Evaluating the Impact of COVID-19 on Hospital Profit Compensation Activities: A Difference-in-Differences Event Study Analysis in China
Abstract
1. Introduction
2. Background
2.1. Brief Introduction to China’s Healthcare Delivery System
2.2. Compensation Mechanism of Chinese Public Hospitals and Its Potential Influence by COVID-19
3. Methods
3.1. Data
3.2. Intervention Identification
3.3. Causal Inference Strategy
- denotes the logarithmic form of total expenses, out-of-pocket expenses, and claiming expenses from health insurance for each patient i admitted at week t.
- and are the lowest and highest numbers of week of leads and lags to consider for the period of week 4 to week 8 of the year (23 January to 19 February). The value of k is −1, −2, when the week of the year is 3, 2, 1. The value of k is 0, 1, , when the week of the year is 8, 9, , 48 (30 November).
- is a dummy variable equaling 1 if the observation is from 2020, otherwise it is 0.
- and are week and hospital fixed effects.
- represent a series of control variables that would have significant confounding effects on inpatient expense, including age, age square, sex, type of health insurance, admission situation, and first ICD-10 code for primary diagnosis.
- Estimation is generally performed with standard errors clustered at the hospital level.
- The −1 week lag is used as the dropped reference to avoid perfect multicollinearity.
4. Results
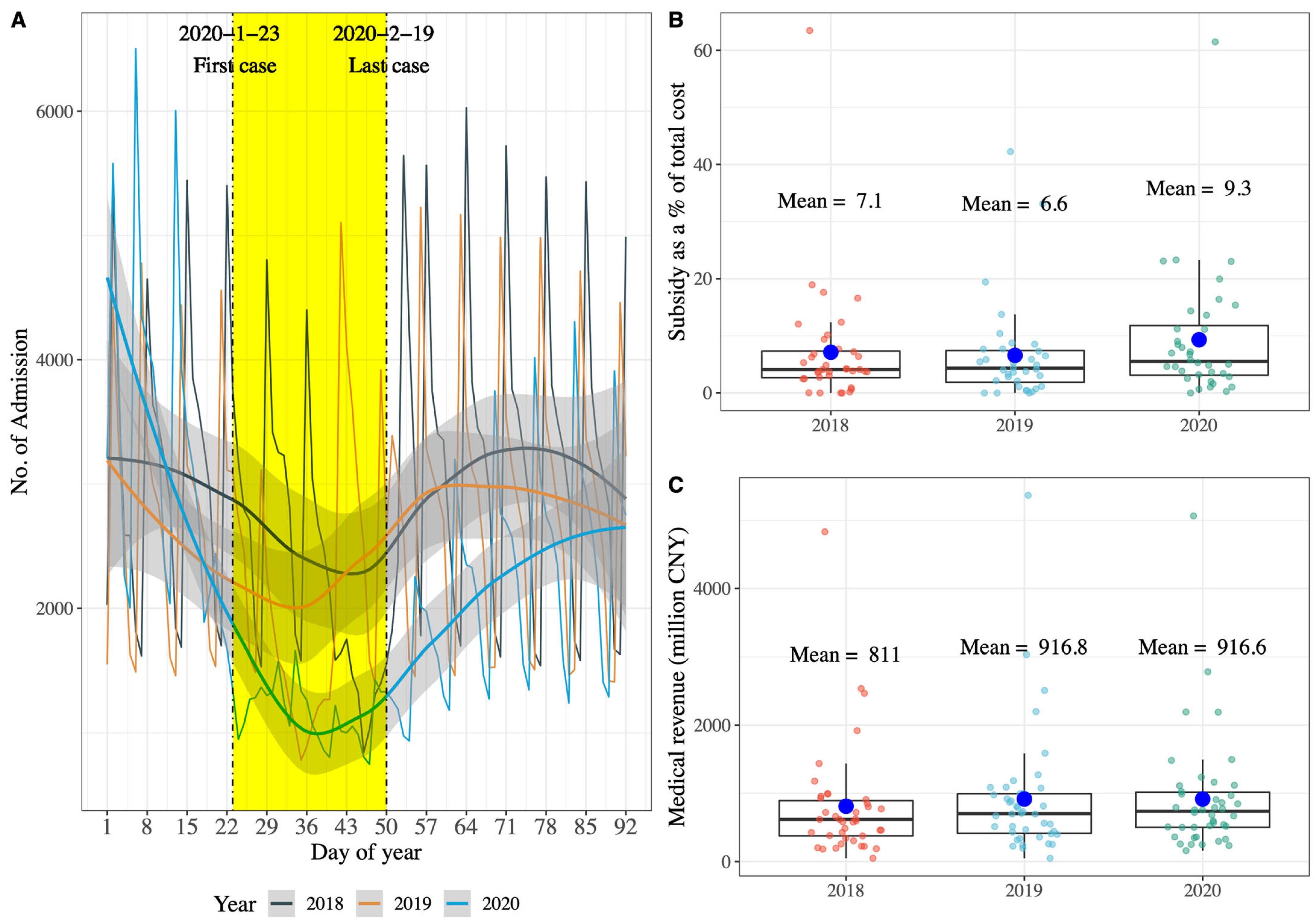
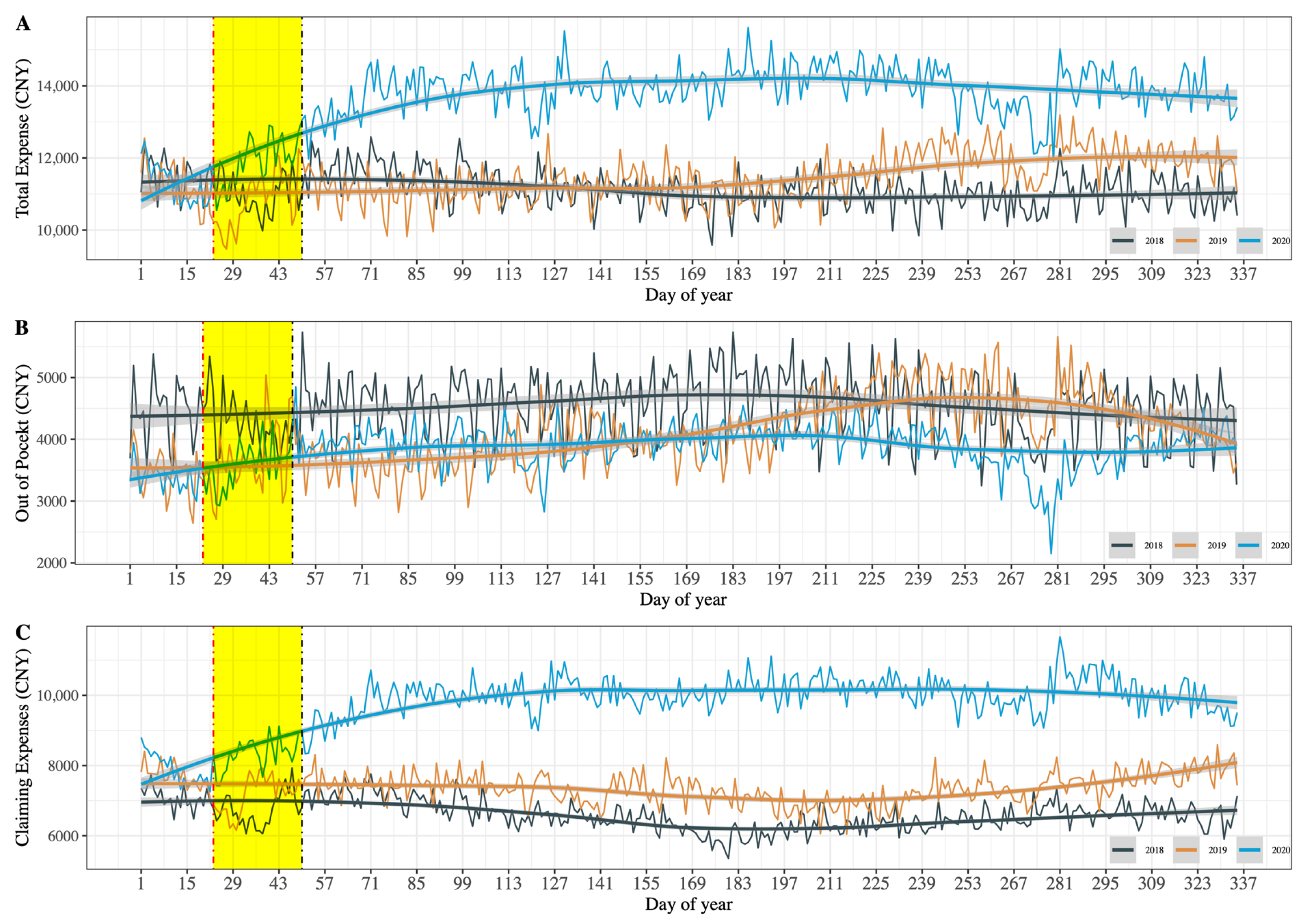
4.1. Descriptive Analysis
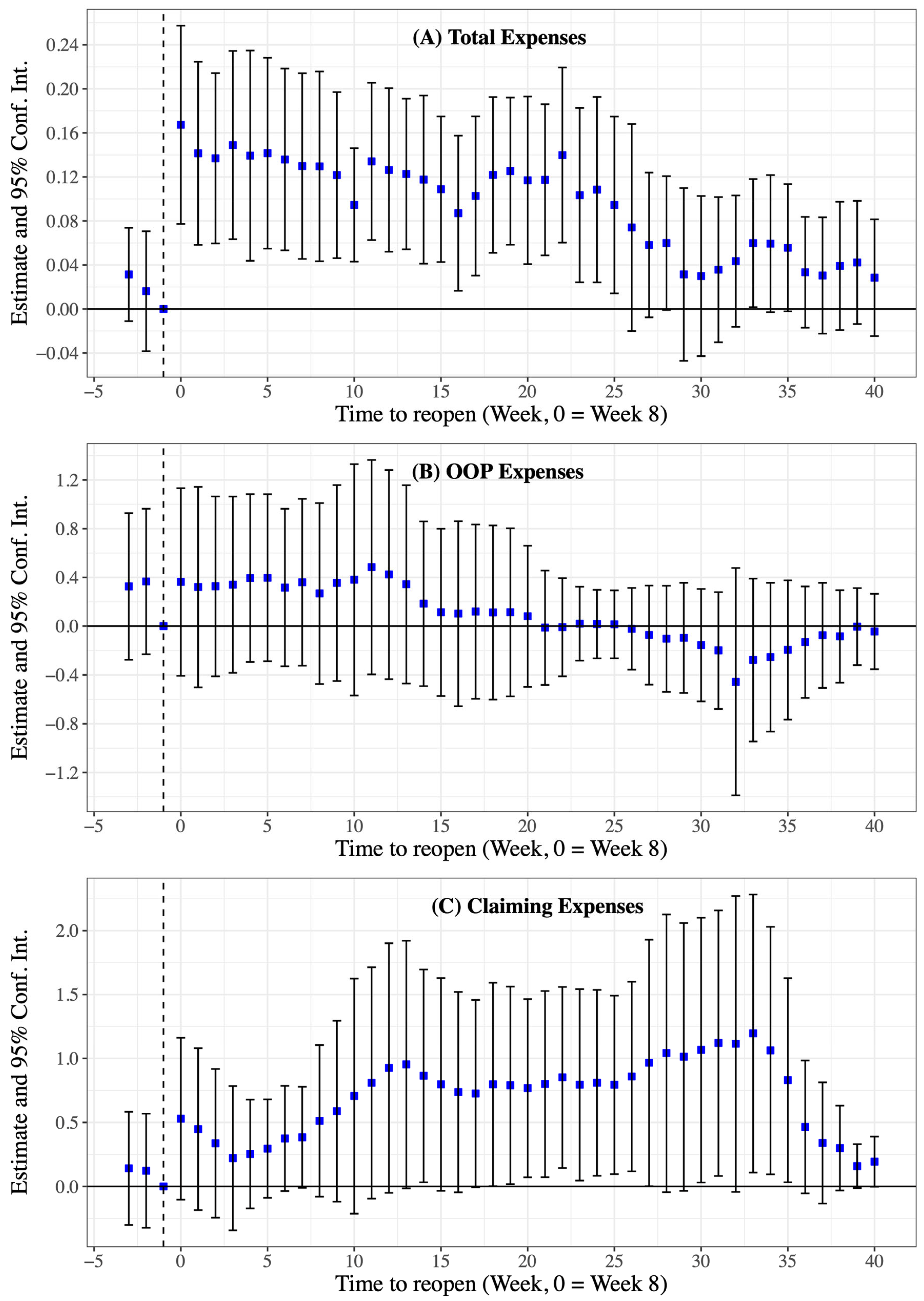
4.2. DID Event Study Analysis
4.3. Heterogeneous and Sensitivity Analysis
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Shen, H.; Fu, M.; Pan, H.; Yu, Z.; Chen, Y. The Impact of the COVID-19 Pandemic on Firm Performance. Emerg. Mark. Financ. Trade 2020, 56, 2213–2230. [Google Scholar] [CrossRef]
- Tisdell, C.A. Economic, Social and Political Issues Raised by the COVID-19 Pandemic. Econ. Anal. Policy 2020, 68, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Severo, E.A.; De Guimarães, J.C.F.; Dellarmelin, M.L. Impact of the COVID-19 Pandemic on Environmental Awareness, Sustainable Consumption and Social Responsibility: Evidence from Generations in Brazil and Portugal. J. Clean. Prod. 2021, 286, 124947. [Google Scholar] [CrossRef] [PubMed]
