The Future of Total Elbow Arthroplasty: A Statistical Forecast Model for Germany
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jacob, L.; Breuer, J.; Kostev, K. Prevalence of chronic diseases among older patients in German general practices. GMS Ger. Med. Sci. 2016, 14, Doc03. [Google Scholar]
- Nowossadeck, E. Population aging and hospitalization for chronic disease in Germany. Dtsch. Ärzteblatt Int. 2012, 109, 151–157. [Google Scholar] [CrossRef]
- Pilz, V.; Hanstein, T.; Skripitz, R. Projections of primary hip arthroplasty in Germany until 2040. Acta Orthop. 2018, 89, 308–313. [Google Scholar] [CrossRef]
- Inacio, M.C.S.; Graves, S.E.; Pratt, N.L.; Roughead, E.E.; Nemes, S. Increase in Total Joint Arthroplasty Projected from 2014 to 2046 in Australia: A Conservative Local Model With International Implications. Clin. Orthop. Relat. Res. 2017, 475, 2130–2137. [Google Scholar] [CrossRef]
- Kurtz, S.; Ong, K.; Lau, E.; Mowat, F.; Halpern, M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J. Bone Jt. Surg. 2007, 89, 780–785. [Google Scholar] [CrossRef]
- Day, J.S.; Lau, E.; Ong, K.L.; Williams, G.R.; Ramsey, M.L.; Kurtz, S.M. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J. Shoulder Elb. Surg. 2010, 19, 1115–1120. [Google Scholar] [CrossRef]
- Rupp, M.; Lau, E.; Kurtz, S.M.; Alt, V. Projections of primary TKA and THA in Germany from 2016 through 2040. Clin. Orthop. Relat. Res. 2020, 478, 1622–1633. [Google Scholar] [CrossRef]
- Coleman, D.; Rowthorn, R. Who’s afraid of population decline? A critical examination of its consequences. Popul. Dev. Rev. 2011, 37, 217–248. [Google Scholar] [CrossRef]
- Weber, H. Could Immigration Prevent Population Decline? The Demographic Prospects of Germany Revisited. Comp. Popul. Stud. 2015, 40, 166–189. [Google Scholar] [CrossRef]
- Schollgen, I.; Huxhold, O.; Tesch-Romer, C. Socioeconomic status and health in the second half of life: Findings from the German Ageing Survey. Eur. J. Ageing 2010, 7, 17–28. [Google Scholar] [CrossRef]
