Exploring the Influence of Family Attitudes and Individual Psychological Factors on Antibiotic Utilization: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Questionnaires
2.3.1. Assessment of Individual Traits
2.3.2. Assessment of Practice, Knowledge, and Awareness about Antibiotics and Antibiotic Resistance
2.3.3. Assessment of Individual and Family Approach to Antibiotics
2.4. Data Analysis
3. Results
3.1. Correlational Analyses: Family Examples, Individual Characteristics, and Illness Behavior
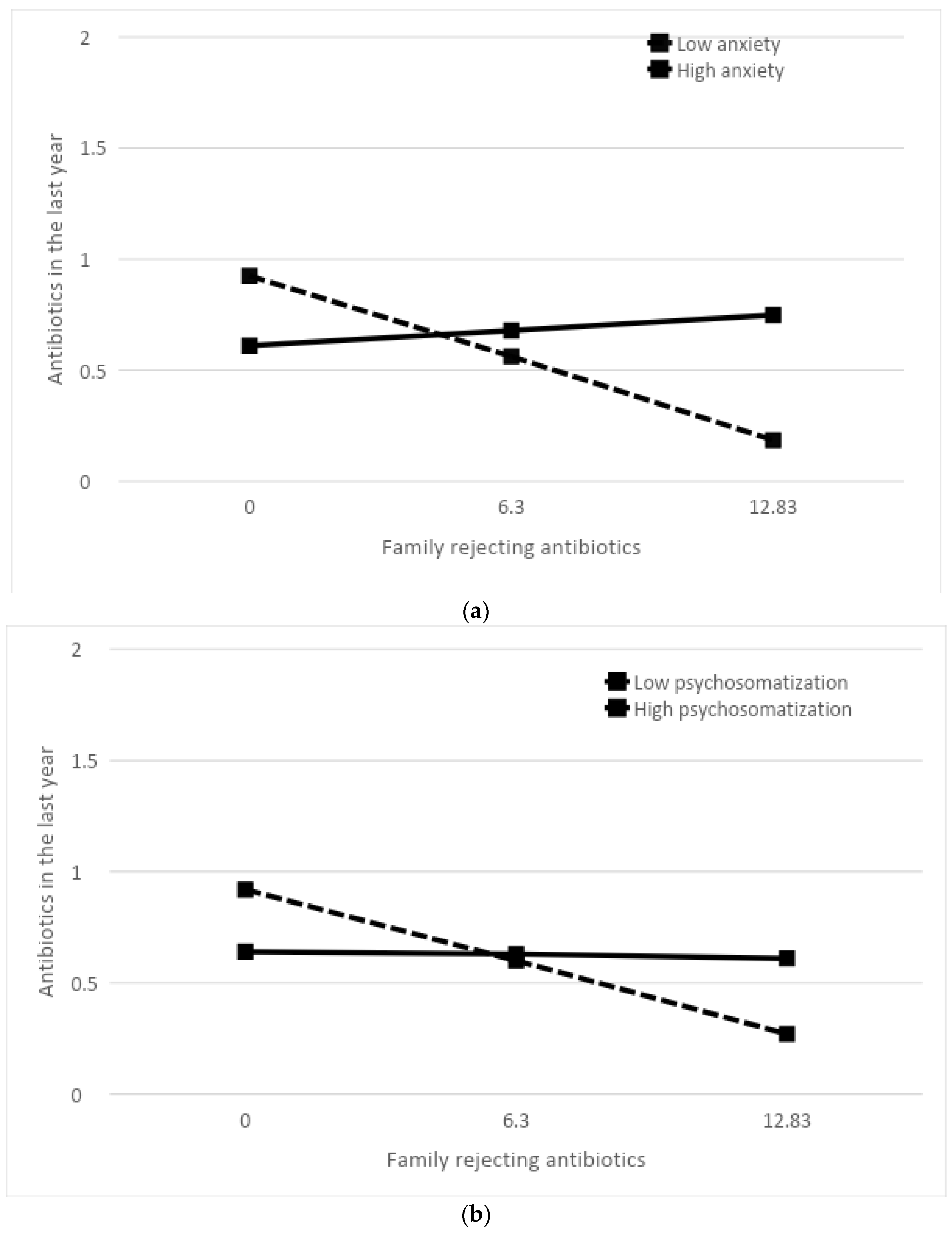
3.2. Moderation Analyses: The Moderating Role of Emotional Well-Being
3.3. Mediation Analysis: The Mediating Role of Awareness
4. Discussion
5. Limitations
6. Implications
7. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Dinan, K.; Dinan, T. Antibiotics and mental health: The good, the bad and the ugly. J. Intern. Med. 2022, 292, 858–869. [Google Scholar] [CrossRef] [PubMed]
- Kraemer, S.A.; Ramachandran, A.; Perron, G.G. Antibiotic Pollution in the Environment: From Microbial Ecology to Public Policy. Microorganisms 2019, 7, 180. [Google Scholar] [CrossRef] [PubMed]
- Munita, J.M.; Arias, C.A. Mechanisms of Antibiotic Resistance. Microbiol. Spectr. 2016, 4, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Mechanic, D. Illness Behaviour: An Overview. In Illness Behavior: A Multidisciplinary Model; McHugh, S., Vallis, T.M., Eds.; Springer: Boston, MA, USA, 1986; pp. 101–109. [Google Scholar] [CrossRef]
- Axelsson, M.; Brink, E.; Lundgren, J.; Lötvall, J. The influence of personality traits on reported adherence to medication in individuals with chronic disease: An epidemiological study in West Sweden. PLoS ONE 2011, 6, e18241. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.M.; Moon, S.J.; Koh, J.H.; Pae, C.U.; Min, J.K. Contribution of Personality Traits, Psychological Factors, and Health-Related Quality of Life to Medication Adherence in Patients with Rheumatoid Arthritis. Yonsei Med. J. 2020, 61, 406–415. [Google Scholar] [CrossRef] [PubMed]
- Emilsson, M.; Gustafsson, P.; Öhnström, G.; Marteinsdottir, I. Impact of personality on adherence to and beliefs about ADHD medication, and perceptions of ADHD in adolescents. BMC Psychiatry 2020, 20, 139. [Google Scholar] [CrossRef] [PubMed]
- Axelsson, M. Report on personality and adherence to antibiotic therapy: A population-based study. BMC Psychol. 2013, 1, 24. [Google Scholar] [CrossRef] [PubMed]
- Linkievicz, N.M.; Sgnaolin, V.; Engroff, P.; Behr Gomes Jardim, G.; Neto Cataldo, A. Association between Big Five personality factors and medication adherence in the elderly. Trends Psychiatry Psychother. 2022, 44, e20200143. [Google Scholar] [CrossRef] [PubMed]
