Hospital Admission Due to Hypotension in Australia and in England and Wales
Abstract
1. Introduction
2. Methods
2.1. Data Sources
2.1.1. Hospital Episode Statistics Database and the Patient Episode Database for Wales
2.1.2. National Hospital Morbidity Database
2.1.3. Office for National Statistics (ONS)
2.1.4. Australian Bureau of Statistics
2.2. Study Population
2.3. Statistical Analysis
3. Results
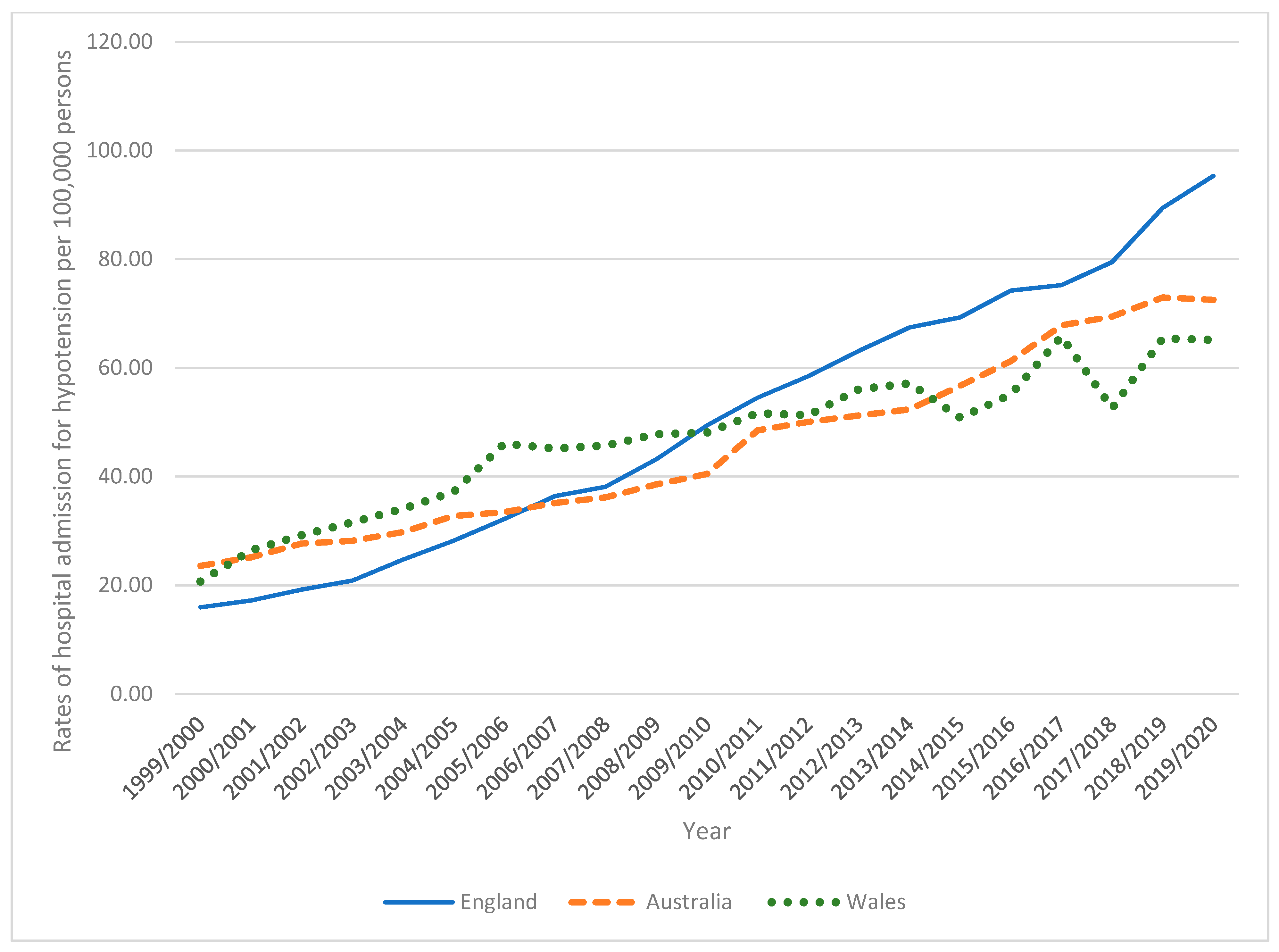
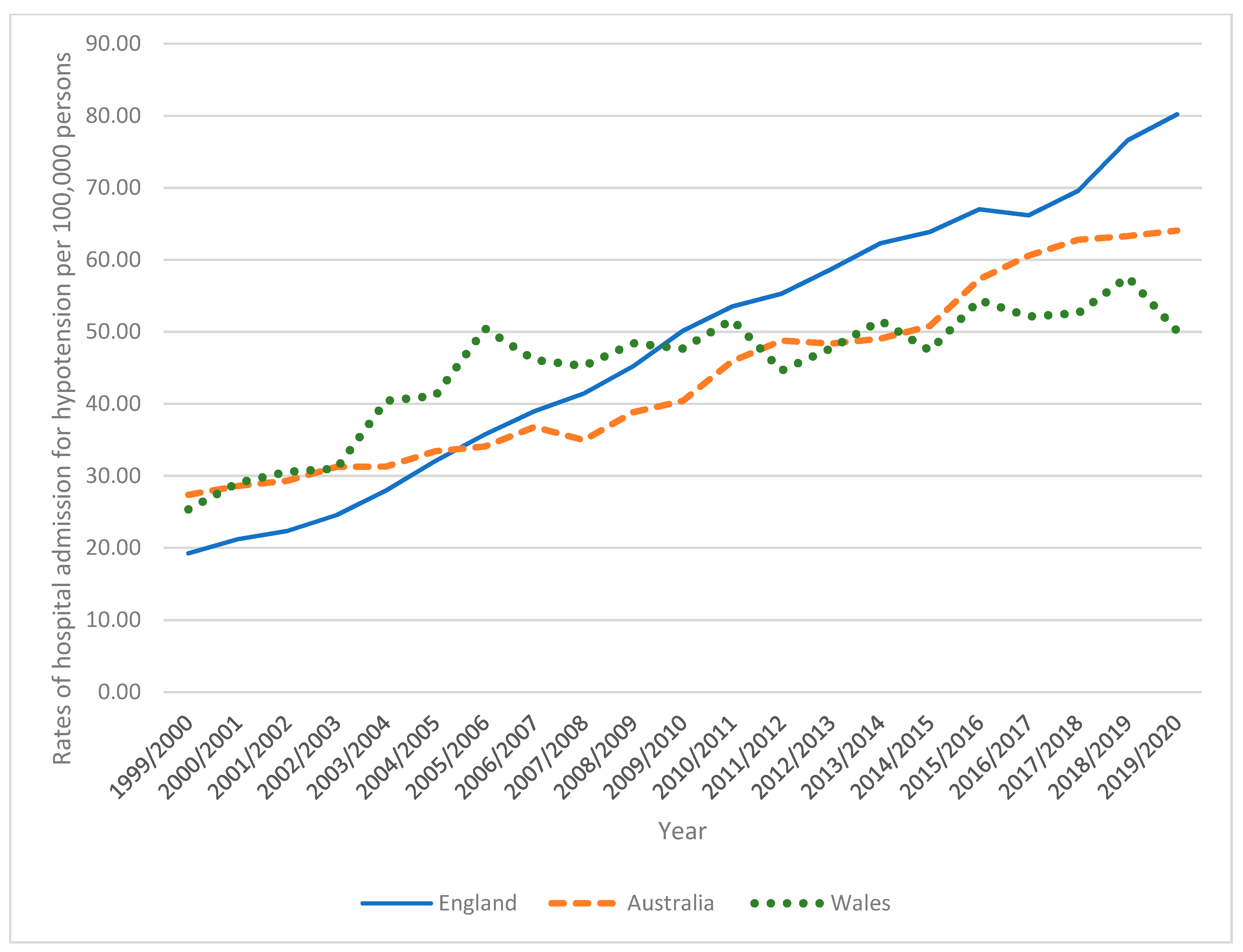
3.1. Trends in Total Hypotension Hospital Admissions
