Effects of Resilience Training on Resilient Functioning in Chronic Stress Situations among Cadets of the Swiss Armed Forces
Abstract
1. Introduction
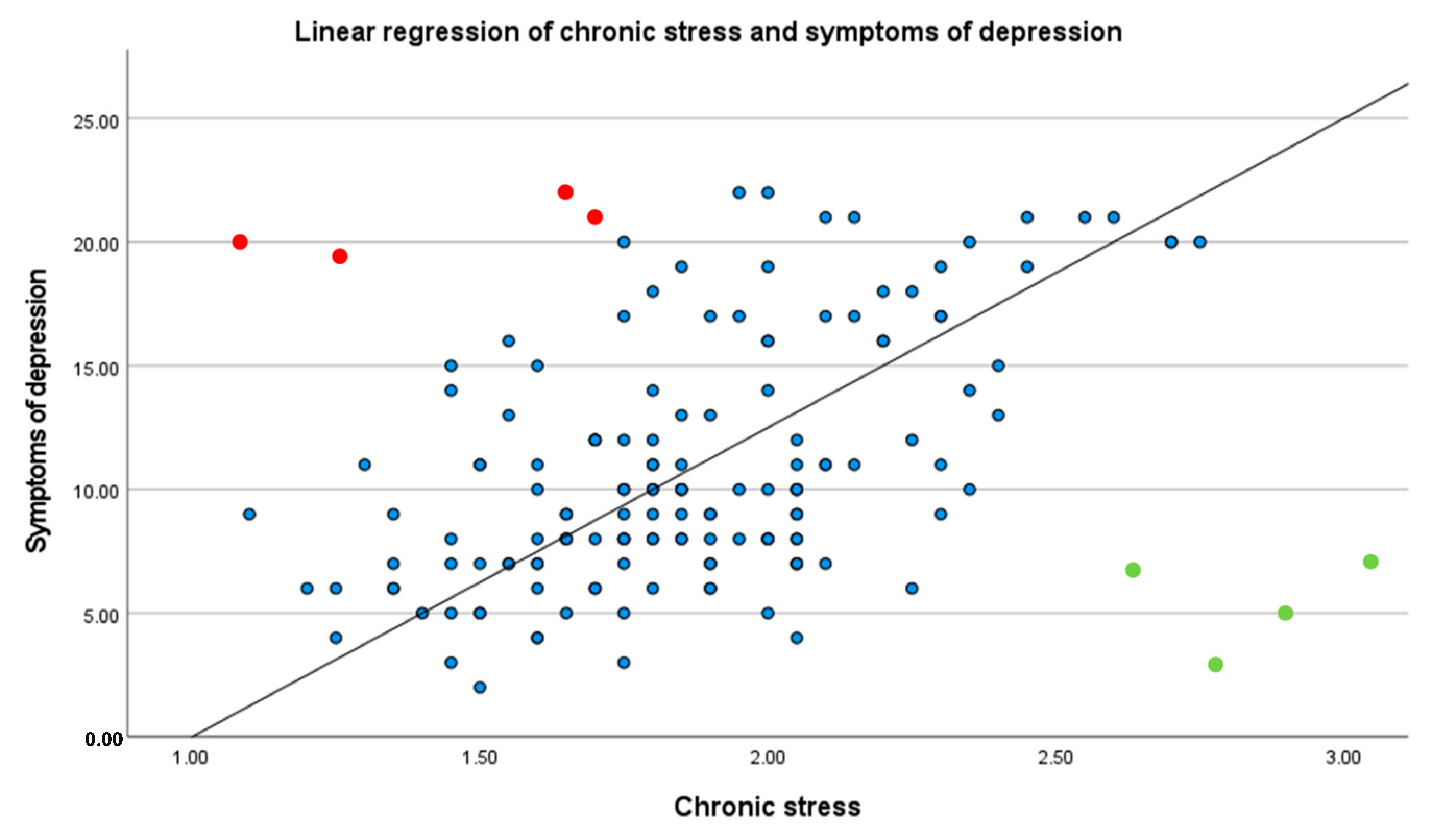
- Whether RFS was related to well-established resilience factors, such as coping, self-efficacy, and stress reactivity;
- Whether RFS was related to well-being in chronic stress situations; and
- Whether resilient functioning could be improved through participation in resilience training.
2. Methods
2.1. Participants and Study Design
2.2. Resilience Training Intervention
- Week Two: Participants learned to identify their values and core beliefs [9].