- Shang, W.-L.; Chen, J.; Bi, H.; Sui, Y.; Chen, Y.; Yu, H. Impacts of COVID-19 Pandemic on User Behaviors and Environmental Benefits of Bike Sharing: A Big-Data Analysis. Appl. Energy 2021, 285, 116429. [Google Scholar] [CrossRef]
- So, M.K.P.; Chu, A.M.Y.; Chan, T.W.C. Impacts of the COVID-19 Pandemic on Financial Market Connectedness. Financ. Res. Lett. 2021, 38, 101864. [Google Scholar] [CrossRef]
- Sun, X.; Wandelt, S.; Zheng, C.; Zhang, A. COVID-19 Pandemic and Air Transportation: Successfully Navigating the Paper Hurricane. J. Air Transp. Manag. 2021, 94, 102062. [Google Scholar] [CrossRef]
- Mafham, M.M. COVID-19 Pandemic and Admission Rates for and Management of Acute Coronary Syndromes in England. Lancet 2020, 396, 381–389. [Google Scholar] [CrossRef]
- Palmer, K.; Monaco, A.; Kivipelto, M.; Onder, G.; Maggi, S.; Michel, J.-P.; Prieto, R.; Sykara, G.; Donde, S. The Potential Long-Term Impact of the COVID-19 Outbreak on Patients with Non-Communicable Diseases in Europe: Consequences for Healthy Ageing. Aging Clin. Exp. Res. 2020, 32, 1189–1194. [Google Scholar] [CrossRef]
- Bodilsen, J.; Nielsen, P.B.; Søgaard, M.; Dalager-Pedersen, M.; Speiser, L.O.Z.; Yndigegn, T.; Nielsen, H.; Larsen, T.B.; Skjøth, F. Hospital Admission and Mortality Rates for Non-Covid Diseases in Denmark during Covid-19 Pandemic: Nationwide Population Based Cohort Study. BMJ 2021, 373, n1135. [Google Scholar] [CrossRef]
- Caminiti, C.; Maglietta, G.; Meschi, T.; Ticinesi, A.; Silva, M.; Sverzellati, N. Effects of the COVID-19 Epidemic on Hospital Admissions for Non-Communicable Diseases in a Large Italian University-Hospital: A Descriptive Case-Series Study. JCM 2021, 10, 880. [Google Scholar] [CrossRef]
- Kalanj, K.; Marshall, R.; Karol, K.; Tiljak, M.K.; Orešković, S. The Impact of COVID-19 on Hospital Admissions in Croatia. Front. Public Health 2021, 9, 720948. [Google Scholar] [CrossRef]
- Santi, L.; Golinelli, D.; Tampieri, A.; Farina, G.; Greco, M.; Rosa, S.; Beleffi, M.; Biavati, B.; Campinoti, F.; Guerrini, S.; et al. Non-COVID-19 Patients in Times of Pandemic: Emergency Department Visits, Hospitalizations and Cause-Specific Mortality in Northern Italy. PLoS ONE 2021, 16, e0248995. [Google Scholar] [CrossRef]