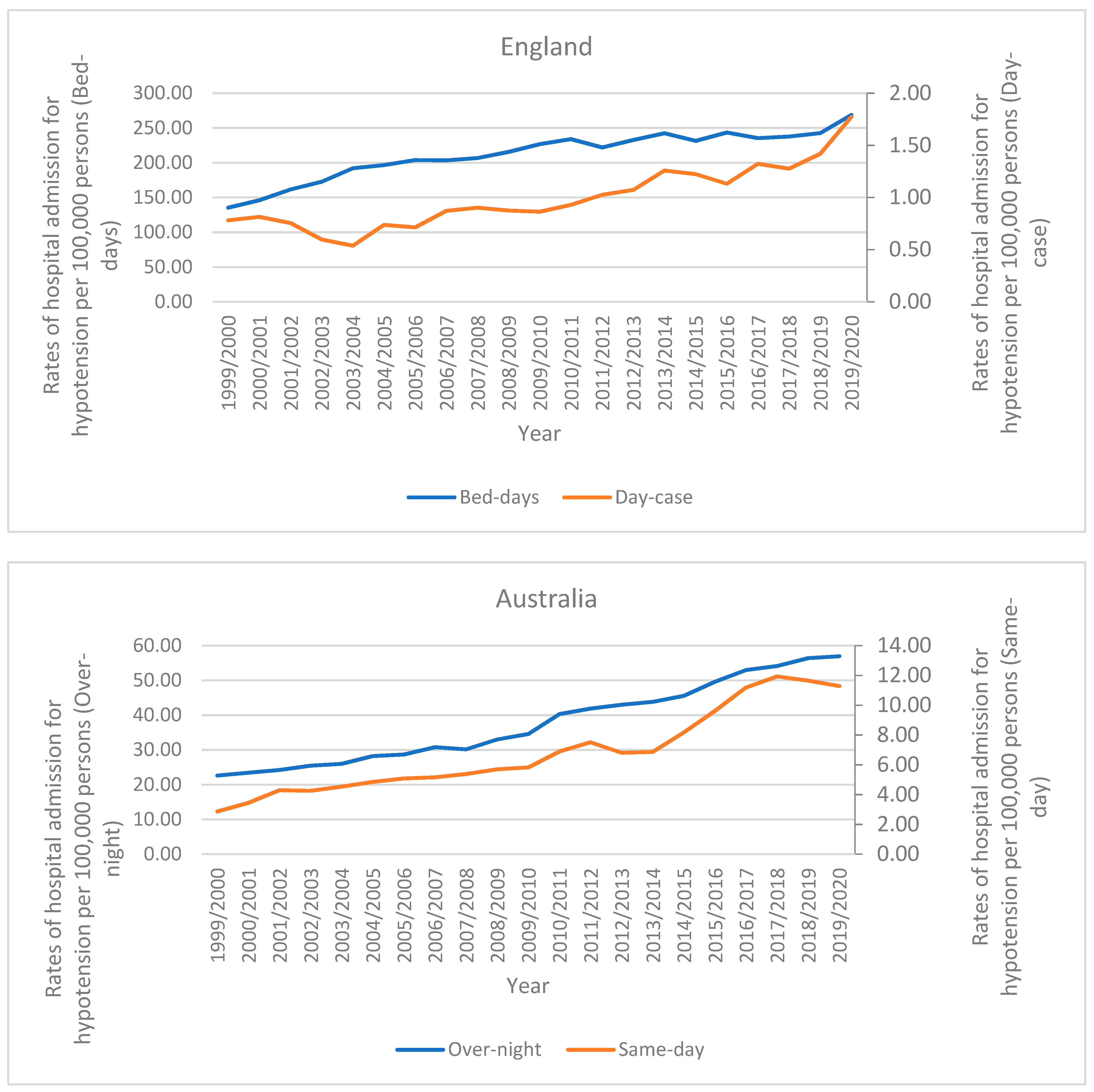
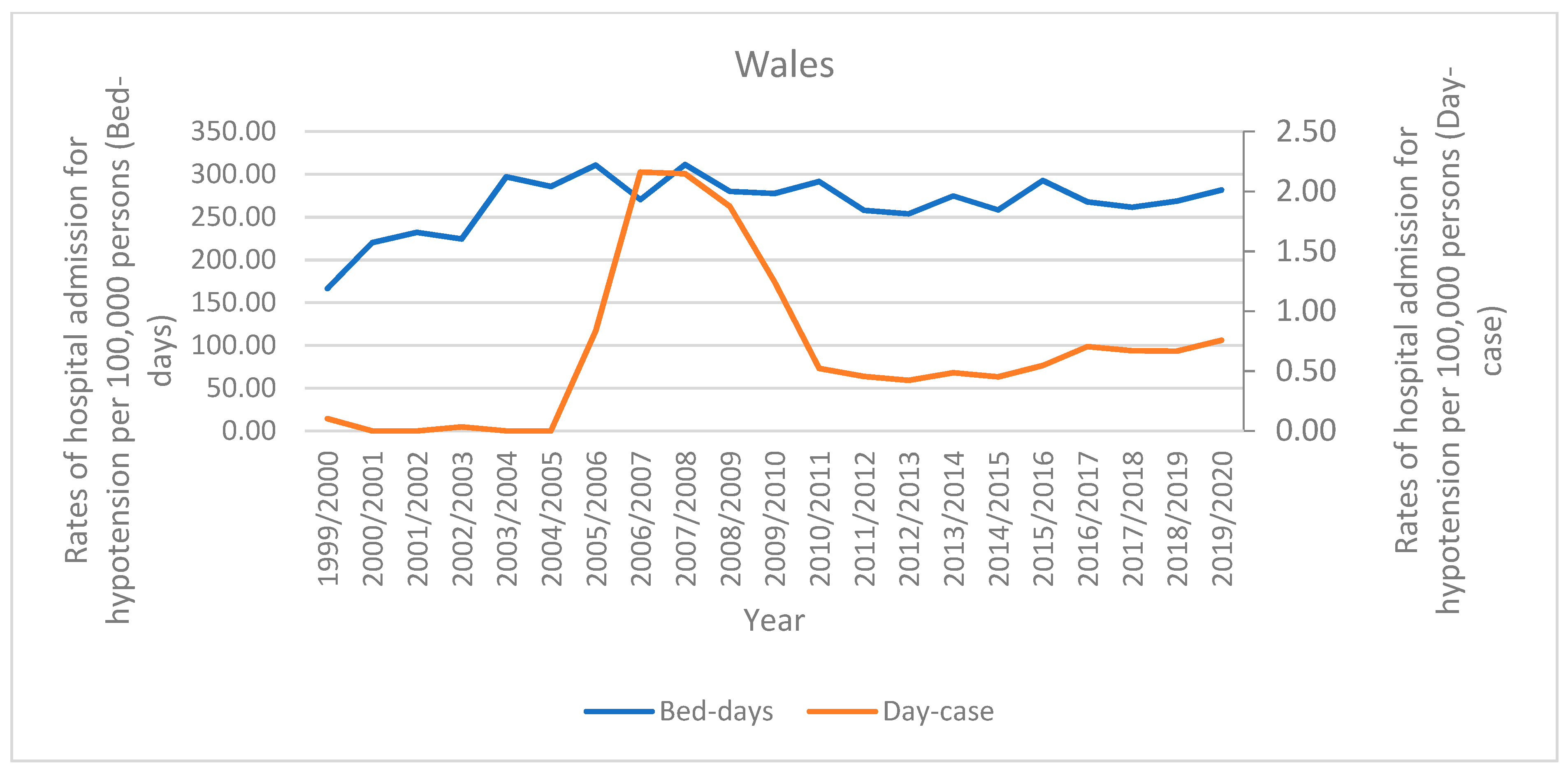
3.2. Trends in Total Hypotension Hospital Admissions Stratified by Hospital Stay
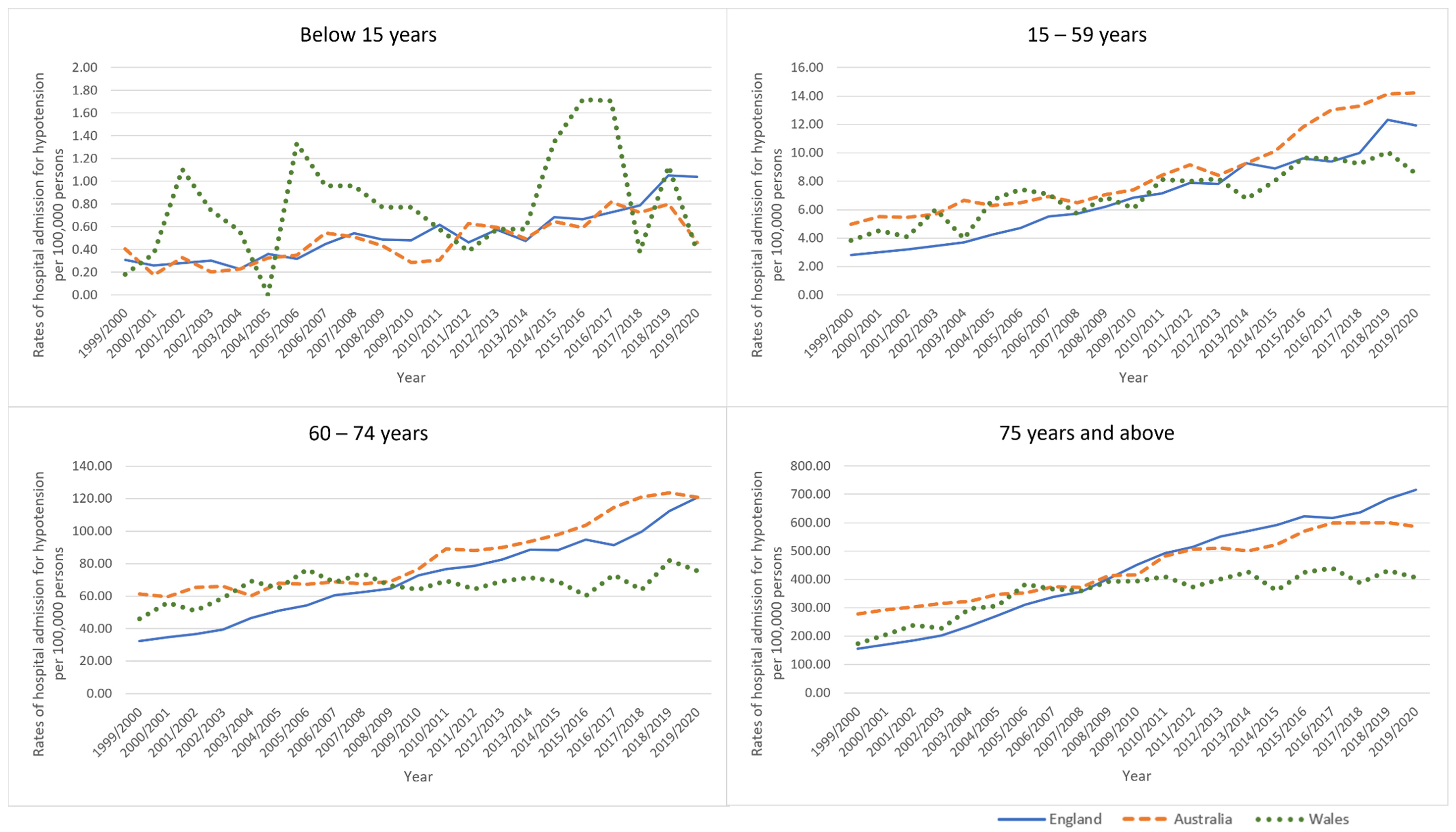
3.3. Trends in Total Hypotension Hospital Admissions Stratified by Age Group
3.4. Trends in Total Hypotension Hospital Admissions Stratified by Gender
3.5. Trends in Types of Hypotension Hospital Admissions
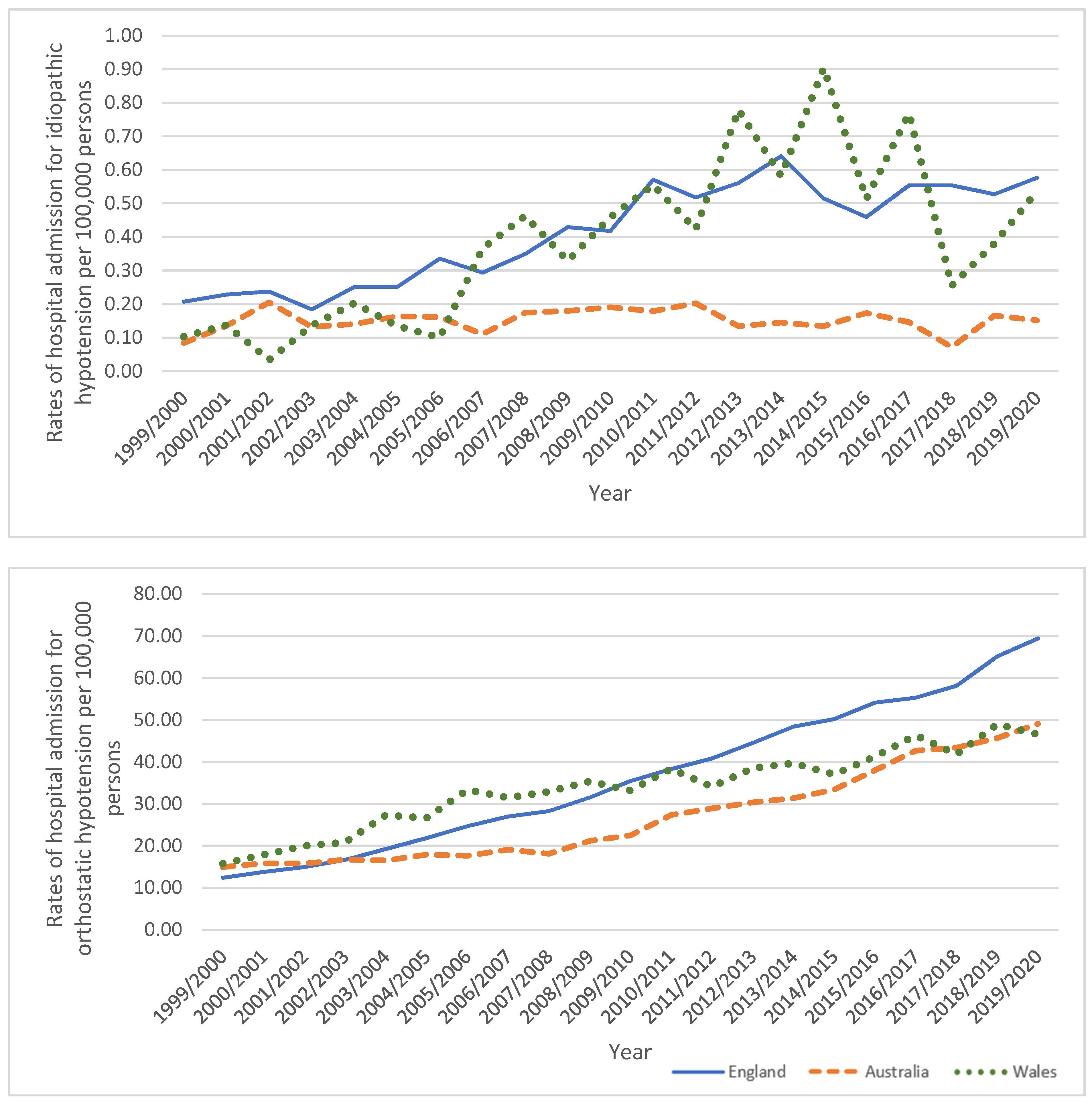
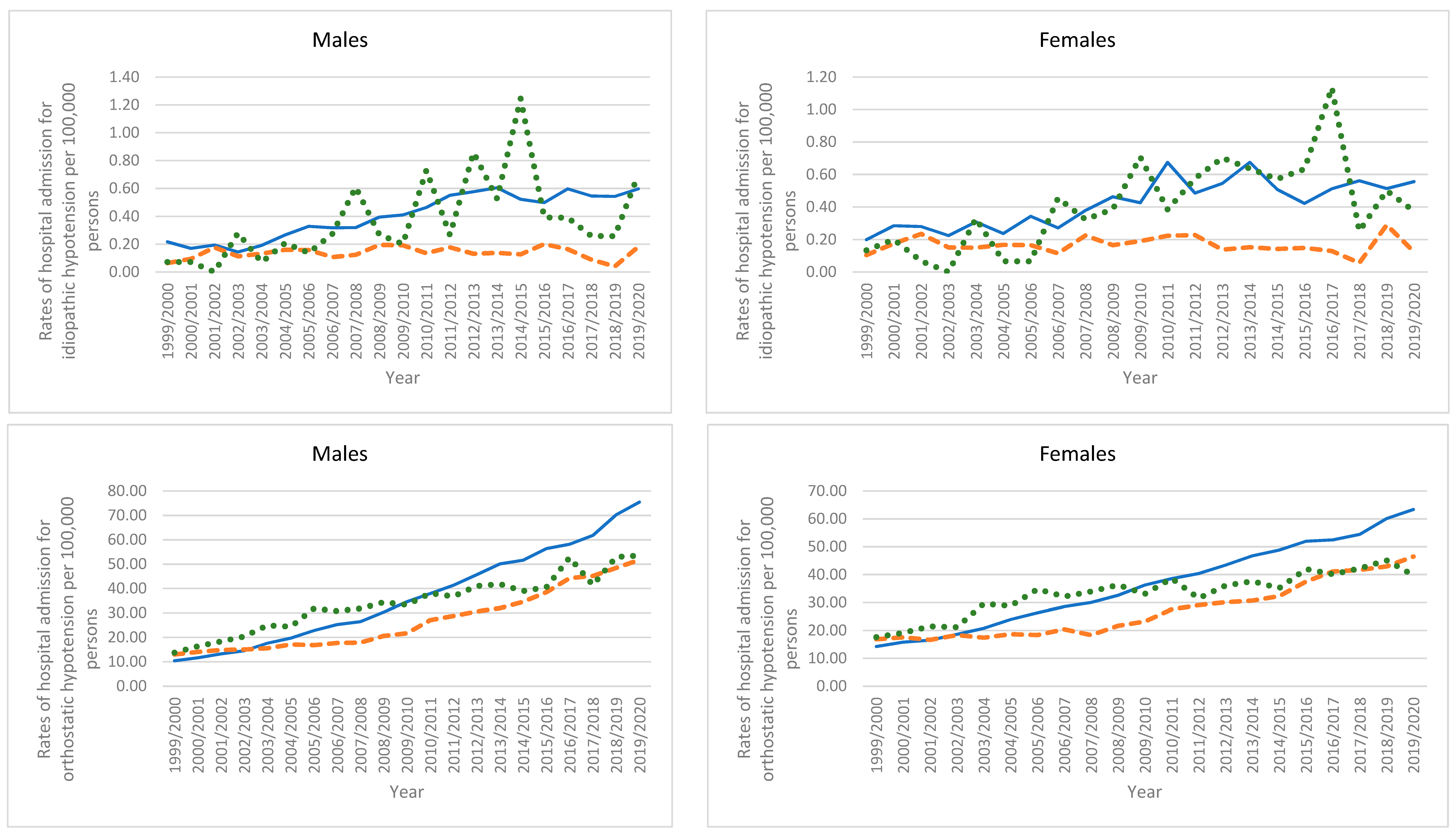
3.5.1. Idiopathic Hypotension
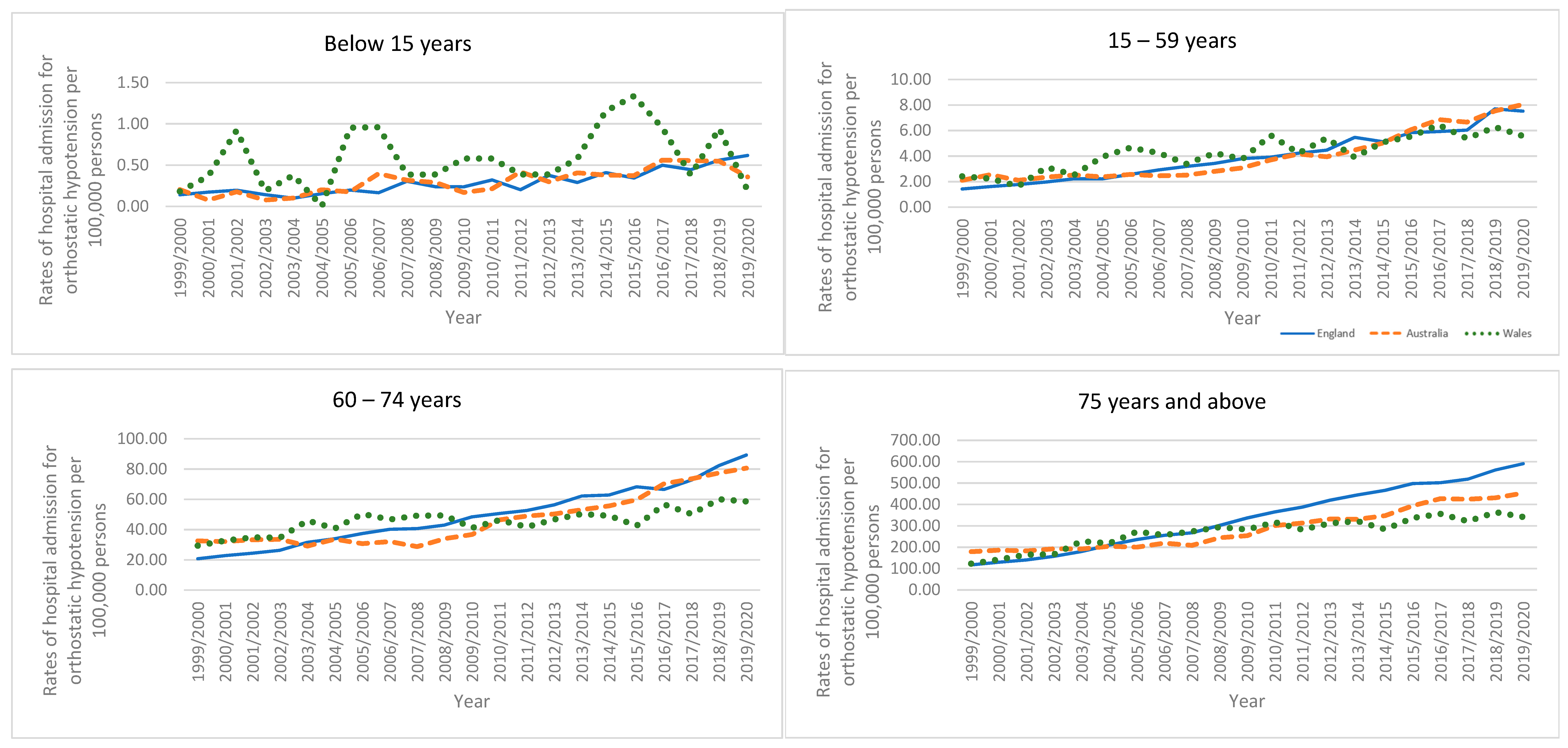
