Work-Related Musculoskeletal Disorders Risk Assessment during Manual Lymphatic Drainage with Compressive Bands among Physiotherapists
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Experimental Design
2.3. Data Analysis–Posture Definition
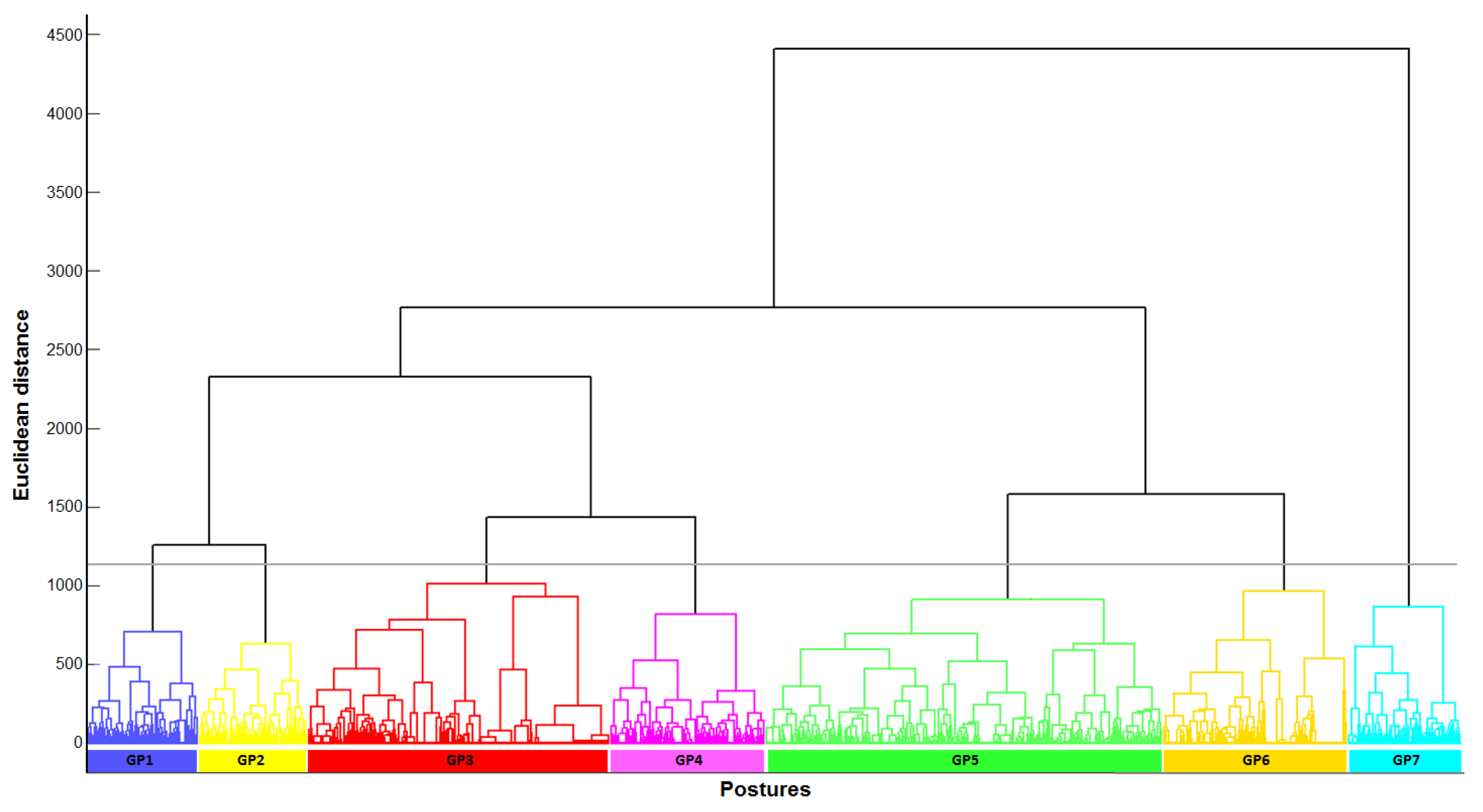
2.4. Data Analysis–Posture Clustering
2.5. Data Analysis–Ergonomic Assessment of Posture
2.6. Statistical Analysis
3. Results
3.1. Generic Posture Definition with the Hierarchical Cluster Analysis
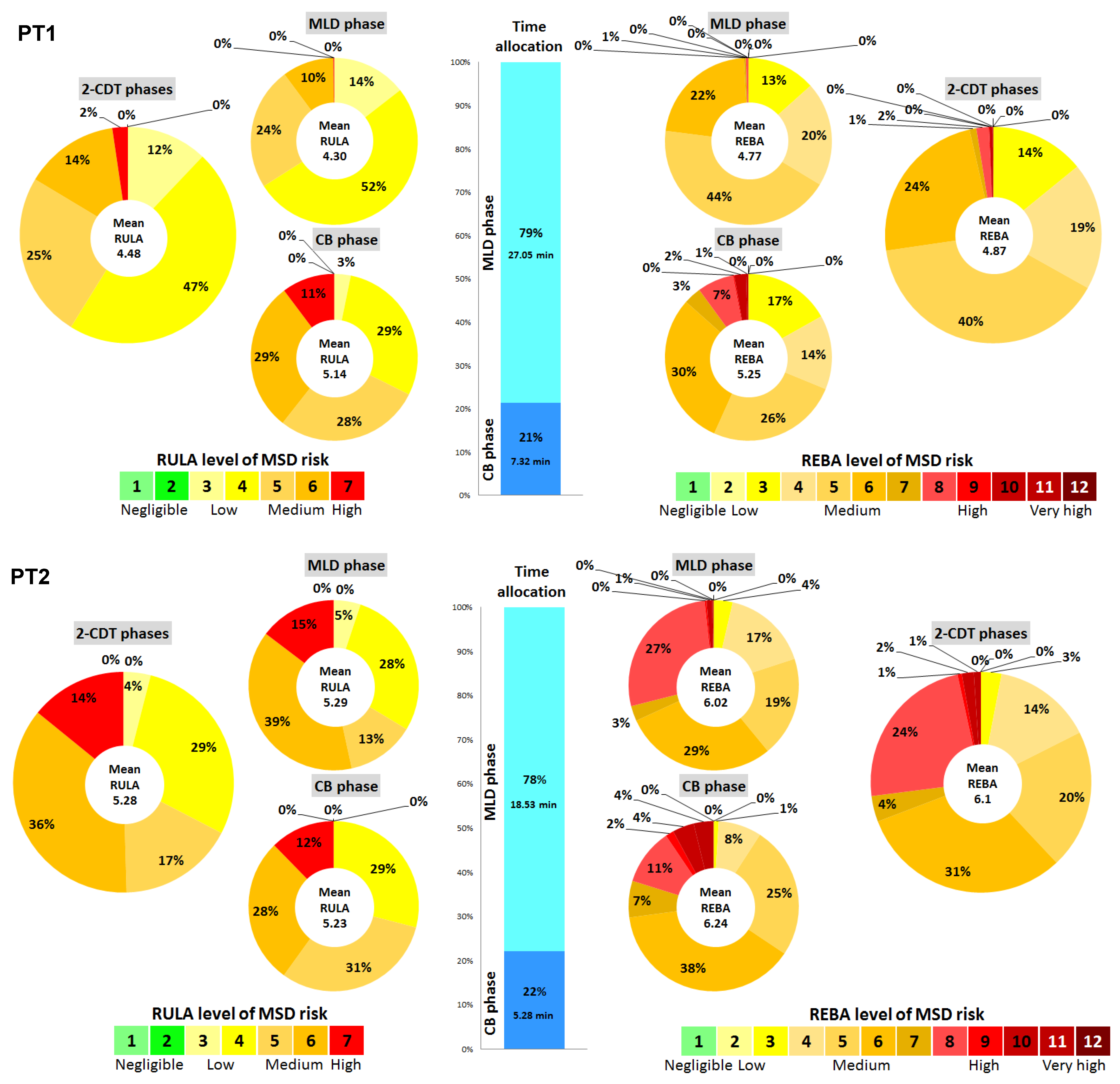
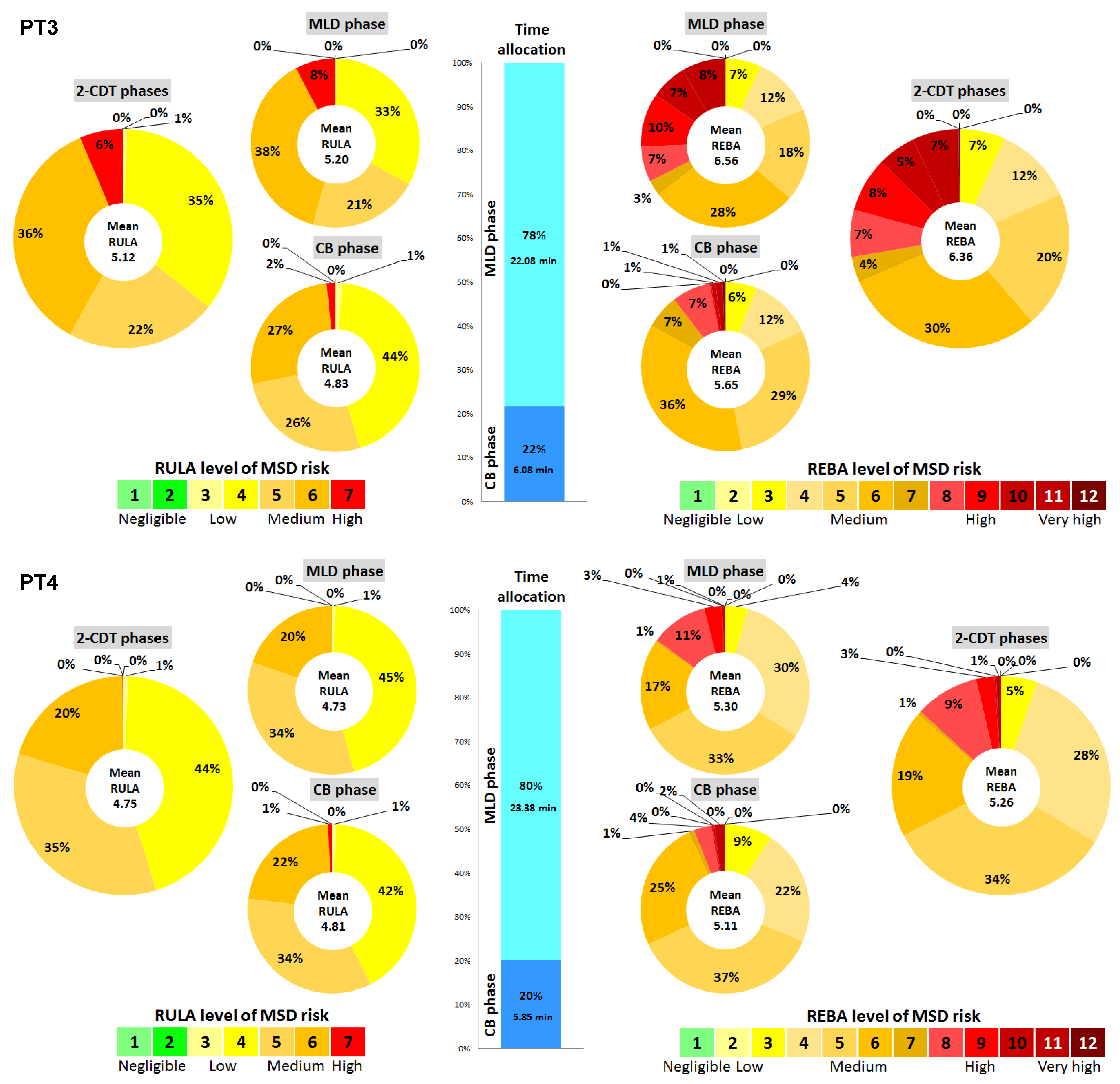
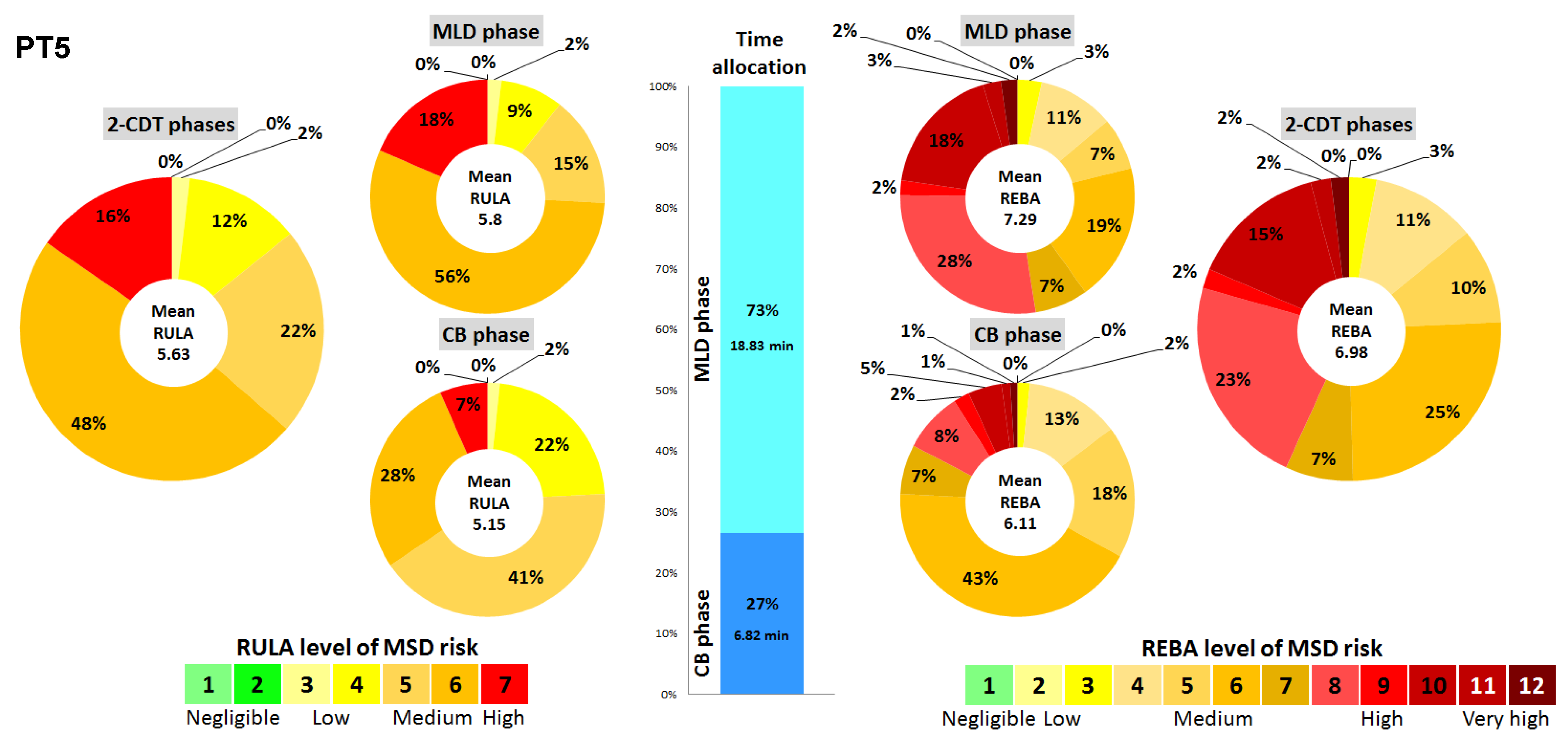
3.2. Ergonomic Assessment of Posture during CDT
3.3. GP Distribution per CDT Phase and Physiotherapist
4. Discussion
- -
- Use foam supports to create support for the upper limbs to reduce muscular strain on the shoulders.
- -
- Position yourself facing the area to be massaged to avoid movements in the frontal plane (abduction and inclination), which increase physical demands and consequently the risk of MSDs.
- -
- Choose postures that are as far away from joint limits as possible.
- -
- Adjust table and seat heights to avoid awkward postures (RULA ≥ 5 and REBA ≥ 4).
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Glover, W.; McGregor, A.; Sullivan, C.; Hague, J. Work-related musculoskeletal disorders affecting members of the Chartered Society of Physiotherapy. Physiotherapy 2005, 91, 138–147. [Google Scholar] [CrossRef]
- Alnaser, M.Z.; Aljadi, S.H. Physical therapists with work-related musculoskeletal disorders in the State of Kuwait: A comparison across countries and health care professions. Work 2019, 63, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Adegoke, B.O.A.; Akodu, A.K.; Oyeyemi, A.L. Work-related musculoskeletal disorders among Nigerian Physiotherapists. BMC Musculoskelet. Disord. 2008, 9, 112. [Google Scholar] [CrossRef] [PubMed]
