al. Air pollution, sociodemographic and health conditions effects on COVID-19 mortality in Colombia: An ecological study. Sci. Total Environ. 2021, 756, 144020. [Google Scholar] [CrossRef] [PubMed]
- Jo, Y.; Hong, A.; Sung, H. Density or Connectivity: What Are the Main Causes of the Spatial Proliferation of COVID-19 in Korea? Int. J. Environ. Res. Public Health 2021, 18, 5084. [Google Scholar] [CrossRef] [PubMed]
- Van Iseghem, T.; Jacobs, I.; Vanden Bossche, D.; Delobelle, P.; Willems, S.; Masquillier, C.; Decat, P. The role of community health workers in primary healthcare in the WHO-EU region: A scoping review. Int. J. Equity Health 2023, 22, 134. [Google Scholar] [CrossRef]
- Hartzler, A.L.; Tuzzio, L.; Hsu, C.; Wagner, E.H. Roles and Functions of Community Health Workers in Primary Care. Ann. Fam. Med. 2018, 16, 240–245. [Google Scholar] [CrossRef]
- Cook, N.; McGrath, B.M.; Navale, S.M.; Koroukian, S.M.; Templeton, A.R.; Crocker, L.C.; Zyzanski, S.J.; Bensken, W.P.; Stange, K.C. Care Delivery in Community Health Centers Before, During, and After the COVID-19 Pandemic (2019–2022). J. Am. Board Fam. Med. 2023, 36, 916–926. [Google Scholar] [CrossRef] [PubMed]
- Meador, M.; Coronado, F.; Roy, D.; Bay, R.C.; Lewis, J.H.; Chen, J.; Cheung, R.; Utman, C.; Hannan, J.A. Impact of COVID-19-related care disruptions on blood pressure management and control in community health centers. BMC Public Health 2022, 22, 2295. [Google Scholar] [CrossRef]
- De Foo, C.; Verma, M.; Tan, S.Y.; Hamer, J.; Van Der Mark, N.; Pholpark, A.; Hanvoravongchai, P.; Cheh, P.L.J.; Marthias, T.; Mahendradhata, Y.; et al. Health financing policies during the COVID-19 pandemic and implications for universal health care: A case study of 15 countries. Lancet Glob. Health 2023, 11, e1964–e1977. [Google Scholar] [CrossRef] [PubMed]
- Swann, W.L.; DiNardi, M.; Schreiber, T.L. Association Between Interorganizational Collaboration in Opioid Response and Treatment Capacity for Opioid Use Disorder in Counties of Five States: A Cross-Sectional Study. Subst. Abus. 2022, 16, 117822182211119. [Google Scholar] [CrossRef] [PubMed]
- Langabeer, J.R.; Champagne-Langabeer, T.; Helton, J.R.; Segrest, W.; Kash, B.; DelliFraine, J.; Fowler, R. Interorganizational Collaboration in Emergency Cardiovascular Care. Qual. Manag. Health Care 2017, 26, 1–6. [Google Scholar] [CrossRef]
- Boterman, W.R. Urban-Rural Polarisation in Times of the Corona Outbreak? The Early Demographic and Geographic Patterns of the SARS-CoV-2 Epidemic in the Netherlands. Tijdschr. Econ. Soc. Geogr. 2020, 111, 513–529. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, R.A.; Kane, A.D.; Cook, T.M. Outcomes from intensive care in patients with COVID-19: A systematic review and meta-analysis of observational studies. Anaesthesia 2020, 75, 1340–1349. [Google Scholar] [CrossRef]
- Castillo, R.C.; Staguhn, E.D.; Weston-Farber, E. The effect of state-level stay-at-home orders on COVID-19 infection rates. Am. J. Infect. Control 2020, 48, 958–960. [Google Scholar] [CrossRef]

| Variables | Measurements | Sources |
|---|---|---|
| Confirmed COVID-19 cases | Cumulative number of confirmed COVID-19 cases per 100,000 people in a city from January 2020 to April 2021 | KDCA [12] |
| Hospitals | Number of hospitals in a city per 1000 people | KOSIS [13] |
| CHCs | Number of community health centers in a city per 1000 people | KOSIS [13] |
| Health budget | Budget amount (converted to millions of USD) allocated to the health sector by a city government † | KOSIS [13] |
| HCPs | Number of medical doctors and nurses in a city per 1000 people | KOSIS [13] |
| ER beds | Number of emergency room beds in a city per 1000 people | KOSIS [13] |
| Sex | Male population divided by the female population, multiplied by 100, in a city | KOSIS [13] |
| Age | Median age of city residents | KOSIS [13] |
| Educational level | Percentage of city residents with a bachelor’s degree or higher | KOSIS [13] |
| Single-person households | Percentage of single-person households in a city | KOSIS [13] |
| Personal annual income | Income per worker reported (converted to thousands of USD) during the year-end tax filing for earned income in a city † | KOSIS [13] |