3.5.2. Orthostatic Hypotension
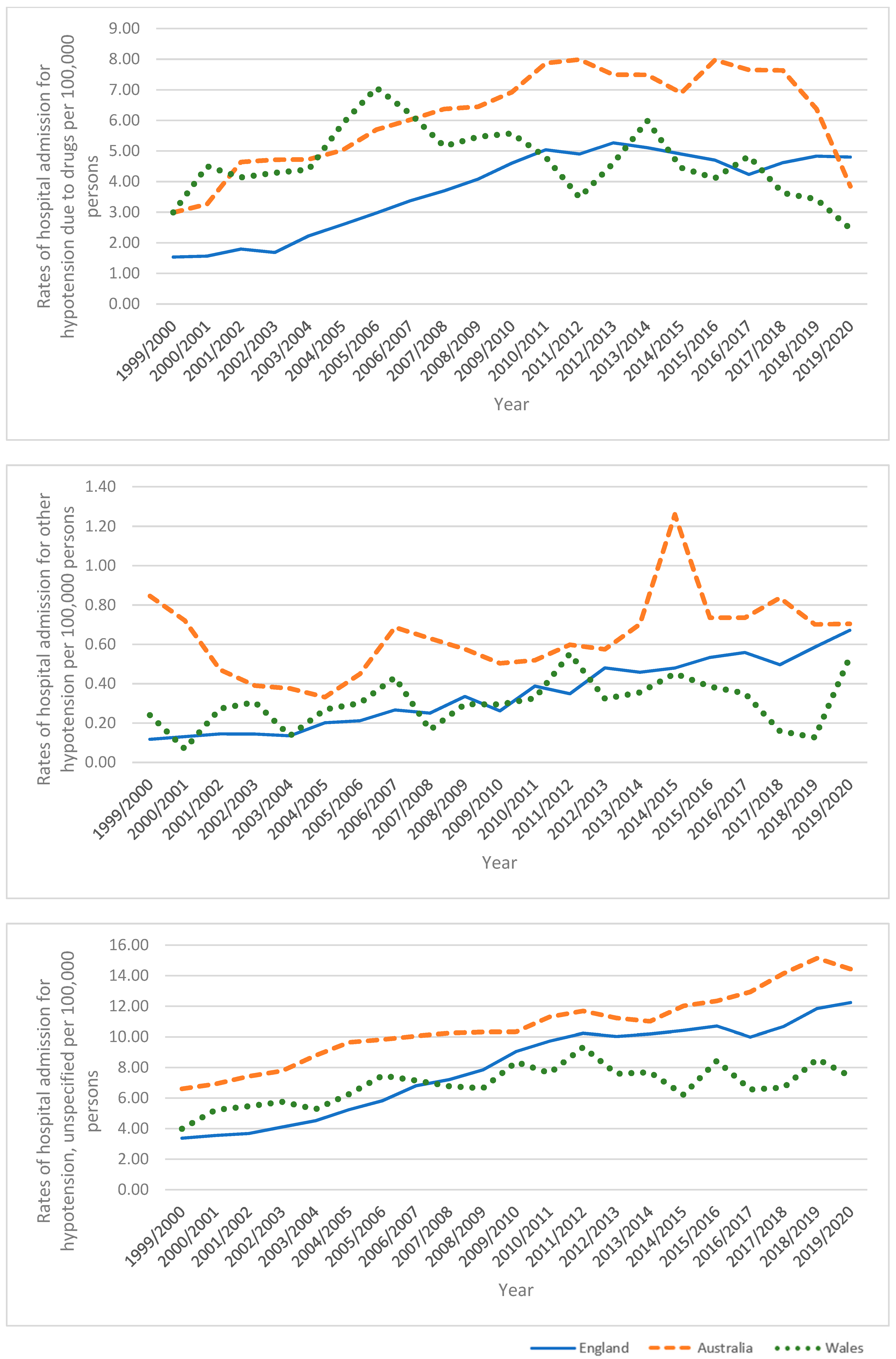
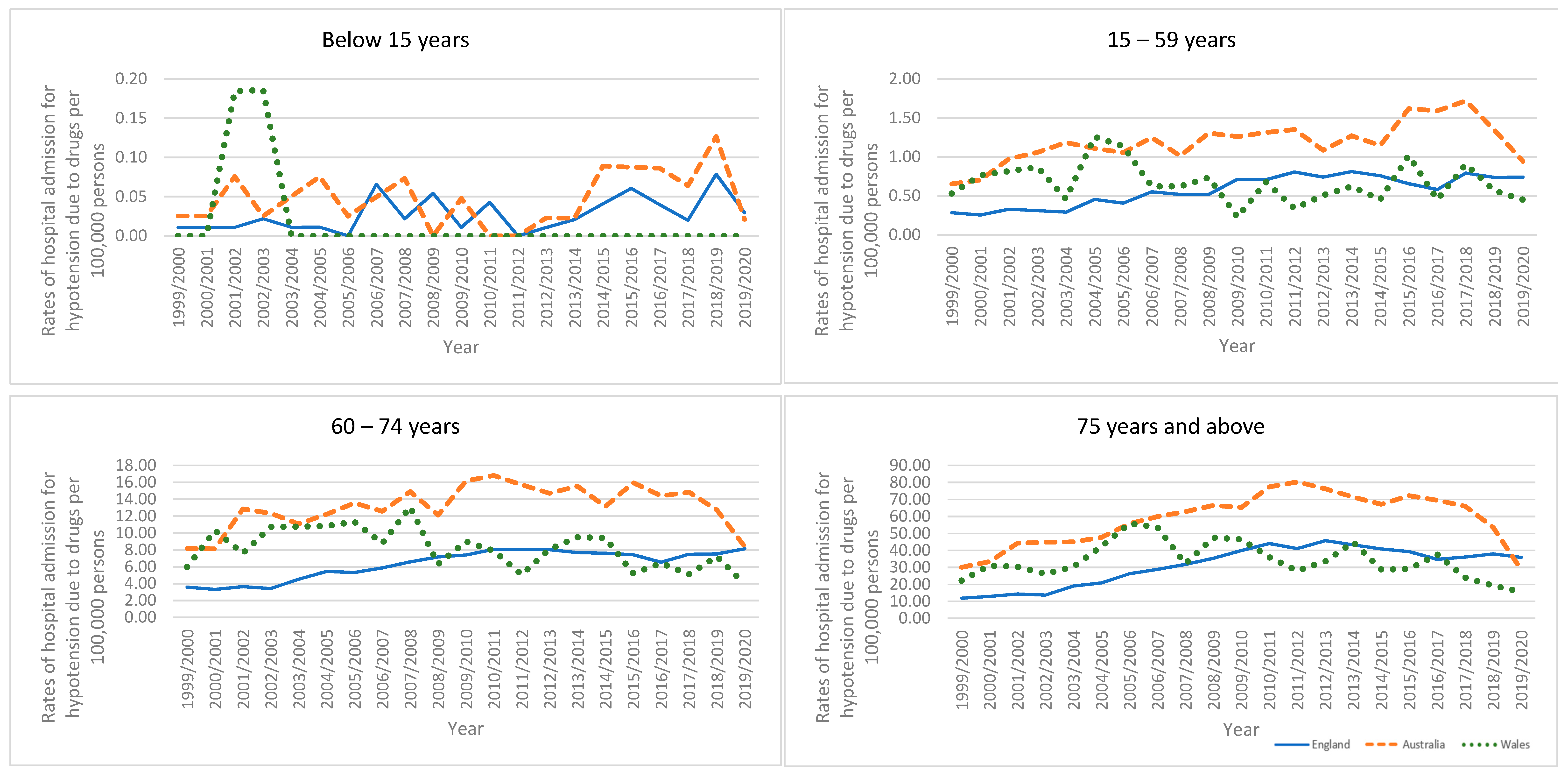
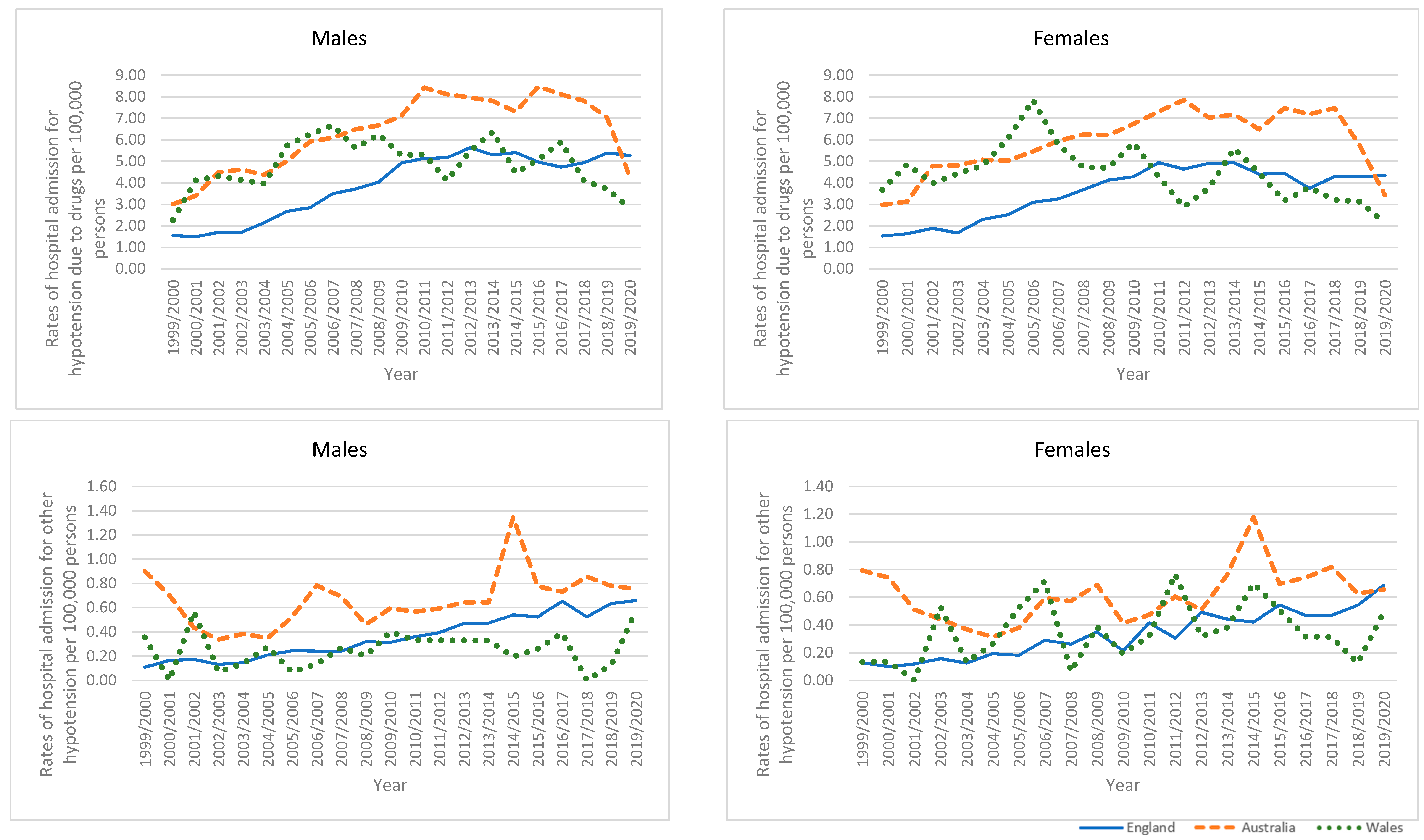
3.5.3. Hypotension Due to Drugs
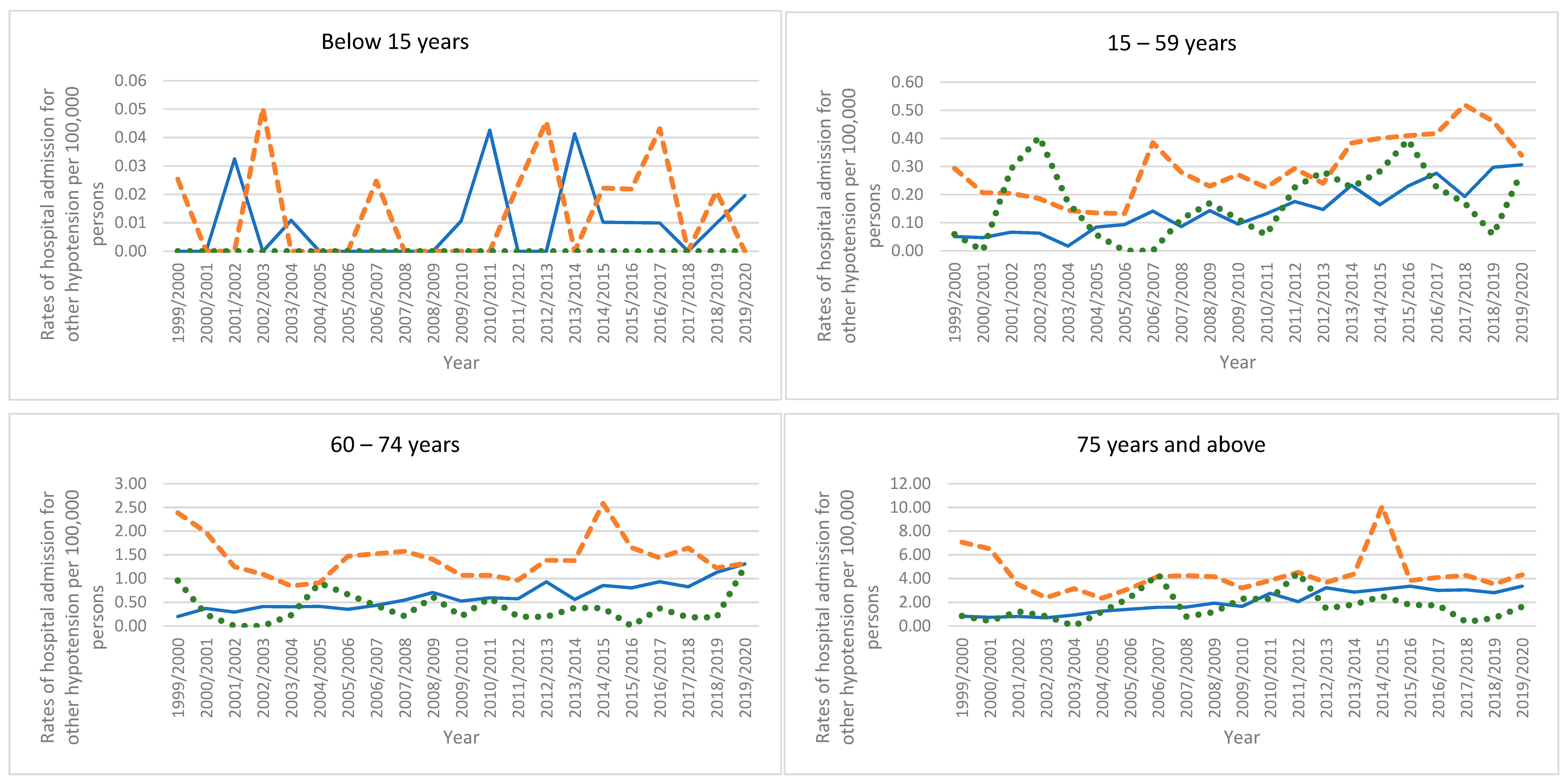
3.5.4. Other Hypotension
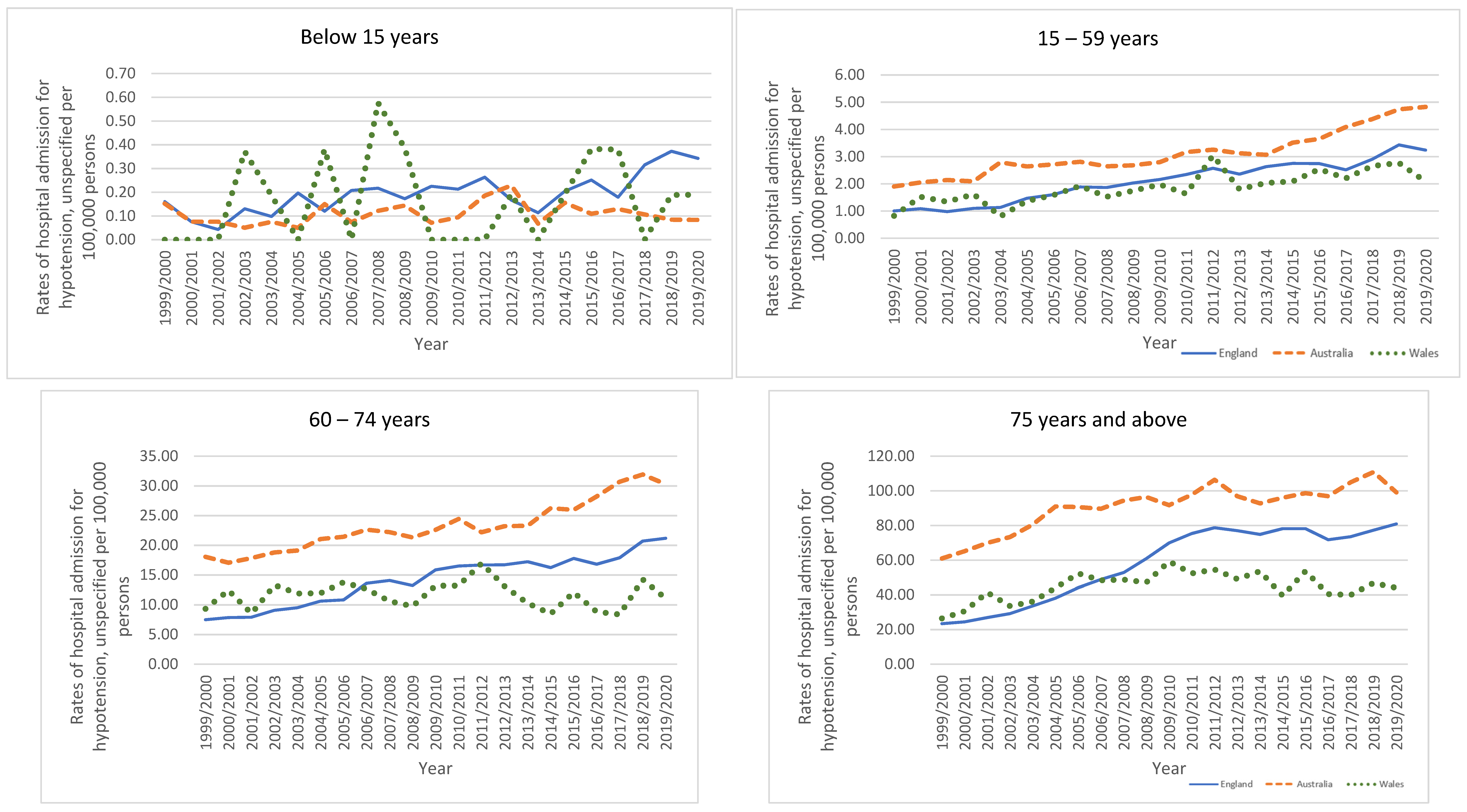
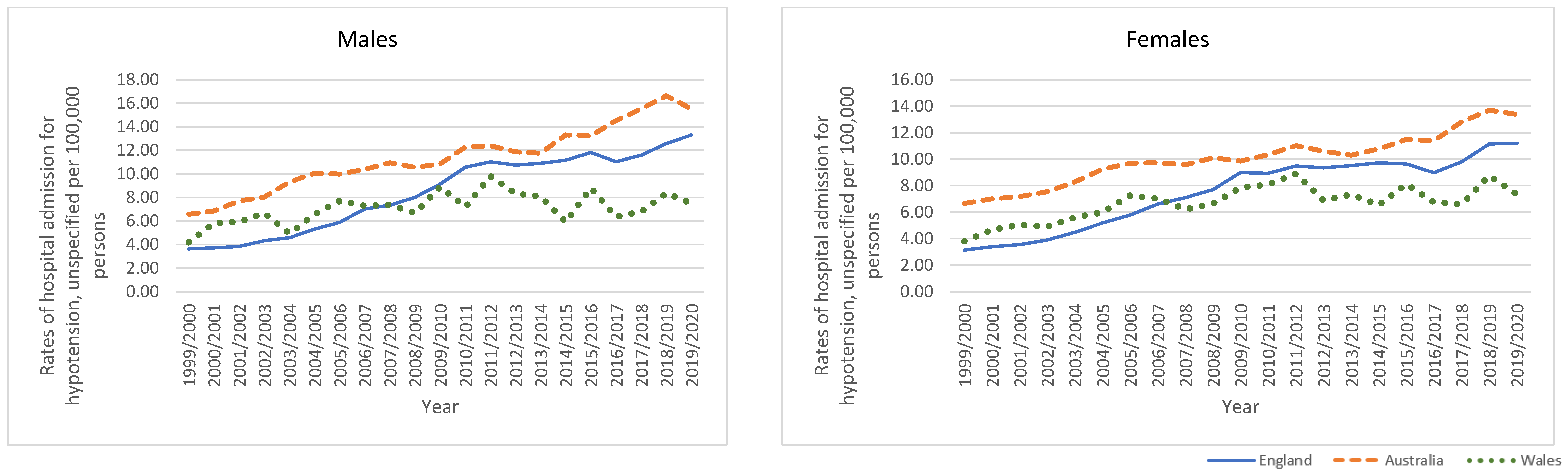
3.5.5. Unspecified Hypotension
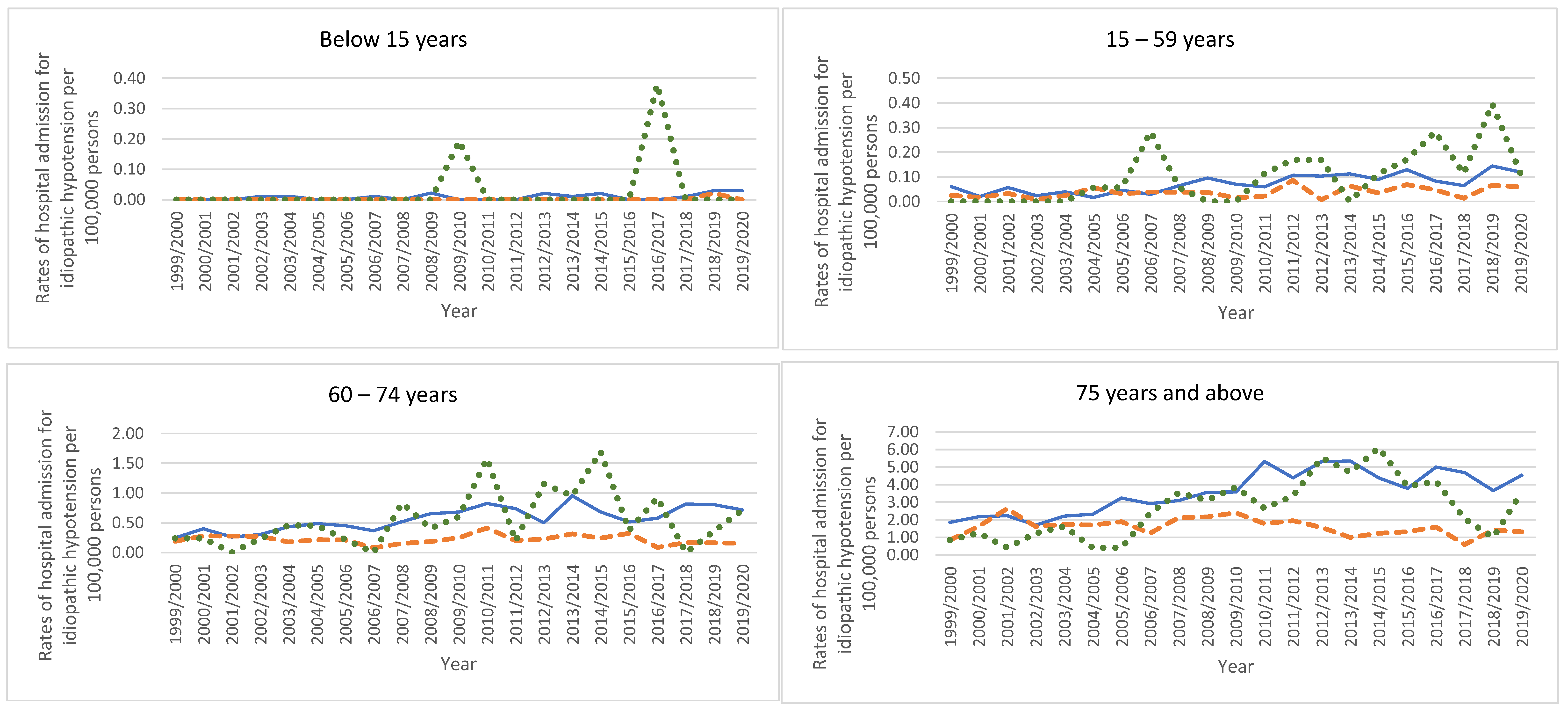
3.5.6. Trends in Types of Hypotension Hospital Admissions Stratified by Age Group
3.6. Trends in Types of Hypotension Hospital Admissions Stratified by Gender