- Faraji, F.; Jalali, R.; Salari, N. The Relationship between Fear of COVID-19 and Self-Medication and the Rate of Antibiotic Use in Patients Referred to COVID-19. Interdiscip. Perspect. Infect. Dis. 2022, 2022, 3044371. [Google Scholar] [CrossRef]
- Nortey, R.A.; Kretchy, I.A.; Koduah, A.; Buabeng, K.O. Biopsychosocial analysis of antibiotic use for the prevention or management of COVID-19 infections: A scoping review. Res. Social. Adm. Pharm. 2023, 19, 573–581. [Google Scholar] [CrossRef]
- Gaygısız, Ü.; Lajunen, T.; Gaygısız, E. Community Use of Antibiotics in Turkey: The Role of Knowledge, Beliefs, Attitudes, and Health Anxiety. Antibiotics 2021, 10, 1171. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Hildon, Z.J.; Lye, D.C.B.; Straughan, P.T.; Chow, A. The Associations between Poor Antibiotic and Antimicrobial Resistance Knowledge and Inappropriate Antibiotic Use in the General Population Are Modified by Age. Antibiotics 2021, 11, 47. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Petelinšek, A.; Lauri Korajlija, A. Predictors of pharmacophobia. Health Psychol. Res. 2020, 8, 8853. [Google Scholar] [CrossRef] [PubMed]
- Alonso-Perez, E.; Gellert, P.; Kreyenfeld, M.; O’Sullivan, J.L.; Consortium for the Proposed Einstein Center for Population Diversity. Family Structure and Family Climate in Relation to Health and Socioeconomic Status for Older Adults: A Longitudinal Moderated Mediation Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11840. [Google Scholar] [CrossRef] [PubMed]
- Woods, S.B.; Priest, J.B.; Roberson, P.N.E. Family versus intimate partners: Estimating who matters more for health in a 20-year longitudinal study. J. Fam. Psychol. 2020, 34, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Michaelson, V.; Pilato, K.A.; Davison, C.M. Family as a health promotion setting: A scoping review of conceptual models of the health-promoting family. PLoS ONE 2021, 16, e0249707. [Google Scholar] [CrossRef] [PubMed]
- Priest, J.B.; Roberson, P.N.E.; Woods, S.B. In Our Lives and Under Our Skin: An Investigation of Specific Psychobiological Mediators Linking Family Relationships and Health Using the Biobehavioral Family Model. Fam. Process 2019, 58, 79–99. [Google Scholar] [CrossRef] [PubMed]
- Hilliard, M.E.; Riekert, K.A.; Hovell, M.F.; Rand, C.S.; Welkom, J.S.; Eakin, M.N. Family Beliefs and Behaviors About Smoking and Young Children’s Secondhand Smoke Exposure. Nicotine Tob. Res. 2015, 17, 1067–1075. [Google Scholar] [CrossRef] [PubMed]