2.3. Measurement Scales
2.3.1. Chronic Stress
2.3.2. Vital Exhaustion
2.3.3. Symptoms of Depression
2.3.4. Irritation
2.3.5. Coping Strategies
2.3.6. Self-Efficacy
2.3.7. Stress Reactivity
2.3.8. Psychological Well-Being
2.4. Analytical Plan
3. Results
3.1. Characteristics of Participants
3.2. Correlations of Resilient Functioning with Coping, Self-Efficacy, Stress Reactivity, and Well-Being
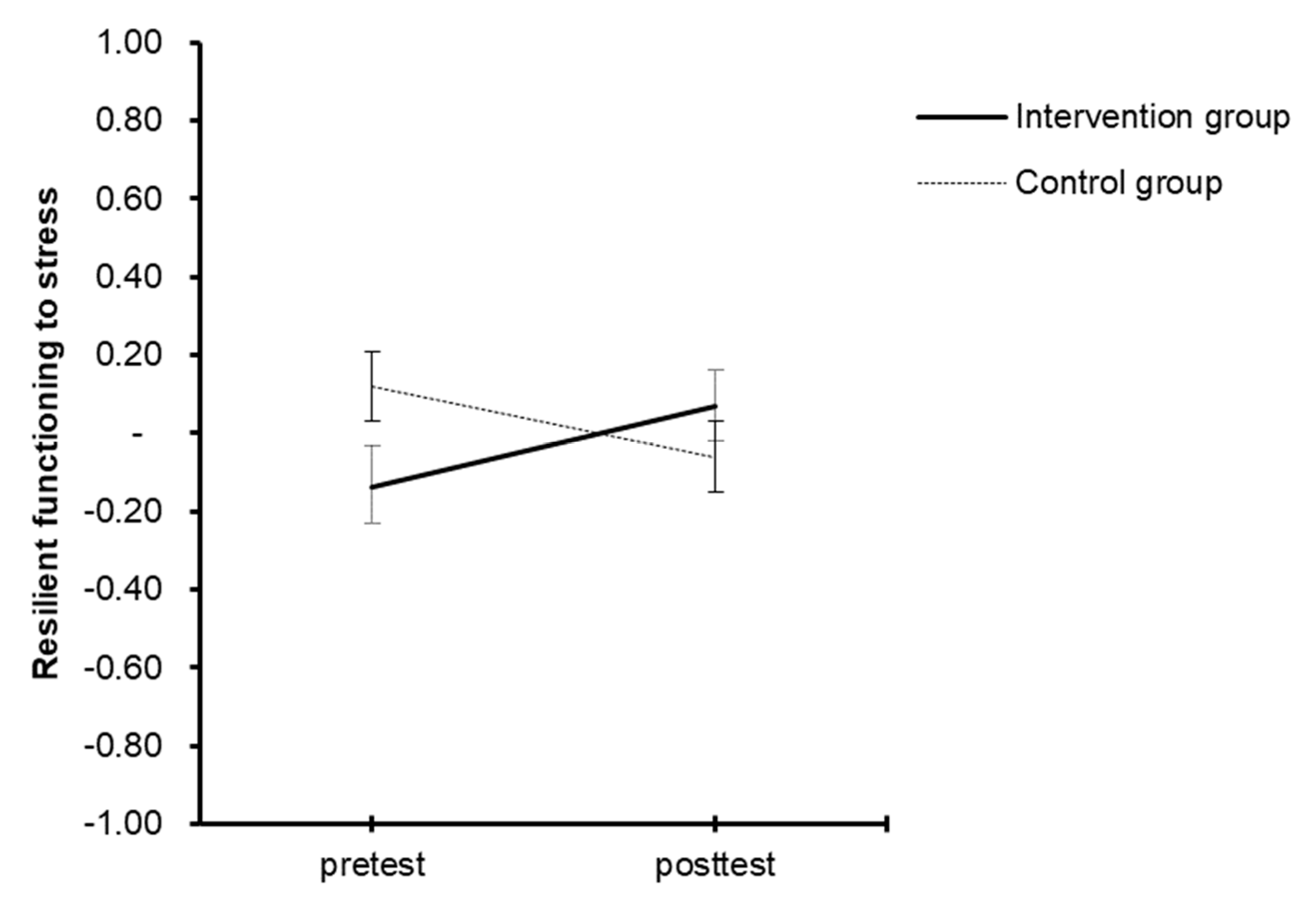
3.3. Improvement of Resilient Functioning from Pre- to Post-Test between and within the Intervention and Control Conditions
3.4. Reliable Change Index of Resilient Functioning
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bonanno, G.A. Loss, trauma, and human resilience: Have we underestimated the human capacity to thrive after extremely aversive events? Am. Psychol. 2004, 59, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Kalisch, R.; Baker, D.G.; Basten, U.; Boks, M.P.; Bonanno, G.A.; Brummelman, E.; Chmitorz, A.; Fernàndez, G.; Fiebach, C.J.; Galatzer-Levy, I.; et al. The resilience framework as a strategy to combat stress-related disorders. Nat. Hum. Behav. 2017, 1, 784–790. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.E.C.; Sudom, K.A.; McCreary, D.R. Higher-order model of resilience in the Canadian forces. Can. J. Behav. Sci. Rev. Can. Des Sci. Du Comport. 2011, 43, 222–234. [Google Scholar] [CrossRef]
- Afifi, T.; MacMillan, H.L. Resilience following Child Maltreatment: A Review of Protective Factors. Can. J. Psychiatry 2011, 56, 266–272. [Google Scholar] [CrossRef] [PubMed]
- Dias, P.C.; Cadime, I. Protective factors and resilience in adolescents: The mediating role of self-regulation. Psicol. Educ. 2017, 23, 37–43. [Google Scholar] [CrossRef]
- Lee, J.-S.; Joo, E.-J.; Choi, K.-S. Perceived stress and self-esteem mediate the effects of work-related stress on depression. Stress Health 2013, 29, 75–81. [Google Scholar] [CrossRef]
- Schueler, K.; Fritz, J.; Dorfschmidt, L.; van Harmelen, A.-L.; Stroemer, E.; Wessa, M. Psychological Network Analysis of General Self-Efficacy in High vs. Low Resilient Functioning Healthy Adults. Front. Psychiatry 2021, 12, 736147. [Google Scholar] [CrossRef]
- Vanhove, A.J.; Herian, M.N.; Perez, A.L.U.; Harms, P.D.; Lester, P.B. Can resilience be developed at work? A meta-analytic review of resilience-building programme effectiveness. J. Occup. Organ. Psychol. 2016, 89, 278–307. [Google Scholar] [CrossRef]
- Reivich, K.J.; Shatté, A. The Resilience Factor: 7 Keys to Finding Your Inner Strength and Overcoming Life’s Hurdles; Three Rivers Press: New York, NY, USA, 2002. [Google Scholar]
- Chmitorz, A.; Kunzler, A.; Helmreich, I.; Tüscher, O.; Kalisch, R.; Kubiak, T.; Wessa, M.; Lieb, K. Intervention studies to foster resilience—A systematic review and proposal for a resilience framework in future intervention studies. Clin. Psychol. Rev. 2018, 59, 78–100. [Google Scholar] [CrossRef]