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Looking for Trouble: Identifying and Treating Hypotension. P T A Peer-Rev. J. Formul. Manag. 2019, 44, 563–565. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6705478/ (accessed on 25 March 2023).
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K.; et al. Worldwide Trends in Hypertension Prevalence and Progress in Treatment and Control from 1990 to 2019: A Pooled Analysis of 1201 Population-Representative Studies with 104 Million Participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. High Blood Pressure Facts. 2023. Available online: https://www.cdc.gov/bloodpressure/facts.htm (accessed on 5 February 2023).
- Sharma, S.; Hashmi, M.F.; Bhattacharya, P.T. Hypotension. In StatPearls [Internet]; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Cleveland Clinic. Low Blood Pressure (Hypotension). In Cleveland Clinic. 2022. Available online: https://my.clevelandclinic.org/health/diseases/21156-low-blood-pressure-hypotension (accessed on 5 February 2023).
- National Health Service. Low Blood Pressure (Hypotension). In NHS. 2020. Available online: https://www.nhs.uk/conditions/low-blood-pressure-hypotension/ (accessed on 5 February 2023).
- Mayo Foundation for Medical Education and Research. Low blood Pressure (Hypotension)—Symptoms and Causes. In Mayo Clinic. 2022. Available online: https://www.mayoclinic.org/diseases-conditions/low-blood-pressure/symptoms-causes/syc-20355465 (accessed on 5 February 2023).
- Cleveland Clinic. Hypovolemic Shock. Available online: https://my.clevelandclinic.org/health/diseases/22795-hypovolemic-shock (accessed on 18 April 2023).