- Gay, D.M.; Lyman, S.; Do, H.; Hotchkiss, R.N.; Marx, R.G.; Daluiski, A. Indications and reoperation rates for total elbow arthroplasty: An analysis of trends in New York State. J. Bone Jt. Surg. Am. 2012, 94, 110–117. [Google Scholar] [CrossRef]
- Burkhart, K.J.; Watts, A.C.; Athwal, G.S.; Hollinger, B.; Wegmann, K.; Müller, L.P. Complication Management in Distal Humerus Hemiarthroplasty. In Elbow Arthroplasty: Current Techniques and Complications; Springer: Berlin/Heidelberg, Germany, 2020; pp. 233–241. [Google Scholar]
- Kolusu, D.N.; Mekala, D.K.R. A study on clinical outcome of total elbow arthroplasty. Int. J. Orthop. Sci. 2018, 4, 522–526. [Google Scholar] [CrossRef]
- Craik, J.D.; Laffer, C.H.; Richards, S.W.; Walsh, S.P.; Evans, S.L. Distal humerus cortical strains following total elbow arthroplasty. Proc. Inst. Mech. Eng. H 2013, 227, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Rotini, R.; Ricciarelli, M.; Guerra, E.; Marinelli, A.; Celli, A. Elbow hemiarthroplasty in distal humeral fractures: Indication, surgical technique and results. Injury 2023, 54 (Suppl. S1), S36–S45. [Google Scholar] [CrossRef] [PubMed]
- Wagener, M.L.; De Vos, M.J.; Hendriks, J.C.; Eygendaal, D.; Verdonschot, N. Stability of the unlinked Latitude total elbow prosthesis: A biomechanical in vitro analysis. Clin. Biomech. 2013, 28, 502–508. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.P.; Hollinger, B.; Burkhart, K. Ellenbogen: Expertise Orthopädie und Unfallchirurgie; Georg Thieme Verlag: New York, NY, USA, 2016. [Google Scholar]
- Bachman, D.; Cil, A. Current concepts in elbow arthroplasty. EFORT Open Rev. 2017, 2, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Samdanis, V.; Manoharan, G.; Jordan, R.W.; Watts, A.C.; Jenkins, P.; Kulkarni, R.; Thomas, M.; Rangan, A.; Hay, S.M. Indications and outcome in total elbow arthroplasty: A systematic review. Shoulder Elb. 2020, 12, 353–361. [Google Scholar] [CrossRef]