| Foreigner population | Percentage of foreigners living in a city at the time of survey who have lived in Korea for more than 3 months, relative to the total city population | KOSIS [13] |
| Traffic volume | Estimated number of vehicles (cars, buses and trucks) travelling along roads within a city per day | KTDB [14] |
| Population density | Persons living in a city per km2 | KOSIS [13] |
| Social distancing | Percentage of city residents who practiced social distancing in the past week at the time of survey | KOSIS [13] |
| CHC utilization | Percentage of city residents who used community health centers in the past year at the time of survey | KOSIS [13] |
| Variable | Count | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Confirmed COVID-19 cases (per 100,000 people) | 225 | 199.66 | 159.19 | 9.58 | 1243.23 |
| Hospitals (per 1000 people) | 225 | 0.66 | 0.36 | 0.13 | 3.70 |
| CHCs (per 1000 people) | 225 | 0.23 | 0.29 | 0.00 | 1.23 |
| Health budget (Million USD) † | 225 | 14.97 | 10.38 | 3.89 | 105.12 |
| HCPs (per 1000 people) | 225 | 5.89 | 6.04 | 0.94 | 50.36 |
| ER beds (per 1000 people) | 225 | 0.21 | 0.16 | 0.00 | 1.11 |
| Sex | 225 | 100.92 | 6.28 | 88.00 | 124.80 |
| Age (years) | 225 | 46.09 | 4.83 | 36.90 | 57.40 |
| Educational level (%) | 225 | 26.24 | 10.09 | 11.50 | 62.75 |
| Single-person households (%) | 225 | 33.48 | 5.06 | 18.26 | 51.91 |
| Personal annual income (Thousand USD) † | 225 | 29.70 | 5.50 | 21.15 | 62.09 |
| Foreigner population (%) | 225 | 3.09 | 2.29 | 0.51 | 12.94 |
| Traffic volume (vehicles/day) | 225 | 6272.99 | 4980.03 | 788.00 | 22,335.00 |
| Population density (persons/km2) | 225 | 3856.49 | 6006.79 | 18.31 | 25,225.51 |
| Social distancing (%) | 225 | 95.35 | 4.61 | 67.20 | 99.90 |
| CHC utilization (%) | 225 | 31.10 | 12.46 | 13.10 | 67.80 |
| Model 1 (OLS) | Model 2 (SLM) | |||||
|---|---|---|---|---|---|---|
| Variable | Coefficient | SE | p | Coefficient | SE | p |
| Spatial Autocorrelation Coefficient for COVID-19 Cases (ρ) | 0.293 | 0.079 | 0.000 ** | |||
| Hospitals | 6.521 | 30.319 | 0.830 | 10.024 | 28.159 | 0.722 |
| CHCs | −177.399 | 73.340 | 0.016 * | −140.806 | 68.334 | 0.039 * |
| Health budget | −44.517 | 18.568 | 0.017 * | −36.967 | 17.333 | 0.033 * |
| HCPs | 4.324 | 2.356 | 0.068 | 3.765 | 2.190 | 0.086 |
| ER beds | 54.143 | 79.222 | 0.495 | 73.261 | 73.603 | 0.320 |
| Sex | 1.653 | 2.127 | 0.438 | 1.191 | 1.978 | 0.547 |
| Age | 4.453 | 3.468 | 0.201 | 2.853 | 3.246 | 0.379 |
| Educational level | 0.788 | 2.209 | 0.722 | 0.188 | 2.058 | 0.927 |
| Single-person households | 4.177 | 2.094 | 0.047 * | 3.106 | 1.952 | 0.112 |
| Personal annual income | 46.619 | 95.008 | 0.624 | 35.393 | 88.239 | 0.688 |
| Foreigner population | 3.361 | 4.564 | 0.462 | 3.051 | 4.243 | 0.472 |
| Traffic volume | 25.873 | 30.270 | 0.394 | 19.207 | 28.119 | 0.495 |
| Population density | 5.327 | 10.713 | 0.620 | 4.311 | 10.089 | 0.669 |
| Social distancing | −1.677 | 1.651 | 0.311 | −2.302 | 1.534 | 0.133 |
| CHC utilization | 2.179 | 1.361 | 0.111 | 1.965 | 1.266 | 0.121 |
| Seoul Capital Area | 180.980 | 25.005 | 0.000 ** | 137.451 | 25.604 | 0.000 ** |
| Daegu Metropolitan City | 300.299 | 43.431 | 0.000 ** | 226.423 | 44.492 | 0.000 ** |
| Constant | −612.624 | 544.290 | 0.262 | −345.673 | 506.731 | 0.495 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, J.; Lee, S. Spatial Analysis of Health System Factors in Infectious Disease Management: Lessons Learned from the COVID-19 Pandemic in Korea. Healthcare 2024, 12, 1484. https://doi.org/10.3390/healthcare12151484
Lee J, Lee S. Spatial Analysis of Health System Factors in Infectious Disease Management: Lessons Learned from the COVID-19 Pandemic in Korea. Healthcare. 2024; 12(15):1484. https://doi.org/10.3390/healthcare12151484
Chicago/Turabian StyleLee, Jeongwook, and SangA Lee. 2024. "Spatial Analysis of Health System Factors in Infectious Disease Management: Lessons Learned from the COVID-19 Pandemic in Korea" Healthcare 12, no. 15: 1484. https://doi.org/10.3390/healthcare12151484
APA StyleLee, J., & Lee, S. (2024). Spatial Analysis of Health System Factors in Infectious Disease Management: Lessons Learned from the COVID-19 Pandemic in Korea. Healthcare, 12(15), 1484. https://doi.org/10.3390/healthcare12151484





