Intraindividual Left–Right Side Differences of Sagittal Condylar Inclination (SCI) in Different Skeletal Classes
Abstract
1. Introduction
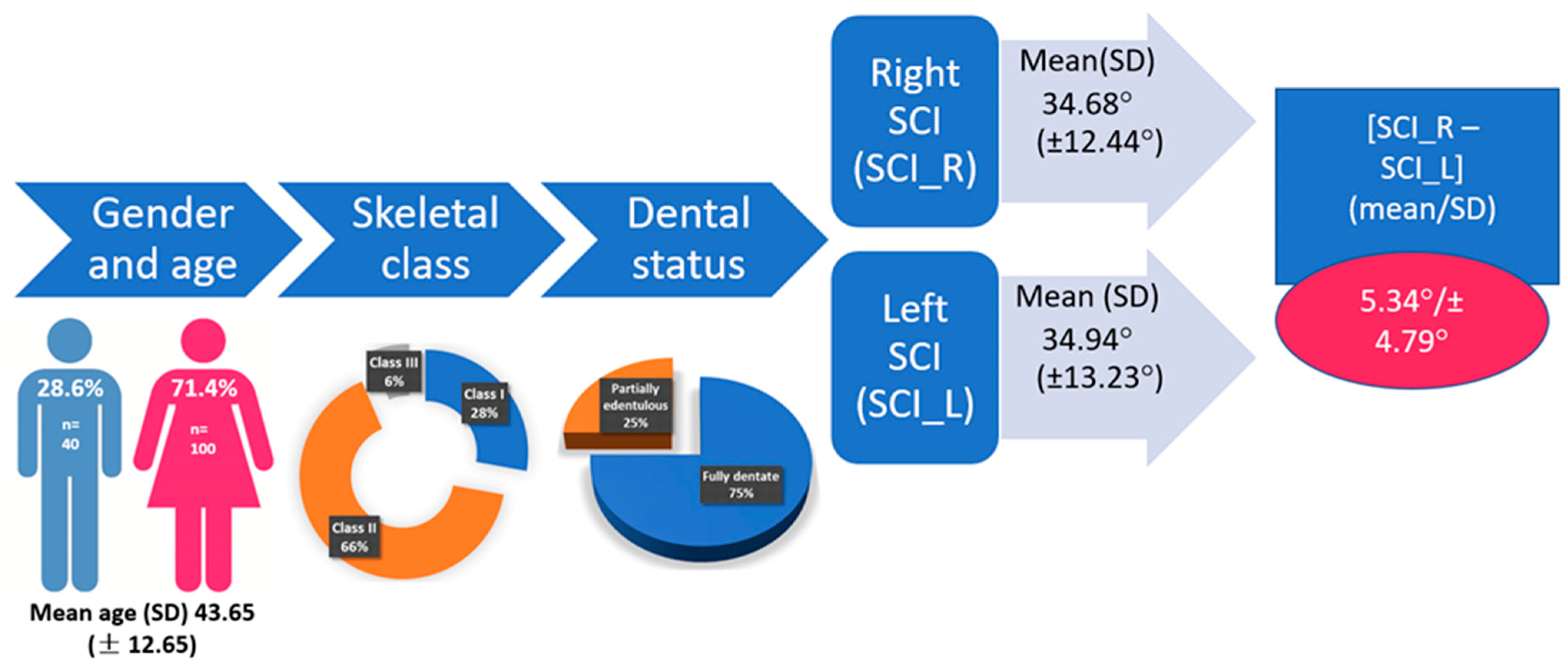
2. Materials and Methods
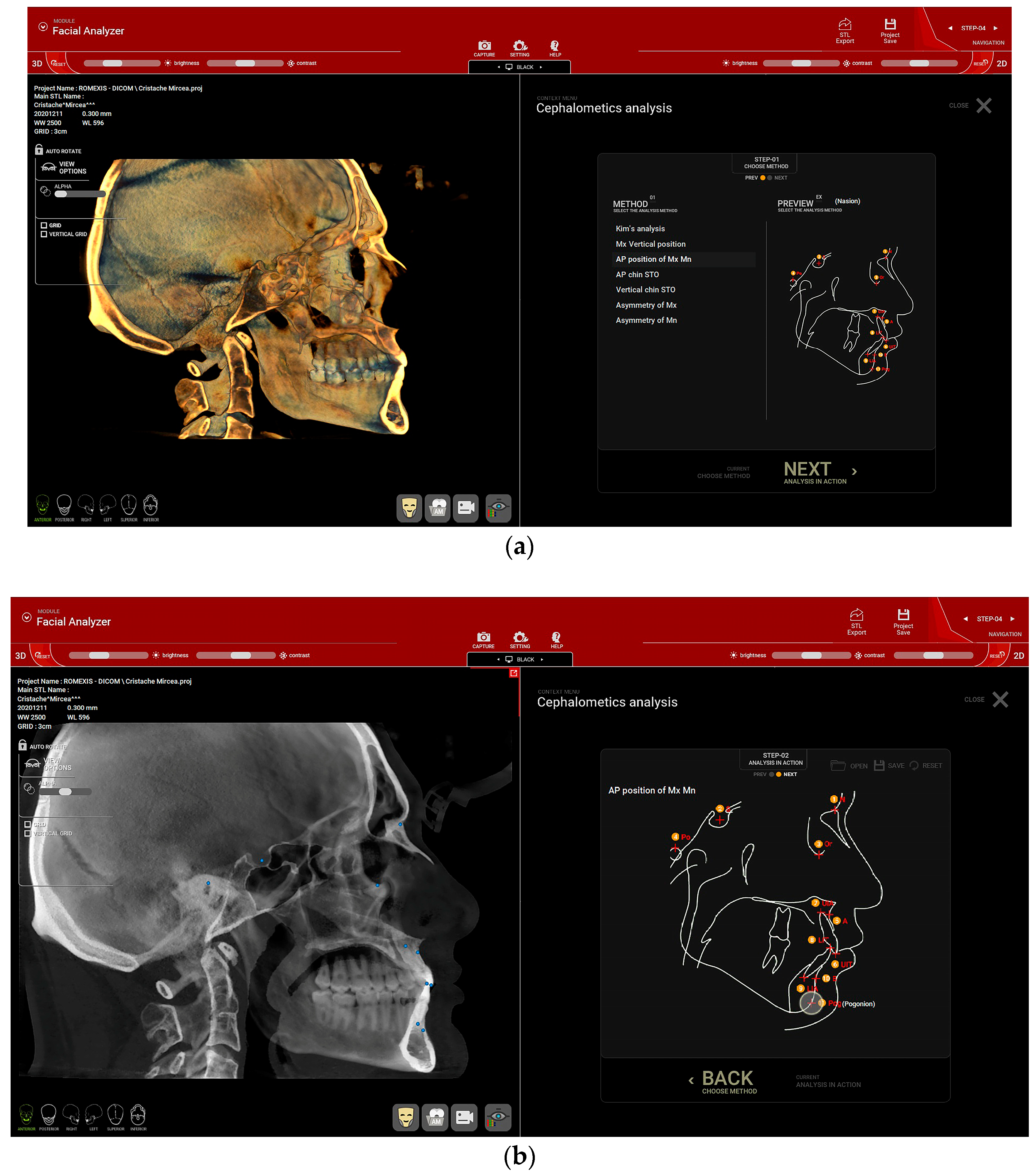
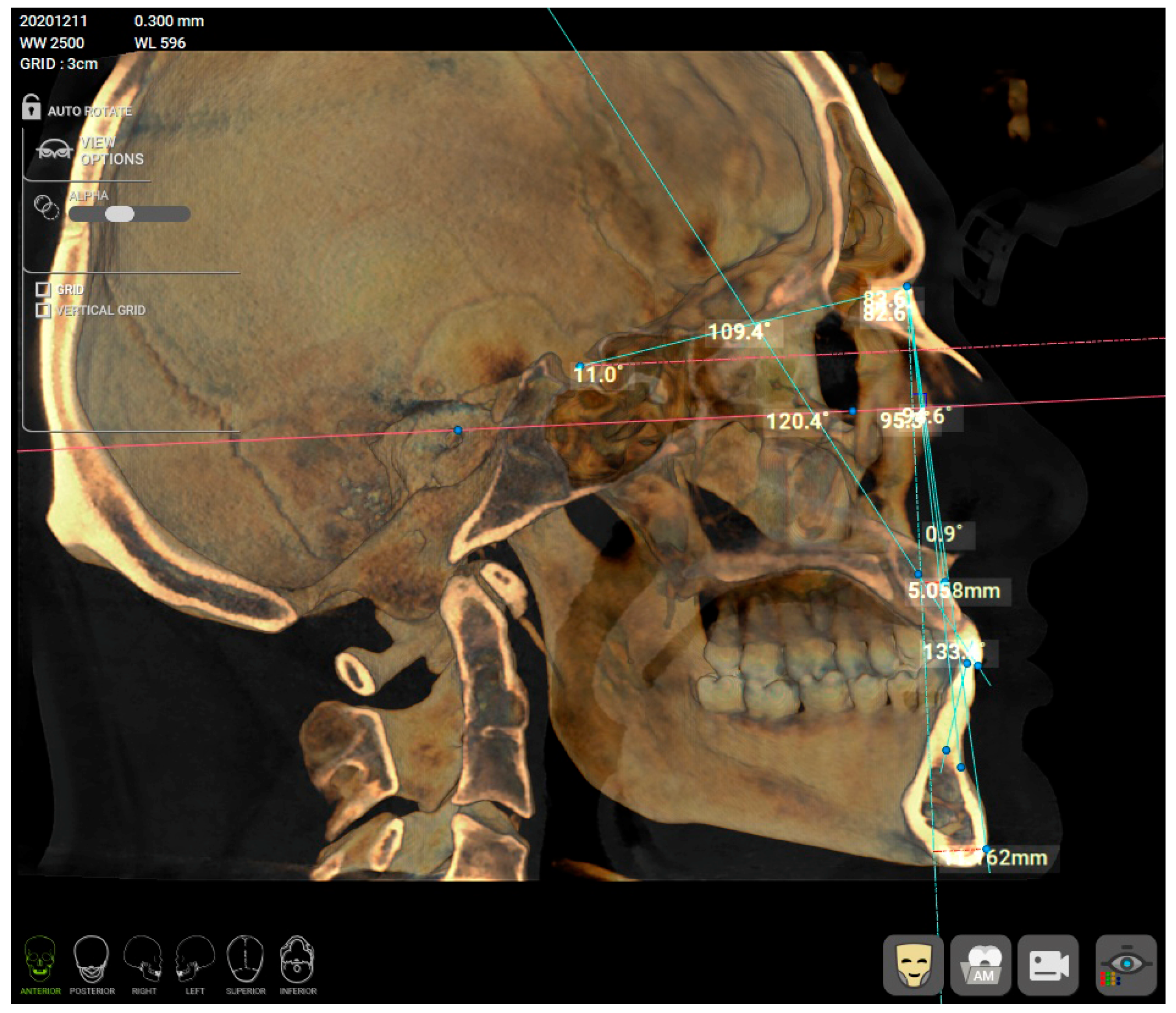
2.1. Skeletal Class
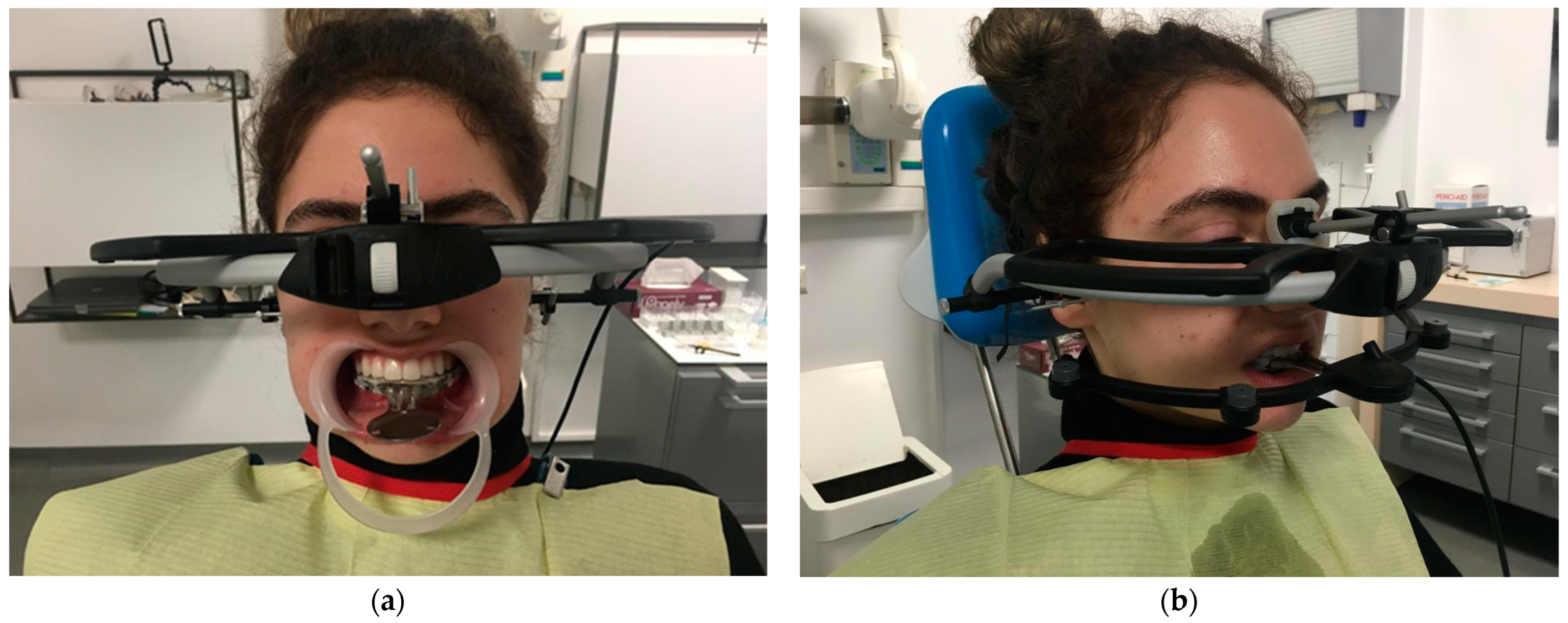
2.2. Condylography
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Chang, C.-L.; Wang, D.-H.; Yang, M.-C.; Hsu, W.-E.; Hsu, M.-L. Functional disorders of the temporomandibular joints: Internal derangement of the temporomandibular joint. Kaohsiung J. Med. Sci. 2018, 34, 223–230. [Google Scholar] [CrossRef]
- Tanteri, G.; Tanteri, E.; Tanteri, C.; Slavicek, G. TMJ Dynamics. In MRI of the Temporomandibular Joint; Robba, T., Tanteri, C., Tanteri, G., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 57–90. [Google Scholar]
- Sójka, A.; Huber, J.; Kaczmarek, E.; Hędzelek, W. Evaluation of mandibular movement functions using instrumental ultrasound system. J. Prosthodont. 2017, 26, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.A. The temporomandibular joint examination. In Clinical Methods: The History, Physical, and Laboratory Examinations, 3rd ed.; Walker, H.K., Hall, W.D., Hurst, J.W., Eds.; Butterworths: Boston, MA, USA, 1990. [Google Scholar]
- Franklin, C.D. Pathology of the temporomandibular joint. Curr. Diagn. Pathol. 2006, 12, 31–39. [Google Scholar] [CrossRef]
- Ferneini, E.M. Temporomandibular Joint Disorders (TMD). J. Oral. Maxillofac. Surg. 2021, 79, 2171–2172. [Google Scholar] [CrossRef]
- Cascone, P.; Gennaro, P.; Gabriele, G.; Chisci, G.; Mitro, V.; De Caris, F.; Iannetti, G. Temporomandibular synovial chondromatosis with numerous nodules. J. Craniofac. Surg. 2014, 25, 1114–1115. [Google Scholar] [CrossRef]