- Vieira, E.R.; Schneider, P.; Guidera, C.; Gadotti, I.C.; Brunt, D. Work-related musculoskeletal disorders among physical therapists: A systematic review. J. Back. Musculoskelet. Rehabil. 2016, 29, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Cromie, J.E.; Robertson, V.J.; Best, M.O. Work-related musculoskeletal disorders in physical therapists: Prevalence, severity, risks, and responses. Phys. Ther. 2000, 80, 336–351. [Google Scholar] [CrossRef] [PubMed]
- Vieira, E.R.; Svoboda, S.; Belniak, A.; Brunt, D.; Rose-St Prix, C.; Roberts, L.; da Costa, B.R. Work-related musculoskeletal disorders among physical therapists: An online survey. Disabil. Rehabil. 2016, 38, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Anyfantis, I.D.; Biska, A. Musculoskeletal Disorders Among Greek Physiotherapists: Traditional and Emerging Risk Factors. Saf. Health Work 2018, 9, 314–318. [Google Scholar] [CrossRef]
- Meh, J.; Bizovičar, N.; Kos, N.; Jakovljević, M. Work-related musculoskeletal disorders among Slovenian physiotherapists. J. Health Sci. 2020, 10, 115–124. [Google Scholar] [CrossRef]
- Gorce, P.; Jacquier-Bret, J. Global prevalence of musculoskeletal disorders among physiotherapists: A systematic review and meta-analysis. BMC Musculoskelet. Disord. 2023, 24, 265. [Google Scholar] [CrossRef]
- Grooten, W.J.A.; Wernstedt, P.; Campo, M. Work-related musculoskeletal disorders in female Swedish physical therapists with more than 15 years of job experience: Prevalence and associations with work exposures. Physiother. Theory Pract. 2011, 27, 213–222. [Google Scholar]
- Albert, W.J.; Currie-Jackson, N.; Duncan, C.A. A survey of musculoskeletal injuries amongst Canadian massage therapists. J. Bodyw. Mov. Ther. 2008, 12, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Holder, N.; Clark, H.A.; DiBlasio, J.M.; Hughes, C.; Scherpf, J.W.; Harding, L.; Shepard, K.F. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys. Ther. 1999, 79, 642–652. [Google Scholar] [CrossRef] [PubMed]
- Chung, S.; Her, J.; Ko, T.; Ko, J.; Kim, H.; Lee, J.; Woo, J.-H. Work-related Musculoskeletal Disorders among Korean Physical Therapists. J. Phys. Ther. Sci. 2013, 25, 55–59. [Google Scholar] [CrossRef][Green Version]