- Bagley, S.M.; Schoenberger, S.F.; dellaBitta, V.; Lunze, K.; Barron, K.; Hadland, S.E.; Park, T.W. An Exploration of Young Adults With Opioid Use Disorder and How Their Perceptions of Family Members’ Beliefs Affects Medication Treatment. J. Addict. Med. 2022, 16, 689–694. [Google Scholar] [CrossRef]
- Kim, Y.; Dillard, J.P.; Smith, R.A. Communicating Antibiotic Stewardship: Emotional Responses and Their Impact on Adherence. Health Commun. 2020, 35, 861–871. [Google Scholar] [CrossRef]
- Burstein, V.R.; Trajano, R.P.; Kravitz, R.L.; Bell, R.A.; Vora, D.; May, L.S. Communication interventions to promote the public’s awareness of antibiotics: A systematic review. BMC Public Health 2019, 19, 899. [Google Scholar] [CrossRef] [PubMed]
- Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Ajzen, I. The theory of planned behavior. In Handbook of Theories of Social Psychology; Van Lange, P.A.M., Kruglanski, A.W., Higgins, E.T., Eds.; Lawrence Erlbaum Associates: New York, NY, USA, 2012; pp. 438–459. [Google Scholar]
- Caprara, G.V.; Barbaranelli, C.; Borgogni, L.; Perugini, M. The “Big five questionnaire”: A new questionnaire to assess the five factor model. Pers. Individ. Differ. 1993, 15, 281–288. [Google Scholar] [CrossRef]
- Spielberger, C.D. State-Trait Anxiety Inventory for Adults; APA PsycTests: Washington, DC, USA, 1983. [Google Scholar]
- Cohen, S.; Kamarck, T.; Mermelstein, R. Perceived stress scale. Meas. Stress Guide Health Soc. Sci. 1994, 10, 1–2. [Google Scholar]
- Hagquist, C. Psychosomatic health problems among adolescents in Sweden—Are the time trends gender related? Eur. J. Public Health 2009, 19, 331–336. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.L.; Woods, S.B.; Sengupta, S.; Nair, T. The Biobehavioral Family Model: An Evidence-Based Approach to Biopsychosocial Research, Residency Training, and Patient Care. Front. Psychiatry 2021, 12, 725045. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.L.; Lim, J.; Miller, B.D.; Cheah, P.; Zwetsch, T.; Ramesh, S.; Simmens, S. Testing the Biobehavioral Family Model in pediatric asthma: Pathways of effect. Fam. Process 2008, 47, 21–40. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.L.; Miller, B.D.; Lehman, H.K. Review of family relational stress and pediatric asthma: The value of biopsychosocial systemic models. Fam. Process 2015, 54, 376–389. [Google Scholar] [CrossRef] [PubMed]
- Khani Jeihooni, A.; Rakhshani, T.; Harsini, P.A.; Layeghiasl, M. Effect of educational program based on theory of planned behavior on promoting nutritional behaviors preventing Anemia in a sample of Iranian pregnant women. BMC Public Health 2021, 21, 2198. [Google Scholar] [CrossRef]
