Gender-Based Socio-Economic Inequalities in the Pre-Vaccination Era of the COVID-19 Pandemic in Istanbul: A Neighborhood-Level Analysis of Excess Mortality
Abstract
1. Introduction
- Older age groups and males are at higher risk of mortality during the pre-vaccination era of the pandemic.
- Neighborhood socio-economic vulnerability is associated with increased excess mortality rates during the pre-vaccination era of the COVID-19 pandemic.
- Neighborhood socio-economic vulnerability influences excess mortality rates differently according to gender during the pre-vaccination era of the COVID-19 pandemic.
2. Materials and Methods
2.1. Data Source
2.2. Preparation of the Dataset for Analysis
2.3. Variable Definition
- Gender data was obtained from the IMM Statistical Office in the initial dataset, which reported it as binary variable (male and female).
- Time of death was reported by the IMM as the day, month and year of death for the years from 2018 to 2020.
- Neighborhoods of deceased people were obtained from the IMM for each individual.
- Population density has been calculated for each neighborhood as number of people per kilometer square. The population census of 2020 and land sizes are obtained from the digital map that contained the Turkish Statistical Institute’s latest data, as mentioned above.
- Share of 50+ year old residents indicated the percentage of people living in each neighborhood who were above 50 years old. Age distribution of each neighborhood was included in the digital map used in the study.
- Educational attainment was categorized as percentages of people in each neighborhood with less than a high school degree, high school degree and college or university degree (undergraduate or graduate degrees were combined). Categories of educational degrees (elementary, secondary, high school, college and university) in percentages for each neighborhood were included in the digital map used in the study.