- Yoshitake, H.; Kayamori, K.; Nakamura, R.; Wake, S.; Harada, K. Pseudotumor in the temporomandibular joint: A case report. Int. J. Surg. Case Rep. 2015, 15, 5–9. [Google Scholar] [CrossRef]
- de Melo Trize, D.; Calabria, M.P.; de Oliveira Braga Franzolin, S.; Cunha, C.O.; Marta, S.N. Is quality of life affected by temporomandibular disorders? Einstein 2018, 16, eAO4339. [Google Scholar] [CrossRef]
- Woodford, S.C.; Robinson, D.L.; Mehl, A.; Lee, P.; Ackland, D.C. Measurement of normal and pathological mandibular and temporomandibular joint kinematics: A systematic review. J. Biomech. 2020, 111, 109994. [Google Scholar] [CrossRef] [PubMed]
- Reisine, S.T.; Weber, J. The effects of temporomandibular joint disorders on patients’ quality of life. Community Dent. Health 1989, 6, 257–270. [Google Scholar] [PubMed]
- Mantout, B.; Giraudeau, A.; Perez, C.; Ré, J.-P.; Orthlieb, J.-D. Technical validation of a computerized condylographic system. Int. J. Stomatol. Occlusion Med. 2008, 1, 45–50. [Google Scholar] [CrossRef]
- Lee, W.-J.; Park, K.-H.; Kang, Y.-G.; Kim, S.-J. Automated Real-Time Evaluation of Condylar Movement in Relation to Three-Dimensional Craniofacial and Temporomandibular Morphometry in Patients with Facial Asymmetry. Sensors 2021, 21, 2591. [Google Scholar] [CrossRef]
- Oancea, L.; Stegaroiu, R.; Cristache, C.M. The influence of temporomandibular joint movement parameters on dental morphology. Ann. Anat. 2018, 218, 49–58. [Google Scholar] [CrossRef]
- Akashi, M.; Shibuya, Y.; Takahashi, S.; Hashikawa, K.; Hasegawa, T.; Kakei, Y.; Negi, N.; Sekitani, T.; Komori, T. Four-dimensional computed tomography evaluation of jaw movement following mandibular reconstruction: A pilot study. J. Cranio-Maxillofac. Surg. 2016, 44, 637–641. [Google Scholar] [CrossRef]