- Domingo, L.; Comas, M.; Jansana, A.; Louro, J.; Tizón-Marcos, H.; Cos, M.L.; Roquer, J.; Chillarón, J.J.; Cirera, I.; Pascual-Guàrdia, S.; et al. Impact of COVID-19 on Hospital Admissions and Healthcare Quality Indicators in Non-COVID Patients: A Retrospective Study of the First COVID-19 Year in a University Hospital in Spain. JCM 2022, 11, 1752. [Google Scholar] [CrossRef]
- Yang, Z.; Wu, M.; Lu, J.; Li, T.; Shen, P.; Tang, M.; Jin, M.; Lin, H.-B.; Shui, L.; Chen, K.; et al. Effect of COVID-19 on Hospital Visits in Ningbo, China: An Interrupted Time-Series Analysis. Int. J. Qual. Health Care 2021, 33, mzab078. [Google Scholar] [CrossRef]
- Cai, Y.; Kwek, S.; Tang, S.S.L.; Saffari, S.E.; Lum, E.; Yoon, S.; Ansah, J.P.; Matchar, D.B.; Kwa, A.L.; Ang, K.A.; et al. Impact of the COVID-19 Pandemic on a Tertiary Care Public Hospital in Singapore: Resources and Economic Costs. J. Hosp. Infect. 2022, 121, 1–8. [Google Scholar] [CrossRef]
- Xiao, H.; Dai, X.; Wagenaar, B.H.; Liu, F.; Augusto, O.; Guo, Y.; Unger, J.M. The Impact of the COVID-19 Pandemic on Health Services Utilization in China: Time-Series Analyses for 2016-2020. Lancet Reg. Health West. Pac. 2021, 9, 10. [Google Scholar] [CrossRef]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The Impact Of The COVID-19 Pandemic On Hospital Admissions In The United States: Study Examines Trends in US Hospital Admissions during the COVID-19 Pandemic. Health Aff. 2020, 39, 2010–2017. [Google Scholar] [CrossRef]
- Boserup, B.; McKenney, M.; Elkbuli, A. The Impact of the COVID-19 Pandemic on Emergency Department Visits and Patient Safety in the United States. Am. J. Emerg. Med. 2020, 38, 1732–1736. [Google Scholar] [CrossRef]
- Jeffery, M.M.; D’Onofrio, G.; Paek, H.; Platts-Mills, T.F.; Soares, W.E.; Hoppe, J.A.; Genes, N.; Nath, B.; Melnick, E.R. Trends in Emergency Department Visits and Hospital Admissions in Health Care Systems in 5 States in the First Months of the COVID-19 Pandemic in the US. JAMA Intern. Med. 2020, 180, 1328. [Google Scholar] [CrossRef]