- The Socio-Economic Vulnerability Index (SEVI) is a composite scale developed by IMM to measure neighborhood-level socio-economic disadvantage. The IMM Statistical Office used age dependency ratio, ratio of working population to dependent population, ratio of university graduates, household size, number of households applied to social support services, number of banks, rental prices for housing and income levels at each neighborhood to formulate the index.
- The Transportation Vulnerability Index (TVI) is a composite scale developed by IMM to measure the neighborhood-level disadvantage in regard to the transportation services available. The TVI includes number of travels, share of public transportation in vehicle transportation, passenger density per station, number of passengers with disabilities, and the number of passengers over 65 years of age at the neighborhood level.
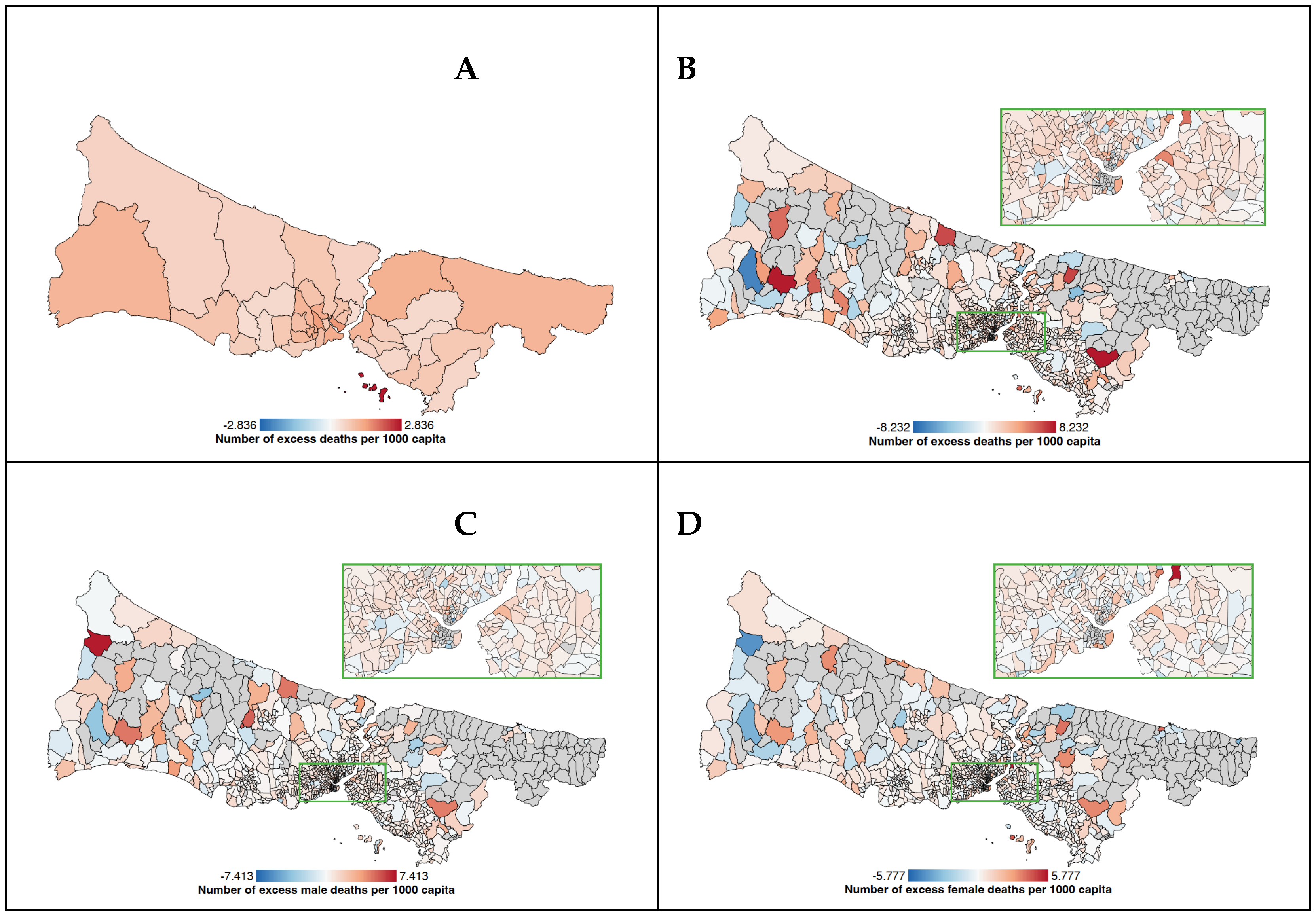
- EMRs at the neighborhood level constitute the dependent variable of the study. The mortality data included death records from 2018, 2019 and 2020. The number of excess deaths has been calculated for the year 2020 by extracting the number of deaths in a neighborhood in 2020 from the expected number of deaths calculated as the mean deaths of 2018 and 2019 (#deaths in 2018 + #deaths in 2019 divided by 2) of the same neighborhoods. The EMR was calculated by dividing the number of excess deaths in each neighborhood by the total neighborhood population in 2020 (per 1000). This procedure was repeated for male and female deaths with a denominator of male or female population in each neighborhood. Positive results indicated that there was an increase in the death rate in 2020 compared to 2018 and 2019, while negative results indicated a decrease in mortality.
2.4. Mapping EMRs of Istanbul Neighborhoods
2.5. Statistical Analysis
3. Results
4. Discussion
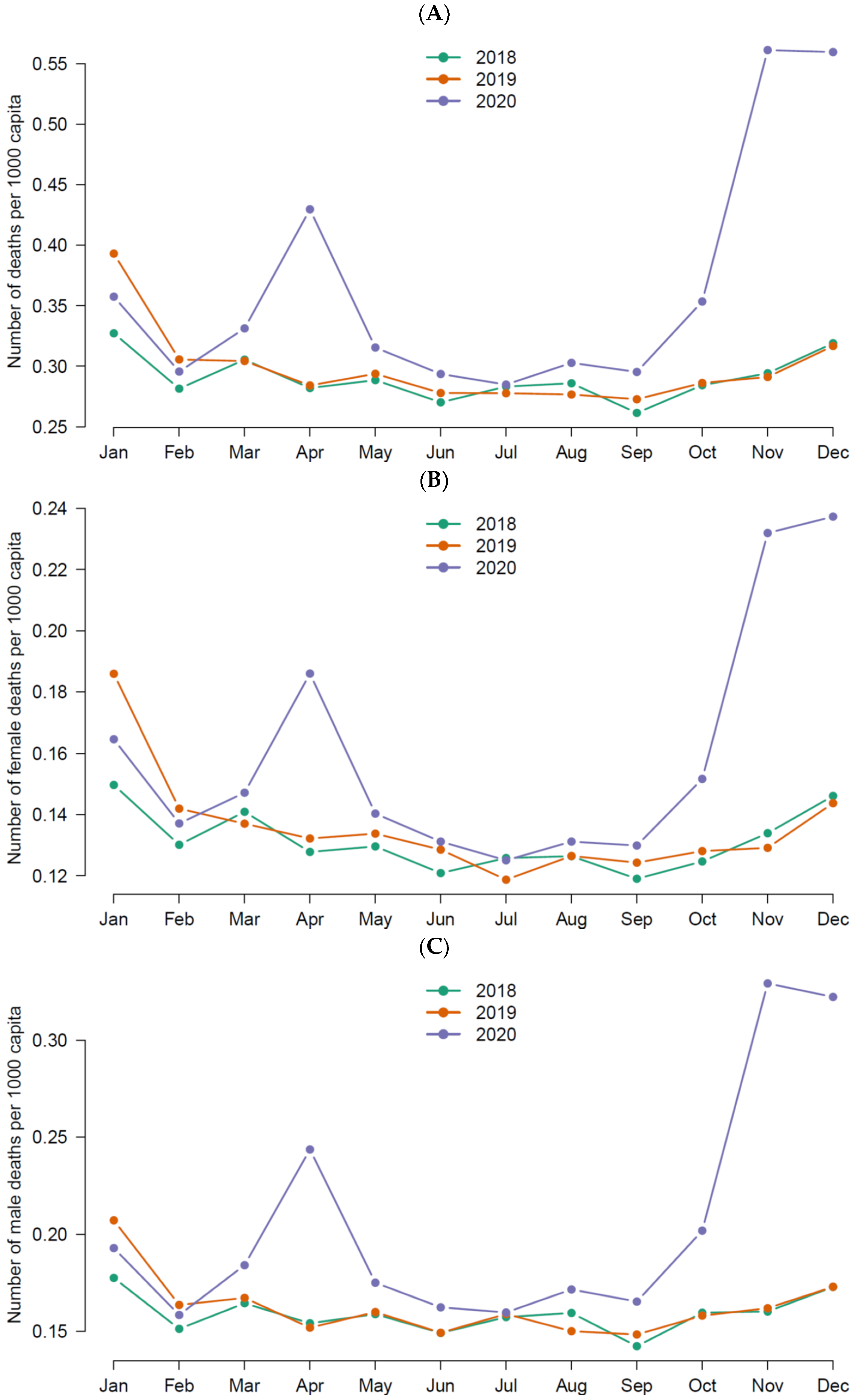
- The temporal distribution of total EMRs in Istanbul mirrored two peaks throughout the pre-vaccination era observed in April and November.
