Postoperative Complications following Open Reduction and Rigid Internal Fixation of Mandibular Condylar Fracture Using the High Perimandibular Approach
Abstract
1. Introduction
2. Patients and Methods
2.1. Study Design
2.2. Patients
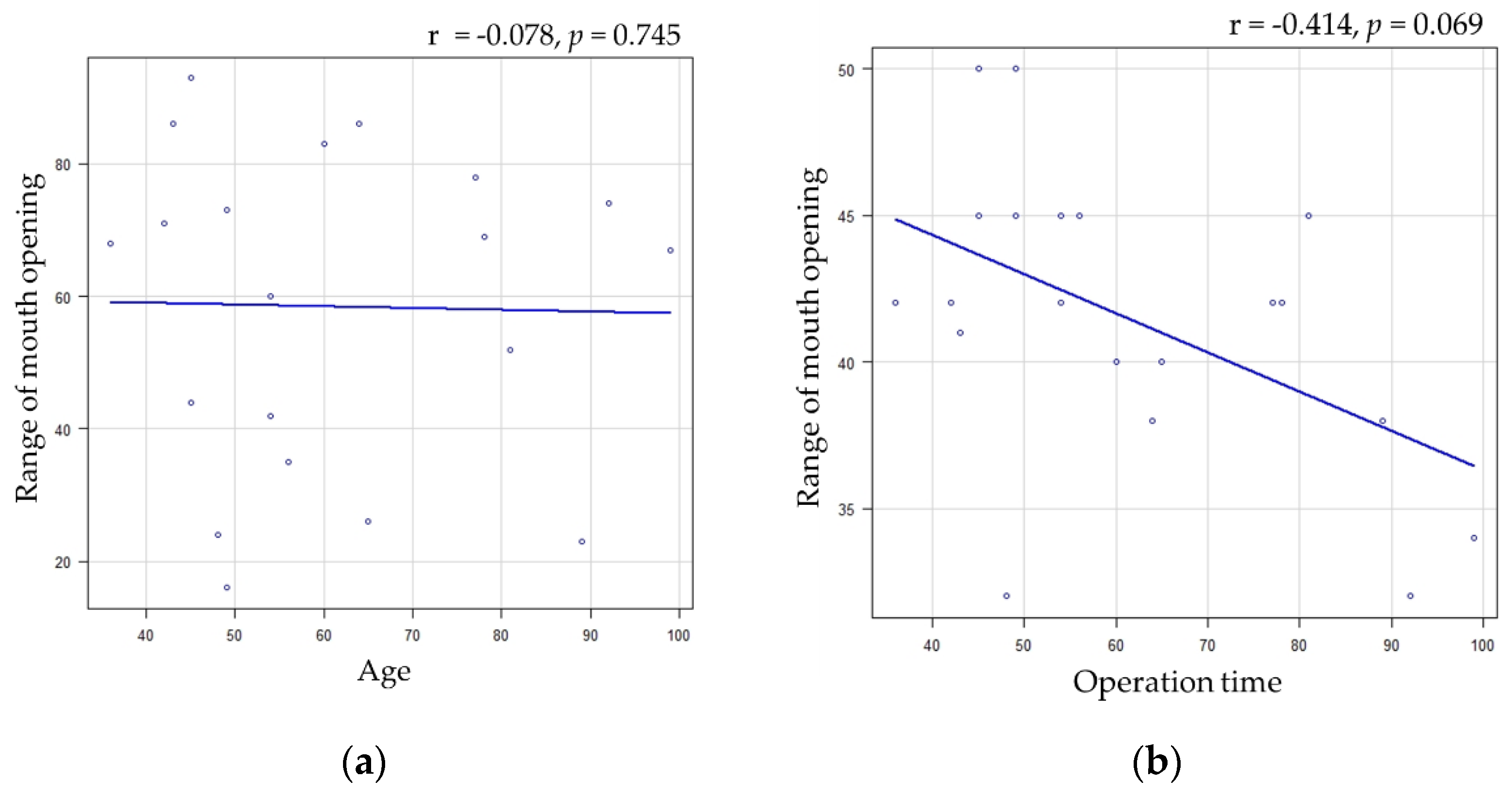
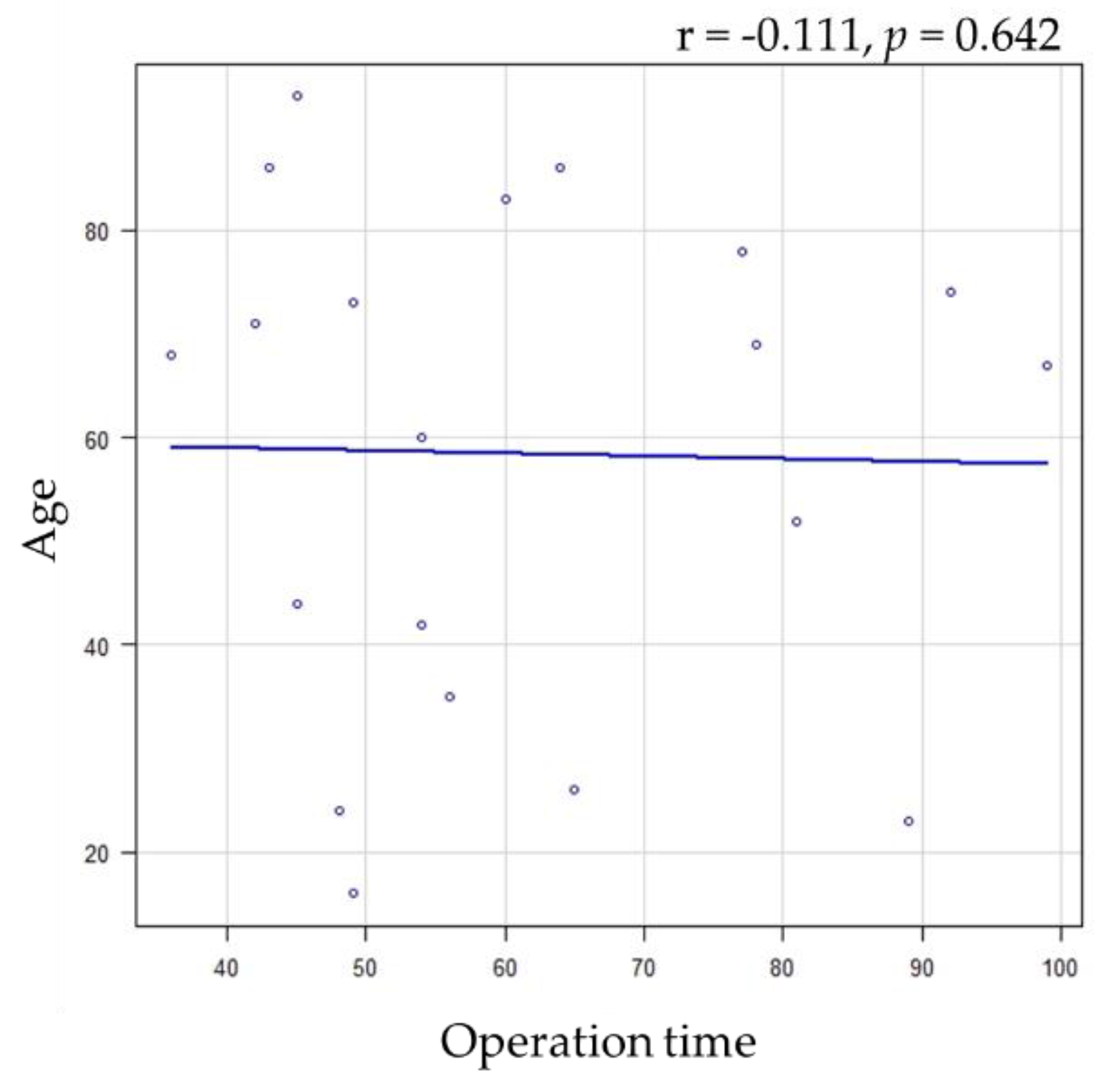
2.3. Evaluated Variables
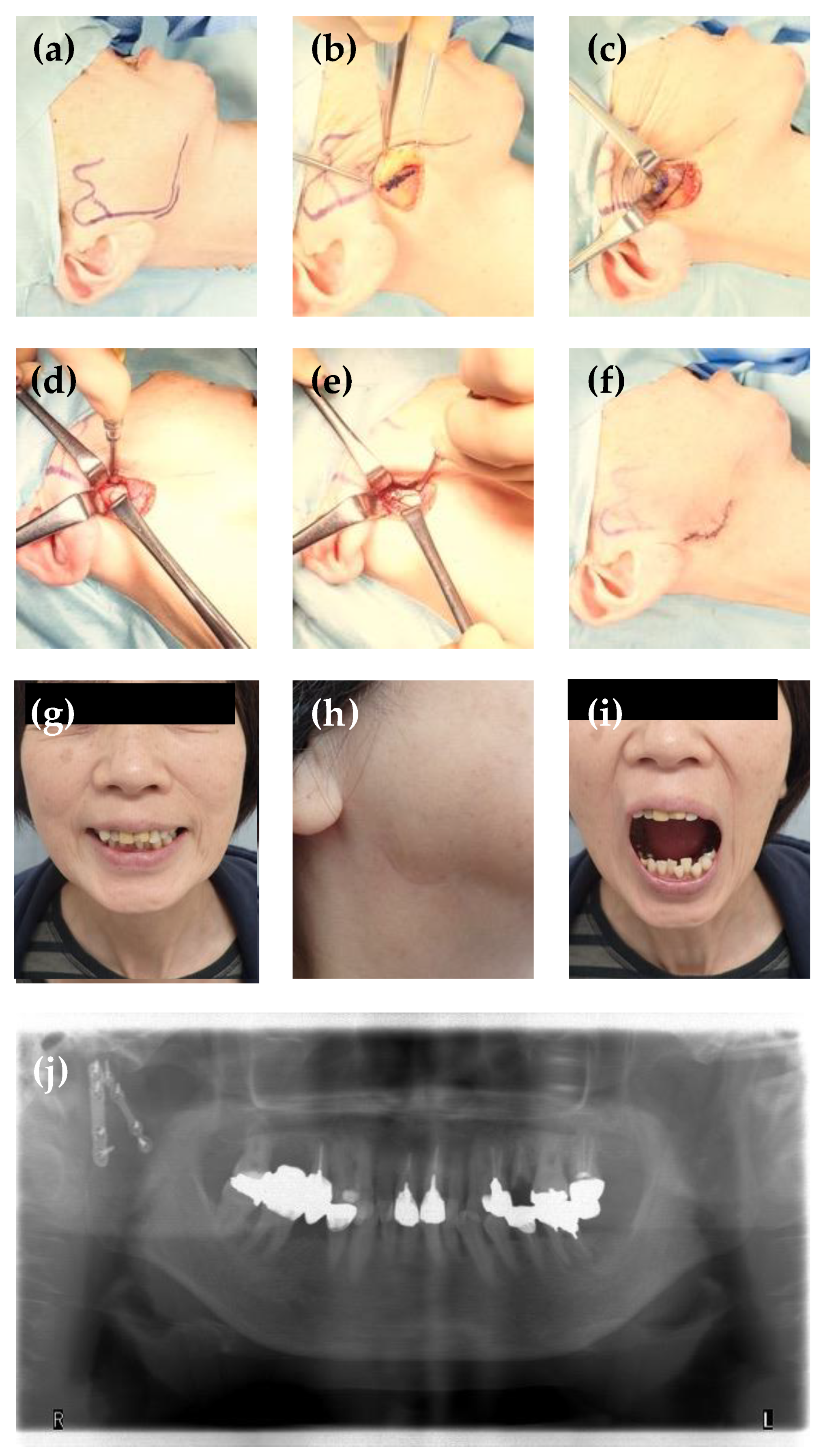
2.4. Surgical Procedures
2.5. Rehabilitation after Operation
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tatsumi, H.; Nakatani, E.; Kanno, T.; Nariai, Y.; Kagimura, T.; Sekine, J. Clinical Features and Treatment Modes of Mandibular Fracture at the Department of Oral and Maxillofacial Surgery, Shimane University Hospital, Japan. PLoS ONE 2015, 10, e0136278. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, R.; Ogiuchi, H.; Kumasaka, A.; Ando, T.; Nakamura, K.; Ueki, T.; Okada, Y.; Asanami, S.; Chigono, Y.; Ichinokawa, Y.; et al. Analysis of the Pattern of Maxillofacial Fracture by Five Departments in Tokyo. A Review of 674 Cases. Oral Sci. Int. 2009, 6, 1–7. [Google Scholar] [CrossRef]
- Simsek, S.; Simsek, B.; Abubaker, A.O.; Laskin, D.M. A comparative study of mandibular fractures in the United States and Turkey. Int. J. Oral. Maxillofac. Surg. 2007, 36, 395–397. [Google Scholar] [CrossRef]
- Uppada, U.K.; Sinha, R.; Susmitha, M.; Praseedha, B.; Kiran, B.R. Mandibular Fracture Patterns in a Rural Setup: A 7-Year Retrospective Study. J. Maxillofac. Oral. Surg. 2022, 21, 1349–1354. [Google Scholar] [CrossRef]
- Revanth Kumar, S.; Sinha, R.; Uppada, U.K.; Ramakrishna Reddy, B.V.; Paul, D. Mandibular Third Molar Position Influencing the Condylar and Angular Fracture Patterns. J. Maxillofac. Oral. Surg. 2015, 14, 956–961. [Google Scholar] [CrossRef]
- Tatsumi, H.; Hideshima, K.; Kanno, T.; Hashimoto, R.; Matsumoto, A.; Otani, H.; Sekine, J. Effect of ageing on healing of bilateral mandibular condyle fractures in a rat model. Int. J. Oral. Maxillofac. Surg. 2014, 43, 185–193. [Google Scholar] [CrossRef]