- Muaidi, Q.; Shanb, A. Prevalence causes and impact of work related musculoskeletal disorders among physical therapists. J. Back. Musculoskelet. Rehabil. 2016, 29, 763–769. [Google Scholar] [CrossRef] [PubMed]
- Kinaci, E.; AtaoĞLu, S. Work Related Musculoskeletal Disorders Among the Physiotherapists: Sample of a Region in Turkey. Turk. Klin. J. Med. Sci. 2020, 5, 495–502. [Google Scholar] [CrossRef]
- West, D.J.; Gardner, D. Occupational injuries of physiotherapists in North and Central Queensland. Aust. J. Physiother. 2001, 47, 179–186. [Google Scholar] [CrossRef]
- Yoopat, P.; Yuangnoon, A.; Krukimsom, K.; Vanwonterghem, K. Risk Assessment for Work-Related Musculoskeletal Disorders in Thai Traditional Massage Therapists. J. Physiol. Biomed. Sci. 2018, 31, 24–31. [Google Scholar]
- Głowiński, S.; Bryndal, A.; Grochulska, A. Prevalence and risk of spinal pain among physiotherapists in Poland. PeerJ 2021, 9, e11715. [Google Scholar] [CrossRef]
- Lasinski, B.B.; Thrift, K.M.; Squire, D.; Austin, M.K.; Smith, K.M.; Wanchai, A.; Green, J.M.; Stewart, B.R.; Cormier, J.N.; Armer, J.M. A Systematic Review of the Evidence for Complete Decongestive Therapy in the Treatment of Lymphedema From 2004 to 2011. PM&R 2012, 4, 580–601. [Google Scholar] [CrossRef]
- Lymphology, I.S.o. The diagnosis and treatment of peripheral lymphedema. 2009 Concensus Document of the International Society of Lymphology. Lymphology 2003, 42, 51–60. [Google Scholar]
- Poage, E.; Singer, M.; Armer, J.M.; Poundall, M.; Shellabarger, M.J. Demystifying lymphedema: Development of the lymphedema putting evidence into practice card. Clin. J. Oncol. Nurs. 2008, 12, 951–964. [Google Scholar] [CrossRef] [PubMed]
- Jacquier-Bret, J.; Gorce, P.; Rouvière, E. Ergonomic risk assessment during massage among physiotherapists: Introduction of Generic Postures notion. Work 2023, 75, 1021–1029. [Google Scholar] [CrossRef]