- Petscavage, J.M.; Ha, A.S.; Chew, F.S. Radiologic review of total elbow, radial head, and capitellar resurfacing arthroplasty. Radiographics 2012, 32, 129–149. [Google Scholar] [CrossRef]
- Keely Boyle, K.; Rachala, S.; Nodzo, S.R. Centers for Disease Control and Prevention 2017 Guidelines for Prevention of Surgical Site Infections: Review and Relevant Recommendations. Curr. Rev. Musculoskelet. Med. 2018, 11, 357–369. [Google Scholar] [CrossRef]
- Nystad, T.W.; Fenstad, A.M.; Havelin, L.I.; Furnes, O.; Skredderstuen, A.K.; Fevang, B.T.S. SAT0061 Reduction in Joint Replacement Surgery in Patients with Reumatoid Arthritis. Ann. Rheum. Dis. 2014, 73, 611–612. [Google Scholar] [CrossRef]
- Klug, A.; Gramlich, Y.; Buckup, J.; Schweigkofler, U.; Hoffmann, R.; Schmidt-Horlohe, K. Trends in total elbow arthroplasty: A nationwide analysis in Germany from 2005 to 2014. Int. Orthop. 2018, 42, 883–889. [Google Scholar] [CrossRef] [PubMed]
- Klug, A.; Herrmann, E.; Fischer, S.; Hoffmann, R.; Gramlich, Y. Projections of Primary and Revision Shoulder Arthroplasty until 2040: Facing a Massive Rise in Fracture-Related Procedures. J. Clin. Med. 2021, 10, 5123. [Google Scholar] [CrossRef] [PubMed]
- Alabdulrazzaq, H.; Alenezi, M.N.; Rawajfih, Y.; Alghannam, B.A.; Al-Hassan, A.A.; Al-Anzi, F.S. On the accuracy of ARIMA based prediction of COVID-19 spread. Results Phys. 2021, 27, 104509. [Google Scholar] [CrossRef]
- Park, J.G.; Cho, N.S.; Song, J.H.; Lee, D.S.; Rhee, Y.G. Clinical outcomes of semiconstrained total elbow arthroplasty in patients who were forty years of age or younger. JBJS 2015, 97, 1781–1791. [Google Scholar] [CrossRef]
- Sjögren, K.; Stjernberg, L. A gender perspective on factors that influence outdoor recreational physical activity among the elderly. BMC Geriatr. 2010, 10, 34. [Google Scholar] [CrossRef]