- Kyzas, P.A.; Saeed, A.; Tabbenor, O. The treatment of mandibular condyle fractures: A meta-analysis. J. Craniomaxillofac. Surg. 2012, 40, e438–e452. [Google Scholar] [CrossRef]
- Li, J.; Yang, H.; Han, L. Open versus closed treatment for unilateral mandibular extra-capsular condylar fractures: A meta-analysis. J. Craniomaxillofac. Surg. 2019, 47, 1110–1119. [Google Scholar] [CrossRef]
- Chen, C.T.; Feng, C.H.; Tsay, P.K.; Lai, J.P.; Chen, Y.R. Functional outcomes following surgical treatment of bilateral mandibular condylar fractures. Int. J. Oral. Maxillofac. Surg. 2011, 40, 38–44. [Google Scholar] [CrossRef]
- Dayalan, N.; Kumari, B.; Khanna, S.S.; Ansari, F.M.; Grewal, R.; Kumar, S.; Tiwari, R.V.C. Is Open Reduction and Internal Fixation Sacrosanct in the Management of Subcondylar Fractures: A Comparative Study. J. Pharm. Bioallied. Sci. 2021, 13, S1633–S1636. [Google Scholar] [CrossRef]
- Gupta, M.; Iyer, N.; Das, D.; Nagaraj, J. Analysis of different treatment protocols for fractures of condylar process of mandible. J. Oral. Maxillofac. Surg. 2012, 70, 83–91. [Google Scholar] [CrossRef]
- Petronis, Z.; Spaicyte, N.; Sakalys, D.; Januzis, G. Functional Rehabilitation after Mandibular Fracture—A Systematic Review. Ann. Maxillofac. Surg. 2022, 12, 197–202. [Google Scholar] [CrossRef]
- Jazayeri, H.E.; Lopez, J.; Khavanin, N.; Xun, H.; Lee, U.K.; Best, D.L.; Reategui, A.; Urata, M.M.; Dorafshar, A.H. Comparative Benefits of Open versus Closed Reduction of Condylar Fractures: A Systematic Review and Meta-Analysis. Plast. Reconstr. Surg. 2023, 151, 664e–672e. [Google Scholar] [CrossRef]
- Ellis, E., 3rd; Dean, J. Rigid fixation of mandibular condyle fractures. Oral. Surg. Oral. Med. Oral. Pathol. 1993, 76, 6–15. [Google Scholar] [CrossRef]
- Kanno, T.; Mitsugi, M.; Sukegawa, S.; Fujioka, M.; Furuki, Y. Submandibular approach through the submandibular gland fascia for treating mandibular fractures without identifying the facial nerve. J. Trauma 2010, 68, 641–643. [Google Scholar] [CrossRef]