- Jacquier-Bret, J.; Gorce, P. Six-Month Work Related Musculoskeletal Disorders Assessment During Manual Lymphatic Drainage: A Physiotherapist Case Report. Int. J. Health Sci. Res. 2022, 12, 148–153. [Google Scholar] [CrossRef]
- McAtamney, L.; Corlett, N.E. RULA: A survey method for the investigation of work-related upper limb disorders. Appl. Ergon. 1993, 24, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Hignett, S.; McAtamney, L. Rapid Entire Body Assessment (REBA). Appl. Ergon. 2000, 31, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Gorce, P.; Jacquier-Bret, J. Three-month work-related musculoskeletal disorders assessment during manual lymphatic drainage in physiotherapists using Generic Postures notion. J. Occup. Health 2023, 65, e12420. [Google Scholar] [CrossRef]
- Kuorinka, I.; Jonsson, B.; Kilbom, A.; Vinterberg, H.; Biering-Sørensen, F.; Andersson, G.; Jørgensen, K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl. Ergon. 1987, 18, 233–237. [Google Scholar] [CrossRef]
- World Medical, A. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Wu, G.; Siegler, S.; Allard, P.; Kirtley, C.; Leardini, A.; Rosenbaum, D.; Whittle, M.; D’Lima, D.D.; Cristofolini, L.; Witte, H.; et al. ISB recommendation on definitions of joint coordinate system of various joints for the reporting of human joint motion—Part I: Ankle, hip, and spine. J. Biomech. 2002, 35, 543–548. [Google Scholar] [CrossRef]
- Wu, G.; van der Helm, F.C.T.; Veeger, H.E.J.; Makhsous, M.; Van Roy, P.; Anglin, C.; Nagels, J.; Karduna, A.R.; McQuade, K.; Wang, X.; et al. ISB recommendation on definitions of joint coordinate systems of various joints for the reporting of human joint motion—Part II: Shoulder, elbow, wrist and hand. J. Biomech. 2005, 38, 981–992. [Google Scholar] [CrossRef]
- Ward, J.H. Hierarchical Grouping to Optimize an Objective Function. J. Am. Stat. Assoc. 1963, 58, 236–244. [Google Scholar] [CrossRef]
- Kee, D. Comparison of OWAS, RULA and REBA for assessing potential work-related musculoskeletal disorders. Int. J. Ind. Ergon. 2021, 83, 103140. [Google Scholar] [CrossRef]