- Cantor, J.; Sood, N.; Bravata, D.M.; Pera, M.; Whaley, C. The Impact of the COVID-19 Pandemic and Policy Response on Health Care Utilization: Evidence from County-Level Medical Claims and Cellphone Data. J. Health Econ. 2022, 82, 102581. [Google Scholar] [CrossRef]
- McIntosh, A.; Bachmann, M.; Siedner, M.J.; Gareta, D.; Seeley, J.; Herbst, K. Effect of COVID-19 Lockdown on Hospital Admissions and Mortality in Rural KwaZulu-Natal, South Africa: Interrupted Time Series Analysis. BMJ Open 2021, 11, e047961. [Google Scholar] [CrossRef] [PubMed]
- Sevalie, S.; Youkee, D.; van Duinen, A.J.; Bailey, E.; Bangura, T.; Mangipudi, S.; Mansaray, E.; Odland, M.L.; Parmar, D.; Samura, S.; et al. The Impact of the COVID-19 Pandemic on Hospital Utilisation in Sierra Leone. BMJ Glob. Health 2021, 6, e005988. [Google Scholar] [CrossRef] [PubMed]
- Yuan, Z.; Xiao, Y.; Dai, Z.; Huang, J.; Zhang, Z.; Chen, Y. Modelling the Effects of Wuhan’s Lockdown during COVID-19, China. Bull. World Health Organ. 2020, 98, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Meng, X.; Guo, M.; Gao, Z.; Yang, Z.; Yuan, Z.; Kang, L. The Effects of Wuhan Highway Lockdown Measures on the Spread of COVID-19 in China. Transp. Policy 2022, 117, 169–180. [Google Scholar] [CrossRef]
- Liu, J.; Zhang, L.; Yan, Y.; Zhou, Y.; Yin, P.; Qi, J.; Wang, L.; Pan, J.; You, J.; Yang, J.; et al. Excess Mortality in Wuhan City and Other Parts of China during the Three Months of the COVID-19 Outbreak: Findings from Nationwide Mortality Registries. BMJ 2021, 372, n415. [Google Scholar] [CrossRef]
- Qiu, Y.; Chen, X.; Shi, W. Impacts of Social and Economic Factors on the Transmission of Coronavirus Disease 2019 (COVID-19) in China. J. Popul. Econ. 2020, 33, 1127–1172. [Google Scholar] [CrossRef]
- Beck da Silva Etges, A.P.; Bertoglio Cardoso, R.; Marcolino, M.S.; Brasil Ruschel, K.; Coutinho, A.P.; Pereira, E.C.; Anschau, F.; Aranha, F.; Nader Bastos, G.A.; Lyra Batista, J.d.; et al. The Economic Impact of COVID-19 Treatment at a Hospital-Level: Investment and Financial Registers of Brazilian Hospitals. J. Health Econ. Outcomes Res. 2021, 8, 36–41. [Google Scholar] [CrossRef]
- Meng, Q.; Mills, A.; Wang, L.; Han, Q. What Can We Learn from China’s Health System Reform? BMJ 2019, 365, l2349. [Google Scholar] [CrossRef]