- Kanno, T.; Sukegawa, S.; Tatsumi, H.; Nariai, Y.; Ishibashi, H.; Furuki, Y.; Sekine, J. The retromandibular transparotid approach for reduction and rigid internal fixation using two locking miniplates in mandibular condylar neck fractures. Int. J. Oral. Maxillofac. Surg. 2014, 43, 177–184. [Google Scholar] [CrossRef]
- Trost, O.; Abu El-Naaj, I.; Trouilloud, P.; Danino, A.; Malka, G. High cervical transmasseteric anteroparotid approach for open reduction and internal fixation of condylar fracture. J. Oral. Maxillofac. Surg. 2008, 66, 201–204. [Google Scholar] [CrossRef]
- Wilk, A.; Biotchane, I.; Rosenstiel, M.; Charles, X.; Meyer, C. Osteosynthesis of subcondylar fractures using a rectangular 3-dimensional stabilization plate. Rev. Stomatol. Chir. Maxillofac. 1997, 98 (Suppl. 1), 40–44. [Google Scholar]
- Wilk, A. High perimandubular approach. In Fractures of the Mandibular Condyle; Kleinhenz, J.M.C., Ed.; Quintessence Publishing: London, UK, 2009; pp. 143–154. [Google Scholar]
- Nowair, I.M.; Essa, E.F.; Eid, M.K. A comparative evaluation of retromandibular versus Modified Risdon approach in surgical treatment of condylar fracture. J. Craniomaxillofac. Surg. 2021, 50, 237–245. [Google Scholar] [CrossRef]
- Ruiz, R.; Schlund, M.; Raoul, G.; Kyheng, M.; Fontaine, C.; Nicot, R. Mandibular subcondylar fracture accessibility with transparotid approach by rhytidectomy and modified Risdon approach: An anatomical comparative study. J. Craniomaxillofac. Surg. 2018, 46, 2256–2260. [Google Scholar] [CrossRef]
- Lee, S.J.; Chun, Y.J.; Jun, S.H.; Song, I.S. Modified high-submandibular appraoch for open reduction and internal fixation of condylar fracture: Case series report. J. Korean Assoc. Oral. Maxillofac. Surg. 2022, 48, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Zrounba, H.; Lutz, J.C.; Zink, S.; Wilk, A. Epidemiology and treatment outcome of surgically treated mandibular condyle fractures. A five years retrospective study. J. Craniomaxillofac. Surg. 2014, 42, 879–884. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.M.; Lee, J.H.; Kim, J.H. The application of the Risdon approach for mandibular condyle fractures. BMC Surg. 2013, 13, 25. [Google Scholar] [CrossRef] [PubMed]