- Chiasson, M.-È.; Imbeau, D.; Aubry, K.; Delisle, A. Comparing the results of eight methods used to evaluate risk factors associated with musculoskeletal disorders. Int. J. Ind. Ergon. 2012, 42, 478–488. [Google Scholar] [CrossRef]
- de Leva, P. Adjustments to Zatsiorsky-Seluyanov’s segment inertia parameters. J. Biomech. 1996, 29, 1223–1230. [Google Scholar] [CrossRef]
- Khairy, W.A.; Bekhet, A.H.; Sayed, B.; Elmetwally, S.E.; Elsayed, A.M.; Jahan, A.M. Prevalence, Profile, and Response to Work-Related Musculoskeletal Disorders among Egyptian Physiotherapists. Open Access Maced. J. Med. Sci. 2019, 7, 1692–1699. [Google Scholar] [CrossRef]
- Jang, Y.; Chi, C.-F.; Tsauo, J.-Y.; Wang, J.-D. Prevalence and Risk Factors of Work-Related Musculoskeletal Disorders in Massage Practitioners. J. Occup. Rehabil. 2006, 16, 425–638. [Google Scholar] [CrossRef]

| GP1 | GP2 | GP3 | GP4 | GP5 | GP6 | GP7 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
 |  |  |  |  |  |  | ||||||||
| Neck flexion (°) | 26.74 | (9.07) #343567 | 27.38 | (9.50) #343567 | 20.92 | (7.33) #12457 | 23.27 | (7.01) #12367 | 20.10 | (11.48) #12467 | 23.06 | (9.46) #12357 | 25.82 | (10.76) #123456 |
| Neck inclination (°) | 5.52 | (6.44) #234567 | 3.99 | (5.84) #1346 | 5.33 | (8.34) #1257 | 7.51 | (7.66) #1257 | 2.94 | (4.08) #13456 | 6.05 | (9.09) #1257 | 3.63 | (5.15) #1346 |
| Neck rotation (°) | 2.82 | (3.50) #23467 | 3.03 | (6.27) #15 | 2.68 | (4.55) #14567 | 2.39 | (2.84) #135 | 5.44 | (8.56) #23456 | 3.04 | (4.19) #135 | 2.57 | (3.78) #135 |
| Trunk flexion (°) | 30.32 | (10.46) #234567 | 26.21 | (11.86) #13567 | 15.68 | (8.99) #124567 | 23.81 | (7.39) #13567 | 15.05 | (7.56) #12347 | 13.52 | (9.36) #12347 | 29.27 | (12.70) #123456 |
| Trunk inclination (°) | 7.42 | (8.14) #34567 | 7.96 | (8.32) #467 | 8.19 | (7.99) #1467 | 17.21 | (11.04) #123567 | 7.33 | (6.67) #1467 | 10.38 | (8.72) #123457 | 4.21 | (5.54) #123456 |