- Melton, L.J., 3rd. The prevalence of osteoporosis: Gender and racial comparison. Calcif. Tissue Int. 2001, 69, 179–181. [Google Scholar] [CrossRef]
- Dorbritz, J. Germany: Family Diversity with Low Actual and Desired Fertility. Demogr. Res. 2008, 19, 557–598. [Google Scholar] [CrossRef]
- Kappenschneider, T.; Maderbacher, G.; Weber, M.; Greimel, F.; Holzapfel, D.; Parik, L.; Schwarz, T.; Leiss, F.; Knebl, M.; Reinhard, J.; et al. Special orthopaedic geriatrics (SOG)—A new multiprofessional care model for elderly patients in elective orthopaedic surgery: A study protocol for a prospective randomized controlled trial of a multimodal intervention in frail patients with hip and knee replacement. BMC Musculoskelet. Disord. 2022, 23, 1079. [Google Scholar] [CrossRef]
- Charissoux, J.L.; Vergnenegre, G.; Pelissier, M.; Fabre, T.; Mansat, P.; Sofcot. Epidemiology of distal humerus fractures in the elderly. Orthop. Traumatol. Surg. Res. 2013, 99, 765–769. [Google Scholar] [CrossRef]
- Macken, A.A.; Prkic, A.; Kodde, I.F.; Lans, J.; Chen, N.C.; Eygendaal, D. Global trends in indications for total elbow arthroplasty: A systematic review of national registries. EFORT Open Rev. 2020, 5, 215–220. [Google Scholar] [CrossRef]
- Stone, A.; Chan, G.; Sinclair, L.; Phadnis, J. Elbow arthroplasty in trauma-current concepts review. J. Orthop. 2023, 35, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Celli, A.; Paroni, C.; Bonucci, P.; Celli, L. Total elbow arthroplasty for acute distal humeral fractures with humeral condyle resection or retention: A long-term follow-up study. JSES Int. 2021, 5, 797–803. [Google Scholar] [CrossRef]
- Loisel, F.; Amar, Y.; Rochet, S.; Obert, L. Distal humerus fracture in older patients: ORIF vs. total elbow arthroplasty. Orthop. Traumatol. Surg. Res. 2024, 110, 103759. [Google Scholar] [CrossRef] [PubMed]