- Conci, R.A.; Tomazi, F.H.; Kalaoun, R.; Fritscher, G.G.; de Oliveira, G.R.; Heitz, C. Modified submandibular access for open reduction and internal rigid fixation in condylar fractures. J. Craniofac Surg. 2015, 26, 232–234. [Google Scholar] [CrossRef] [PubMed]
- Pau, M.; Navisany, K.; Reinbacher, K.E.; Zrnc, T.; Wallner, J.; Schwenzer-Zimmerer, K. Use of a modified high submandibular approach to treat condylar base fractures: Experience with 44 consecutive cases treated in a single institution. J. Craniomaxillofac. Surg. 2016, 44, 1641–1645. [Google Scholar] [CrossRef] [PubMed]
- Kudva, A.; Kamath, A.T.; Rajan, J.; D’Souza, C. A Modified Peri-Angular Approach for Exposure of Condylar Fractures. J. Oral. Maxillofac. Surg. 2018, 76, 1504–1508. [Google Scholar] [CrossRef]
- Meyer, C.; Zink, S.; Chatelain, B.; Wilk, A. Clinical experience with osteosynthesis of subcondylar fractures of the mandible using TCP plates. J. Craniomaxillofac. Surg. 2008, 36, 260–268. [Google Scholar] [CrossRef]
- Al-Moraissi, E.A.; Louvrier, A.; Colletti, G.; Wolford, L.M.; Biglioli, F.; Ragaey, M.; Meyer, C.; Ellis, E., 3rd. Does the surgical approach for treating mandibular condylar fractures affect the rate of seventh cranial nerve injuries? A systematic review and meta-analysis based on a new classification for surgical approaches. J. Craniomaxillofac. Surg. 2018, 46, 398–412. [Google Scholar] [CrossRef]
- Handschel, J.; Rüggeberg, T.; Depprich, R.; Schwarz, F.; Meyer, U.; Kübler, N.R.; Naujoks, C. Comparison of various approaches for the treatment of fractures of the mandibular condylar process. J. Craniomaxillofac. Surg. 2012, 40, e397–e401. [Google Scholar] [CrossRef]