| Trunk rotation (°) | 4.67 | (6.01) #56 | 4.13 | (6.05) #3456 | 7.60 | (8.45) #2567 | 5.29 | (5.56) #2567 | 10.62 | (10.77) #12347 | 8.59 | (9.03) #12347 | 3.49 | (4.86) #3456 |
| Shoulder flexion (°) | 35.89 | (16.96) #23567 | 25.46 | (15.24) #13457 | 51.63 | (15.54) #124567 | 35.38 | (11.86) #23567 | 13.81 | (12.67) #123467 | 27.25 | (13.87) #13457 | 21.73 | (15.11) #123456 |
| Shoulder abduction (°) | 25.06 | (13.53) #34567 | 23.17 | (15.06) #456 | 23.48 | (16.61) #14567 | 30.14 | (12.59) #123567 | 13.03 | (9.93) #123467 | 49.50 | (18.90) #123457 | 20.42 | (14.86) #13456 |
| Elbow flexion (°) | 38.63 | (13.71) #234567 | 85.49 | (8.75) #13467 | 44.89 | (16.53) #124567 | 59.99 | (20.05) #123567 | 86.65 | (14.51) #13467 | 84.06 | (16.33) #123457 | 65.10 | (25.95) #123456 |
| Hip flexion (°) | 75.60 | (17.76) #34567 | 72.64 | (15.85) #34567 | 84.20 | (8.17) #12457 | 87.57 | (6.65) #123567 | 85.47 | (7.02) #123467 | 83.56 | (6.50) #12457 | 5.37 | (15.16) #123456 |
| Hip abduction (°) | 11.19 | (13.75) #34567 | 8.66 | (12.79) #34567 | −2.84 | (7.85) #12467 | 27.04 | (6.73) #123567 | −1.61 | (12.99) #12467 | −4.41 | (7.80) #123457 | 0.00 | (0.00) #123456 |
| Hip rotation (°) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) | 0.47 | (5.97) | 0.00 | (0.00) | 0.00 | (0.00) | 0.00 | (0.00) |
| Knee flexion (°) | 134.60 | (11.16) #34567 | 133.57 | (12.98) #34567 | 84.27 | (6.92) #12457 | 90.07 | (2.58) #123567 | 88.70 | (5.18) #123467 | 83.61 | (11.80) #12457 | 0.18 | (1.53) #123456 |
| Frequency (%) | 8.13% | 7.88% | 22.11% | 11.21% | 28.98% | 13.55% | 8.14% | |||||||
| GP1 | GP2 | GP3 | GP4 | GP5 | GP6 | GP7 | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| RULA score distribution by GP | 1 | - | - | - | - | - | - | - | ||
| 2 | - | - | - | - | - | - | - | RULA level of MSD risk | ||
| 3 | 0.7% | 1.9% | 4.1% | 3.4% | 8.7% | 0.3% | 2.0% | 1–2 | Negligible risk. No action is needed | |
| 4 | 10.9% | 41.2% | 27.6% | 14.8% | 46.1% | 48.1% | 35.4% | 3–4 | Low risk. Change may be needed | |
| 5 | 32.9% | 23.7% | 20.3% | 16.2% | 31.3% | 10.6% | 38.7% | 5–6 | Medium risk. Further investigation. change soon | |