- Jin, Z.; Wang, D.; Zhang, H.; Liang, J.; Feng, X.; Zhao, J.; Sun, L. Incidence trend of five common musculoskeletal disorders from 1990 to 2017 at the global, regional and national level: Results from the global burden of disease study 2017. Ann. Rheum. Dis. 2020, 79, 1014–1022. [Google Scholar] [CrossRef] [PubMed]
- Sizova, L. Approaches to the treatment of early rheumatoid arthritis with disease-modifying antirheumatic drugs. Br. J. Clin. Pharmacol. 2008, 66, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Harb, M.A.; Solow, M.; Newman, J.M.; Sodhi, N.; Pivec, R.; George, J.; Sultan, A.A.; Khlopas, A.; Shah, N.V.; Roche, M.W. Have the annual trends of total knee arthroplasty in rheumatoid arthritis patients changed? J. Knee Surg. 2018, 31, 841–845. [Google Scholar] [CrossRef] [PubMed]
- Yasui, T.; Nishino, J.; Kadono, Y.; Matsui, T.; Nakamura, K.; Tanaka, S.; Tohma, S. Impact of biologics on the prevalence of orthopedic surgery in the National Database of Rheumatic Diseases in Japan. Mod. Rheumatol. 2010, 20, 233–237. [Google Scholar] [CrossRef]
- Singh, J.A.; Yu, S.; Chen, L.; Cleveland, J.D. Rates of Total Joint Replacement in the United States: Future Projections to 2020-2040 Using the National Inpatient Sample. J. Rheumatol. 2019, 46, 1134–1140. [Google Scholar] [CrossRef]
- Dissanayake, K.; Jayasinghe, C.; Wanigasekara, P.; Sominanda, A. Potential applicability of cytokines as biomarkers of disease activity in rheumatoid arthritis: Enzyme-linked immunosorbent spot assay-based evaluation of TNF-α, IL-1β, IL-10 and IL-17A. PLoS ONE 2021, 16, e0246111. [Google Scholar] [CrossRef]
- Kiradzhiyska, D.D.; Mantcheva, R.D. Overview of biocompatible materials and their use in medicine. Folia Medica 2019, 61, 34–40. [Google Scholar] [CrossRef]
- Song, J.; Winkeljann, B.; Lieleg, O. Biopolymer-based coatings: Promising strategies to improve the biocompatibility and functionality of materials used in biomedical engineering. Adv. Mater. Interfaces 2020, 7, 2000850. [Google Scholar] [CrossRef]