- Wollast, R.; Schmitz, M.; Bigot, A.; Luminet, O. The Theory of Planned Behavior during the COVID-19 pandemic: A comparison of health behaviors between Belgian and French residents. PLoS ONE 2021, 16, e0258320. [Google Scholar] [CrossRef]
- Beisel, C.; Poretta, T.; Sheppard, V.B.; Hurtado-de Mendoza, A.; Sipsma, H.; Fuqua, E.; Stwalley, B.; Salvatore, A.; Yang, M. Adherence to Adjuvant Therapy in Patients with Resected Melanoma: An Application of the Theory of Planned Behavior. Adv. Ther. 2022, 39, 4061–4075. [Google Scholar] [CrossRef] [PubMed]
- Dilekler, İ.; Doğulu, C.; Bozo, Ö. A test of theory of planned behavior in type II diabetes adherence: The leading role of perceived behavioral control. Curr. Psychol. 2019, 40, 3546–3555. [Google Scholar] [CrossRef]
- Şanlıtürk, D.; Ayaz-Alkaya, S. The Effect of a Theory of Planned Behavior Education Program on Asthma Control and Medication Adherence: A Randomized Controlled Trial. J. Allergy Clin. Immunol. Pract. 2021, 9, 3371–3379. [Google Scholar] [CrossRef] [PubMed]
- Adachi, T.; Tsunekawa, Y.; Tanimura, D. Association between the Big Five personality traits and medication adherence in patients with cardiovascular disease: A cross-sectional study. PLoS ONE 2022, 17, e0278534. [Google Scholar] [CrossRef] [PubMed]
- Hazrati-Meimaneh, Z.; Amini-Tehrani, M.; Pourabbasi, A.; Gharlipour, Z.; Rahimi, F.; Ranjbar-Shams, P.; Nasli-Esfahani, E.; Zamanian, H. The impact of personality traits on medication adherence and self-care in patients with type 2 diabetes mellitus: The moderating role of gender and age. J. Psychosom. Res. 2020, 136, 110178, Erratum in J. Psychosom. Res. 2021, 148, 110571. [Google Scholar] [CrossRef] [PubMed]
- Scarella, T.M.; Boland, R.J.; Barsky, A.J. Illness Anxiety Disorder: Psychopathology, Epidemiology, Clinical Characteristics, and Treatment. Psychosom. Med. 2019, 81, 398–407. [Google Scholar] [CrossRef] [PubMed]
- Norbye, A.D.; Abelsen, B.; Førde, O.H.; Ringberg, U. Health anxiety is an important driver of healthcare use. BMC Health Serv. Res. 2022, 22, 138. [Google Scholar] [CrossRef] [PubMed]
- Zhang, A.; Hobman, E.V.; De Barro, P.; Young, A.; Carter, D.J.; Byrne, M. Self-Medication with Antibiotics for Protection against COVID-19: The Role of Psychological Distress, Knowledge of, and Experiences with Antibiotics. Antibiotics 2021, 10, 232. [Google Scholar] [CrossRef] [PubMed]