| 6 | 42.2% | 31.1% | 33.6% | 46.8% | 13.8% | 38.7% | 21.4% | 6+ | High risk. Investigate and implement the change now | |
| 7 | 13.2% | 2.1% | 14.4% | 18.7% | 0.1% | 2.2% | 2.5% | |||
| Mean RULA score | 5.56 (0.88) #23567 | 4.90 (0.94) #1345 | 5.27 (1.13) #124567 | 5.63 (1.05) #23567 | 4.51 (0.84) #123467 | 4.94 (0.98) #1345 | 4.87 (0.86) #1345 | |||
| REBA score distribution by GP | 1 | - | - | - | - | - | - | - | ||
| 2 | - | - | - | - | - | - | - | |||
| 3 | 1.7% | 8.7% | - | 0.3% | 15.6% | 5.4% | 9.9% | |||
| 4 | 2.8% | 15.6% | 3.7% | 8.3% | 30.2% | 28.5% | 18.0% | REBA level of MSD risk | ||
| 5 | 15.4% | 27.7% | 38.5% | 19.4% | 19.6% | 26.4% | 31.9% | 1 | Negligible risk. No action is needed | |
| 6 | 40.6% | 30.5% | 32.7% | 18.3% | 18.9% | 17.0% | 33.6% | 2–3 | Low risk. Change may be needed | |
| 7 | 10.2% | 0.9% | 5.9% | 3.7% | 0.6% | 1.5% | 1.2% | 4–7 | Medium risk. Further investigation. change soon | |
| 8 | 16.1% | 12.7% | 7.0% | 28.8% | 12.5% | 7.1% | 2.2% | 8–10 | High risk. Investigate and implement change | |
| 9 | 1.7% | 1.8% | 2.3% | 1.1% | 2.0% | 8.3% | 1.2% | 11+ | Very high risk. Implement the change now | |
| 10 | 8.6% | 0.7% | 5.9% | 17.2% | 0.1% | 0.7% | 1.2% | |||
| 11 | 1.5% | 1.2% | 3.6% | 1.9% | 0.5% | 5.1% | 0.6% | |||
| 12 | 1.5% | 0.1% | 0.4% | 1.1% | 0.0% | 0.0% | 0.4% | |||
| Mean REBA score | 6.72 (1.75) #23567 | 5.57 (1.63) #13457 | 6.25 (1.74) #124567 | 7.12 (2.05) #23567 | 5.08 (1.67) #123467 | 5.69 (2.06) #1345 | 5.22 (1.42) #12345 | |||
| PT1 | PT2 | PT3 | PT4 | PT5 | RULA | REBA | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MLD | CB | MLD + CB | MLD | CB | MLD + CB | MLD | CB | MLD + CB | MLD | CB | MLD + CB | MLD | CB | MLD + CB | ||||
| GP1 | Freq. (%) | - | 15.9% | 3.4% | - | 3.8% | 0.8% | - | 26.3% | 5.7% | 5.5% | 33.3% | 11.1% | 13.4% | 40.3% | 20.6% | 5.56 | 6.72 |
| GP2 | Freq. (%) | - | 14.8% | 3.2% | - | 6.0% | 1.3% | - | 65.2% | 14.1% | 2.1% | 41.6% | 10.0% | 7.7% | 20.3% | 11.0% | 4.90 | 5.57 |