- Kermavnar, T.; Shannon, A.; O’Sullivan, K.J.; McCarthy, C.; Dunne, C.P.; O’Sullivan, L.W. Three-Dimensional Printing of Medical Devices Used Directly to Treat Patients: A Systematic Review. 3d Print. Addit. Manuf. 2021, 8, 366–408. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.M.Y.; Wong, P.Y.; Liu, C.; Chung, Y.L.; Wong, K.C.; Tso, C.Y.; Chow, S.K.-H.; Cheung, W.-H.; Yung, P.S.-H.; Chui, C.S. 3D printing in orthopaedic surgery: A scoping review of randomized controlled trials. Bone Jt. Res. 2021, 10, 807–819. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Li, S. Computational Radiology for Orthopaedic Interventions; Springer: Berlin/Heidelberg, Germany, 2016. [Google Scholar]
- Tanji, A.; Nagura, T.; Iwamoto, T.; Matsumura, N.; Nakamura, M.; Matsumoto, M.; Sato, K. Total elbow arthroplasty using an augmented reality–assisted surgical technique. J. Shoulder Elb. Surg. 2022, 31, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Hemmann, P.; Ziegler, P.; Konrads, C.; Ellmerer, A.; Klopfer, T.; Schreiner, A.J.; Bahrs, C. Trends in fracture development of the upper extremity in Germany-a population-based description of the past 15 years. J. Orthop. Surg. Res. 2020, 15, 65. [Google Scholar] [CrossRef] [PubMed]
- Europe, A. Looking at the Lives of Older People in the EU; Publications Office of the European Union: Luxbembourg, 2020. [Google Scholar]
- Viveen, J.; Prkic, A.; Koenraadt, K.L.; Kodde, I.F.; The, B.; Eygendaal, D. Clinical and radiographic outcome of revision surgery of total elbow prosthesis: Midterm results in 19 cases. J. Shoulder Elb. Surg. 2017, 26, 716–722. [Google Scholar] [CrossRef] [PubMed]
- Davey, M.S.; Hurley, E.T.; Gaafar, M.; Molony, D.; Mullett, H.; Pauzenberger, L. Long-term outcomes of total elbow arthroplasty: A systematic review of studies at 10-year follow-up. J. Shoulder Elb. Surg. 2021, 30, 1423–1430. [Google Scholar] [CrossRef] [PubMed]