- Lutz, J.C.; Clavert, P.; Wolfram-Gabel, R.; Wilk, A.; Kahn, J.L. Is the high submandibular transmasseteric approach to the mandibular condyle safe for the inferior buccal branch? Surg. Radiol. Anat. 2010, 32, 963–969. [Google Scholar] [CrossRef]
- Trost, O.; Trouilloud, P.; Malka, G. Open reduction and internal fixation of low subcondylar fractures of mandible through high cervical transmasseteric anteroparotid approach. J. Oral. Maxillofac. Surg. 2009, 67, 2446–2451. [Google Scholar] [CrossRef]
- Neff, A.; Cornelius, C.P.; Rasse, M.; Torre, D.D.; Audigé, L. The Comprehensive AOCMF Classification System: Condylar Process Fractures—Level 3 Tutorial. Craniomaxillofac. Trauma Reconstr. 2014, 7, S044–S058. [Google Scholar] [CrossRef]
- Mac, L.W. Consideration of 180 cases of typical fractures of the mandibular condylar process. Br. J. Plast. Surg. 1952, 5, 122–128. [Google Scholar] [CrossRef]
- Dos Santos, K.W.; Hugo, F.N.; da Cunha Rodrigues, E.; Stein, A.T.; Hilgert, J.B. Effect of oral exercises and photobiomodulation therapy in the rehabilitation of patients with mandible fractures: Randomized double-blind clinical trial. Lasers Med. Sci. 2022, 37, 1727–1735. [Google Scholar] [CrossRef]
- Nogami, S.; Takahashi, T.; Yamauchi, K.; Miyamoto, I.; Kaneuji, T.; Yamamoto, N.; Yoshiga, D.; Yamashita, Y. Clinical comparison between the retromandibular approach for reduction and fixation and endoscope-assisted open reduction and internal fixation for mandibular condyle fractures. J. Craniomaxillofac. Surg. 2012, 23, 1815–1818. [Google Scholar] [CrossRef]
- Ellis, E.; Throckmorton, G.S. Treatment of mandibular condylar process fractures: Biological considerations. J. Oral. Maxillofac. Surg. 2005, 63, 115–134. [Google Scholar] [CrossRef]
- Vesnaver, A.; Gorjanc, M.; Eberlinc, A.; Dovsak, D.A.; Kansky, A.A. The periauricular transparotid approach for open reduction and internal fixation of condylar fractures. J. Craniomaxillofac. Surg. 2005, 33, 169–179. [Google Scholar] [CrossRef]