- Xu, J.; Jian, W.; Zhu, K.; Kwon, S.; Fang, H. Reforming Public Hospital Financing in China: Progress and Challenges. BMJ 2019, 365, l4015. [Google Scholar] [CrossRef]
- Deng, C.; Li, X.; Pan, J. Private Hospital Expansion in China: A Global Perspective. Glob. Health J. 2018, 2, 33–46. [Google Scholar] [CrossRef]
- Yi, H.; Miller, G.; Zhang, L.; Li, S.; Rozelle, S. Intended And Unintended Consequences of China’s Zero Markup Drug Policy. Health Aff. 2015, 34, 1391–1398. [Google Scholar] [CrossRef]
- Yang, C.; Shen, Q.; Cai, W.; Zhu, W.; Li, Z.; Wu, L.; Fang, Y. Impact of the Zero-Markup Drug Policy on Hospitalisation Expenditure in Western Rural China: An Interrupted Time Series Analysis. Trop. Med. Int. Health 2017, 22, 180–186. [Google Scholar] [CrossRef]
- Fu, H.; Li, L.; Yip, W. Intended and Unintended Impacts of Price Changes for Drugs and Medical Services: Evidence from China. Soc. Sci. Med. 2018, 211, 114–122. [Google Scholar] [CrossRef]
- Shi, X.; Zhu, D.; Man, X.; Wang, W.; Zhu, K.; Nicholas, S.; He, P. “The Biggest Reform to China’s Health System”: Did the Zero-Markup Drug Policy Achieve Its Goal at Traditional Chinese Medicines County Hospitals? Health Policy Plan. 2019, 34, 483–491. [Google Scholar] [CrossRef]
- Zeng, J.; Chen, X.; Fu, H.; Lu, M.; Jian, W. Short-Term and Long-Term Unintended Impacts of a Pilot Reform on Beijing’s Zero Markup Drug Policy: A Propensity Score-Matched Study. BMC Health Serv. Res. 2019, 19, 916. [Google Scholar] [CrossRef]
- Cheng, H.; Zhang, Y.; Sun, J.; Liu, Y. Impact of Zero-Mark-up Medicines Policy on Hospital Revenue Structure: A Panel Data Analysis of 136 Public Tertiary Hospitals in China, 2012–2020. BMJ Glob. Health 2021, 6, e007089. [Google Scholar] [CrossRef]
- Yan, J.; Lin, H.-H.; Zhao, D.; Hu, Y.; Shao, R. China’s New Policy for Healthcare Cost-Control Based on Global Budget: A Survey of 110 Clinicians in Hospitals. BMC Health Serv. Res. 2019, 19, 84. [Google Scholar] [CrossRef]
- Zhu, N.; Chen, S.; Yang, G.; Ning, S.; Li, X.; Nian, Y.; Zhang, Y.; Li, C. Analysis of the Path from Discovery of Novel Coronavirus Disease 2019 Cases to Its Diagnosis in Shaanxi Province. J. Xi’an Jiaotong Univ. Med. Sci. 2020, 41, 923–926. (In Chinese) [Google Scholar] [CrossRef]