- Fischer, S.; Lemmer, G.; Gollwitzer, M.; Nater, U.M. Stress and resilience in functional somatic syndromes—A structural equation modeling approach. PLoS ONE 2014, 9, e111214. [Google Scholar] [CrossRef]
- Meredith, L.S.; Sherbourn, C.D.; Gaillot, S.J.; Hansell, L.; Ritschard, H.V.; Parker, A.M.; Wrenn, G. Promoting Psychological Resilience in the U.S. Military. Rand Health Q. 2011, 1. [Google Scholar]
- Ursu, A.; Măirean, C. Cognitive Emotion Regulation Strategies as Mediators between Resilience and Stress during COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 12631. [Google Scholar] [CrossRef]
- Williams, A.; Hagerty, B.M.; Andrei, A.-C.; Yousha, S.M.; Hirth, R.A.; Hoyle, K.S. STARS: Strategies to assist navy recruits’ success. Mil. Med. 2007, 172, 942–949. [Google Scholar] [CrossRef]
- Williams, A.; Hagerty, B.M.; Yousha, S.M.; Horrocks, J.; Hoyle, K.S.; Liu, D. Psychosocial effects of the Boot Strap intervention in Navy recruits. Mil. Med. 2004, 169, 814–820. [Google Scholar] [CrossRef] [PubMed]
- Harms, P.D.; Krasikova, D.V.; Vanhove, A.J.; Herian, M.N.; Lester, P.B. Stress and Emotional Well-being in Military Organizations. Res. Occup. Stress Well Being 2013, 11, 103–132. [Google Scholar] [CrossRef]
- Burton, N.W.; Pakenham, K.I.; Brown, W.J. Feasibility and effectiveness of psychosocial resilience training: A pilot study of the READY program. Psychol. Health Med. 2010, 15, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Cohn, A.; Pakenham, K. Efficacy of a cognitive-behavioral program to improve psychological adjustment among soldiers in recruit training. Mil. Med. 2008, 173, 1151–1157. [Google Scholar] [CrossRef] [PubMed]
- Abbott, J.-A.; Klein, B.; Hamilton, C.; Rosenthal, A. The impact of online resilience training for sales managers on wellbeing and performance. Electron. J. Appl. Psychol. 2009, 5, 89–95. [Google Scholar] [CrossRef]
- Crane, M.F.; Boga, D.; Karin, E.; Gucciardi, D.F.; Rapport, F.; Callen, J.; Sinclair, L. Strengthening resilience in military officer cadets: A group-randomized controlled trial of coping and emotion regulatory self-reflection training. J. Consult. Clin. Psychol. 2019, 87, 125–140. [Google Scholar] [CrossRef]
- Grime, P.R. Computerized cognitive behavioural therapy at work: A randomized controlled trial in employees with recent stress-related absenteeism. Occup. Med. 2004, 54, 353–359. [Google Scholar] [CrossRef]
- Adler, A.B.; Williams, J.; McGurk, D.; Moss, A.; Bliese, P.D. Resilience training with soldiers during basic combat training: Randomisation by platoon. Appl. Psychol. Health Well Being 2015, 7, 85–107. [Google Scholar] [CrossRef]