- Maman, D.; Weishahe, N.; Norman, D.; Keren, Y.; Yelton, M.; Trior, Y.; Apt, E.A.; Peskin, B.; Ghrayeb, N.; Shapira, J. Outcomes of Total Elbow Arthroplasty in Trauma Patients Compared with Patients Following Fixation of Distal Humerus Fractures. Preprints 2022. [Google Scholar] [CrossRef]
- Siala, M.; Laumonerie, P.; Hedjoudje, A.; Delclaux, S.; Bonnevialle, N.; Mansat, P. Outcomes of semiconstrained total elbow arthroplasty performed for arthritis in patients under 55 years old. J. Shoulder Elbow Surg. 2020, 29, 859–866. [Google Scholar] [CrossRef]
| Model | MAPE | RMSE | MAE |
|---|---|---|---|
| ARIMA | 7.30% | 47.9 | 39.3 |
| ETS | 5.80% | 37.4 | 31.6 |
| Poisson | 8.20% | 58.8 | 51.4 |
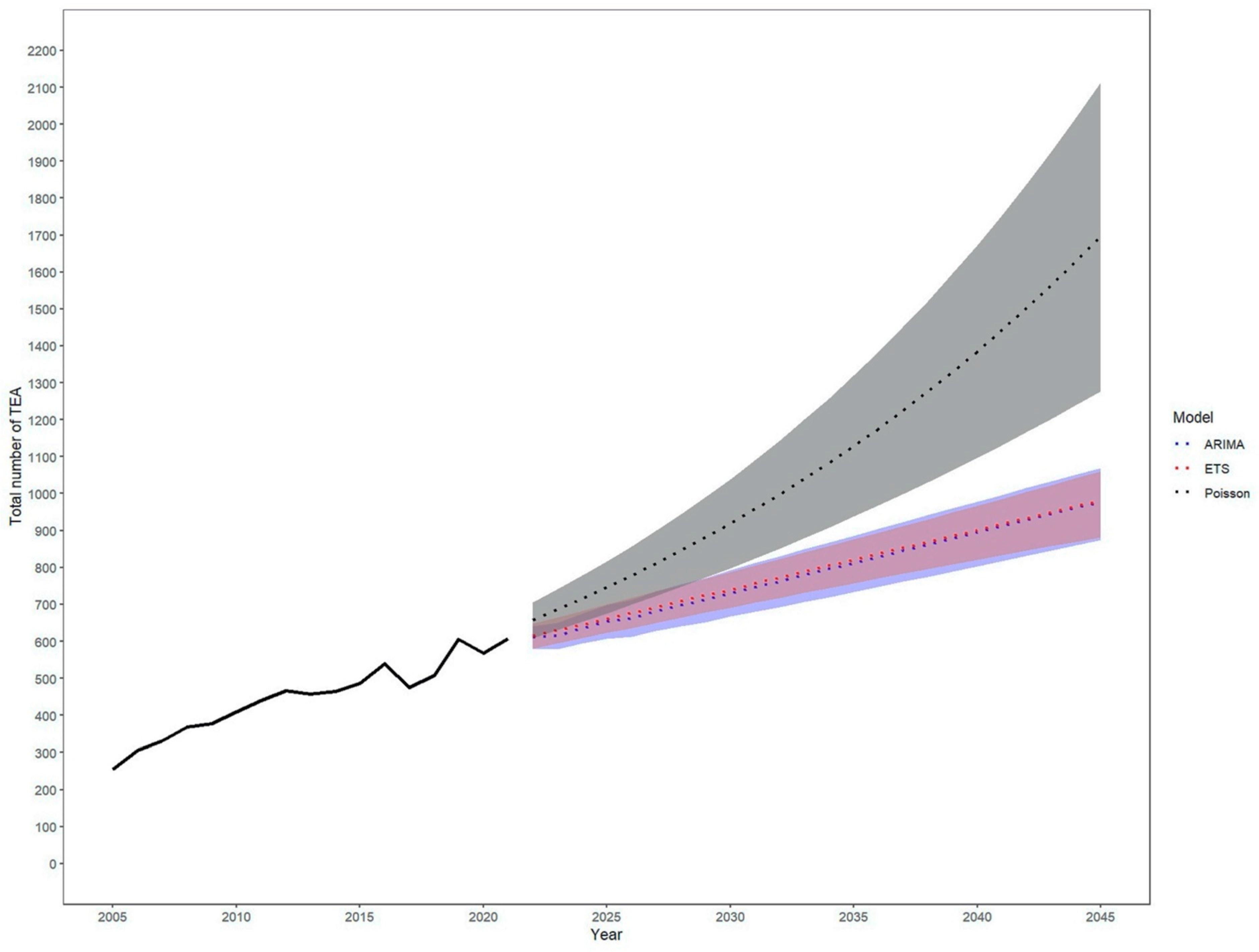
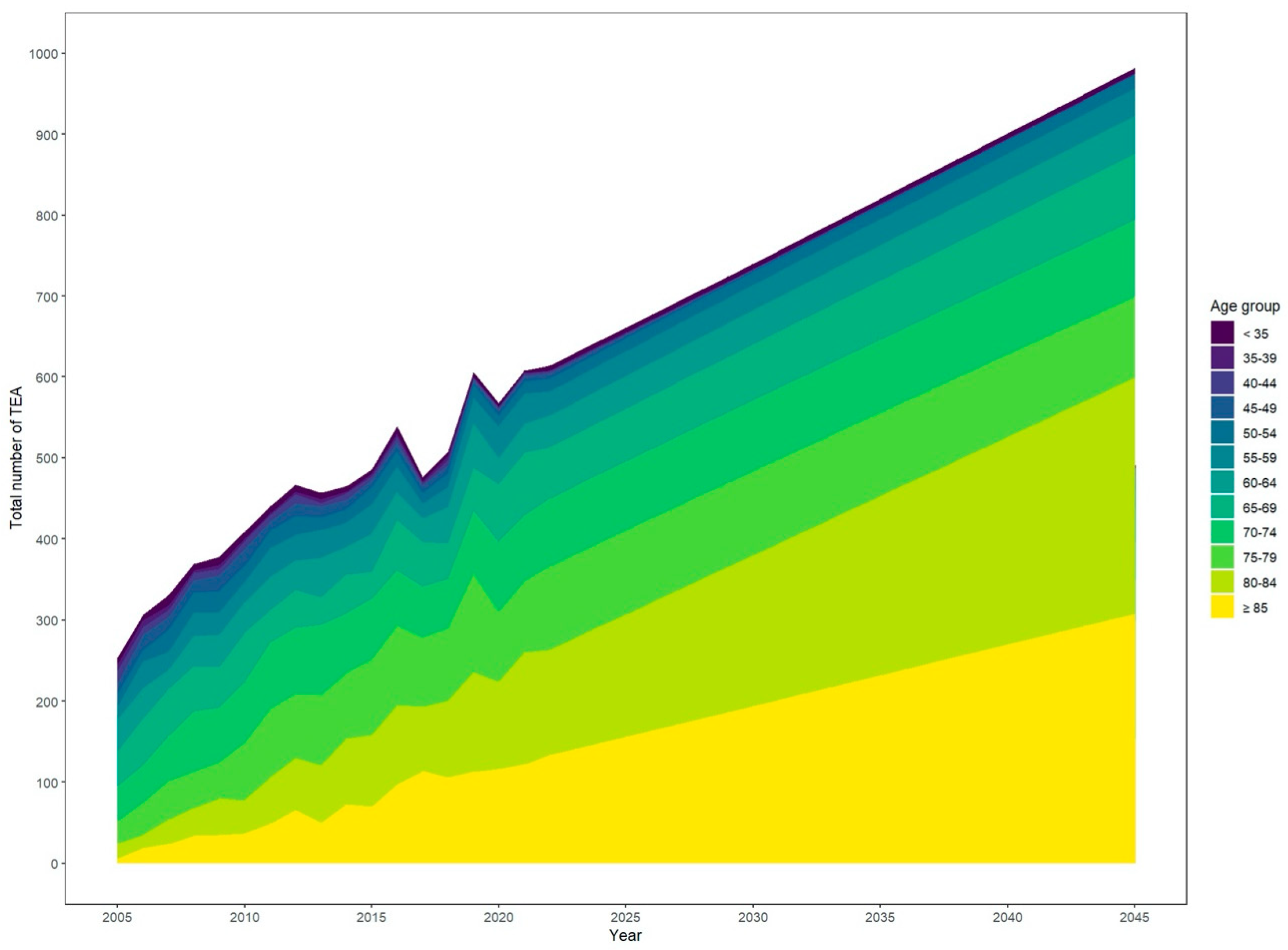
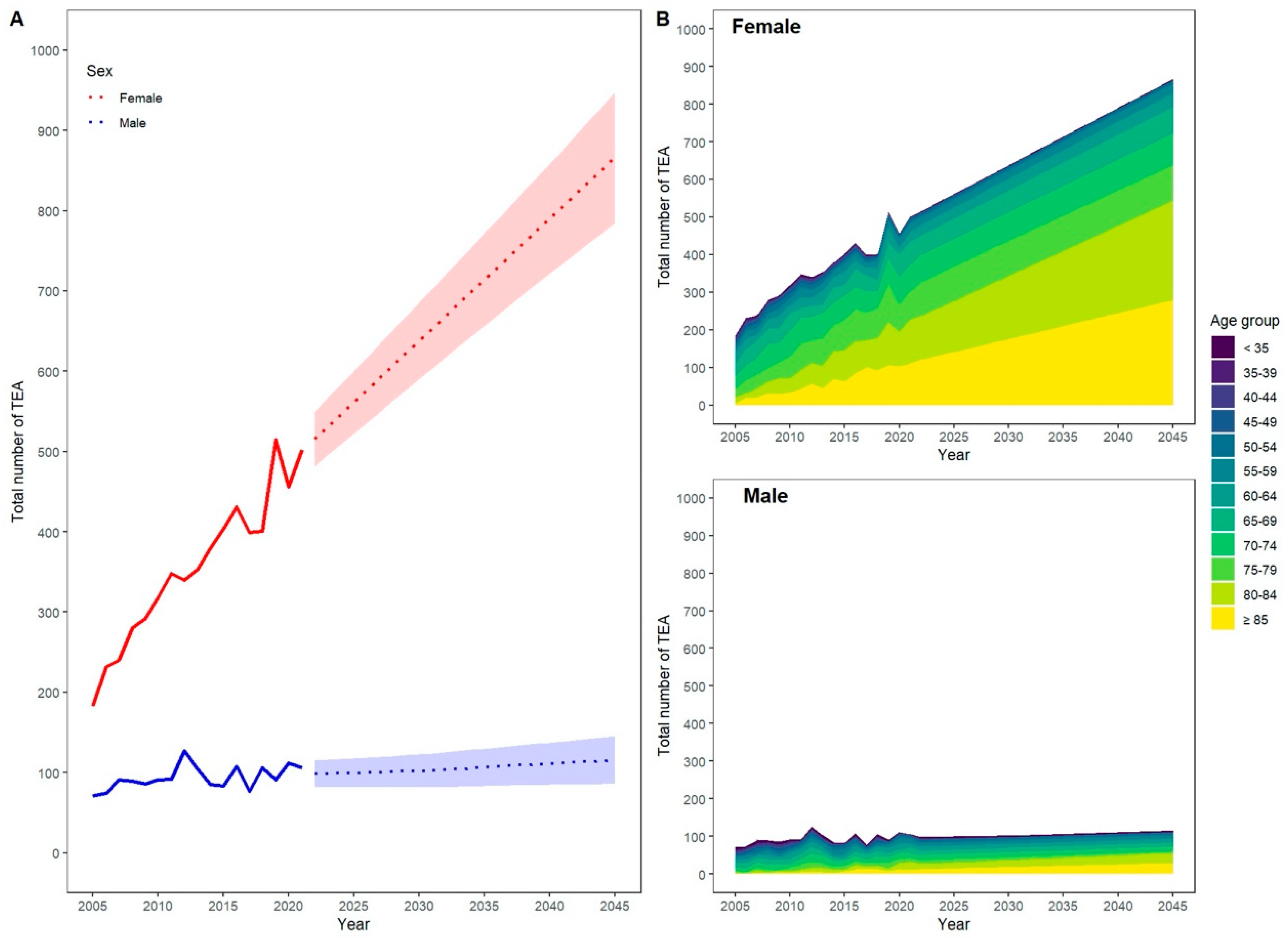
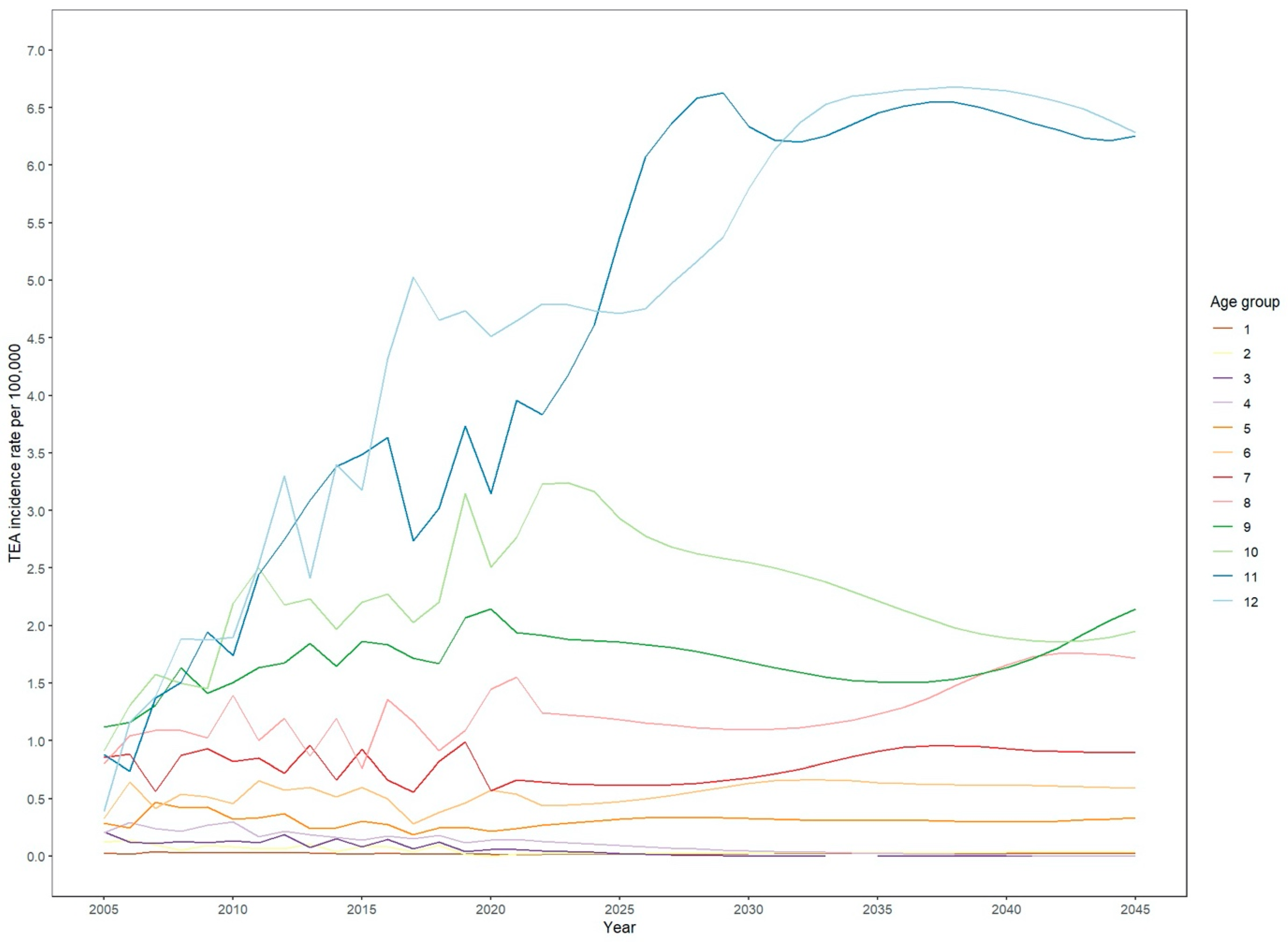
| Year | Absolute Numbers | Relative Increase [%] | Population | Incidence Rate (per 100,000) | Relative Increase [%] |
|---|---|---|---|---|---|
| 2021 | 608 | 82,675,100 | 0.74 | ||
| 2022 | 614 [580–648] | 0.94 | 83,620,000 | 0.73 [0.69–0.77] | −0.20 |
| 2023 | 630 [594–665] | 3.55 | 83,701,000 | 0.75 [0.71–0.79] | 2.28 |
| 2024 | 645 [608–682] | 6.14 | 83,752,000 | 0.77 [0.73–0.81] | 4.77 |
| 2025 | 661 [622–700] | 8.73 | 83,759,000 | 0.79 [0.74–0.84] | 7.32 |
| 2026 | 677 [636–717] | 11.31 | 83,749,000 | 0.81 [0.76–0.86] | 9.88 |
| 2027 | 692 [650–735] | 13.88 | 83,711,000 | 0.83 [0.78–0.88] | 12.47 |
| 2028 | 708 [664–752] | 16.47 | 83,683,000 | 0.85 [0.79–0.90] | 15.06 |
| 2029 | 724 [678–770] | 19.07 | 83,638,000 | 0.87 [0.81–0.92] | 17.70 |
| 2030 | 740 [691–787] | 21.68 | 83,572,000 | 0.89 [0.83–0.94] | 20.37 |
| 2031 | 756 [705–805] | 24.33 | 83,515,000 | 0.91 [0.84–0.96] | 23.08 |
| 2032 | 772 [718–823] | 27.00 | 83,443,000 | 0.93 [0.86–0.99] | 25.83 |
| 2033 | 788 [731–840] | 29.66 | 83,367,000 | 0.95 [0.88–1.01] | 28.58 |
| 2034 | 804 [745–858] | 32.31 | 83,290,000 | 0.97 [0.89–1.03] | 31.34 |
| 2035 | 821 [758–876] | 34.97 | 83,213,000 | 0.99 [0.91–1.05] | 34.10 |