- Male EMRs were higher compared to females in Istanbul during the pre-vaccination era of the pandemic, with notable increases seen in both peaks of the EMR surges.
- Age significantly influenced EMRs during the pandemic, with higher mortality seen in neighborhoods with a higher share of 50+ year old age groups.
- The distribution of EM during the pandemic was uneven across neighborhoods, with higher neighborhood socio-economic vulnerability associated with increased total EMRs.
- Neighborhood socio-economic vulnerability was significantly associated with EMRs in males but not in females, indicating a gender-specific impact of neighborhood socio-economic vulnerability on mortality rates.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard; WHO: Geneva, Switzerland, 2021. [Google Scholar]
- Ioannidis, J.P.A. Over- and under-estimation of COVID-19 deaths. Eur. J. Epidemiol. 2021, 36, 581–588. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Paulson, K.R.; Pease, S.A.; Watson, S.; Comfort, H.; Zheng, P.; Aravkin, A.Y.; Bisignano, C.; Barber, R.M.; Alam, T.; et al. Estimating excess mortality due to the COVID-19 pandemic: A systematic analysis of COVID-19-related mortality, 2020–2021. Lancet 2022, 399, 1513–1536. [Google Scholar] [CrossRef] [PubMed]
- Dahal, S.; Luo, R.; Swahn, M.H.; Chowell, G. Geospatial Variability in Excess Death Rates during the COVID-19 Pandemic in Mexico: Examining Socio Demographic, Climate and Population Health Characteristics. Int. J. Infect. Dis. 2021, 113, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Vestergaard, L.S.; Nielsen, J.; Richter, L.; Schmid, D.; Bustos, N.; Braeye, T.; Mølbak, K. Excess all-cause mortality during the COVID-19 pandemic in Europe-preliminary pooled estimates from the EuroMOMO network, March to April 2020. Eurosurveillance 2020, 25, 2001214. [Google Scholar] [CrossRef] [PubMed]
- Turkish Statistical Institute. Population Censuses; Turkish Statistical Institute: Ankara, Turkey, 2022.