- Imai, T.; Nakazawa, M.; Uzawa, N. Advanced Model of a 4-Step Chart for Percutaneous Approaches to Condylar Fractures: A Tool to Comprehend Trends in Classification Based on the Dissection Route. J. Oral. Maxillofac. Surg. 2019, 77, 1962–1964. [Google Scholar] [CrossRef]
- Haug, R.H.; Brandt, M.T. Closed reduction, open reduction, and endoscopic assistance: Current thoughts on the management of mandibular condyle fractures. Plast. Reconstr. Surg. 2007, 120, 90s–102s. [Google Scholar] [CrossRef]
- Wei, C.; Gu, A.; Almeida, N.D.; Bestourous, D.; Quan, T.; Fassihi, S.C.; Recarey, M.; Malahias, M.A.; Haney, V.; Moghtaderi, S. Operation time effect on rates of perioperative complications after operative treatment of distal radius fractures. J. Orthop. 2021, 24, 82–85. [Google Scholar] [CrossRef]
- Cheng, H.; Chen, B.P.; Soleas, I.M.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged Operative Duration Increases Risk of Surgical Site Infections: A Systematic Review. Surg. Infect. 2017, 18, 722–735. [Google Scholar] [CrossRef]
- Cheng, H.; Clymer, J.W.; Po-Han Chen, B.; Sadeghirad, B.; Ferko, N.C.; Cameron, C.G.; Hinoul, P. Prolonged operative duration is associated with complications: A systematic review and meta-analysis. J. Surg. Res. 2018, 229, 134–144. [Google Scholar] [CrossRef]
- Tang, M.; Wang, L.; Zhang, M.; Sun, L.; Fu, G.; Xiao, J. Modified Tragus Edge and Transmasseteric Anteroparotid Approach for Intracapsular and Condylar Neck Fractures. J. Craniofac. Surg. 2020, 31, 1822–1826. [Google Scholar] [CrossRef]
- Adnot, J.; Feuss, A.; Duparc, F.; Trost, O. Retraction force necessary to expose the mandibular neck in Risdon and high cervical anteroparotid transmasseteric approaches: An anatomic comparative study. Surg. Radiol. Anat. 2017, 39, 1079–1084. [Google Scholar] [CrossRef]
- Özkan, H.S.; Sahin, B.; Görgü, M.; Melikoglu, C. Results of transmasseteric anteroparotid approach for mandibular condylar fractures. J. Craniofac. Surg. 2010, 21, 1882–1883. [Google Scholar] [CrossRef]