- Adler, A.B.; Bliese, P.D.; McGurk, D.; Hoge, C.W.; Castro, C.A. Battlemind debriefing and battlemind training as early interventions with soldiers returning from iraq: Randomization by platoon. J. Consult. Clin. Psychol. 2009, 77, 928–940. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.E.; Perkins, K.; Cook, J.H.; Ong, A.L. Intensive coping skills training to reduce anxiety and depression for forward-deployed troops. Mil. Med. 2008, 173, 241–246. [Google Scholar] [CrossRef][Green Version]
- Maddi, S.R.; Kahn, S.; Maddi, K.L. The effectiveness of hardiness training. Consult. Psychol. J. Pract. Res. 1998, 50, 78–86. [Google Scholar] [CrossRef]
- Sood, A.; Prasad, K.; Schroeder, D.; Varkey, P. Stress management and resilience training among Department of Medicine faculty: A pilot randomized clinical trial. J. Gen. Intern. Med. 2011, 26, 858–861. [Google Scholar] [CrossRef] [PubMed]
- Kalisch, R.; Köber, G.; Binder, H.; Ahrens, K.F.; Basten, U.; Chmitorz, A.; Choi, K.W.; Fiebach, C.J.; Goldbach, N.; Neumann, R.J.; et al. The Frequent Stressor and Mental Health Monitoring-Paradigm: A Proposal for the Operationalization and Measurement of Resilience and the Identification of Resilience Processes in Longitudinal Observational Studies. Front. Psychol. 2021, 12, 710493. [Google Scholar] [CrossRef]
- Mancini, A.D.; Bonanno, G.A. Predictors and parameters of resilience to loss: Toward an individual differences model. J. Pers. 2009, 77, 1805–1832. [Google Scholar] [CrossRef]
- Arnetz, B.B.; Nevedal, D.C.; Lumley, M.A.; Backman, L.; Lublin, A. Trauma Resilience Training for Police: Psychophysiological and Performance Effects. J. Police Crim. Psychol. 2009, 24, 1–9. [Google Scholar] [CrossRef]
- Rose, R.D.; Buckey, J.C.; Zbozinek, T.D.; Motivala, S.J.; Glenn, D.E.; Cartreine, J.A.; Craske, M.G. A randomized controlled trial of a self-guided, multimedia, stress management and resilience training program. Behav. Res. Ther. 2013, 51, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Zueger, R.; Niederhauser, M.; Utzinger, C.; Annen, H.; Ehlert, U. Effects of resilience training on mental, emotional, and physical stress outcomes in military officer cadets. Mil. Psychol. 2022, 1–11. [Google Scholar] [CrossRef]
- Lazarus, R.S.; Folkman, S. Stress, Appraisal, and Coping; Springer: New York, NY, USA, 1984. [Google Scholar]
- Carr, W.; Bradley, D.; Ogle, A.D.; Eonta, S.E.; Pyle, B.L.; Santiago, P. Resilience Training in a Population of Deployed Personnel. Mil. Psychol. 2013, 25, 148–155. [Google Scholar] [CrossRef]
- Nakkas, C.; Annen, H.; Brand, S. Psychological distress and coping in military cadre candidates. Neuropsychiatr. Dis. Treat. 2016, 12, 2237–2243. [Google Scholar] [CrossRef]
- Sefidan, S.; Pramstaller, M.; La Marca, R.; Wyss, T.; Sadeghi-Bahmani, D.; Annen, H.; Brand, S. Resilience as a Protective Factor in Basic Military Training, a Longitudinal Study of the Swiss Armed Forces. Int. J. Environ. Res. Public Health 2021, 18, 6077. [Google Scholar] [CrossRef] [PubMed]