- Ucar, A.; Arslan, S. Estimation of Excess Deaths Associated with the COVID-19 Pandemic in Istanbul, Turkey. Front. Public Health 2022, 10, 888123. [Google Scholar] [CrossRef] [PubMed]
- Aykac, N.; Etiler, N. COVID-19 mortality in Istanbul in association with air pollution and socioeconomic status: An ecological study. Environ. Sci. Pollut. Res. Int. 2022, 29, 13700–13708. [Google Scholar] [CrossRef] [PubMed]
- Martins-Filho, P.R.; Tavares, C.S.S.; Santos, V.S. Factors associated with mortality in patients with COVID-19. A quantitative evidence synthesis of clinical and laboratory data. Eur. J. Intern. Med. 2020, 76, 97–99. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Hu, X.; Xie, J. Spatial inequalities of COVID-19 mortality rate in relation to socioeconomic and environmental factors across England. Sci. Total Environ. 2021, 758, 143595. [Google Scholar] [CrossRef]
- World Health Organization. COVID-19 and the Social Determinants of Health and Health Equity: Evidence Brief; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Clouston, S.A.P.; Natale, G.; Link, B.G. Socioeconomic inequalities in the spread of coronavirus-19 in the United States: A examination of the emergence of social inequalities. Soc. Sci. Med. 2021, 268, 113554. [Google Scholar] [CrossRef]
- Stokes, A.C.; Lundberg, D.J.; Elo, I.T.; Hempstead, K.; Bor, J.; Preston, S.H. COVID-19 and excess mortality in the United States: A county-level analysis. PLoS Med. 2021, 18, e1003571. [Google Scholar] [CrossRef]
- Cifuentes, M.P.; Rodriguez-Villamizar, L.A.; Rojas-Botero, M.L.; Alvarez-Moreno, C.A.; Fernandez-Nino, J.A. Socioeconomic inequalities associated with mortality for COVID-19 in Colombia: A cohort nationwide study. J. Epidemiol. Community Health 2021, 75, 610–615. [Google Scholar] [CrossRef] [PubMed]
- Rizzi, S.; Strozza, C.; Zarulli, V. Sex-differences in excess death risk during the COVID-19 pandemic: An analysis of the first wave across Italian regions. What have we learned? Genus 2022, 78, 24. [Google Scholar] [CrossRef]
- Pothisiri, W.; Prasitsiriphon, O.; Apakupakul, J.; Ploddi, K. Gender differences in estimated excess mortality during the COVID-19 pandemic in Thailand. BMC Public Health 2023, 23, 1900. [Google Scholar] [CrossRef] [PubMed]
- Kartoglu, U.; Pala, K. Evaluation of COVID-19 pandemic management in Turkiye. Front. Public Health 2023, 11, 1142471. [Google Scholar] [CrossRef]
- Bayram, H.; Köktürk, N.; Elbek, O.; Kılınç, O.; Sayıner, A.; Dağlı, E. Interference in scientific research on COVID-19 in Turkey. Lancet 2020, 396, 463–464. [Google Scholar] [CrossRef] [PubMed]
- Yardim, M.; Eser, S. COVID-19 Pandemic and Excess Mortality: The Case of Istanbul. Türkiye Halk Sağlığı Dergisi. 2020, 18, 14–24. [Google Scholar] [CrossRef]