- Sforza, C.; Ugolini, A.; Sozzi, D.; Galante, D.; Mapelli, A.; Bozzetti, A. Three-dimensional mandibular motion after closed and open reduction of unilateral mandibular condylar process fractures. J. Craniomaxillofac. Surg. 2011, 39, 249–255. [Google Scholar] [CrossRef] [PubMed]
| Item | Category | N (%) or Median (25–75 Percentile) |
|---|---|---|
| Sex | Male | 11 (55.0) |
| Female | 9 (45.0) | |
| Age | 67.5 (40.3–75.0) | |
| Cause of injury | Fall | 15 (75.0) |
| Traffic accident | 2 (10.0) | |
| Sports | 1 (5.0) | |
| Violence | 1 (5.0 | |
| Work | 1 (5.0) | |
| Site of fracture | Neck | 10 (50.0) |
| Subcondyle | 10 (50.0) | |
| Type of fracture | Deviation | 12 (60.0) |
| Displacement | 5 (25.0) | |
| Dislocation | 3 (15.0) | |
| Presence of associated maxillofacial fractures | Yes | 13 (65.0) |
| Item | Category | N (%) or Median (25–75 Percentile) |
|---|---|---|
| Operation time (only condyle fracture) | 55.0 (47.25–77.25) | |
| Range of mouth opening | 42.0 (39.5–45.0) | |
| Surgical site infection | Yes | 0 (0) |
| Facial nerve palsy | Yes | 0 (0) |
| Surgical scar perceptibility | Yes | 0 (0) |
| Malocclusion | Yes | 0 (0) |
| Temporomandibular joint pain | Yes | 0 (0) |
| Poor state of reduction | Yes | 0 (0) |
| Plate breakage | Yes | 0 (0) |
| Screw loosening | Yes | 0 (0) |
| Item | Category | Range of Mouth Opening (Median (25–75 Percentile)) | p Value |
|---|---|---|---|
| Sex | Male (n = 11) | 45.0 (42.0–45.0) | 0.15 |
| Female (n = 9) | 41.0 (40.0–42.0) | ||
| Cause of trauma | Fall (n = 15) | 42.0 (39.0–45.0) | 0.64 |
| Traffic accident (n = 2) | 42.0 (42.0–42.0) | ||
| Others (n = 3) | 45.0 (41.5–47.5) | ||
| Site of fracture | Neck (n = 10) | 39.0 (35.0–42.0) | 0.02 * |
| Subcondyle (n = 10) | 43.5 (42.0–45.0) | ||
| Type of fracture | Deviation (n = 12) | 41.5 (40.0–45.0) | 0.38 |
| Displacement (n = 5) | 38.0 (38.0–42.0) | ||
| Dislocation (n = 3) | 45.0 (43.5–45.0) | ||
| Presence of associated maxillofacial fractures | Yes (n = 13) | 42.0 (40.0–45.0) | 0.31 |
| None (n = 7) | 42.0 (38.0–42.0) |