- Elliman, T.D.; Schwalb, M.E.; Adler, A.B. Sleep deprivation and hazardous unintended sleep in US army drill sergeants. Sleep Health 2020, 6, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Adler, A.B.; Castro, C.A. An Occupational Mental Health Model for the Military. Mil. Behav. Health 2013, 1, 41–45. [Google Scholar] [CrossRef]
- McGurk, D.; Cotting, D.I.; Britt, T.W.; Adler, A.B. Joining the ranks: The role of indoctrination in transforming civilians to service members. In Military life: The Psychology of Serving in Peace and Combat: Operational Stress; Adler, A.B., Castro, C.A., Britt, T.W., Eds.; Praeger Security International: Westport, CT, USA, 2006; pp. 13–31. [Google Scholar]
- Lieberman, H.R.; Bathalon, G.P.; Falco, C.M.; Kramer, F.M.; Morgan, C.A.; Niro, P. Severe decrements in cognition function and mood induced by sleep loss, heat, dehydration, and undernutrition during simulated combat. Biol. Psychiatry 2005, 57, 422–429. [Google Scholar] [CrossRef] [PubMed]
- Schumacher, J.; Leppert, K.; Gunzelmann, T.; Strauss, B.; Brähler, E. Die Resilienzskala—Ein Fragebogen zur Erfassung der psychischen Widerstandsfähigkeit als Personmerkmal. Ztg. Klin. Psychol. Psychiatr. Psychother. 2005, 53, 16–39. [Google Scholar]
- Connor, K.M.; Davidson, J.R.T. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress. Anxiety 2003, 18, 76–82. [Google Scholar] [CrossRef]
- Chmitorz, A.; Wenzel, M.; Stieglitz, R.-D.; Kunzler, A.; Bagusat, C.; Helmreich, I.; Gerlicher, A.; Kampa, M.; Kubiak, T.; Kalisch, R.; et al. Population-based validation of a German version of the Brief Resilience Scale. PLoS ONE 2018, 13, e0192761. [Google Scholar] [CrossRef] [PubMed]
- Alschuler, K.N.; Arewasikporn, A.; Nelson, I.K.; Molton, I.R.; Ehde, D.M. Promoting resilience in individuals aging with multiple sclerosis: Results from a pilot randomized controlled trial. Rehabil. Psychol. 2018, 63, 338–348. [Google Scholar] [CrossRef]
- Hendriks, T.; Schotanus-Dijkstra, M.; Hassankhan, A.; Sardjo, W.; Graafsma, T.; Bohlmeijer, E.; de Jong, J. Resilience and well-being in the Caribbean: Findings from a randomized controlled trial of a culturally adapted multi-component positive psychology intervention. J. Posit. Psychol. 2020, 15, 238–253. [Google Scholar] [CrossRef]
- Heydarpour, S.; Parvane, E.; Saqqezi, A.; Ziapour, A.; Dehghan, F.; Parvaneh, A. Effectiveness of group counseling based on the reality therapy on resilience and psychological well-being of mothers with an intellectual disabled child. Int. J. Pediatr. 2018, 6, 7851–7860. [Google Scholar]
- Van Harmelen, A.-L.; Kievit, R.A.; Ioannidis, K.; Neufeld, S.; Jones, P.B.; Bullmore, E.; Dolan, R.; Fonagy, P.; Goodyer, I. Adolescent friendships predict later resilient functioning across psychosocial domains in a healthy community cohort. Psychol. Med. 2017, 13, 2312–2322. [Google Scholar] [CrossRef] [PubMed]
- Scripts to Calculate Stress Resilience Scores as Regression Residuals. Available online: https://osf.io/s7u23/ (accessed on 4 February 2023).