- BIMTAS. Project Report on Istanbul Vulnerability Map during the Fight against COVID-19 Pandemic; Ozturk, N.K., Ed.; Istanbul Metropolitan Municipality: Istanbul, Turkey, 2020. [Google Scholar]
- Khader, Y.; Al Nsour, M. Excess Mortality during the COVID-19 Pandemic in Jordan: Secondary Data Analysis. JMIR Public Health Surveill. 2021, 7, e32559. [Google Scholar] [CrossRef] [PubMed]
- Todd, M.; Pharis, M.; Gulino, S.P.; Robbins, J.M.; Bettigole, C. Excess Mortality during the COVID-19 Pandemic in Philadelphia. Am. J. Public Health 2021, 111, 1352–1357. [Google Scholar] [CrossRef] [PubMed]
- Joy, M.; Hobbs, F.R.; Bernal, J.L.; Sherlock, J.; Amirthalingam, G.; McGagh, D.; Akinyemi, O.; Byford, R.; Dabrera, G.; Dorward, J.; et al. Excess mortality in the first COVID pandemic peak: Cross-sectional analyses of the impact of age, sex, ethnicity, household size, and long-term conditions in people of known SARS-CoV-2 status in England. Br. J. Gen. Pract. 2020, 70, e890–e898. [Google Scholar] [CrossRef]
- Islam, N.; Jdanov, D.A.; Shkolnikov, V.M.; Khunti, K.; Kawachi, I.; White, M.; Lewington, S.; Lacey, B. Effects of covid-19 pandemic on life expectancy and premature mortality in 2020, time series analysis in 37 countries. BMJ 2021, 375, e066768. [Google Scholar] [CrossRef]
- Santesmasses, D.; Castro, J.P.; Zenin, A.A.; Shindyapina, A.V.; Gerashchenko, M.V.; Zhang, B.; Kerepesi, C.; Yim, S.H.; Fedichev, P.O.; Gladyshev, V.N. COVID-19 is an emergent disease of aging. Aging Cell 2020, 19, e13230. [Google Scholar] [CrossRef]
- Mauvais-Jarvis, F.; Bairey Merz, N.; Barnes, P.J.; Brinton, R.D.; Carrero, J.J.; DeMeo, D.L.; De Vries, G.J.; Epperson, C.N.; Govindan, R.; Klein, S.L.; et al. Sex and gender: Modifiers of health, disease, and medicine. Lancet 2020, 396, 565–582. [Google Scholar] [CrossRef] [PubMed]
- Modig, K.; Ahlbom, A.; Ebeling, M. Excess mortality from COVID-19, weekly excess death rates by age and sex for Sweden and its most affected region. Eur. J. Public Health 2021, 31, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Kontopantelis, E.; Mamas, M.A.; Deanfield, J.; Asaria, M.; Doran, T. Excess mortality in England and Wales during the first wave of the COVID-19 pandemic. J. Epidemiol. Community Health 2021, 75, 213–223. [Google Scholar] [CrossRef]
- Demetriou, C.A.; Achilleos, S.; Quattrocchi, A.; Gabel, J.; Critselis, E.; Constantinou, C.; Nicolaou, N.; Ambrosio, G.; Bennett, C.M.; Le Meur, N.; et al. Impact of the COVID-19 pandemic on total, sex- and age-specific all-cause mortality in 20 countries worldwide during 2020, results from the C-MOR project. Int. J. Epidemiol. 2022, 52, 664–676. [Google Scholar] [CrossRef]
- Ministry of Health of Turkey. Türkiye Bulaşici Olmayan Hastaliklar ve Risk Faktörleri Kohort Çalişmasi; Ünal, B.E.G., Ed.; Ministry of Health Turkey: Ankara, Turkey, 2021.