- Das, A.; Muddugangadhar, B.C.; Mawani, D.P.; Mukhopadhyay, A. Comparative evaluation of sagittal condylar guidance obtained from a clinical method and with cone beam computed tomography in dentate individuals. J. Prosthet. Dent. 2021, 125, 753–757. [Google Scholar] [CrossRef] [PubMed]
- Cimić, S.; Simunković, S.K.; Badel, T.; Dulcić, N.; Alajbeg, I.; Catić, A. Measurements of the sagittal condylar inclination: Intraindividual variations. Cranio 2014, 32, 104–109. [Google Scholar] [CrossRef]
- Hija, A.; Allon, D.M. Comparative Assessment of Perception about Angle Inclination of Mandibular and Maxillary Incisors on the Cephalometric Analysis between Skeletal Class 3 and Orthognathic Cases. Appl. Sci. 2022, 12, 6228. [Google Scholar] [CrossRef]
- Da Fontoura, C.S.G.; Miller, S.F.; Wehby, G.L.; Amendt, B.A.; Holton, N.E.; Southard, T.E.; Allareddy, V.; Moreno Uribe, L.M. Candidate gene analyses of skeletal variation in malocclusion. J. Dent. Res. 2015, 94, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Kotuła, J.; Kuc, A.E.; Lis, J.; Kawala, B.; Sarul, M. New Sagittal and Vertical Cephalometric Analysis Methods: A Systematic Review. Diagnostics 2022, 12, 1723. [Google Scholar] [CrossRef]
- Cimić, S.; Simunković, S.K.; Kocijan, S.S.; Matijević, J.; Dulcić, N.; Catić, A. Articulator-related registration and analysis of sagittal condylar inclination. Acta Clin. Croat. 2015, 54, 432–437. [Google Scholar]
- Schierz, O.; Wagner, P.; Rauch, A.; Reissmann, D.R. Impact of mounting methods in computerized axiography on assessment of condylar inclination. Cranio 2019, 37, 60–67. [Google Scholar] [CrossRef]