- Szeto, A.C.H.; Dobson, K.S. Mental disorders and their association with perceived work stress: An investigation of the 2010 Canadian Community Health Survey. J. Occup. Health Psychol. 2013, 18, 191–197. [Google Scholar] [CrossRef]
- Leak, R.K.; Calabrese, E.J.; Kozumbo, W.J.; Gidday, J.M.; Johnson, T.E.; Mitchell, J.R.; Ozaki, C.K.; Wetzker, R.; Bast, A.; Belz, R.G.; et al. Enhancing and Extending Biological Performance and Resilience. Dose Response 2018, 16, 1559325818784501. [Google Scholar] [CrossRef] [PubMed]
- Mjelde, F.V.; Smith, K.; Lunde, P.; Espevik, R. Military teams-A demand for resilience. Work 2016, 54, 283–294. [Google Scholar] [CrossRef] [PubMed]
- Bonanno, G.A.; Westphal, M.; Mancini, A.D. Resilience to loss and potential trauma. Annu. Rev. Clin. Psychol. 2011, 7, 511–535. [Google Scholar] [CrossRef]
- Kalisch, R.; Cramer, A.O.J.; Binder, H.; Fritz, J.; Leertouwer, I.; Lunansky, G.; Meyer, B.; Timmer, J.; Veer, I.M.; van Harmelen, A.-L. Deconstructing and Reconstructing Resilience: A Dynamic Network Approach. Perspect. Psychol. Sci. 2019, 14, 765–777. [Google Scholar] [CrossRef]
- Van Harmelen, A.-L.; Blakemore, S.J.; Goodyer, I.M.; Kievit, R.A. The Interplay Between Adolescent Friendship Quality and Resilient Functioning Following Childhood and Adolescent Adversity. Adv. Res. Sci. 2021, 2, 37–50. [Google Scholar] [CrossRef]
- Meine, L.E.; Strömer, E.; Schönfelder, S.; Eckhardt, E.I.; Bergmann, A.K.; Wessa, M. Look After Yourself: Students Consistently Showing High Resilience Engaged in More Self-Care and Proved More Resilient During the COVID-19 Pandemic. Front. Psychiatry 2021, 12, 784381. [Google Scholar] [CrossRef]
- Ioannidis, K.; Askelund, A.D.; Kievit, R.A.; van Harmelen, A.-L. The complex neurobiology of resilient functioning after childhood maltreatment. BMC Med. 2020, 18, 32. [Google Scholar] [CrossRef]
- Kalisch, R.; Müller, M.B.; Tüscher, O. A conceptual framework for the neurobiological study of resilience. Behav. Brain Sci. 2015, 38, e92. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Wang, Z.; Lü, W. Resilience and affect balance as mediators between trait emotional intelligence and life satisfaction. Personal. Individ. Differ. 2013, 54, 850–855. [Google Scholar] [CrossRef]
- Doyle, N.; MacLachlan, M.; Fraser, A.; Stilz, R.; Lismont, K.; Cox, H.; McVeigh, J. Resilience and well-being amongst seafarers: Cross-sectional study of crew across 51 ships. Int. Arch. Occup. Environ. Health 2016, 89, 199–209. [Google Scholar] [CrossRef]
- Cacioppo, J.T.; Adler, A.B.; Lester, P.B.; McGurk, D.; Thomas, J.L.; Chen, H.-Y.; Cacioppo, S. Building social resilience in soldiers: A double dissociative randomized controlled study. J. Pers. Soc. Psychol. 2015, 109, 90–105. [Google Scholar] [CrossRef]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef]
- Niederhauser, M.; Zueger, R.; Sefidan, S.; Annen, H.; Brand, S.; Sadeghi-Bahmani, D. Does Training Motivation Influence Resilience Training Outcome on Chronic Stress? Results from an Interventional Study. Int. J. Environ. Res. Public Health 2022, 19, 6179. [Google Scholar] [CrossRef] [PubMed]
- Reivich, K.J.; Seligman, M.E.P.; McBride, S. Master resilience training in the U.S. Army. Am. Psychol. 2011, 66, 25–34. [Google Scholar] [CrossRef]
- Hanin, Y.L. Emotions and athletic performance: Individual zones of optimal functioning model. Eur. Yearb. Sport Psychol. 1997, 1, 29–72. [Google Scholar]
- Seiler, R.; Stock, A. Handbuch psychotraining im sport: Methoden im überblick. In Handbook of Psychotraining in Sport: Methods at a Glance; Rowohlt: Hamburg, Germany, 1994. [Google Scholar]
- Yerkes, R.M.; Dodson, J.D. The relation of strength of stimulus to rapidity of habit-formation. J. Comp. Neurol. Psychol. 1908, 18, 459–482. [Google Scholar] [CrossRef]
- Gable, S.L.; Reis, H.T.; Impett, E.A.; Asher, E.R. What do you do when things go right? The intrapersonal and interpersonal benefits of sharing positive events. J. Pers. Soc. Psychol. 2004, 87, 228–245. [Google Scholar] [CrossRef] [PubMed]