- Shah, S.; Rajiv, R.M.; Lokre, A. Moving Toward Gender-Equitable Transportation in Post-COVID-19 Urban South Asia. Transp. Res. Rec. 2023, 2677, 865–879. [Google Scholar] [CrossRef] [PubMed]
- Murat, Y.S.C.; Cakici, Z. Analysis of the COVID-19 pandemic on preferences of transport modes. In Proceedings of the Institution of Civil Engineers-Transport; Emerald Publishing Limited.: Bingley, UK, 2023; pp. 1–31. [Google Scholar]
- Mena, G.E.; Martinez, P.P.; Mahmud, A.S.; Marquet, P.A.; Buckee, C.O.; Santillana, M. Socioeconomic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science 2021, 372, 934. [Google Scholar] [CrossRef]
- Calderon-Larranaga, A.; Vetrano, D.L.; Rizzuto, D.; Bellander, T.; Fratiglioni, L.; Dekhtyar, S. High excess mortality in areas with young and socially vulnerable populations during the COVID-19 outbreak in Stockholm Region, Sweden. BMJ Glob. Health 2020, 5, e003595. [Google Scholar] [CrossRef] [PubMed]
- Khanijahani, A.; Tomassoni, L. Socioeconomic and Racial Segregation and COVID-19, Concentrated Disadvantage and Black Concentration in Association with COVID-19 Deaths in the USA. J. Racial Ethn. Health Disparities 2022, 9, 367–375. [Google Scholar] [CrossRef]
- Drefahl, S.; Wallace, M.; Mussino, E.; Aradhya, S.; Kolk, M.; Branden, M.; Andersson, G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020, 11, 5097. [Google Scholar] [CrossRef]
- Figueiredo, A.M.; Figueiredo, D.; Gomes, L.B.; Massuda, A.; Gil-Garcia, E.; Vianna, R.P.T.; Daponte, A. Social determinants of health and COVID-19 infection in Brazil: An analysis of the pandemic. Rev. Bras. Enferm. 2020, 73, e20200673. [Google Scholar] [CrossRef] [PubMed]
- Flores, G.; Abbasi, A.; Korachais, C.; Lavado, R. Unaffordability of COVID-19 tests: Assessing age-related inequalities in 83 countries. Int. J. Equity Health 2022, 21, 177. [Google Scholar] [CrossRef] [PubMed]
- Kirkby, K.; Bergen, N.; Vidal Fuertes, C.; Schlotheuber, A.; Hosseinpoor, A.R. Education-related inequalities in beliefs and behaviors pertaining to COVID-19 non-pharmaceutical interventions. Int. J. Equity Health 2022, 21, 158. [Google Scholar] [CrossRef] [PubMed]
- Gaitens, J.; Condon, M.; Fernandes, E.; McDiarmid, M. COVID-19 and Essential Workers: A Narrative Review of Health Outcomes and Moral Injury. Int. J. Environ. Res. Public Health 2021, 18, 1446. [Google Scholar] [CrossRef]
- Carranza, A.; Goic, M.; Lara, E.; Olivares, M.; Weintraub, G.Y.; Covarrubia, J.; Basso, L.J. The Social Divide of Social Distancing: Shelter-in-Place Behavior in Santiago during the COVID-19 Pandemic. Manag. Sci. 2020, 68, 3691373. [Google Scholar] [CrossRef]
- Peksan, S.A.C.; Altinay Cingoz, A.R.A. İstanbul’da Kentsel Yoksulluk ve Kırılganlık: COVID-19 Salgininin dar Gelirli Haneler Üzerindeki Etkileri; Istanbul Metropolitan Municipality: Istanbukl, Turkey, 2021. [Google Scholar]
- Turkish Statistical Institute. Workforce Statistics 2021; Turkish Statistical Institute: Ankara, Turkey, 2022.
- Doerre, A.; Doblhammer, G. The influence of gender on COVID-19 infections and mortality in Germany: Insights from age- and gender-specific modeling of contact rates, infections, and deaths in the early phase of the pandemic. PLoS ONE 2022, 17, e0268119. [Google Scholar] [CrossRef]
- Pilkington, H.; Feuillet, T.; Rican, S.; de Bouille, J.G.; Bouchaud, O.; Cailhol, J.; Bihan, H.; Lombrail, P.; Julia, C. Spatial determinants of excess all-cause mortality during the first wave of the COVID-19 epidemic in France. BMC Public Health 2021, 21, 2157. [Google Scholar] [CrossRef]
| Variable | Min. | 1st Quartile | Median | Mean | 3rd Quartile | Max. |
|---|---|---|---|---|---|---|