- Thorgaard, M.V.; Frostholm, L.; Walker, L.; Jensen, J.S.; Morina, B.; Lindegaard, H.; Salomonsen, L.; Rask, C.U. Health anxiety by proxy in women with severe health anxiety: A case control study. J. Anxiety Disord. 2017, 52, 8–14. [Google Scholar] [CrossRef]
- Thorgaard, M.V.; Frostholm, L.; Rask, C.U. Childhood and family factors in the development of health anxiety: A systematic review. Child. Health Care 2018, 47, 198–238. [Google Scholar] [CrossRef]


| Variable | N; M ± SD |
|---|---|
| Gender | 74 F, 26 M |
| Age (M ± SD) | 33.37 ± 11.36 |
| Marital status | 54 Unmarried, 30 Married, 11 Cohabitating, 3 Divorced, 2 Widowed |
| Qualification | 6 Middle School, 37 High School, 46 Degree, 11 PhD/Postgraduate Specialization |
| Occupation | 31 Student, 31 Employee, 6 Freelance, 5 Retired, 4 Unemployed, 23 Other |
| BFQ-Openness (M ± SD) | 3.53 ± 0.64 |
| BFQ-Conscientiousness (M ± SD) | 3.58 ± 0.63 |
| BFQ-Extraversion (M ± SD) | 3.15 ± 0.54 |
| BFQ-Agreeableness (M ± SD) | 3.53 ± 0.52 |
| BFQ-Neuroticism (M ± SD) | 3.19 ± 0.76 |
| STAI-Y2 (M ± SD) | 46.52 ± 12.61 |
| PSS (M ± SD) | 19.27 ± 7.93 |
| PSP (M ± SD) | 20.20 ± 6.23 |
| Family Antibiotic Rejection | 6.30 ± 6.53 |
| Family Antibiotic Appropriate Use | 17.27 ± 3.95 |
| Family Antibiotic Improper Use | 14.86 ± 7.39 |
| Antibiotics taken in the last month * | 92 Never, 5 Once, 2 Twice |
| Antibiotics taken in the last year * | 52 Never, 32 Once, 16 Twice |
| Knowledge of good intake practices | 4.91 ± 1.15 |
| Knowledge of antibiotic resistance | 13.64 ± 1.35 |
| Awareness about antibiotics | 40.40 ± 4.45 |
| Past compliance | 9.08 ± 1.46 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castellano, P.; Russo, P.M.; Mazzetti, M. Exploring the Influence of Family Attitudes and Individual Psychological Factors on Antibiotic Utilization: A Pilot Study. Healthcare 2024, 12, 1213. https://doi.org/10.3390/healthcare12121213
Castellano P, Russo PM, Mazzetti M. Exploring the Influence of Family Attitudes and Individual Psychological Factors on Antibiotic Utilization: A Pilot Study. Healthcare. 2024; 12(12):1213. https://doi.org/10.3390/healthcare12121213
Chicago/Turabian StyleCastellano, Paola, Paolo Maria Russo, and Michela Mazzetti. 2024. "Exploring the Influence of Family Attitudes and Individual Psychological Factors on Antibiotic Utilization: A Pilot Study" Healthcare 12, no. 12: 1213. https://doi.org/10.3390/healthcare12121213
APA StyleCastellano, P., Russo, P. M., & Mazzetti, M. (2024). Exploring the Influence of Family Attitudes and Individual Psychological Factors on Antibiotic Utilization: A Pilot Study. Healthcare, 12(12), 1213. https://doi.org/10.3390/healthcare12121213