- Kamins, M.L.; Dweck, C.S. Person versus process praise and criticism: Implications for contingent self-worth and coping. Dev. Psychol. 1999, 35, 835–847. [Google Scholar] [CrossRef]
- Peterson, C.; Seligman, M.E.P. Character Strengths and Virtues: A handbook and Classification; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Vopel, K.W. Interaktionsspiele I—Lebendiges Lernen und Lehren. In Interaction Games I—Living Learning and Teaching; Iskopress Verlags GmbH: Salzhausen, Germany, 2004. [Google Scholar]
- Fliege, H.; Rose, M.; Arck, P.; Levenstein, S.; Klapp, B.F. Validierung des “Perceived Stress Questionnaire” (PSQ) an einer deutschen Stichprobe. Diagnostica 2001, 47, 142–152. [Google Scholar] [CrossRef]
- Von Känel, R.; Bellingrath, S.; Kudielka, B.M. Association of vital exhaustion and depressive symptoms with changes in fibrin D-dimer to acute psychosocial stress. J. Psychosom. Res. 2009, 67, 93–101. [Google Scholar] [CrossRef]
- Hautzinger, M.; Bailer, M. Allgemeine Depressionsskala [General Depression Scale]; Beltz: Weinheim, Germany, 1993. [Google Scholar]
- Mohr, G.; Rigotti, T.; Müller, A. Irritation—ein Instrument zur Erfassung psychischer Beanspruchung im Arbeitskontext. Skalen- und Itemparameter aus 15 Studien. Z. Arb. Organ. AO 2005, 49, 44–48. [Google Scholar] [CrossRef]
- Kälin, W. Deutsche 24-Item Kurzform des “Coping Inventory for Stressful Situations” (CISS) von N.S.Endler & J.D.A. Parker; Universität, Institut für Psychologie: Bern, Switzerland, 1995. [Google Scholar]
- Krampen, G. Fragebogen zu Kompetenz- und Kontrollüberzeugungen (FKK); Hogrefe: Göttingen, Germany, 1991. [Google Scholar]
- Schulz, P.; Jansen, L.J.; Schlotz, W. Stressreaktivität: Theoretisches Konzept und Messung. Diagnostica 2005, 51, 124–133. [Google Scholar] [CrossRef]
- Brähler, E.; Mühlan, H.; Albani, C.; Schmidt, S. Teststatistische Prüfung und Normierung der deutschen Versionen des EUROHIS-QOL Lebensqualität-Index und des WHO-5 Wohlbefindens-Index. Diagnostica 2007, 53, 83–96. [Google Scholar] [CrossRef]
- Abdi, H. Partial least squares regression and projection on latent structure regression (PLS Regression). WIREs Comp. Stat. 2010, 2, 97–106. [Google Scholar] [CrossRef]
- Jacobson, N.S.; Truax, P. Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. J. Consult. Clin. Psychol. 1991, 59, 12–19. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1988. [Google Scholar]
- Cohen, J. A power primer. Psychol. Bull 1992, 112, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. (Ed.) Self-Efficacy; Acacemic Press: New York, NY, USA, 1994. [Google Scholar]
- Haidt, J.; Rodin, J. Control and Efficacy as Interdisciplinary Bridges. Rev. Gen. Psychol. 1999, 3, 317–337. [Google Scholar] [CrossRef]
- Cherniss, C. Role of Professional self-efficacy in the Etiology and Amelioration of Burnout. In Professional Burnout: Recent Developments in Theory and Research; Schaufeli, W., Maslach, C., Marek, T., Eds.; Taylor Francis: Washington, DC, USA, 1993; pp. 135–149. ISBN 9781315227979. [Google Scholar]
- Korman, J.V.; van Quaquebeke, N.; Tröster, C. Managers are Less Burned-Out at the Top: The Roles of Sense of Power and Self-Efficacy at Different Hierarchy Levels. J. Bus Psychol. 2022, 37, 151–171. [Google Scholar] [CrossRef]
- Jones, N.; Whelan, C.; Harden, L.; Macfarlane, A.; Burdett, H.; Greenberg, N. Resilience-based intervention for UK military recruits: A randomised controlled trial. Occup. Environ. Med. 2019, 76, 90–96. [Google Scholar] [CrossRef] [PubMed]
- Christopher, M.S.; Hunsinger, M.; Goerling, L.R.J.; Bowen, S.; Rogers, B.S.; Gross, C.R.; Dapolonia, E.; Pruessner, J.C. Mindfulness-based resilience training to reduce health risk, stress reactivity, and aggression among law enforcement officers: A feasibility and preliminary efficacy trial. Psychiatry Res. 2018, 264, 104–115. [Google Scholar] [CrossRef] [PubMed]