| Population density (per km2) | 6.85 | 4689.59 | 15,838.07 | 21,240.07 | 31,947.52 | 95,270.13 |
| Share of 50+ year old residents (%) | 2.81 | 16.67 | 21.97 | 23.09 | 28.09 | 52.11 |
| Share of residents with less than high school degree (%) | 7.84 | 48.07 | 61.03 | 58.40 | 70.11 | 88.53 |
| Share of residents with high school degree (%) | 8.49 | 18.74 | 22.00 | 22.01 | 24.73 | 81.84 |
| Share of residents with college or university degree (%) | 2.69 | 10.46 | 16.08 | 19.59 | 25.79 | 60.51 |
| SEVI score (0–100) | 22.22 | 51.92 | 60.07 | 57.92 | 65.99 | 83.78 |
| TVI score (0–100) | <0.001 | 17.17 | 19.71 | 20.49 | 22.78 | 79.15 |
| Total EMR (per 1000) | −6.84 | 0.38 | 0.88 | 0.95 | 1.42 | 8.23 |
| Female EMR (per 1000) | −4.34 | 0.02 | 0.33 | 0.37 | 0.64 | 5.78 |
| Male EMR (per 1000) | −4.92 | 0.16 | 0.55 | 0.59 | 0.95 | 7.41 |
| Total EMR (per 1000) in 10 neighborhoods with lowest SEVI scores | −0.79 | -0.48 | 0.55 | 0.83 | 1.69 | 3.77 |
| Total EMR (per 1000) in 10 neighborhoods with highest SEVI scores | −0.06 | 1.04 | 1.59 | 1.73 | 2.21 | 3.73 |
| Total | Female | Male | ||||
|---|---|---|---|---|---|---|
| Neighborhood Variables | Standardized Coefficient | p-Value | Standardized Coefficient | p-Value | Standardized Coefficient | p-Value |
| Population density | 0.604 | 0.546 | −0.383 | 0.701 | 1.169 | 0.243 |
| Share of 50+ year old residents (%) | 3.073 | 0.002 | 2.004 | 0.045 | 2.472 | 0.014 |
| Share of residents with less than high school degree (%) | 2.636 | 0.009 | 0.620 | 0.535 | 3.096 | 0.002 |
| Share of residents with high school degree (%) | −1.654 | 0.099 | −0.016 | 0.988 | −2.272 | 0.023 |
| Share of residents with college or university degree (%) | −2.589 | 0.010 | −0.794 | 0.428 | −2.877 | 0.004 |
| SEVI Score | 2.475 | 0.014 | 0.692 | 0.489 | 2.810 | 0.005 |
| TVI Score | −2.725 | 0.007 | −1.635 | 0.102 | −2.321 | 0.021 |
| Total | Female | Male | ||||
|---|---|---|---|---|---|---|
| Neighborhood Variables | Standardized Coefficient | p-Value | Standardized Coefficient | p-Value | Standardized Coefficient | p-Value |
| Population density | 1.816 | 0.070 | 0.317 | 0.751 | 2.220 | 0.027 |
| Share of 50+ year old residents (%) | 4.865 | <0.001 | 2.427 | 0.015 | 4.544 | <0.001 |
| SEVI Score | 4.064 | <0.001 | 1.527 | 0.127 | 4.241 | <0.001 |
| TVI Score | −1.329 | 0.184 | 0.944 | 0.345 | −0.992 | 0.321 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kayı, İ.; Gönen, M.; Sakarya, S.; Eryiğit, Ö.Y.; Ergönül, Ö. Gender-Based Socio-Economic Inequalities in the Pre-Vaccination Era of the COVID-19 Pandemic in Istanbul: A Neighborhood-Level Analysis of Excess Mortality. Healthcare 2024, 12, 1406. https://doi.org/10.3390/healthcare12141406
Kayı İ, Gönen M, Sakarya S, Eryiğit ÖY, Ergönül Ö. Gender-Based Socio-Economic Inequalities in the Pre-Vaccination Era of the COVID-19 Pandemic in Istanbul: A Neighborhood-Level Analysis of Excess Mortality. Healthcare. 2024; 12(14):1406. https://doi.org/10.3390/healthcare12141406
Chicago/Turabian StyleKayı, İlker, Mehmet Gönen, Sibel Sakarya, Önder Yüksel Eryiğit, and Önder Ergönül. 2024. "Gender-Based Socio-Economic Inequalities in the Pre-Vaccination Era of the COVID-19 Pandemic in Istanbul: A Neighborhood-Level Analysis of Excess Mortality" Healthcare 12, no. 14: 1406. https://doi.org/10.3390/healthcare12141406
APA StyleKayı, İ., Gönen, M., Sakarya, S., Eryiğit, Ö. Y., & Ergönül, Ö. (2024). Gender-Based Socio-Economic Inequalities in the Pre-Vaccination Era of the COVID-19 Pandemic in Istanbul: A Neighborhood-Level Analysis of Excess Mortality. Healthcare, 12(14), 1406. https://doi.org/10.3390/healthcare12141406