| GP3 | Freq. (%) | 46.4% | - | 36.5% | 18.3% | 13.2% | 17.1% | 38.6% | - | 30.2% | 17.2% | - | 13.8% | 10.9% | - | 8.0% | 5.27 | 6.25 |
| GP4 | Freq. (%) | 2.9% | - | 2.3% | 10.9% | 4.1% | 9.4% | - | - | - | 12.5% | - | 10.0% | 52.0% | 1.0% | 38.5% | 5.63 | 7.12 |
| GP5 | Freq. (%) | 34.3% | 0.2% | 27.1% | 62.1% | 25.9% | 54.0% | 26.3% | 2.5% | 21.2% | 46.3% | 4.3% | 37.9% | 9.2% | - | 6.7% | 4.51 | 5.08 |
| GP6 | Freq. (%) | 16.4% | 7.5% | 14.5% | 8.8% | 15.8% | 10.4% | 33.8% | - | 26.5% | 12.2% | 0.9% | 9.9% | 6.9% | 0.5% | 5.2% | 4.94 | 5.69 |
| GP7 | Freq. (%) | - | 61.5% | 13.1% | - | 31.2% | 6.9% | 1.3% | 6.0% | 2.3% | 4.1% | 19.9% | 7.2% | - | 37.9% | 10.1% | 4.87 | 5.22 |
| Mean RULA score from GP | 4.97 | 4.98 | 4.98 | 4.81 | 4.90 | 4.82 | 4.95 | 5.06 | 4.98 | 4.91 | 5.10 | 4.95 | 5.38 | 5.16 | 5.32 | |||
| Mean REBA score from GP | 5.78 | 5.54 | 5.74 | 5.58 | 5.55 | 5.56 | 5.74 | 5.84 | 5.76 | 5.71 | 5.86 | 5.74 | 6.57 | 5.92 | 6.40 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jacquier-Bret, J.; Gorce, P. Work-Related Musculoskeletal Disorders Risk Assessment during Manual Lymphatic Drainage with Compressive Bands among Physiotherapists. Healthcare 2024, 12, 118. https://doi.org/10.3390/healthcare12010118
Jacquier-Bret J, Gorce P. Work-Related Musculoskeletal Disorders Risk Assessment during Manual Lymphatic Drainage with Compressive Bands among Physiotherapists. Healthcare. 2024; 12(1):118. https://doi.org/10.3390/healthcare12010118
Chicago/Turabian StyleJacquier-Bret, Julien, and Philippe Gorce. 2024. "Work-Related Musculoskeletal Disorders Risk Assessment during Manual Lymphatic Drainage with Compressive Bands among Physiotherapists" Healthcare 12, no. 1: 118. https://doi.org/10.3390/healthcare12010118
APA StyleJacquier-Bret, J., & Gorce, P. (2024). Work-Related Musculoskeletal Disorders Risk Assessment during Manual Lymphatic Drainage with Compressive Bands among Physiotherapists. Healthcare, 12(1), 118. https://doi.org/10.3390/healthcare12010118