- Cooper, E. Chapter 8—Hypotension; W.B. Saunders: Philadelphia, PA, USA, 2015; pp. 46–50. [Google Scholar] [CrossRef]
- Benvenuto, L.J.; Krakoff, L.R. Morbidity and mortality of orthostatic hypotension: Implications for management of cardiovascular disease. Am. J. Hypertens. 2011, 24, 135–144. [Google Scholar] [CrossRef] [PubMed]
- Cappell, M.S. Principles and Practice of Hospital Medicine; McKean, S.C., Ross, J.J., Dressler, D.D., Scheurer, D.B., Eds.; McGraw-Hill Education Medical: New York, NY, USA, 2017. [Google Scholar]
- Ricci, F.; Manzoli, L.; Sutton, R.; Melander, O.; Flacco, M.E.; Gallina, S.; De Caterina, R.; Fedorowski, A. Hospital admissions for orthostatic hypotension and syncope in later life: Insights from the Malmö Preventive Project. J. Hypertens. 2017, 35, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Masoli JA, H.; Delgado, J.; Pilling, L.; Strain, D.; Melzer, D. Blood pressure in frail older adults: Associations with cardiovascular outcomes and all-cause mortality. Age Ageing 2020, 49, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Amnuaypattanapon, K.; Khansompop, S. Characteristics and factors associated with the mortality of hypotensive patients attending the emergency department. J. Clin. Med. Res. 2018, 10, 576. [Google Scholar] [CrossRef]
- Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics. Health and Social Care Information Centre (HSCIC). Hospital Episode Statistics. Available online: http://content.digital.nhs.uk/hes (accessed on 5 February 2023).
- NHS Wales Informatics Service. Data Quality Status Report: Admitted Patient Care Data Set. (n.d.). Available online: https://dhcw.nhs.wales/information-services/health-intelligence/annual-pedw-data-tables/pedw-publications-table/apc-dq-status-report-2019-20/ (accessed on 5 February 2023).
- AIHW. National Hospitals Data Collection—Australian Institute of Health and Welfare; Australian Institute of Health and Welfare, 2022. Available online: https://www.aihw.gov.au/about-our-data/our-data-collections/national-hospitals (accessed on 5 February 2023).
- AIHW. About the Data. Australian Institute of Health and Welfare. 2022. Available online: https://www.aihw.gov.au/reports-data/myhospitals/content/about-the-data (accessed on 5 February 2023).
- Office for National Statistics (ONS) Population Estimates. (n.d.). Available online: https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesforukenglandandwalesscotlandandnorthernireland (accessed on 5 February 2023).
- Australian Bureau of Statistics. (n.d.). About the Australian Bureau of Statistics. Abs.Gov.Au; c=AU; o=Commonwealth of Australia; ou=Australian Bureau of Statistics. Available online: https://www.abs.gov.au/about (accessed on 5 February 2023).
- Australian Bureau of Statistics. Historical Population, 2016|Australian Bureau of Statistics. Www.Abs.Gov.Au. 2019. Available online: https://www.abs.gov.au/statistics/people/population/historical-population/2016 (accessed on 5 February 2023).
- Australian Bureau of Statistics. National, state and territory population, March 2021|Australian Bureau of Statistics. Www.Abs.Gov.Au. 2022. Available online: https://www.abs.gov.au/statistics/people/population/national-state-and-territory-population/latest-release#media-releases (accessed on 5 February 2023).
- NHS Wales Informatics Service. Annual PEDW Data Tables. (n.d.). Available online: http://www.infoandstats.wales.nhs.uk/page.cfm?pid=41010&orgid=869 (accessed on 5 February 2023).
- AIHW. (n.d.); Principal Diagnosis Data Cubes, Data Cubes; Australian Institute of Health and Welfare. Available online: https://www.aihw.gov.au/reports/hospitals/principal-diagnosis-data-cubes/contents/data-cubes (accessed on 5 February 2023).
- Roser, M.; Ortiz-Ospina, E.; Ritchie, H. Life expectancy. Our World Data 2013. Available online: https://ourworldindata.org/life-expectancy (accessed on 5 February 2023).
- Roser, M.; Ritchie, H. Burden of disease. Our World in Data 2021. Available online: https://ourworldindata.org/burden-of-disease (accessed on 5 February 2023).
- Beckerman, J. Understanding Low Blood Pressure—The Basics. 2021. Available online: https://www.webmd.com/heart/understanding-low-blood-pressure-basics (accessed on 5 February 2023).
- Cheshire, W.P. Chemical pharmacotherapy for the treatment of orthostatic hypotension. Expert Opin. Pharmacother. 2019, 20, 187–199. [Google Scholar] [CrossRef]
- Ricci, F.; De Caterina, R.; Fedorowski, A. Orthostatic hypotension: Epidemiology, prognosis, and treatment. J. Am. Coll. Cardiol. 2015, 66, 848–860. [Google Scholar] [CrossRef]
- Saedon, N.I.; Tan, M.P.; Frith, J. The Prevalence of Orthostatic Hypotension: A Systematic Review and Meta-Analysis. J. Gerontol. Ser. A 2018, 75, 117–122. [Google Scholar] [CrossRef]
- Mar, P.; Raj, S.R. Orthostatic hypotension for the cardiologist. Curr. Opin. Cardiol. 2018, 33, 66–72. [Google Scholar] [CrossRef]
- AIHW. Heart, Stroke and Vascular Disease—Australian Facts, Hospital Care and Procedures; Australian Institute of Health and Welfare, 2021. Available online: https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/hsvd-facts/contents/treatment-and-management/hospital-care-and-procedures (accessed on 5 February 2023).
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef] [PubMed]
- Kocyigit, S.E.; Soysal, P.; Bulut, E.A.; Aydin, A.E.; Dokuzlar, O.; Isik, A.T. What is the relationship between frailty and orthostatic hypotension in older adults? J. Geriatr. Cardiol. JGC 2019, 16, 272. [Google Scholar] [PubMed]
- Fryar, C.D.; Ostchega, Y.; Hales, C.M.; Zhang, G.; Kruszon-Moran, D. Hypertension prevalence and control among adults: United States, 2015–2016. NCHS Data Brief 2017. Available online: https://www.cdc.gov/nchs/data/databriefs/db289.pdf#:~:text=Overall%2C%20the%20U.S.%20prevalence%20of%20hypertension%20among%20adults,significant%20differences%20were%20seen%20between%202013%E2%80%932014%20and%202015%E2%80%932016 (accessed on 14 January 2023).
- Patel, P.A.; Heizer, G.; O’Connor, C.M.; Schulte, P.J.; Dickstein, K.; Ezekowitz, J.A.; Armstrong, P.W.; Hasselblad, V.; Mills, R.M.; McMurray, J.J.V. Hypotension during hospitalization for acute heart failure is independently associated with 30-day mortality: Findings from ASCEND-HF. Circ. Heart Fail. 2014, 7, 918–925. [Google Scholar] [CrossRef] [PubMed]
- Sessler, D.I.; Sigl, J.C.; Kelley, S.D.; Chamoun, N.G.; Manberg, P.J.; Saager, L.; Kurz, A.; Greenwald, S. Hospital stay and mortality are increased in patients having a “triple low” of low blood pressure, low bispectral index, and low minimum alveolar concentration of volatile anesthesia. J. Am. Soc. Anesthesiol. 2012, 116, 1195–1203. [Google Scholar] [CrossRef] [PubMed]
- Wakefield, D.S.; Pfaller, M.A.; Hammons, G.T.; Massanari, R.M. Use of the appropriateness evaluation protocol for estimating the incremental costs associated with nosocomial infections. Med. Care 1987, 25, 481–488. [Google Scholar] [CrossRef]
- Librero, J.; Marín, M.; Peiró, S.; Munujos, A.V. Exploring the impact of complications on length of stay in major surgery diagnosis-related groups. Int. J. Qual. Health Care 2004, 16, 51–57. [Google Scholar] [CrossRef]
- Gianino, M.M.; Vallino, A.; Minniti, D.; Abbona, F.; Mineccia, C.; Silvaplana, P.; Zotti, C.M. A model for calculating costs of hospital-acquired infections: An Italian experience. J. Health Organ. Manag. 2007, 21, 39–53. [Google Scholar] [CrossRef]
- Hauck, K.; Zhao, X. How dangerous is a day in hospital? A model of adverse events and length of stay for medical inpatients. Med. Care 2011, 49, 1068–1075. [Google Scholar] [CrossRef]
- NHS. (n.d.). NHS England Reducing Length of stay. Available online: https://www.england.nhs.uk/urgent-emergency-care/reducing-length-of-stay/ (accessed on 5 February 2023).
- Rojas-García, A.; Turner, S.; Pizzo, E.; Hudson, E.; Thomas, J.; Raine, R. Impact and experiences of delayed discharge: A mixed-studies systematic review. Health Expect. 2018, 21, 41–56. [Google Scholar] [CrossRef]
- Wahba, A.; Shibao, C.A.; Muldowney, J.A.; Peltier, A.; Habermann, R.; Biaggioni, I. Management of Orthostatic Hypotension in the Hospitalized Patient: A Narrative Review. Am. J. Med. 2022, 135, 24–31. [Google Scholar] [CrossRef]
- Siddique, S.M.; Tipton, K.; Leas, B.; Greysen, S.R.; Mull, N.K.; Lane-Fall, M.; McShea, K.; Tsou, A.Y. Interventions to reduce hospital length of stay in high-risk populations: A systematic review. JAMA Netw. Open 2021, 4, e2125846. [Google Scholar] [CrossRef] [PubMed]
- Tipton, K.; Leas, B.F.; Mull, N.K.; Siddique, S.M.; Greysen, S.R.; Lane-Fall, M.B.; Tsou, A.Y. Interventions To Decrease Hospital Length of Stay. Tech. Brief 2021. Available online: https://www.ncbi.nlm.nih.gov/books/NBK574435/pdf/Bookshelf_NBK574435.pdf (accessed on 5 February 2023).
- Mayo Clinic. Low Blood Pressure (Hypotension). 2023. Available online: https://www.mayoclinic.org/diseases-conditions/low-blood-pressure/diagnosis-treatment/drc-20355470 (accessed on 18 April 2023).