- Zhu, N.; Li, C.; Ning, S.; Chen, S.; Cao, L.; Yang, G.; Li, X.; Nian, Y.; Wang, W.; Liu, Y.; et al. Epidemiological Characteristics of COVID-19 in Shaanxi Province. Chin. J. Epidemiol. 2020, 41, 1411–1414. (In Chinese) [Google Scholar] [CrossRef]
- Guo, W.; Guo, X.; Li, P.; Cao, L.; Pei, L.; Zeng, L.; Chen, Z.; Zhuang, G.; Qi, X.; Liu, F. Spatial Epidemiology Characteristics and Influencing Factors of Confirmed COVID-19 Cases in Shaanxi Province. Chin. J. Dis. Control Prev. 2021, 25, 400–404. (In Chinese) [Google Scholar] [CrossRef]
- Wang, T.; Gao, Q.; Zhao, L. Supply-side Responses to Zero Markup Drug Policy: Evidence from Inpatient Claims Data. J. World Econ. 2021, 44, 135. (In Chinese) [Google Scholar]
- Deshpande, M. Does Welfare Inhibit Success? The Long-Term Effects of Removing Low-Income Youth from the Disability Rolls. Am. Econ. Rev. 2016, 106, 3300–3330. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.C.; Kim, S.; Koh, K. The Impact of COVID-19 on Subjective Well-Being: Evidence from Singapore; Institute of Labor Economics (IZA): Bonn, Germany, 2020. [Google Scholar]
- Sun, L.; Abraham, S. Estimating Dynamic Treatment Effects in Event Studies with Heterogeneous Treatment Effects. J. Econom. 2020, 225, 175–199. [Google Scholar] [CrossRef]
- Callaway, B.; Sant’Anna, P.H.C. Difference-in-Differences with Multiple Time Periods. J. Econom. 2021, 225, 200–230. [Google Scholar] [CrossRef]
- Goodman-Bacon, A. Difference-in-Differences with Variation in Treatment Timing. J. Econom. 2021, 225, 254–277. [Google Scholar] [CrossRef]
- Athey, S.; Imbens, G.W. Design-Based Analysis in Difference-In-Differences Settings with Staggered Adoption. J. Econom. 2022, 226, 62–79. [Google Scholar] [CrossRef]
- National Health Commission of the People’ s Republic of China. China Health Statistical Yearbook 2021, 4-4-1: Public Hospital Revenues and Expenses; Peking Union Medical College Publishing House: Beijing, China, 2021. [Google Scholar]
- Ministry of Finance of China. National Health Commission of China Notice on the New Coronavirus Infection Pneumonia Outbreak Prevention and Control Related Funding Security Policy. Available online: http://www.gov.cn/zhengce/zhengceku/2020-01/30/content_5473079.htm (accessed on 10 July 2022).