- Ferro, K.J.; Morgano, S.M.; Driscoll, C.F.; Freilich, M.A.; Guckes, A.D.; Knoernschild, K.L.; McGarry, T.J. The Glossary of Prosthodontic Terms, Ninth Edition. J. Prosthet. Dent. 2017, 117, e1–e105. [Google Scholar] [CrossRef]
- Wieckiewicz, M.; Zietek, M.; Nowakowska, D.; Wieckiewicz, W. Comparison of selected kinematic facebows applied to mandibular tracing. Biomed Res. Int. 2014, 2014, 818694. [Google Scholar] [CrossRef] [PubMed]
- Hong, S.-J.; Noh, K. Setting the sagittal condylar inclination on a virtual articulator by using a facial and intraoral scan of the protrusive interocclusal position: A dental technique. J. Prosthet. Dent. 2021, 125, 392–395. [Google Scholar] [CrossRef]
- Lepidi, L.; Galli, M.; Mastrangelo, F.; Venezia, P.; Joda, T.; Wang, H.-L.; Li, J. Virtual Articulators and Virtual Mounting Procedures: Where Do We Stand? J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2021, 30, 24–35. [Google Scholar] [CrossRef]
- Corbett, N.E.; DeVincenzo, J.P.; Huffer, R.A.; Shryock, E.F. The relation of the condylar path to the articular eminence in mandibular protrusion. Angle Orthod. 1971, 41, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Parkash, H.; Bhargava, A.; Gupta, S.; Bagga, D.K. Reliability of Anatomic Reference Planes in Establishing the Occlusal Plane in Different Jaw Relationships: A Cephalometric Study. J. Indian Prosthodont. Soc. 2013, 13, 571–577. [Google Scholar] [CrossRef]
- Caro, A.J.; Peraire, M.; Martinez-Gomis, J.; Anglada, J.M.; Samsó, J. Reproducibility of lateral excursive tooth contact in a semi-adjustable articulator depending on the type of lateral guidance. J. Oral Rehabil. 2005, 32, 174–179. [Google Scholar] [CrossRef] [PubMed]
- Ahlers, M.O. Simulation of Occlusion in Restorative Dentistry: The Artex System; Denta Concept: Hamburg, Germany, 2000; 256p. [Google Scholar]