- Pirmohamed, M.; James, S.; Meakin, S.; Green, C.; Scott, A.K.; Walley, T.J.; Farrar, K.; Park, B.K.; Breckenridge, A.M. Adverse drug reactions as cause of admission to hospital: Prospective analysis of 18,820 patients. BMJ 2004, 329, 15–19. [Google Scholar] [CrossRef] [PubMed]
- Schoenenberger, A.W.; Stuck, A.E. Inappropriate drug use among older persons: Is it time for action? Age Ageing 2014, 43, 737–739. [Google Scholar]
- Onder, G.; van der Cammen, T.J.M.; Petrovic, M.; Somers, A.; Rajkumar, C. Strategies to reduce the risk of iatrogenic illness in complex older adults. Age Ageing 2013, 42, 284–291. [Google Scholar] [CrossRef]
- Guthrie, B.; Payne, K.; Alderson, P.; McMurdo, M.E.T.; Mercer, S. Adapting clinical guidelines to take account of multimorbidity. BMJ 2012, 345, e6341. [Google Scholar] [CrossRef]
- Duerden, M.; Avery, T.; Payne, R. Polypharmacy and medicines optimisation. In Making It Safe and Sound; The King’s Fund: London, UK, 2013. [Google Scholar]
- Wright, A.J.; Gomes, T.; Mamdani, M.M.; Horn, J.R.; Juurlink, D.N. The risk of hypotension following co-prescription of macrolide antibiotics and calcium-channel blockers. Can. Med. Assoc. J. 2011, 183, 303–307. [Google Scholar] [CrossRef]
- Wabe, N.; Thomas, J.; Hardie, R.-A.; Dai, Z.; Imai, C.; Sezgin, G.; Li, J.; Georgiou, A. Changes in Medication Prescribing in General Practice during the COVID-19 Pandemic. 2021. Available online: https://www.mq.edu.au/__data/assets/pdf_file/0003/1170732/COVID-19-GP-snapshot-6_Prescribing_Final.pdf (accessed on 14 January 2023).
- Dale, C.E.; Takhar, R.; Carragher, R.; Torabi, F.; Katsoulis, M.; Duffield, S.; Kent, S.; Mueller, T.; Kurdi, A.; McTaggart, S. The adverse impact of COVID-19 pandemic on cardiovascular disease prevention and management in England, Scotland and Wales: A population-scale analysis of trends in medication data. MedRxiv 2022, 2012–2021. [Google Scholar] [CrossRef]
- Moynihan, R.; Sanders, S.; Michaleff, Z.A.; Scott, A.M.; Clark, J.; To, E.J.; Jones, M.; Kitchener, E.; Fox, M.; Johansson, M.; et al. Impact of COVID-19 pandemic on utilisation of healthcare services: A systematic review. BMJ Open 2021, 11, e045343. [Google Scholar] [CrossRef]
- Parekh, N.; Page, A.; Ali, K.; Davies, K.; Rajkumar, C. A practical approach to the pharmacological management of hypertension in older people. Ther. Adv. Drug Saf. 2016, 8, 117–132. [Google Scholar] [CrossRef]
- Méndez, A.S.; Melgarejo, J.D.; Mena, L.J.; A Chávez, C.; González, A.C.; Boggia, J.; Terwilliger, J.D.; Lee, J.H.; E Maestre, G. Risk Factors for Orthostatic Hypotension: Differences Between Elderly Men and Women. Am. J. Hypertens. 2018, 31, 797–803. [Google Scholar] [CrossRef]

| ICD Code | Description | Percentage from Total Number of Admissions | ||
|---|---|---|---|---|
| England | Wales | Australia | ||
| I95.0 | “Idiopathic hypotension” | 0.8% | 0.9% | 0.3% |
| I95.1 | “Orthostatic hypotension” | 74.7% | 73.5% | 61.0% |
| I95.2 | “Hypotension due to drugs” | 7.6% | 10.0% | 13.5% |
| I95.8 | “Other hypotension (Postprocedural hypotension, iatrogenic, and chronic)” | 0.7% | 0.7% | 1.4% |
| I95.9 | “Hypotension, unspecified” | 16.2% | 15.0% | 23.8% |
| Age Group | Percentage from Total Number of Admissions | ||
|---|---|---|---|
| England | Wales | Australia | |
| Below 15 years | 0.2% | 0.3% | 0.2% |
| 15–59 years | 8.3% | 8.9% | 11.9% |
| 60–74 years | 21.1% | 23.4% | 24.7% |
| 75 years and above | 70.4% | 67.4% | 63.2% |
| Rate of Hypotension in 1999 per 100,000 Persons (95% CI) | Rate of Hypotension in 2020 per 100,000 Persons (95% CI) | Percentage Change | |
|---|---|---|---|
| Below 15 years | |||
| England | 0.31 (0.20–0.42) | 1.04 (0.84–1.24) | 234.8% |
| Wales | 0.18 (−0.17–0.54) | 0.38 (−0.15–0.90) | 109.3% |
| Australia | 0.41 (0.21–0.60) | 0.46 (0.27–0.65) | 13.5% |
| 15–59 years | |||
| England | 2.82 (2.63–3.01) | 11.93 (11.56–12.31) | 323.2% |
| Wales | 3.83 (2.90–4.76) | 8.50 (7.15–9.86) | 122.2% |
| Australia | 4.98 (4.58–5.38) | 14.22 (13.62–14.82) | 185.5% |
| 60–74 years | |||
| England | 32.28 (30.90–33.66) | 120.66 (118.36–122.95) | 273.8% |
| Wales | 45.94 (39.45–52.44) | 75.64 (68.43–82.84) | 64.6% |
| Australia | 61.35 (58.00–64.70) | 120.76 (117.27–124.25) | 96.8% |
| 75 years and above | |||
| England | 155.20 (151.17–159.22) | 715.37 (707.88–722.86) | 360.9% |
| Wales | 173.41 (156.70–190.12) | 406.52 (384.00–429.04) | 134.4% |
| Australia | 277.99 (267.98–288.01) | 586.70 (575.64–597.76) | 111.0% |
| Rate of Hypotension in 1999 per 100,000 Persons (95% CI) | Rate of Hypotension in 2020 per 100,000 Persons (95% CI) | Percentage Change | |
|---|---|---|---|
| Males | |||
| England | 15.93 (15.42–16.43) | 95.33 (94.18–96.47) | 498.6% |
| Wales | 20.67 (18.29–23.04) | 65.11 (61.11–69.11) | 215.1% |
| Australia | 23.55 (22.57–24.53) | 72.48 (71.00–73.96) | 207.8% |
| Females | |||
| England | 19.24 (18.70–19.78) | 80.20 (79.16–81.23) | 316.7% |
| Wales | 25.35 (22.81–27.90) | 50.12 (46.66–53.58) | 97.7% |
| Australia | 27.38 (26.33–28.42) | 64.06 (62.69–65.44) | 134.0% |
| Rate of Hypotension in 1999 per 100,000 Persons (95% CI) | Rate of Hypotension in 2020 per 100,000 Persons (95% CI) | Percentage Change from 1999–2020 | |
|---|---|---|---|
| Idiopathic hypotension | |||
| England | 0.21 (0.17–0.25) | 0.58 (0.51–0.64) | 178.3% |
| Wales | 0.10 (−0.01–0.22) | 0.54 (0.28–0.79) | 419.7% |
| Australia | 0.08 (0.04–0.13) | 0.15 (0.10–0.20) | 80.5% |
| Orthostatic hypotension | |||
| England | 12.38 (12.07–12.69) | 69.43 (68.74–70.12) | 460.6% |
| Wales | 15.76 (14.31–17.20) | 46.57 (44.19–48.94) | 195.6% |
| Australia | 14.95 (14.40–15.50) | 49.11 (48.25–49.96) | 228.6% |
| Hypotension due to drugs | |||
| England | 1.54 (1.43–1.65) | 4.80 (4.62–4.98) | 212.7% |
| Wales | 2.99 (2.36–3.62) | 2.46 (1.91–3.01) | −17.8% |
| Australia | 2.99 (2.74–3.24) | 3.85 (3.61–4.09) | 28.6% |
| Other hypotension | |||
| England | 0.12 (0.09–0.15) | 0.67 (0.60–0.74) | 470.4% |
| Wales | 0.24 (0.06–0.42) | 0.54 (0.28–0.79) | 122.7% |
| Australia | 0.85 (0.72–0.98) | 0.70 (0.60–0.81) | −16.7% |
| Hypotension, unspecified | |||
| England | 3.38 (3.22–3.54) | 12.25 (11.96–12.53) | 262.3% |
| Wales | 3.99 (3.26–4.72) | 7.41 (6.47–8.36) | 85.8% |
| Australia | 6.61 (6.25–6.98) | 14.43 (13.97–14.90) | 118.3% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hemmo, S.I.; Naser, A.Y.; Taybeh, E.O. Hospital Admission Due to Hypotension in Australia and in England and Wales. Healthcare 2023, 11, 1210. https://doi.org/10.3390/healthcare11091210
Hemmo SI, Naser AY, Taybeh EO. Hospital Admission Due to Hypotension in Australia and in England and Wales. Healthcare. 2023; 11(9):1210. https://doi.org/10.3390/healthcare11091210
Chicago/Turabian StyleHemmo, Sara Ibrahim, Abdallah Y. Naser, and Esra’ O. Taybeh. 2023. "Hospital Admission Due to Hypotension in Australia and in England and Wales" Healthcare 11, no. 9: 1210. https://doi.org/10.3390/healthcare11091210
APA StyleHemmo, S. I., Naser, A. Y., & Taybeh, E. O. (2023). Hospital Admission Due to Hypotension in Australia and in England and Wales. Healthcare, 11(9), 1210. https://doi.org/10.3390/healthcare11091210