- Czeisler, M.É.; Marynak, K.; Clarke, K.E.N.; Salah, Z.; Shakya, I.; Thierry, J.M.; Ali, N.; McMillan, H.; Wiley, J.F.; Weaver, M.D.; et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns—United States, June 2020. Cent. Dis. Control Prev. Morb. Mortal. Wkly. Rep. 2020, 69, 8. [Google Scholar]
- Maung, K.K.; Marques-Vidal, P. Impact of COVID-19 Pandemic on Cardiovascular Diseases Hospitalisation, Management and Mortality in Switzerland. Open Heart 2023, 10, e002259. [Google Scholar] [CrossRef]
- Roth, G.A.; Vaduganathan, M.; Mensah, G.A. Impact of the COVID-19 Pandemic on Cardiovascular Health in 2020. J. Am. Coll. Cardiol. 2022, 80, 631–640. [Google Scholar] [CrossRef]
- Cedrone, F.; Di Martino, G.; Di Giovanni, P.; Greco, E.; Trebbi, E.; Romano, F.; Staniscia, T. Reduction in Hospital Admissions for Cardiovascular Diseases (CVDs) during the Coronavirus Disease 2019 (COVID-19) Pandemic: A Retrospective Study from a Southern Italian Region in the Year 2020. Healthcare 2022, 10, 871. [Google Scholar] [CrossRef]
- Wu, Y.; Chen, F.; Sun, Z.; Zhang, Y.; Song, Y.; Feng, W.; Wang, Y.; Liu, Y.; Song, H. Impact of the Pandemic of COVID-19 on Emergency Attendance for Stroke and Acute Myocardial Infarction in Beijing, China. J. Thromb. Thrombolysis 2021, 52, 1047–1055. [Google Scholar] [CrossRef]
- Jiang, Q.; Lang, J.; Cai, J.; Wu, C.; Eggleston, K. Avoidable Hospital Admissions and Resource Use in China: An Exploratory Analysis of 2·57 Million Hospital Admissions. Lancet 2015, 386, S25. [Google Scholar] [CrossRef]
- Chen, S.; Fu, H.; Jian, W. Trends in Avoidable Hospitalizations in a Developed City in Eastern China: 2015 to 2018. BMC Health Serv. Res. 2022, 22, 856. [Google Scholar] [CrossRef]
- Jiang, L.; Ma, H. Surgical Protocol in a West China Day Surgery Center During the COVID-19 Pandemic: Practice and Experience. Surg. Innov. 2021, 28, 53–57. [Google Scholar] [CrossRef]
- National Healthcare Security Administration 2021 National Medical Security Business Development Statistics Bulletin. Available online: http://www.nhsa.gov.cn:8000/art/2022/6/8/art_7_8276.html (accessed on 17 April 2023).
- State Council of The People’s Republic of China China’s Health Insurance Coverage for COVID-19 Patients Tops 1.6b Yuan. Available online: http://english.www.gov.cn/statecouncil/ministries/202101/16/content_WS60021b9dc6d0f72576943e6c.html (accessed on 17 April 2023).
- Yip, W.; Fu, H.; Chen, A.T.; Zhai, T.; Jian, W.; Xu, R.; Pan, J.; Hu, M.; Zhou, Z.; Chen, Q.; et al. 10 Years of Health-Care Reform in China: Progress and Gaps in Universal Health Coverage. Lancet 2019, 394, 1192–1204. [Google Scholar] [CrossRef]



| Indicators | 2018 (n = 889,102) | 2019 (n = 884,408) | 2020 (n = 843,079) | Overall (n = 2,616,589) |
|---|---|---|---|---|
| Age (year) | ||||
| Mean (SD) | 50.1 (22.4) | 50.1 (22.5) | 51.8 (21.2) | 50.7 (22.1) |
| Median [Min, Max] | 54.0 [1.00, 119] | 54.0 [1.00, 110] | 56.0 [1.00, 107] | 55.0 [1.00, 119] |
| Sex | ||||
| Male | 421,330 (47.4%) | 416,751 (47.1%) | 414,921 (49.2%) | 1,253,002 (47.9%) |
| Female | 467,772 (52.6%) | 467,657 (52.9%) | 428,158 (50.8%) | 1,363,587 (52.1%) |
| Insurance Payment | ||||
| UEBMI | 260,256 (29.3%) | 266,725 (30.2%) | 266,296 (31.6%) | 793,277 (30.3%) |
| URBMI | 115,294 (13.0%) | 125,926 (14.2%) | 227,737 (27.0%) | 468,957 (17.9%) |
| NRCMSI | 304,335 (34.2%) | 276,585 (31.3%) | 129,458 (15.4%) | 710,378 (27.1%) |
| Poverty relief | 5004 (0.6%) | 6468 (0.7%) | 10,365 (1.2%) | 21,837 (0.8%) |
| Commercial medical insurance | 902 (0.1%) | 751 (0.1%) | 670 (0.1%) | 2323 (0.1%) |
| Publicly funded medical care | 2869 (0.3%) | 2001 (0.2%) | 1855 (0.2%) | 6725 (0.3%) |