- Curtis, D.A. A comparison of protrusive interocclusal records to pantographic tracings. J. Prosthet. Dent. 1989, 62, 154–156. [Google Scholar] [CrossRef]
- Shreshta, P.; Jain, V.; Bhalla, A.; Pruthi, G. A comparative study to measure the condylar guidance by the radiographic and clinical methods. J. Adv. Prosthodont. 2012, 4, 153–157. [Google Scholar] [CrossRef]
- Zamacona, J.M.; Otaduy, E.; Aranda, E. Study of the sagittal condylar path in edentulous patients. J. Prosthet. Dent. 1992, 68, 314–317. [Google Scholar] [CrossRef]
- El-Gheriani, A.S.; Winstanley, R.B. Graphic tracings of condylar paths and measurements of condylar angles. J. Prosthet. Dent. 1989, 61, 77–87. [Google Scholar] [CrossRef] [PubMed]
- Lewandowska, A.; Mańka-Malara, K.; Kostrzewa-Janicka, J. Sagittal Condylar Inclination and Transversal Condylar Inclination in Different Skeletal Classes. J. Clin. Med. 2022, 11, 2664. [Google Scholar] [CrossRef] [PubMed]
- Zimmer, B.; Jäger, A.; Kubein-Meesenburg, D. Comparison of ‘normal’ TMJ-function in Class I, II, and III individuals. Eur. J. Orthod. 1991, 13, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Canning, T.; O’Connell, B.C.; Houston, F.; O’Sullivan, M. The effect of skeletal pattern on determining articulator settings for prosthodontic rehabilitation: An in vivo study. Int. J. Prosthodont. 2011, 24, 16–25. [Google Scholar]


| Gender | Mean (SD) | Mean Difference | 95% Confidence Interval of the Difference | t Value (df) | p Value | |
|---|---|---|---|---|---|---|
| SCI right (SCI_R) | Male (n = 40) | 37.68 (±12.23) | 4.20 | −0.37 to 8.76 | 1.82 (138) | 0.07 |
| Female (n = 100) | 33.48 (±12.37) | |||||
| SCI left (SCI_L) | Male (n = 40) | 36.89 (±12.67) | 2.73 | −2.16 to 7.62 | 1.10 (138) | 0.27 |
| Female (n = 100) | 34.16 (±13.43) | |||||