| Item | Category | Operation Time (Median (25–75 Percentile)) | p Value |
|---|---|---|---|
| Sex | Male (n = 11) | 54.0 (48.5–79.5) | 0.88 |
| Female (n = 9) | 60.0 (45.0–65.0) | ||
| Cause of trauma | Fall (n = 15) | 60.0 (51.5–77.5) | 0.68 |
| Traffic accident (n = 2) | 39.0 (37.5–40.5) | ||
| Others (n = 3) | 49.0 (47.0–69.0) | ||
| Site of fracture | Neck (n = 10) | 70.5 (55.5–87.0) | 0.03 * |
| Subcondyle (n = 10) | 49.0 (43.5–55.5) | ||
| Type of fracture | Deviation (n = 12) | 49.0 (44.5–57.0) | 0.08 |
| Displacement (n = 5) | 78.0 (64.0–89.0) | ||
| Dislocation (n = 3) | 77.0 (65.5–79.0) | ||
| Presence of associated maxillofacial fractures | Yes (n = 13) | 54.0 (45.0–65.0) | 0.38 |
| None (n = 7) | 64.0 (51.5–83.5) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tatsumi, H.; Matsuda, Y.; Toda, E.; Okui, T.; Okuma, S.; Kanno, T. Postoperative Complications following Open Reduction and Rigid Internal Fixation of Mandibular Condylar Fracture Using the High Perimandibular Approach. Healthcare 2023, 11, 1294. https://doi.org/10.3390/healthcare11091294
Tatsumi H, Matsuda Y, Toda E, Okui T, Okuma S, Kanno T. Postoperative Complications following Open Reduction and Rigid Internal Fixation of Mandibular Condylar Fracture Using the High Perimandibular Approach. Healthcare. 2023; 11(9):1294. https://doi.org/10.3390/healthcare11091294
Chicago/Turabian StyleTatsumi, Hiroto, Yuhei Matsuda, Erina Toda, Tatsuo Okui, Satoe Okuma, and Takahiro Kanno. 2023. "Postoperative Complications following Open Reduction and Rigid Internal Fixation of Mandibular Condylar Fracture Using the High Perimandibular Approach" Healthcare 11, no. 9: 1294. https://doi.org/10.3390/healthcare11091294
APA StyleTatsumi, H., Matsuda, Y., Toda, E., Okui, T., Okuma, S., & Kanno, T. (2023). Postoperative Complications following Open Reduction and Rigid Internal Fixation of Mandibular Condylar Fracture Using the High Perimandibular Approach. Healthcare, 11(9), 1294. https://doi.org/10.3390/healthcare11091294