| No medical insurance | 135,812 (15.3%) | 165,384 (18.7%) | 127,847 (15.2%) | 429,043 (16.4%) |
| Other social medical insurance | 8023 (0.9%) | 9693 (1.1%) | 6949 (0.8%) | 24,665 (0.9%) |
| Other insurance | 56,607 (6.4%) | 30,875 (3.5%) | 71,902 (8.5%) | 159,384 (6.1%) |
| Type of Admission | ||||
| Emergency | 228,982 (25.8%) | 226,141 (25.6%) | 270,103 (32.0%) | 725,226 (27.7%) |
| Outpatient | 622,129 (70.0%) | 614,395 (69.5%) | 557,553 (66.1%) | 1,794,077 (68.6%) |
| Referrals from other institutions | 1018 (0.1%) | 1355 (0.2%) | 1785 (0.2%) | 4158 (0.2%) |
| Other | 36,973 (4.2%) | 42,517 (4.8%) | 13,638 (1.6%) | 93,128 (3.6%) |
| Surgical | ||||
| No | 515,599 (58.0%) | 479,911 (54.3%) | 408,859 (48.5%) | 1,404,369 (53.7%) |
| Yes | 373,503 (42.0%) | 404,497 (45.7%) | 434,220 (51.5%) | 1,212,220 (46.3%) |
| Length of Admission | ||||
| Mean (SD) | 9.67 (6.97) | 9.32 (6.91) | 9.58 (6.88) | 9.52 (6.92) |
| Median [Min, Max] | 8.00 [1.00, 90.0] | 8.00 [1.00, 90.0] | 8.00 [1.00, 90.0] | 8.00 [1.00, 90.0] |
| Total Inpatient Expenses (CNY) | ||||
| Mean (SD) | 11,300 (12,800) | 11,600 (13,500) | 13,700 (16,400) | 12,200 (14,300) |
| Median [Min, Max] | 7070 [825, 90,100] | 7200 [768, 94,700] | 7860 [782, 108,000] | 7350 [768, 108,000] |
| Out-of-Pocket (CNY) | ||||
| Mean (SD) | 4690 (10,400) | 4200 (9100) | 3870 (9200) | 4260 (9590) |
| Median [Min, Max] | 0 [0, 90,100] | 0 [0, 94,700] | 0 [0, 108,000] | 0 [0, 108,000] |
| Claim Expenses (CNY) | ||||
| Mean (SD) | 6590 (10,300) | 7410 (11,300) | 9840 (14,200) | 7920 (12,100) |
| Median [Min, Max] | 3800 [0, 90,100] | 4280 [0, 94,700] | 5460 [0, 108,000] | 4520 [0, 108,000] |
| Laboratory Test Expenses (CNY) | ||||
| Mean (SD) | 1050 (1090) | 1180 (1150) | 1290 (1280) | 1170 (1180) |
| Median [Min, Max] | 830 [0, 35,000] | 943 [0, 47,600] | 1010 [0, 37,200] | 923 [0, 47,600] |
| Imaging Test Expenses (CNY) | ||||
| Mean (SD) | 732 (1330) | 768 (1360) | 909 (1570) | 801 (1420) |
| Median [Min, Max] | 331 [0, 58,300] | 330 [0, 58,600] | 435 [0, 70,700] | 369 [0, 70,700] |
| Drug Expenses (CNY) | ||||
| Mean (SD) | 2850 (4140) | 2740 (3960) | 3120 (4520) | 2900 (4210) |
| Median [Min, Max] | 1580 [0, 73,900] | 1570 [0, 86,600] | 1750 [0, 86,100] | 1630 [0, 86,600] |
| Medical Consumables Expenses (CNY) | ||||
| Mean (SD) | 1440 (5420) | 2220 (7210) | 3310 (9350) | 2310 (7500) |
| Median [Min, Max] | 0 [0, 85,300] | 85.1 [0, 86,500] | 163 [0, 100,000] | 79.9 [0, 100,000] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shen, C.; Cao, D.; Deng, Q.; Lai, S.; Liu, G.; Yang, L.; Zhu, Z.; Zhou, Z. Evaluating the Impact of COVID-19 on Hospital Profit Compensation Activities: A Difference-in-Differences Event Study Analysis in China. Healthcare 2023, 11, 1303. https://doi.org/10.3390/healthcare11091303
Shen C, Cao D, Deng Q, Lai S, Liu G, Yang L, Zhu Z, Zhou Z. Evaluating the Impact of COVID-19 on Hospital Profit Compensation Activities: A Difference-in-Differences Event Study Analysis in China. Healthcare. 2023; 11(9):1303. https://doi.org/10.3390/healthcare11091303
Chicago/Turabian StyleShen, Chi, Dan Cao, Qiwei Deng, Sha Lai, Guanping Liu, Liu Yang, Zhonghai Zhu, and Zhongliang Zhou. 2023. "Evaluating the Impact of COVID-19 on Hospital Profit Compensation Activities: A Difference-in-Differences Event Study Analysis in China" Healthcare 11, no. 9: 1303. https://doi.org/10.3390/healthcare11091303
APA StyleShen, C., Cao, D., Deng, Q., Lai, S., Liu, G., Yang, L., Zhu, Z., & Zhou, Z. (2023). Evaluating the Impact of COVID-19 on Hospital Profit Compensation Activities: A Difference-in-Differences Event Study Analysis in China. Healthcare, 11(9), 1303. https://doi.org/10.3390/healthcare11091303