| [SCI_R–SCI_L] | Male (n = 40) | 4.92 (±4.44) | −0.59 | −2.37 to 1.18 | 0.66 (138) | 0.51 |
| Female (n = 100) | 5.50 (±4.93) |
| Skeletal Class | Mean (SD) | p Value | |
|---|---|---|---|
| SCI right (SCI_R) | Class I (n = 39) | 35.10 (±10.03) | 0.207 |
| Class II (n = 92) | 34.79 (±13.29) | ||
| Class III (n = 9) | 27.84 (±11.74) | ||
| SCI left (SCI_L) | Class I (n = 39) | 35.87 (±11.10) | 0.02 * |
| Class II (n = 92) | 35.75 (±13.92) | ||
| Class III (n = 9) | 22.69 (±8.58) | ||
| [SCI_R–SCI_L] | Class I (n = 39) | 4.91 (±4.18) | 0.75 |
| Class II (n = 92) | 5.44 (±4.95) | ||
| Class III (n = 9) | 6.13 (±5.90) |
| Dental Status | Mean (SD) | Mean Difference | 95% Confidence Interval of the Difference | t Value (df) | p Value | |
|---|---|---|---|---|---|---|
| SCI Right (SCI_R) | Fully dentate (n = 105) | 33.19 (±12.43) | −5.96 | −10.67 to −1.25 | −2.50 (138) | 0.01 * |
| Partially edentulous (n = 35) | 39.15 (±11.51) | |||||
| SCI left (SCI_L) | Fully dentate (n = 105) | 33.74 (±13.56) | −4.80 | −9.86 to −0.26 | −1.88 (138) | 0.06 |
| Partially edentulous (n = 35) | 38.54 (±11.65) | |||||
| [SCI_R–SCI_L] | Fully dentate (n = 105) | 5.70 (±4.88) | 1.44 | −0.40 to 3.27 | 1.55 (138) | 0.13 |
| Partially edentulous (n = 35) | 4.26 (±4.39) |
| TMJ Disorder (Yes/No) | Mean (SD) | Mean Difference | 95% Confidence Interval of the Difference | t Value (df) | p Value | |
|---|---|---|---|---|---|---|
| SCI Right (SCI_R) | No (n = 92) | 33.40 (±12.49) | −3.72 | −8.07 to 0.63 | −1.69 (138) | 0.09 |
| Yes (n = 48) | 37.12 (±12.09) | |||||
| SCI left (SCI_L) | No (n = 92) | 33.80 (±13.91) | −3.32 | −7.96 to 1.33 | −1.41 (138) | 0.16 |
| Yes (n = 48) | 37.12 (±11.65) | |||||
| [SCI_R–SCI_L] | No (n = 92) | 5.39 (±5.15) | 0.15 | −1.54 to1.84 | 0.17 (138) | 0.86 |