- Ledford, A.K.; Dixon, D.; Luning, C.R.; Martin, B.J.; Miles, P.C.; Beckner, M.; Bennett, D.; Conley, J.; Nindl, B.C. Psychological and Physiological Predictors of Resilience in Navy SEAL Training. Behav. Med. 2020, 46, 290–301. [Google Scholar] [CrossRef]
- Deeks, J.J.; Dinnes, J.; D’Amico, R.; Sowden, A.J.; Sakarovitch, C.; Song, F.; Petticrew, M.; Altman, D.G.; The International Stroke Trial Collaborative Group; the European Carotid Surgery Trial Collaborative Group. Evaluating non-randomised intervention studies. Health Technol. Assess. 2003, 7, 1–173. [Google Scholar] [CrossRef]
- Goldammer, P.; Annen, H.; Stöckli, P.L.; Jonas, K. Careless responding in questionnaire measures: Detection, impact, and remedies. Leadersh. Q. 2020, 31, 101384. [Google Scholar] [CrossRef]
- Krieger, N.; Smith, K.; Naishadham, D.; Hartman, C.; Barbeau, E.M. Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Soc. Sci. Med. 2005, 61, 1576–1596. [Google Scholar] [CrossRef] [PubMed]
| Groups | Statistics | ||
|---|---|---|---|
| Intervention | Control | ||
| M (SD) | M (SD) | ||
| N | 51 | 59 | |
| Age (in years) | 20.84 (1.42) | 21.02 (1.81) | t(107.09) = −0.57, p = 0.580; d = 0.11) |
| Education level | n (%) | n (%) | χ2 (N = 110; df = 1) = 0.762, p = 0.383 |
| Upper secondary school | 98.0% | 94.9% | |
| Tertiary level | 2.0% | 5.1% | |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M (SD) |
|---|---|---|---|---|---|---|---|---|
| 1. Resilient functioning | 0 (0.72) | |||||||
| 2. Task-oriented coping | 0.17 | 3.93 (0.51) | ||||||
| 3. Emotion-oriented coping | −0.38 *** | −0.46 *** | 2.32 (0.61) | |||||
| 4. Avoidance-oriented coping | 0.08 | −0.08 | 0.08 | 3.10 (0.75) | ||||
| 5. Self-efficacy | 0.18 | 0.53 *** | −0.60 *** | −0.01 | 72.60 (6.76) | |||
| 6. Stress reactivity | −0.30 ** | −0.43 *** | 0.65 *** | −0.06 | −0.52 *** | 45.63 (6.29) | ||
| 7. Well-being | 0.23 * | 0.15 | 0.32 *** | −0.04 | 0.32 *** | 0.29 ** | 17.00 (4.12) |
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | M (SD) |
|---|---|---|---|---|---|---|---|---|
| 1. Resilient functioning | 0 (0.68) | |||||||
| 2. Task-oriented coping | 0.19 * | 3.92 (0.57) | ||||||
| 3. Emotion-oriented coping | −0.20 * | −0.41 *** | 2.28 (0.63) | |||||
| 4. Avoidance-oriented coping | 0.02 | −0.12 | 0.10 | 2.88 (0.75) | ||||
| 5. Self-efficacy | 0.13 | 0.51 *** | −0.52 *** | −0.15 | 72.65 (7.61) | |||
| 6. Stress reactivity | −0.22 * | −0.39 *** | 0.61 *** | −0.06 | −0.49 *** | 44.61 (7.28) | ||
| 7. Well-being | 0.19 | 0.33 | 0.24 ** | −0.08 | 0.36 *** | 0.37 ** | 16.09 (4.06) |
| IG (n = 51) | CG (n = 59) | Fisher’s Exact Test, Cramer’s V | ||
|---|---|---|---|---|
| Resilient functioning | Increase | 8% | 0% | p = 0.043, V = 0.209 [S] |
| Decrease | 0% | 3% | p = 0.498, V = 0.127 [S] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Niederhauser, M.; Zueger, R.; Annen, H.; Gültekin, N.; Stanga, Z.; Brand, S.; Sadeghi-Bahmani, D. Effects of Resilience Training on Resilient Functioning in Chronic Stress Situations among Cadets of the Swiss Armed Forces. Healthcare 2023, 11, 1329. https://doi.org/10.3390/healthcare11091329
Niederhauser M, Zueger R, Annen H, Gültekin N, Stanga Z, Brand S, Sadeghi-Bahmani D. Effects of Resilience Training on Resilient Functioning in Chronic Stress Situations among Cadets of the Swiss Armed Forces. Healthcare. 2023; 11(9):1329. https://doi.org/10.3390/healthcare11091329
Chicago/Turabian StyleNiederhauser, Madlaina, Regula Zueger, Hubert Annen, Nejla Gültekin, Zeno Stanga, Serge Brand, and Dena Sadeghi-Bahmani. 2023. "Effects of Resilience Training on Resilient Functioning in Chronic Stress Situations among Cadets of the Swiss Armed Forces" Healthcare 11, no. 9: 1329. https://doi.org/10.3390/healthcare11091329
APA StyleNiederhauser, M., Zueger, R., Annen, H., Gültekin, N., Stanga, Z., Brand, S., & Sadeghi-Bahmani, D. (2023). Effects of Resilience Training on Resilient Functioning in Chronic Stress Situations among Cadets of the Swiss Armed Forces. Healthcare, 11(9), 1329. https://doi.org/10.3390/healthcare11091329