| 2036 | 837 [771–894] | 37.62 | 83,125,000 | 1.01 [0.93–1.08] | 36.88 |
| 2037 | 853 [783–912] | 40.28 | 83,028,000 | 1.03 [0.94–1.10] | 39.68 |
| 2038 | 869 [796–930] | 42.92 | 82,925,000 | 1.05 [0.96–1.12] | 42.49 |
| 2039 | 885 [809–948] | 45.57 | 82,823,000 | 1.07 [0.98–1.15] | 45.31 |
| 2040 | 901 [821–967] | 48.22 | 82,707,000 | 1.09 [0.99–1.17] | 48.16 |
| 2041 | 917 [834–985] | 50.86 | 82,587,000 | 1.11 [1.01–1.19] | 51.02 |
| 2042 | 933 [846–1004] | 53.51 | 82,470,000 | 1.13 [1.03–1.22] | 53.89 |
| 2043 | 949 [858–1023] | 56.16 | 82,330,000 | 1.15 [1.04–1.24] | 56.82 |
| 2044 | 966 [870–1041] | 58.83 | 82,200,000 | 1.17 [1.06–1.27] | 59.75 |
| 2045 | 982 [882–1060] | 61.50 | 82,055,000 | 1.20 [1.07–1.29] | 62.72 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krane, F.; Heck, V.J.; Leyendecker, J.; Klug, K.; Klug, A.; Hackl, M.; Kircher, J.; Müller, L.P.; Leschinger, T. The Future of Total Elbow Arthroplasty: A Statistical Forecast Model for Germany. Healthcare 2024, 12, 1322. https://doi.org/10.3390/healthcare12131322
Krane F, Heck VJ, Leyendecker J, Klug K, Klug A, Hackl M, Kircher J, Müller LP, Leschinger T. The Future of Total Elbow Arthroplasty: A Statistical Forecast Model for Germany. Healthcare. 2024; 12(13):1322. https://doi.org/10.3390/healthcare12131322
Chicago/Turabian StyleKrane, Felix, Vincent Johann Heck, Jannik Leyendecker, Kristina Klug, Alexander Klug, Michael Hackl, Jörn Kircher, Lars Peter Müller, and Tim Leschinger. 2024. "The Future of Total Elbow Arthroplasty: A Statistical Forecast Model for Germany" Healthcare 12, no. 13: 1322. https://doi.org/10.3390/healthcare12131322
APA StyleKrane, F., Heck, V. J., Leyendecker, J., Klug, K., Klug, A., Hackl, M., Kircher, J., Müller, L. P., & Leschinger, T. (2024). The Future of Total Elbow Arthroplasty: A Statistical Forecast Model for Germany. Healthcare, 12(13), 1322. https://doi.org/10.3390/healthcare12131322