| Yes (n = 48) | 5.24 (±4.05) |
| Parafunctional Habits (Yes/No) | Mean (SD) | Mean Difference | 95% Confidence Interval of the Difference | t Value (df) | p Value | |
|---|---|---|---|---|---|---|
| SCI Right (SCI_R) | No (n = 106) | 34.36 (±12.14) | −1.33 | −8.18 to 3.53 | −0.54 (138) | 0.59 |
| Yes (n = 34) | 35.68 (±13.44) | |||||
| SCI left (SCI_L) | No (n = 106) | 34.85 (±13.24) | −0.37 | −5.54 to 4.80 | −0.14 (138) | 0.89 |
| Yes (n = 34) | 35.22 (±13.39) | |||||
| [SCI_R–SCI_L] | No (n = 106) | 5.50 (±5.12) | −0.66 | −1.21 to 2.53 | 0.70 (138) | 0.49 |
| Yes (n = 34) | 4.84 (±3.57) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dragus, A.C.; Mihai, A.; Tanase, G.; Burlibasa, M.; Cristache, C.M. Intraindividual Left–Right Side Differences of Sagittal Condylar Inclination (SCI) in Different Skeletal Classes. Healthcare 2023, 11, 1341. https://doi.org/10.3390/healthcare11091341
Dragus AC, Mihai A, Tanase G, Burlibasa M, Cristache CM. Intraindividual Left–Right Side Differences of Sagittal Condylar Inclination (SCI) in Different Skeletal Classes. Healthcare. 2023; 11(9):1341. https://doi.org/10.3390/healthcare11091341
Chicago/Turabian StyleDragus, Andi Ciprian, Augustin Mihai, Gabriela Tanase, Mihai Burlibasa, and Corina Marilena Cristache. 2023. "Intraindividual Left–Right Side Differences of Sagittal Condylar Inclination (SCI) in Different Skeletal Classes" Healthcare 11, no. 9: 1341. https://doi.org/10.3390/healthcare11091341
APA StyleDragus, A. C., Mihai, A., Tanase, G., Burlibasa, M., & Cristache, C. M. (2023). Intraindividual Left–Right Side Differences of Sagittal Condylar Inclination (SCI) in Different Skeletal Classes. Healthcare, 11(9), 1341. https://doi.org/10.3390/healthcare11091341








